Abstract
Background
Patients undergoing operative treatment of tibial shaft fractures have considerable pain largely managed with opioids. Regional anesthesia (RA) has been increasingly used to reduce perioperative opioid use.
Methods
This was a retrospective study of 426 patients that underwent operative treatment of tibial shaft fractures with and without RA. Inpatient opioid consumption and 90-day outpatient opioid demand were measured.
Results
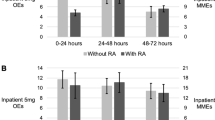
RA significantly decreased inpatient opioid consumption for 48 h post-operatively (p = 0.008). Neither inpatient use after 48 h nor outpatient opioid demand differed in patients with RA (p > 0.05).
Conclusions
RA may help with inpatient pain control and reduce opioid use in tibial shaft fracture.
Level of evidence
Level III, retrospective, therapeutic cohort study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The opioid epidemic is a major public health crisis, with multiple efforts nationwide to reduce opioid prescriptions and use [1, 2]. Prescription opioids are the leading cause of drug overdose deaths in the USA, and many patients are first exposed to opioids in the perioperative period [3]. Orthopedic surgeries are reported as extremely painful by patients, particularly when injury of the lower extremity is involved, and orthopedic surgeons are among the top prescribers of opioids nationwide [4,5,6]. Within orthopedic injuries and surgeries, tibial shaft fracture and surgical repair is particularly painful. These injuries often require a period of external fixation with increases opioid demand perioperatively [6], and 47.4% of patients suffer from anterior knee pain following tibial nailing [7]. The risk of nonunion is high and is associated with an increased likelihood of being prescribed long-term opioid therapy [8].
Notably, opioid demand in the acute perioperative period is a predictor of long-term use and abuse [9], and various factors such as mental health and substance use impact perioperative opioid demand [10,11,12]. Pursuit of opioid-sparing pain management has received increased attention in orthopedic trauma, as this patient population is significantly more likely to use prescription opioids prior to injury, which in turn predicts post-operative opioid use and seeking narcotic prescriptions from multiple providers [13]. To this end, multimodal pain regimens are often used perioperatively.
Regional anesthesia (RA) has been increasingly incorporated into multimodal post-operative analgesia regimens, with some techniques demonstrating reductions in early perioperative opioid consumption and opioid-related side effects [14]. RA encompasses peripheral nerve blocks and paravertebral blocks and provides dynamic pain control targeted to the site of injury, an advantage over global anesthetics [15]. RA has shown promise in its ability to reduce acute pain in the early post-operative period following orthopedic surgery [16]. However, rebound pain—an acute increase in pain upon resolution of nerve blockade—has also been described as a potential detractor from to the overall clinical benefits of RA [17]. The long-term effects of RA on persistent post-operative pain and opioid demand have been understudied and are not yet clearly demonstrated [18].
While the impact of RA on pain and opioid consumption in orthopedic surgery has received growing attention in ankle, hip and distal radius fractures, less is known of its outcomes in tibial shaft fractures. These are particularly important injuries to consider, as the tibia is the most commonly fractured long bone and several factors may predispose these patients to increased opioid use [19]. It is critical to understand the impact regional anesthesia can have on longitudinal opioid demand in tibial shaft fractures; however, there is very limited evidence at present. The purpose of this study is to evaluate the impact of regional anesthesia modalities on inpatient opioid consumption and outpatient opioid demand in patients undergoing tibial shaft fracture surgery. The study hypothesis is that RA will be associated with a decrease in inpatient opioid consumption but will not have an impact on outpatient opioid demand.
Methods
Study design
The Institutional Review Board at our institution approved this retrospective, observational study of inpatient opioid consumption and outpatient opioid demand in all patients aged 18 years and older that underwent tibial shaft fracture surgery at a single institution from 7/1/2013 to 7/1/2018. This study is designed and reported in accordance with the STROBE statement on reporting observational studies [20].
Variables and data sources
Post-operative inpatient opioid consumption (0–24 h, 24–48 h, and 48–72 h post-operative) and outpatient opioid prescribing (discharge to 2-weeks, 6-weeks, and 90-days) in patients undergoing tibial shaft fracture surgery between 7/2013 and 7/2018 at a single, Level I trauma center (Current Procedural Terminology codes 27,758 or 27,759) that were ages 18 and older was recorded [21]. Opioids were converted to oxycodone 5-mg equivalents using conversion factors available through the CDC. Baseline and treatment characteristics including RA usage, age, sex, race, body mass index (BMI), smoking status, American Society of Anesthesiologists (ASA) score, injury mechanism, additional injuries, open fracture, pre-operative opioid prescribing within 6-months to 1-month pre-operative, and additional surgery were recorded through chart review. The definition of pre-operative opioid use was in line with the definition recommended by the Centers for Disease Control (CDC) [22]. General 90-day post-operative complications were also recorded through chart review including mortality, surgical site infection, acute compartment syndrome (ACS), loss of fixation, deep vein thrombosis (DVT), pulmonary embolism (PE), falls, delirium, and ileus. All patients had q4h compartment checks carried out for 24 h postoperatively.
Pain protocol
Although pain management is not rigidly standardized, patients at our institution generally receive multimodal analgesia with oral opioids based on a 10-point pain scale and intravenous (IV) opioids provided for breakthrough pain. Patients routinely receive oral acetaminophen, but non-steroidal anti-inflammatory medications are not routinely used. The decision for including RA in the patient’s perioperative pain regimen is made on a case-by-case basis by the surgeon and treating anesthesiologist. In general, patients are less likely to receive a block if they sustained a high-energy mechanism of injury, underwent surgery within 2 days of initial injury, or sustained an open fracture, due to concern for these patients to be at increased risk of ACS. Sciatic-popliteal, femoral, and/or adductor canal single-shot or continuous blocks are the most commonly used block location, though single-shot and continuous epidural are sometimes used as well. At time of discharge, most patients (390 of 426, 91.5%) received opioid prescriptions.
Missing data
For 7 of 433 (1.6%) patients, BMI could not be evaluated from the available data. Unadjusted analysis was found to be similar with and without them. These patients were excluded after unadjusted analyses to allow adjusted analyses to account for BMI. This left 426 patients for adjusted analysis.
Statistical analysis
Both unadjusted and adjusted statistical analyses were performed. Proportions with percentages and medians with quartiles were calculated. Fisher’s exact test and Wilcoxon rank-sum were used to compare baseline characteristics and outcomes between patients with and without RA. Histograms of outcomes (opioid demand) were created and demonstrated positive skew, as would be expected with data that mirrors count data. Patients within the top 2% of 90-day opioid demand were excluded due to their outlier status. Generalized linear modeling with log link function and negative binomial distribution was planned. Since treatment was not randomly assigned, propensity score weighting was carried out on RA versus no RA, and this analysis included age, sex, race, BMI, smoking, pre-op opioid usage, ASA score (binarized to 1 to 2 vs. 3 or more), injury energy (binarized to high vs low energy), presence of additional injuries, open injury, and additional surgery within 7-days post-fracture surgery as model covariates. Propensity score weighting is a method that closely matches patients based on similarities on covariates provided to the model and allows direct comparison between two groups with non-equal covariates [23].
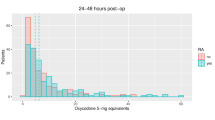
Adjusted analyses using generalized linear modeling incorporated the propensity score weighting and the baseline and treatment factors mentioned above, creating “doubly robust” analyses [24, 25]. Incident rate ratios from adjusted analyses were displayed, and RA versus no RA was simulated through the cohort to create effect estimates, which were derived from medians and 95% confidence intervals. Histograms were also used to display these treatment simulations. R and R Studio (R: A Language and Environment for Statistical Computing, R Core Team, R Foundation for Statistical Computing, Vienna, Austria, 2020) were used for statistical calculations. P-values less than 0.05 were considered significant.
Results
Demographics
Patients without RA tended to be younger, male, non-Caucasian, and had higher rates of smoking, high-energy mechanisms, additional injuries, and open fractures (Table 1). There was no difference between groups in BMI, pre-operative opioid usage, ASA scores, or additional surgeries within either 7 or 90 days. Sciatic-popliteal (65%, 76 of 117), adductor canal (44.4%, 52 of 117), and femoral (17.9%, 21 of 117) nerve blocks were most common forms of RA. Six patients received more than one RA block. Single shot (44.4%, 52 of 117) and continuous (31.6%, 37 of 117) nerve blocks were the most common nerve block routes. Single shot (12.8% 15 of 117) and continuous (6.8%, 8 of 117) epidural analgesia were utilized less frequently than peripheral nerve block. A single patient received a combination of epidural anesthesia and RA.
Inpatient opioid use
After adjustment for baseline patient and treatment factors, RA was associated with significant decreases in opioid consumption from 0–24 to 24–48 h post-operatively (Table 2 and Fig. 1) of approximately 3.7 and 3.0 oxycodone 5-mg equivalents (OE’s), respectively. However, RA had no significant impact on outpatient opioid demand (Table 3 and Fig. 2). RA was also not associated with significant changes in outpatient opioid fills and refills (Table 4).
Outpatient opioid use
As shown in Table 5, general 90-day outcomes did not differ significantly between groups. Rates of acute compartment syndrome (ACS) did not differ significantly between groups.
Independent predictors of opioid use
Appendix Tables 6, 7 and 8 display complete results of multivariable modeling. For inpatient opioid consumption, adjusted models demonstrated significant decreases with increased age and RA but significant increases with female sex, Caucasian race, increased BMI, smoking, increased ASA, high energy mechanism, open fracture, and additional surgery (Appendix Table 6). For outpatient opioid prescribing, adjusted models demonstrated significant decreases with increased age and increased ASA but significant increases with Caucasian race, increased BMI, smoking, pre-operative opioid usage, high energy mechanism, additional injury, and open fracture (Appendix Table 7). Likelihood of outpatient opioid prescription filling or refilling was significantly decreased with increased age (discharge to 2-week timeframe), while it was significantly increased with female sex, Caucasian race, increased BMI, smoking, pre-operative opioid usage, high energy mechanism, additional injuries, open fractures, additional surgery, increased age (6-week to 90-day timeframe). Unadjusted results for inpatient opioid consumption and outpatient opioid demand are shown in Appendix Tables 9, 10, 11.
Discussion
We here found use of RA following tibial shaft fracture and surgical repair significant decreases inpatient opioid consumption in the acute perioperative period but does not change outpatient opioid demand. Age, sex, race, BMI, smoking, pre-operative opioid usage, ASA, injury mechanism, additional injuries, open fracture, and additional surgery were independent significant drivers of inpatient and/or outpatient opioid demand metrics.
Our results show that RA was associated with decreased inpatient opioid consumption from 0 to 48 h after surgical management of tibial shaft fracture. This is likely indicative of superior pain control in patients with RA in the initial post-operative period, as has been demonstrated in prior research. Elkassabany et al. found that peripheral nerve blocks in patients with tibia fractures significantly decreased both pain and frequency of patient-controlled analgesia use up to 24 h post-operatively [26]. They did not report on overall amount of analgesia used. Low pain scores up to 40 h post-operatively have also been documented in a case report of a patient receiving RA after tibial nailing [27]. However, to our knowledge, no previous studies have quantified the impact of RA on post-operative opioid use in tibial shaft fractures.
While information on the effects of RA on opioid consumption in tibial fractures is scarce, our results are consistent with studies of RA in other lower extremity fractures. Christensen et al. found that regional anesthesia modalities significantly reduced 24 h post-operative opioid consumption compared to general anesthesia alone in ankle fracture patients [28]. In patients with talar and calcaneal fractures, continuous peripheral nerve block has been associated with a 30-fold decrease in opioid consumption on the first post-operative day compared to patient-controlled analgesia [29]. The current study agrees with prior research showing that RA is an effective acute analgesic for lower extremity fractures. However, this is the first study of its kind examining tibial shaft fractures. There may be location-specific differences in the effects of RA due to differences in fracture fixation methods, post-operative weight-bearing status, mechanism of injury and damage to surrounding structures, among others. The results from our large sample size add important new evidence of the impact of RA on immediate post-operative opioid demand in tibial shaft fractures.
In considering the potential analgesic and opioid sparing benefits of RA, it is important to account for rebound pain upon discontinuation of nerve blockade. The etiology of rebound pain remains to be fully elucidated, but is believed to be due to an unmasking of nociceptive input from the site of injury as the effects of RA diminish [30]. While duration of RA varies by block type, rebound pain in ankle fractures has been reported 12–24 h after administration and last for 3–6 h [31]. Further, meta-analysis of single-shot interscalene block for shoulder surgeries found an initial opioid-sparing effect up to 12 h, but greater pain 16–24 h post-operatively [32]. Rebound pain has been associated with high levels of opioid use, which may undermine the early clinical benefits of RA [33]. We were able to isolate these time frames of rebound pain by evaluating opioid consumption in 24-h blocks for up to 72 h postoperatively. RA did not lead to increased opioid consumption in the 24–48-h or 48–72-h blocks. This may be due to attenuation of rebound pain by pre-operative nerve blockade, continuous nerve catheter infusions, adjuvant medications or pre-emptive analgesia as previously described [34]. Scheduled acetaminophen is used in post-operative pain management at our institution, and it is possible this afforded pre-emptive analgesia before the blocks resolved. Additionally, RA protocols could not be standardized in this retrospective study and patients received a mix of single-shot and continuous blocks via either epidural or peripheral routes. Patients with continuous blocks may have experienced prolonged duration of analgesia and suppression of rebound pain, masking some patients with increased opioid use in the RA group.
This study found no significant difference in outpatient opioid demand in patients with and without RA. Despite evidence that acute pain and opioid demand predict long-term pain and opioid use [35], our findings are consistent with several previous studies that suggest RA may not confer a long-term reduction in opioid use. In a large database study of patients undergoing abdominal surgery, Ladha et al. found that epidural analgesia was not protective against total 90-day opioid use [36]. Similar results have been reported in a large healthcare claims database study in orthopedic surgery. Mueller et al. determined perioperative nerve blockade was not associated with a reduced risk of persistent opioid use for patients undergoing shoulder arthroplasty [37]. To our knowledge, this is the first study to examine opioid consumption up to 12 weeks in patients with tibial shaft fractures. It is likely that while RA optimized early pain control, there was no significant lasting difference in levels of persistent pain between groups, and therefore, no difference in long-term opioid consumption. While chronic pain is common after tibial shaft fracture, we were unable to measure pain scores and compare differences between groups in this retrospective study. There is a need for high-powered, prospective, randomized studies to clarify the impact of RA on long-term opioid use following discharge after fracture fixation.
With little impact of RA on opioid use following discharge, it is important to acknowledge additional potential disadvantages to this form of analgesia. Nerve blockade prolongs perioperative time, incurs additional cost, and is an additional procedure with added risks for the patient. Furthermore, use of RA remains controversial in the setting of long bone fractures due to concern it may mask symptoms of acute compartment syndrome (ACS) [34]. While rates of all complications occurrence including ACS were similar between groups, diaphyseal fractures are a key risk factor for the development of ACS. A common clinical concern is that RA will delay diagnosis of ACS in tibial shaft fractures, as tibial shaft fractures are responsible for one-third of ACS cases [38]. A recent systematic review found the effect of RA on delayed diagnosis of ACS in tibial shaft fractures was limited to case reports, with limited evidence that the use of RA resulted in a clinically significant delay in ACS diagnoses [39]. In fact, studies in pediatrics have demonstrated no delay in ACS diagnoses in lower extremity fractures when nerve blocks were used [40]. One notable case report discusses a patient that received RA for surgical fixation of a tibial shaft fracture and went on to develop ACS. However, this was diagnosed quickly and resulted in no lasting neuromuscular damage [41]. There is growing evidence that RA may not mask ischemic pain, the hallmark of ACS, to the same degree as non-ischemic pain, although this too is limited to case reports [42, 43]. Despite the lack of clear evidence that RA may delay diagnoses of ACS, there is still significant concern within orthopedics that a peripheral nerve block may potentially mask early clinical signs of ACS. The hesitancy to utilize these blocks in many practices, and the subsequent paucity of evidence on this topic, present further challenges to surgeons in assessing the risks and benefits of RA in tibial shaft fractures.
There are a variety of options for RA in extremity fractures. The present study demonstrated the tendency toward either a single shot in the pre-operative area, designed to both reduce perioperative opioid use and provide postoperative analgesia, as well as use of an indwelling catheter for extended postoperative pain management. We were underpowered to evaluate differences between these groups. Prior research has shown that single shot blocks administered immediately pre-operatively reduced pain scores for at least 24 h after administration within tibial shaft and ankle fractures [26], and reduced opioid use for 24 h post-operatively [28]. Interestingly, indwelling catheters only reduced opioid use for 1 day post-operatively when compared with opioid patient-controlled analgesia (PCA), even when catheters remained in place for longer than 1 day [29]. This may suggest that a single shot block confers the same benefit to an indwelling catheter for postoperative analgesia. As single shot blocks are easier and cheaper to perform, future studies should closely evaluate differences between these forms of regional anesthesia.
There are several limitations to this study given its retrospective nature. First, the proportion of patients who experienced a high-energy injury mechanism and/or had multiple injuries was significantly higher in the non-RA group. This as expected as these patients are at higher risk for ACS and thus, less likely to be offered a block by anesthesia. We were able to control for this difference between groups by utilizing both a propensity score, and further including this score into a generalized linear model. These are well-established statistical methods to control for non-equal covariates between groups, and the difference in inpatient opioid consumption between RA and non-RA groups was significant in both these analyses. Second, adjunctive non-opioid perioperative analgesia was not evaluated as this was not standardized, and many non-opioid medications are provided PRN. Third, as this was a retrospective study, we were unable to evaluate pain scores. Despite this limitation, a prior prospective trial had not demonstrated consistent pain reductions with nerve blockade after 24 h, and it is unlikely that we would have discovered more significant differential pain reductions given our findings regarding opioid usage in this study [28]. Further, opioid prescribing rather than opioid consumption was measured in the outpatient setting. This was the most accurate, objective way to determine opioid use in the outpatient setting, as clinic notes regarding opioid use were inconsistent and patient reporting on opioid use is unreliable [44]. Lastly, our data included patients that received RA at a variety of anatomic locations and with varying medication type, rate, and quantity. This heterogeneity may decrease the specificity of our results to a single technique.
In conclusion, perioperative RA in tibial shaft fracture surgery was associated with reduced inpatient opioid consumption, but no significant change in outpatient opioid demand without notable increases in rates of perioperative complications. Regional anesthesia seems appropriate to utilize to reduce perioperative opioid demand in tibial shaft fracture surgery, but its role in outpatient opioid prescribing seems limited. Further research is needed to evaluate the mediating effect of pain scores and the role of continuous vs single-shot blocks on perioperative pain.
References
Hsu JR, Mir H, Wally MK, Seymour RB, Orthopaedic Trauma Association Musculoskeletal Pain Task F (2019) Clinical practice guidelines for pain management in acute musculoskeletal injury. J Orthop Trauma 33(5):e158–e182. https://doi.org/10.1097/BOT.0000000000001430
Opioid prescription limits and policies by state. (2020). https://ballotpedia.org/Opioid_prescription_limits_and_policies_by_state. Accessed 25 May 2020
Hedegaard H, Warner M, Minino AM (2017) Drug Overdose Deaths in the United States, 1999–2016. NCHS Data Brief 294:1–8
Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SR (2011) Characteristics of opioid prescriptions in 2009. JAMA 305(13):1299–1301. https://doi.org/10.1001/jama.2011.401
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W (2013) Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 118(4):934–944. https://doi.org/10.1097/ALN.0b013e31828866b3
Cunningham D, LaRose M, Yoon RS, Gage MJ (2020) Factors associated with perioperative opioid demand in lower extremity fractures: Does consumption vary by anatomic location? Injury. https://doi.org/10.1016/j.injury.2020.10.038
Katsoulis E, Court-Brown C, Giannoudis PV (2006) Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg Br 88(5):576–580. https://doi.org/10.1302/0301-620X.88B5.16875
Tay WH, de Steiger R, Richardson M, Gruen R, Balogh ZJ (2014) Health outcomes of delayed union and nonunion of femoral and tibial shaft fractures. Injury 45(10):1653–1658. https://doi.org/10.1016/j.injury.2014.06.025
Rosenbloom BN, McCartney CJL, Canzian S, Kreder HJ, Katz J (2017) Predictors of prescription opioid use 4 months after traumatic musculoskeletal injury and corrective surgery: a prospective study. J Pain 18(8):956–963. https://doi.org/10.1016/j.jpain.2017.03.006
Cunningham DJ, LaRose MA, Klifto CS, Gage MJ (2020) Mental health and substance use affect perioperative opioid demand in upper extremity trauma surgery. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2020.06.024
Cunningham D, LaRose M, Gage M (2020) The impact of substance use and abuse on opioid demand in lower extremity fracture surgery. J Orthop Trauma. https://doi.org/10.1097/BOT.0000000000001958
Cunningham DJ, LaRose MA, Gage MJ (2020) The impact of mental health and substance use on opioid demand after hip fracture surgery. J Am Acad Orthop Surg. https://doi.org/10.5435/JAAOS-D-20-00146
Morris BJ, Zumsteg JW, Archer KR, Cash B, Mir HR (2014) Narcotic use and postoperative doctor shopping in the orthopaedic trauma population. J Bone Joint Surg Am 96(15):1257–1262. https://doi.org/10.2106/JBJS.M.01114
Richman JM, Liu SS, Courpas G, Wong R, Rowlingson AJ, McGready J, Cohen SR, Wu CL (2006) Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis Anesth Analg 102(1):248–257. https://doi.org/10.1213/01.ANE.0000181289.09675.7D
Guay J, Parker MJ, Griffiths R, Kopp S (2017) Peripheral nerve blocks for hip fractures. Cochrane Datab Syst Rev 5(5):CD001159. https://doi.org/10.1002/14651858.CD001159.pub2
Chan EY, Fransen M, Parker DA, Assam PN, Chua N (2014) Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Datab Syst Rev 5:41. https://doi.org/10.1002/14651858.CD009941.pub2
Dada O, Gonzalez Zacarias A, Ongaigui C, Echeverria-Villalobos M, Kushelev M, Bergese SD, Moran K (2019) Does Rebound Pain after Peripheral Nerve Block for Orthopedic Surgery Impact Postoperative Analgesia and Opioid Consumption? Int J Environ Res Public Health Narrat Rev. https://doi.org/10.3390/ijerph16183257
Weinstein EJ, Levene JL, Cohen MS, Andreae DA, Chao JY, Johnson M, Hall CB, Andreae MH (2018) Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children. Cochrane Database Syst Rev 6(6):CD007105. https://doi.org/10.1002/14651858.CD007105.pub4
Miller NC, Askew AE (2007) Tibia fractures. An overview of evaluation and treatment. Orthop Nurs 26(4):216–223. https://doi.org/10.1097/01.NOR.0000284648.52968.27
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
National Center for Injury Prevention and Control CfDCaP (2018) CDC compilation of benzodiazepines, muscle relaxants, stimulants, zolpidem, and opioid analgesics with oral morphine milligram equivalent conversion factors.
Prevention. CfDCa (2016) definitions relevant to the clinical qi opioid measures. https://www.cdc.gov/drugoverdose/pdf/prescribing/CDC-DUIP-FactSheet-At-A-Glance_Opioid-Measures-508.pdf. Accessed 28 May 2020
Li F, Morgan KL, Zaslavsky AM (2018) Balancing covariates via propensity score weighting. J Am Stat Assoc 113(521):390–400
Glynn AN, Quinn KM (2010) An introduction to the augmented inverse propensity weighted estimator. Polit Anal 18:36–56. https://doi.org/10.1093/pan/mpp036
Antonio Olmos PG (2015) A practical guide for using propensity score weighting in R. Pract Assess Res Eval 20(1):13
Elkassabany N, Cai LF, Mehta S, Ahn J, Pieczynski L, Polomano RC, Picon S, Hogg R, Liu J (2015) Does regional anesthesia improve the quality of postoperative pain management and the quality of recovery in patients undergoing operative repair of tibia and ankle fractures? J Orthop Trauma 29(9):404–409. https://doi.org/10.1097/BOT.0000000000000344
Imbelloni LE, Rava C, Gouveia MA (2013) A new, lateral, continuous, combined, femoral-sciatic nerve approach via a single skin puncture for postoperative analgesia in intramedullary tibial nail insertion. Local Reg Anesth 6:9–12. https://doi.org/10.2147/LRA.S37261
Christensen KP, Moller AM, Nielsen JK, Klausen TW, Sort R (2016) The effects of anesthetic technique on postoperative opioid consumption in Ankle fracture surgery. Clin J Pain 32(10):870–874. https://doi.org/10.1097/AJP.0000000000000335
Luiten WE, Schepers T, Luitse JS, Goslings JC, Hermanides J, Stevens MF, Hollmann MW, van Samkar G (2014) Comparison of continuous nerve block versus patient-controlled analgesia for postoperative pain and outcome after talar and calcaneal fractures. Foot Ankle Int 35(11):1116–1121. https://doi.org/10.1177/1071100714546640
Munoz-Leyva F, Cubillos J, Chin KJ (2020) Managing rebound pain after regional anesthesia. Korean J Anesthesiol 73(5):372–383. https://doi.org/10.4097/kja.20436
Goldstein RY, Montero N, Jain SK, Egol KA, Tejwani NC (2012) Efficacy of popliteal block in postoperative pain control after ankle fracture fixation: a prospective randomized study. J Orthop Trauma 26(10):557–561. https://doi.org/10.1097/BOT.0b013e3182638b25
Abdallah F, Halpern S, Aoyama K, Brull R (2015) Will the real benefits of single-shot interscalene block please stand up? A systematic review and meta-analysis. Anesth Analg. https://doi.org/10.1213/ANE.0000000000000688
Henningsen MJ, Sort R, Moller AM, Herling SF (2018) Peripheral nerve block in ankle fracture surgery: a qualitative study of patients’ experiences. Anaesthesia 73(1):49–58. https://doi.org/10.1111/anae.14088
Gadsden J, Warlick A (2015) Regional anesthesia for the trauma patient: improving patient outcomes. Local Reg Anesth. https://doi.org/10.2147/LRA.S55322
Hsia HL, Takemoto S, van de Ven T, Pyati S, Buchheit T, Ray N, Wellman S, Kuo A, Wallace A, Raghunathan K (2018) Acute pain is associated with chronic opioid use after total knee arthroplasty. Reg Anesth Pain Med 43(7):705–711. https://doi.org/10.1097/AAP.0000000000000831
Ladha KS, Patorno E, Liu J, Bateman BT (2016) Impact of perioperative epidural placement on postdischarge opioid use in patients undergoing abdominal surgery. Anesthesiology 124(2):396–403. https://doi.org/10.1097/ALN.0000000000000952
Mueller KG, Memtsoudis SG, Mariano ER, Baker LC, Mackey S, Sun EC (2017) Lack of association between the use of nerve blockade and the risk of persistent opioid use among patients undergoing shoulder arthroplasty: evidence from the marketscan database. Anesth Analg 125(3):1014–1020. https://doi.org/10.1213/ANE.0000000000002031
Duckworth AD, McQueen MM (2017) The diagnosis of acute compartment syndrome: a critical analysis review. JBJS Rev 5(12):e1. https://doi.org/10.2106/JBJS.RVW.17.00016
Tran AA, Lee D, Fassihi SC, Smith E, Lee R, Siram G (2020) A systematic review of the effect of regional anesthesia on diagnosis and management of acute compartment syndrome in long bone fractures. Eur J Trauma Emerg Surg 46(6):1281–1290. https://doi.org/10.1007/s00068-020-01320-5
Brovman EY, Wallace FC, Weaver MJ, Beutler SS, Urman RD (2019) Anesthesia type is not associated with postoperative complications in the care of patients with lower extremity traumatic fractures. Anesth Analg 129(4):1034–1042
Munk-Andersen H, Laustrup T (2013) Compartment syndrome diagnosed in due time by breakthrough pain despite continuous peripheral nerve block. Acta Anaesthesiol Scand 57(10):1328–1330
Camelo CR, Eklund SE, Brusseau R, Gomez-Morad AD (2020) Ischemic pain not masked by regional anesthesia. Reg Anesth Pain Med 45(3):244–245
Kucera TJ, Boezaart AP (2014) Regional anesthesia does not consistently block ischemic pain: two further cases and a review of the literature. Pain Med 15(2):316–319
Ahn J, Bohl DD, Tabaraee E, Aboushaala K, Elboghdady IM, Singh K (2016) Preoperative narcotic utilization: accuracy of patient self-reporting and its association with postoperative narcotic consumption. J Neurosurg Spine 24(1):206–214
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Gage has no relevant conflicts of interest but reports the following: AO: research support, Arthrex, Inc: paid consultant; Research support Elsevier: publishing royalties, financial or material support Foundation for Orthopaedic Trauma: research support TrackX: paid consultant. Otherwise, none of the other authors have any conflicts of interest.
Ethical approval
This study was approved by the institutional review board.
Informed consent
Informed consent was not applicable for this retrospective review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Tables
6,
7,
8,
9,
10 and
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cunningham, D., LaRose, M., Patel, P. et al. Regional anesthesia improves inpatient but not outpatient opioid demand in tibial shaft fracture surgery. Eur J Orthop Surg Traumatol 33, 2921–2931 (2023). https://doi.org/10.1007/s00590-023-03504-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03504-2