Abstract
A variety of graft sources have been used for ACL reconstruction to improve functions and kinematics in ACL deficient knees. The two most commonly used autogenous grafts are the central third of the patellar tendon and the hamstring tendon constructs. The choice of different grafts and different construct influence the final clinical outcome of ACL reconstruction. The 3 groups, of 25 patients each, were generated by choosing the technique (PT tendon, 4 strand hamstring, and single hamstring plus extraarticular plasty) to utilize and followed for 5 years, with an alternate systematic sampling. Our comparison has shown significant kneeling pain in the patellar tendon with respect to the groups with hamstrings techniques. Single hamstring plus extraarticular plasty achieved subjective score significantly higher with respect to the other two groups as well as for the time to resume sport. The study confirms that patellar tendon and hamstring can be equivalent options for ACL reconstruction. This study demonstrated that a superior outcome as far as subjective clinical findings were concerned, was obtained in group III. Patients in the latter group were also able to return to sports sooner than those in the bone-patellar tendon graft group and the four-strand hamstring group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone-patellar tendon-bone reconstruction technique has been for many years the most commonly used method utilized for ACL reconstruction and its popularity and success oblige authors to use it as a basis of comparison. Post-operative disadvantages of patellar tendon include patellofemoral pain [1, 2, 9, 11, 14, 27–29, 46], quadriceps weakness [27], possible patella fracture [10, 26, 47], or rupture of patellar tendon [17, 26].
In recent years the rise of hamstring tendon grafts is due to perceptions as a lower post-operative morbidity compared with patellar tendon graft. Hamstring concerns are failure to achieve immediate rigid fixation, lower stiffness compared to patellar tendon or native ACL, mild loosening at long term follow-up [1, 2, 8, 16, 19, 33, 34, 43, 44, 52], incidence of increased tunnel size [15, 32] and weakness of hamstring with difficulties controlling internal tibial rotation [4, 12].
In the literature several prospective studies have compared the two grafts [1–3, 6, 8, 9, 16, 18–20, 23, 26, 35, 37, 38, 40, 44].
However, only Aglietti [2] and Pinczewski [40] studies have more than 5 years follow-up and many intraoperative and postoperative variables as well as the inclusion criteria of these studies make difficult to analyze the data obtained.
Extraarticular reconstructions have been combined with both grafts to reduce the amount of rotational laxity [3, 14, 33, 49]. Roth [42], Strum [49] and Barrett [7] have found no significant clinical improvement with the use of an extraarticular plasty. While Lerat [31] and Noyes [36] have found an increased success rate by the addition of an extraarticular procedure.
Only Anderson [3] has compared prospectively patellar tendon to hamstring reconstruction plus extraarticular plasty. Beynnon [9] and O’Neill [37] have compared patellar tendon versus two strand hamstring graft. In all these three randomized clinical trial [3, 9, 37] the use of hamstring graft led to a worse clinical outcome.
Five years ago we began a prospective randomized study to compare the gold standard patellar tendon graft with a four strand hamstring graft and with a two strand hamstring graft combined with an extraarticular plasty to reduce rotational laxity.
The purpose of this study was to analyze the subjective, objective and radiographic performances of these reconstructions to evaluate the graft selection as well as different surgical solutions for ACL rotational laxity.
Materials and methods
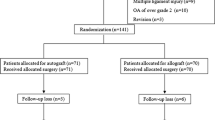
In 1998 a prospective randomized study was designed to compare three different methods of ACL reconstruction. The inclusion criteria to be part of the study were: no prior knee surgery, no meniscus injury, normal contralateral knee, no chondral injury, no sign of joint degenerative changes, no history of patello-femoral pain, age less than 50 years, intact PCL and maximum grade 1 MCL injury. All patients should be involved in cutting sports at competitive or amateur level. Of the 311 patients that were evaluated at our Clinic for ACL rupture in 1998 (min 4 week–max 1 year, mean value 6 months), we were able to recruit 75 patients to be included in the study meeting the inclusion criteria. The 3 groups, of 25 patients each, were generated by choosing the technique to utilize, with an alternate systematic sampling, under a previous consent of the patient.
Group 1 consisted of 25 patients treated with bone patellar tendon bone graft. In group 2 ACL reconstruction was performed with four strand hamstring tendon. Group 3 included ACL reconstruction with two strand hamstring plus extraarticular plasty.
The mean age of the 75 patients was 29.5 years (min 15, max 49). Forty-nine patients were male and 26 were female. The right knee was involved in 47 patients and the left 1 in 28.
There were no significant differences among the three groups pre-operatively regarding age, sex, time from injury to surgery, pre-injury activity level, ROM, KT 2000 measurements, comparing the A-P laxity of the injured knee to the contralateral uninjured knee, and radiographic changes (Table 1).
All ACL reconstructions were performed by the same surgeon (SZ), evaluations were executed by two independent surgeons at post resident fellowship. All patients underwent the same post operative rehabilitation protocol.
Surgical techniques
Group I (Bone-patellar tendon-bone)
The patellar tendon autograft was harvested through a single midline incision. Central third of the ipsilateral patellar tendon was used in all cases. A 9 mm central portion of the tendon was removed with the bone plugs taken from patella and tibial tubercle. The bone plugs were approximately 9 mm width and 25 mm of length; 9 mm diameter was chosen because in the hamstring reconstruction the tunnel was drilled of this diameter, in order to have a good press fit. In this way the two groups were similar at least for tunnel size. A 2 mm guide pin was placed at the junction of middle and posterior third of ACL insertion area at the tibia. Then a 9 mm tibial tunnel was drilled, according to Howell’s [24, 25] suggestion for tibial tunnel angle. The femoral tunnel of the same size was performed through the tibial tunnel with a classic half tunnel technique [13]. The femoral tunnel was drilled to a depth of 3 cm. The bone-patellar tendon-bone autograft was passed through the tibial and femoral tunnels with a suture passer and fixed in the femur and tibia with metal interference screw. The interference screw (Smith and Nephew Endoscopy) size was different depending on the filling of the tunnel by the bone plug and usually was 7–9 mm screws and 1 mm less in diameter in the femur respect to the tibia to avoid breakage of the posterior cortical wall. Ten cycles of the knee were performed for graft pretensioning. Fixation of the graft was at 20° of knee flexion. Graft was tensioned with maximal manual force applied. Graft length and tunnel length mismatch was never encountered.
There was no bone grafting of the harvest sites and peritendon closure was performed.
Group II (Four strand hamstrings)
In this technique, ST-G tendons were isolated and harvested through a medial incision on the pes anserinus. Ends of the tendons were detached and sutured together. In all cases we were able to achieve a complete four strand graft. The graft was prepared on the graft master in tension to achieve a four strand construct. In our series the four strand hamstring for men was modeled always at 9 mm using a cylindrical calliper (Acufex) in order to have a good press-fit in the tunnel and similar tunnel size to group one. For the ten women only four have a 8 mm graft, but we decided to drill 9 mm to have comparable tunnel size and we used in these cases a bigger interference screw. The others six cases reached 9 mm of construct.
The tibial and femoral tunnels were performed as for the group I. The polyester-tape of the endobutton was tied at a length equivalent to the length of the small femoral tunnel going from the graft to the endobutton plate outside the femoral cortex. After femoral fixation with the flipped endobutton, the remaining part of the tendons were fixed with interference screw in the tibial tunnel (after execution of ten cyclic knee bendings with graft tensioned). The screw used was of the polylactic absorbable type (Smith and Nephew Endoscopy, Andover, MA, USA) and their size was normally of the same size of the tunnel in order to achieve a good graft stability. However in the cases with smaller graft bigger diameter screws were used. During graft fixation the knee was at 20° of flexion. This degree was chosen in order to have similar condition respect to group I.
Group III (ST-G intra and extra-articular reconstruction)
The original technique has been already described by the senior author [33].
This technique involves the use of a single limb of ST-G sutured together. The tibial insertion of the tendons was left intact. The tendons were passed through the tibial tunnel and “over the top”. Ten cycles of the knee were performed for graft pretensioning at maximum tension from 0° to 120°. The tendons were then fixed in the cortical bone of the femur at the end of the lateral condyle with two staples with the knee at 90° of flexion. Then the remaining part of the graft was fixed with a single staple in manual maximum tension to Gerdy’s tubercle as an extra-articular plasty keeping the tibia in a forced external rotation and at the same flexion angle. In this reconstruction a different fixation angle was chosen compared to other two groups because with “over the top” technique to obtain a good tension of the graft in extension, the tendons should be fixed in a flexion angle.
Postoperative protocol
All patients received the same postoperative protocol. No brace were used. Range of motion, quadriceps muscle active exercises, straight leg raises, prone hamstring muscle stretching exercises were all begun the day after surgery. Functional muscle stimulation was used 2 h three times daily for 4 weeks. Patients were allowed partial weight-bearing during the first 2 weeks, and full passive extension and active flexion over a range of 0–120° from the third postoperative day in isometric and isotonic fashion. At 2 weeks postoperatively full weight bearing was allowed. Stationary biking, active knee extension with weights and one-quarter squats were introduced at 4 weeks after surgery. All exercises were done always under the direction of a physical therapist in a routine fashion that control patient compliance to the program.
Proprioceptive exercises were started at 4 weeks, running at 2 months, and sports activities after the 4 month. Patients were allowed to return to full sports activities when muscle atrophy of operated leg was equal or less 1 cm respect to contralateral leg and one leg hop was more than 90%. These measurements and decisions were made by the surgeon and the physical therapist.
Functional assessments
IKDC score (A, normal; B, nearly normal; C, abnormal; D, severely abnormal) was recorded for every patient. According to the IKDC recommendation, the final result in each patient was the lowest grade in any category that they had. Subjective evaluation was also performed with IKDC subjective score (0 being worst possible-100 being normal).
Pre and post-op Tegner score [50] was evaluated at the follow up to assess the functional capability of the knee.
Thigh circumference at 5 and 15 cm above the patella to evaluate muscle performance restoration and one leg hop test was also executed.
Anterior knee pain as well as kneeling pain was recorded in each group.
The patients were classified as having subjective anterior knee pain if they registered pain during stair walking, sitting with knee in 90° of flexion, and during or after activity. All functional assessments were performed at 5 years follow up.
Knee laxity was determined by clinical evaluation with Pivot shift test (laxity score as 0, +1, +2, +3), the manual Lachman test (grades as 0, +1, +2, or +3) and by the KT-2000 arthrometer test (MED metric corp, San Diego, CA, USA) evaluating manual maximum displacement, quadriceps active test and passive displacement test at 30 pounds, comparing the A-P laxity of the injured knee to the contralateral uninjured knee.
Evaluation of ROM was performed comparing the operated knee with contralateral one, flexion loss was estimated with the patient in the supine position as the angular difference in maximum active flexion. Extension loss was measured with the patient in the prone position.
Time required returning to sports activities after surgery was also analyzed.
No complications (infections, sepsis or DVT) were observed in all three groups; therefore no patient was excluded from the study for complications.
Radiographic evaluation
The day before surgery antero-posterior, lateral X-ray and Rosenberg radiographs [41] were performed in every patient of the three groups. At 5 years follow-up the same projections were performed. Tunnel enlargement and placement of the graft were evaluated and compared with postoperative control immediately after surgery.
To determine the tunnel enlargement, we measured femoral and tibial tunnels in both coronal and sagittal planes. The femoral tunnel widening was measured longitudinal to the sclerotic tunnel wall at 1 and 2 cm proximal to the tunnel origin, and the tibial tunnel was measured in the same way, but at 1 and 2 cm distal to the tibial plateau [39]. Measurements were compared to the original tunnel size at time of surgery.
In relationship to tunnel placement, femoral tunnel placement was measured on the lateral radiograph, by determination of the distance from the posterior aspect of the Blumensaat’s line to the posterior margin of the femoral tunnel. Measurements of tibial tunnel placement were determined by Good method, analizing the inner orifices position respect to sagittal depth of medial plateau at the bone cartilage junction [21]. With this method, antero-posterior tunnel placement can be determined.
Degenerative joint disease was evaluated measuring the tibiofemoral space on Rosenberg X-ray at pre-operative and follow up control, considering presence of degenerative changes when a difference of 2 mm or more was present between pre-op and follow-up control [41]. The Rosenberg projection was performed by our radiologist in a standardize setting to reduce bios.
Ethics
The Ethics Committee of Rizzoli Orthopedic Institute approved our prospective randomized study.
Statistical analysis
All continuous data were expressed in terms of mean and standard deviation of the mean. To evaluate differences between and among groups, One Way ANOVA and Pearson Chi Square Test evaluated by Monte Carlo method for small samples have been performed.
Post hoc power analysis was performed to non-significant tests.
For all tests P<0.05 was considered significant.
Statistical analysis was performed by means of SPSS 7.5.
Results
IKDC evaluation was normal or nearly normal in all three groups with mean range 72–84% without significant difference (Table 2, Fig. 1).
On the contrary subjective IKDC evaluation for the first and the third group had significantly higher scores than the second group (P = 0.04) (Table 2).
The Tegner score was almost equal in the three groups (Table 2).
The muscle thigh circumference at 5 cm (P = 0.02) and 15 cm to the top of the patella was greater for the patellar tendon group in comparison to the other two groups, considering that no patella baja was found in the first group (Table 2).
One leg hop test was similar in all three groups.
Anterior knee pain and kneeling pain (P = 0.0001) were higher in the patellar tendon group compared to the other two hamstring groups (Table 2).
There was a trend to less pathologic laxity in group I and III (Pivot and Lachman tests) compared to group II. In fact the Pivot shift test was negative in 88% in group I and 92% in group III, these scores were significantly higher (P = 0.03) respect to group II (64%); while for Lachman test we had 88% no laxity in group I, 78% in group II and 92% for group III (Table 3).
KT 2000 arthrometer revealed laxity in the groups I and III compared with group II, in particular the quadriceps activity test showed a significant laxity (P = 0.0492) in the II group respect the other ones (Table 4).
Post operative range of motion among the three groups, was significantly different: patellar tendon group showed a trend to higher extension and flexion (P = 0.03) deficit compared to the other two groups (Tables 5, 6).
All patients returned to the same sports practiced before trauma. However the time to return to sport was shorter for the third group respect to the other two, and this data was statistically significant (P = 0.05) (Table 7).
About radiographic evaluation, the tibial tunnel enlargement was significantly higher in the second group respect to the other ones (P = 0.03) (Table 8). Moreover the II group showed a femoral tunnel enlargement higher respect to the I group (Table 8).
Regarding arthritic changes [41], only one case in group II showed narrowing of the medial cartilage space of more than 2 mm comparing the preoperative Rosenberg views with those at final follow-up.
No hardware removal was necessary in all three groups.
Discussion
The overall results with these surgical techniques were satisfactory. To maximize the strength of our study we used strict inclusion criteria to reduce the number of potentially confounding variables. The surgical techniques for PT and double loop hamstring group were similar, except the graft and the femoral fixation of the hamstring group where an endobutton system was utilized. Group 3, on the contrary, have different fixation methods for tibial and femoral side and the tibial tunnel was slightly smaller. We were aiming to specifically really evaluate the effectiveness of surgical reconstruction without any associated pathology that could influence on laxity and osteoarthritic changes at five years follow up. This goal was confirmed by the fact that only one patient had degenerative change as demonstrated by joint space narrowing at the final follow-up [41]. The X-ray evaluation also confirmed that the tunnel position in frontal and lateral planes was correct in all three groups, permitting us to consider only the graft performance and the extraarticular plasty in the third group. The findings of this study are different to those of Anderson [3] and Beynnon [9] that showed better performance and stability for BPTB group. Anterior knee pain for patellar-tendon reconstruction has been found as a minor problem for Beynnon [9], Aglietti [1, 2], Anderson [3] and Marder [35]. On the contrary our results are in line with the longer follow up study of Pinczewsky [40], Eriksson [19] and Feller [20].
The results of our four strand hamstring are lower in these evaluations: Tegner score, IKDC, muscle tight circumference (15 cm), KT 2000 (manual max displacement and 30 pounds test), tunnel enlargement (femoral), but not significantly different respect to PT group. This data are in line with Pinczewsky [40] and Feller [20] studies with 5 and 3 years follow up respectively and with other authors at shorter follow up [9]. On the contrary the two strand hamstring graft plus extra-articular plasty group has superior outcome with respect to the other two groups and differs from the literature. Only Anderson [3] and Beynnon [9] have prospectively evaluated the two strand hamstring graft with PT and only Anderson has evaluated the use of an extra-articular plasty with a two strand hamstring reconstruction. Beynnon [9] has found significant difference regarding ACL laxity: 86% of normal pivot shift for PT group with respect to 59% for the two strand hamstring group. In our series at 5 years we did find better ACL laxity (P = 0.03) for PT and two strand hamstring with extraarticular plasty groups compared to the four strand hamstring group (Table 3).
The difference between our results and those of Beynnon [9] could relate to the use of extra-articular plasty.
However there are other important factors that differ in the two studies. First of all, our two strand technique was performed utilizing over the top position and maintaining the tibial tendon insertion intact. In Beynnon study a staple was put distal to the tibial tunnel affecting the vascular supply of the tendons.
We have observed [51] that the tibial hamstring insertion is well vascularized and innerved by vessels and nerves that proceed along the tendon unit. Preservation of this neurovascular supply could enhance the neoligamentization process that is still not well understood, permitting easier and faster resumption of graft biology. Another important difference about results between our series and those of Anderson [3] and Beynnon [9] was the post-op rehabilitation protocol. These studies used conservative rehabilitation. A knee brace was utilized with restricted range of motion and restricted active exercise. Recently Arnoczky [5] and Lavagnino [30] have demonstrated that the biological response of cells and the ultimate remodeling of the ACL graft appear to be governed in large part by the mechanical environment to which the graft is exposed. This suggest the importance of initial graft placement and tensioning, that is still not completely understood, as well as immediate application of cyclic loading to stimulate anabolic activity of the transplanted graft.
The fixation angle of the graft is again extremely important. In the third group the hamstring graft was fixed at 90 degrees. According to Feller [20], hamstring graft fixation at 70°, we believe that this 90° of flexion improves final knee stability. This is not only in relation to the over the top position but also considering the different viscoelastic properties of the two graft type. Hoher [22] has shown that in hamstring graft reconstruction the stress relaxation with preconditioning was 48 and 42% depending on the type of construct. Fixation of hamstring at 90°, certainly decreases the elongation of the tissue due to its viscoelastic properties. The difference of fixation angle respect to the II group could also explain the better stability achieved results in the III group. The over the top position is non anatomic site of attachment for the graft compared to the other two groups and certainly it could have also influenced the final results.
Anderson [3] has found that an extraarticular procedure did not improve the result of intraarticular hamstring reconstruction increasing the incidence of patello femoral crepitation and loss of motion. Also Roth [42] and Strum [49] have underlined the risk of excessive load of lateral compartment. In the Anderson [3] series a passive lateral plasty was used with a large lateral exposure and tightening of iliotibial tract. Such a procedure certainly affects the patellofemoral joint and could explain the difference in results. Our lateral plasty is performed with the remnant part of the graft after fixation on the lateral aspect of the femur and practically it is a single unit with the intraarticular graft. In our series no lateral compartment degeneration, in relation to the lateral plasty, was observed as also underlined in Lerat series [31].
No fixed flexion deformity was found in our patellar tendon group, while Pinczewsky [40] observed at 5 years follow up 31% of flexion deformity in patellar tendon group, compared with 19% of the hamstring group. A possible explanation is that in our groups we did not observed any osteoarthritic changes except for one case. The resumption of the same activity level was comparable in all groups as was observed by Pinczewsky [40].
A higher incidence of tunnel widening was seen in the four strand hamstring group with respect to the patellar tendon group and also to the two hamstring group. L’Insalata [32] and Clatworthy [15] have observed this phenomena and have underlined that there is no detrimental effect on final laxity. However, the four strand hamstring group had the lower value regarding laxity.
The limit of this study is that a higher number for each group could have enhanced the power of the results obtained.
In conclusion the IKDC score showed similar results for these three groups suggesting that the graft choice is not influencing the final clinical outcome of ACL reconstruction. However analyzing in detail the results obtained, the technique with lateral plasty showed a significantly better subjective evaluation, a faster return to sport, less kneeling pain and a higher capacity of return to normal muscle trophysm.
Therefore we agree with the conclusion of a recent work of Spindler [48] that the graft type may not be the primary determinant for successful outcomes after ACL surgery.
The success of a surgical reconstruction depends on many biomechanical and biological factors such as the properties and construction of the graft, the correct placement of the tunnels, the type of fixation, the control of rotational stability and kinematic performance of the graft, the post-operative program and the biological stimuli that affect the ligamentization and tunnel fixation process.
The variety of all these different parameters, not only the type of the graft, should be taken into account and completely evaluated, to fully understand the variables that are responsible of the final results of ACL reconstruction.
References
Aglietti P, Buzzi R, Zaccherotti G, De Biase P (1994) Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med 22(2):211–218
Aglietti P, Zaccherotti G, Buzzi R, De Biase P (1997) A comparison between patellar tendon and doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. A minimum 5 year f.u.. J Sports Traumatol Rel Res 19:57–68
Anderson AF, Snyder RB, Lipscomb AB Jr (2001) Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am J Sports Med 29:272–279
Armour T, Forwell L, Litchfield R et al (2004) Isokinetic evaluation of internal/external tibial rotation strength after the use of hamstring tendons for anterior cruciate ligament reconstruction. Am J Sports Med 32(7):1639–1643
Arnoczky SP, Lavagnino M, Gardner KL, Tian T, Vaupel ZM, Stick JA (2004) In vitro effects of oxytetracycline on matrix metalloproteinase-1 mRNA expression and on collagen gel contraction by cultured myofibroblasts obtained from the accessory ligament of foals. Am J Vet Res 65(4):491–496
Aune AK, Holm I, Risberg MA et al (2001) Four strand hamstring tendon autograft compared with patellar tendon bone autograft for anterior cruciate ligament reconstruction. A randomized study with two years follow up. Am J Sports Med 29:722–728
Barrett GR, Richardson KJ (1995) The effect of added extra-articular procedure on results of ACL reconstruction. Am J Knee Surg Winter 8(1):1–6
Beard DJ, Anderson JL, Davies S, Price AJ, Dodd CA (2001) Hamstrings vs. patella tendon for anterior cruciate ligament reconstruction: a randomised controlled trial. Knee 8(1):45–50
Beynnon BD, Johnson RJ, Fleming BC, Kannus P, Kaplan M, Samani J, Renstrom P (2002) Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts. A prospective, randomized study. J Bone Joint Surg Am 84(9):1503–1513
Bonatus TJ, Alexander AH (1991) Patellar fracture and avulsion of the patellar ligament complicating arthroscopic anterior cruciate ligament reconstruction. Orthop Rev 20(9):770–774
Brandsson S, Faxen E, Eriksson BI et al (1998) Closing patellar tendon defects after anterior cruciate ligament reconstruction: absence of any benefit. Knee Surg Sports Traumatol Arthrosc 6(2):82–87
Carofino B, Fulkerson J (2005) Medial hamstring tendon regeneration following harvest for anterior cruciate ligament reconstruction: fact, myth, and clinical implication. Arthroscopy 21(10):257–265
Chen L, Cooley V, Rosenberg T (2003) ACL reconstruction with hamstring tendon (Review). Orthop Clin North Am 34(1):9–18
Clancy WG Jr, Nelson DA, Reider B, Narechania RG (1982) Anterior cruciate ligament reconstruction using one-third of the patellar ligament, augmented by extraarticular tendon transfers. J Bone Joint Surg Am 64(3):352–359
Clatworthy MG, Annear P, Bulow JU, Bartlett RJ (1999) Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthros 7(3):138–145
Corry IS, Webb JM, Clingeleffer AJ, Pinczewsky LA (1999) Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four strand hamstring tendon autograft. Am J Sports Med 27(4):444–454
DeLee JC, Craviotto DF (1991) Rupture of the quadriceps tendon after a central third patellar tendon anterior cruciate ligament reconstruction. Am J Sports Med 19(4):415–416
Ejerhed L, Kartus J, Sernert N, Kohler K, Karlsson J (2003) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med 31(1):19–25
Eriksson K, Anderberg P, Hamberg P et al (2001) A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 83(3):348–354
Feller JA, Webster KE (2003) A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 31(4):564–573
Good L, Odensten M, Gillquist J (1987) Precision in reconstruction of the anterior cruciate ligament. A new positioning device compared with hand drilling. Acta Orthop Scand 58(6):658–661
Hoher J, Scheffler SU, Withrow JD, Livesay GA et al (2000) Mechanical behavior of two hamstring graft constructs for reconstruction of the anterior cruciate ligament. J Orthop Res 18(3):456–461
Holmes PF, James SL, Larson RL et al (1991) Retrospective direct comparison of three intraarticular anterior cruciate ligament reconstructions. Am J Sports Med 19(6):596–600
Howell SM, Wallace MP, Hull ML, Deutsch ML (1999) Evaluation of the single-incision arthroscopic technique for anterior cruciate ligament replacement: a study of tibial tunnel placement, intraoperative graft tension, and stability. Am J Sports Med 27(3):284–293
Howell SM, Gittins ME, Gottlieb JE, Traina SM, Zoellner TM (2001) The relationship between the angle of the tibial tunnel in the coronal plane and loss of flexion and anterior laxity after anterior cruciate ligament reconstruction. Am J Sports Med 29(5):567–574
Jansson KA, Linko E, Sandelin J, Harilainen A (2003) A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med 31(1):12–18
Jarvela T, Kannus P, Jarvinen M (2000) Anterior knee pain 7 years after an anterior cruciate ligament reconstruction with a bone patellar tendon bone autograft. Scand J Med Sci Sports 10(4):221–227
Kartus J, Magnusson L, Stener S et al (1999) Complications following arthroscopic anterior cruciate ligament reconstruction. A 2–5 year follow up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatolol Arthrosc 7(1):2–8
Kartus J, Ejerhed L, Sernert N, Brandsson S, Karlsson J (2000) Comparison of traditional and subcutaneous patellar tendon harvest. A prospective study of donor site-related problems after anterior cruciate ligament reconstruction using different graft harvesting techniques. Am J Sports Med 28(3):328–335
Lavagnino M, Arnoczky SP, Tian T, Vaupel Z (2003) Effect of amplitude and frequency of cyclic tensile strain on the inhibition of MMP-1 mRNA expression in tendon cells: an in vitro study. Connect Tissue Res 44(3–4):181–187
Lerat JL, Chotel F, Besse JL et al (1998) Les résultats après 10 à 16 ans du traitement de la laxité chronique antérieure du genou par une reconstruction du ligament croisé antérieur avec une greffe de tendon rotulien associée à une plastie extra-articulaire externe. A propos de 138 cas. Rev Chir Orthop Reparatrice Appar Mot 84(8):712–727
L’ Insalata JC, Klatt B, Fu FH, Harner CD (1997) Tunnel expansion following anterior cruciate ligament reconstruction: a comparison of hamstring and patellar tendon autografts. Knee Surg Sports Traumatol Arthrosc 5(4):234–238
Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, Petitto A (1998) Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc 6(2):68–75
Marcacci M, Zaffagnini S, Iacono F, Vascellari A, Loreti I, Kon E, Lo Presti M (2003) Intra- and extra-articular anterior cruciate ligament reconstruction utilizing autogeneous semitendinosus and gracilis tendons: 5-year clinical results. Knee Surg Sports Traumatol Arthrosc 11(1):2–8
Marder RA, Raskind JR, Carroll M (1991) Prospective evaluation of arthroscopically assisted anterior cruciate ligament reconstruction. Patellar tendon versus semitendinosus and gracilis tendons. Am J Sports Med 19(5):478–484
Noyes FR, Barber SD (1991) The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am 73(6):882–892
O’Neill DB (1996) Arthroscopically assisted reconstruction of the anterior cruciate ligament. A prospective randomized analysis of three techniques. J Bone Joint Surg Am 78(6):803–813
Otero AL, Hutcheson L (1993) A comparison of the doubled semitendinosus/gracilis and central third of the patellar tendon autografts in arthroscopic anterior cruciate ligament reconstruction. Arthroscopy 9(2):143–148
Peyrache MD, Djian P, Christel P, Witvoet J (1996) Tibial tunnel enlargement after reconstruction by autogenous bone-patellar tendon-bone graft. Knee Surg Sports Traumatol Arthrosc 4(1):2–8
Pinczewski LA, Deehan D, Salmon LJ, Russell VJ, Clingeleffer A (2002) A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 30(4):523–536. Erratum in: Am J Sports Med 2005 Jun;33(6):927
Rosenberg TD, Paulos LE, Parker RD, Coward DB, Scott SM (1988) The forty-five degree posteroanterior flexion weight bearing radiograph of the knee. J Bone Joint Surg Am 70(10):1479–1483
Roth JH, Kennedy JC, Lockstadt H et al (1987) Intra-articular reconstruction of the anterior cruciate ligament with and without extra-articular supplementation by transfer of the biceps femoris tendon. J Bone Joint Surg 69(2):275–278
Sgaglione NA, Del Pizzo W, Fox JM et al (1992) Arthroscopic-assisted anterior cruciate ligament reconstruction with the semitendinous tendon: comparison of results with and without braided polypropylene augmentation. Arthroscopy 8(1):65–77
Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB (2002) A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med 30(2):214–220
Shelbourne KD, Klootwyk TE et al (1995) Ligament stability two to six years after anterior cruciate ligament reconstruction with autogenous patellar tendon graft and participation in accelerated rehabilitation program. Am J Sports Med 23(5):575–579
Shelbourne KD, Trumper RV (1997) Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med 25(1):41–47
Simonian PT, Mann FA, Mandt PR (1995) Indirect forces and patella fracture after anterior cruciate ligament reconstruction with the patellar ligament. Case report. Am J Knee Surg 8(2):60–65
Spindler KP, Kuhn JE, Freedman KB et al (2004) Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med 32(8):1986–1995
Strum GM, Fox JM, Ferkel RD et al (1989) Intraarticular versus intraarticular and extraarticular reconstruction for chronic anterior cruciate ligament instability. Clin Orthop 245:188–198
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Zaffagnini S, Golano P, Farinas O, Depasquale V, Strocchi R, Cortecchia S, Marcacci M, Visani A (2003) Vascularity and neuroreceptors of the pes anserinus: anatomic study. Clin Anat 16(1):19–24
Zaricznyj B (1987) Reconstruction of the anterior cruciate ligament of the knee using a doubled tendon graft. Clin Orthop 220:162–175
Acknowledgment
We are grateful to Dr. Daniele Di Motta, Mr. Simone Bignozzi and Mr. Gianpaolo Bernagozzi for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaffagnini, S., Marcacci, M., Lo Presti, M. et al. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc 14, 1060–1069 (2006). https://doi.org/10.1007/s00167-006-0130-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0130-x