Abstract
Purpose
Regional anesthesia (RA) is used for pain control, but its impacts on the orthopedic trauma population are not well known. This study evaluated the impact of peripheral nerve blocks after distal tibia and ankle fracture repair on opioid use and pain scores and quantified the magnitude and duration of any changes.
Methods
This retrospective cohort study included patients treated operatively for distal tibia and ankle fractures over a 5-year period, both with and without peripheral nerve blocks. Total inpatient 5 mg oxycodone equivalents (OEs) used in the post-operative period, from 0–24, 24–48, to 48–72 h and maximum visual analog scale (VAS) pain ratings from 0–24, 24–48, to 48–72 h were recorded.
Results
540 non-polytrauma patients and 183 polytrauma patients were included. Patients in the non-polytrauma group who received nerve blocks required fewer opioids on post-operative day (POD) 1 compared to the non-nerve block group (4.8 [95% CI 4.2–5.4] vs. 10.5 [95% CI: 9.2–11.8]; p < 0.001) and had lower VAS scores on POD1 (5.0 [95% CI 4.6–5.4] vs. 7.7 [95% CI: 7.3–8.1]; p < 0.001). However, there were no differences between these groups on POD2 or POD3 and no differences at any timepoints in the polytrauma group.
Conclusion
Patients with isolated distal tibia and ankle fractures who receive peripheral nerve blocks demonstrate modest reductions in inpatient opioids and pain scores on POD1. However, there are no clear benefits beyond this point. Furthermore, polytrauma patients do not experience any reductions in opioid consumption or pain scores.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sufficient pain control after surgery is an important goal, as inadequately managed pain has been shown to potentially worsen both short- and long-term patient outcomes. Poor pain control has been shown to lengthen hospital stays, delay post-operative ambulation, and worsen long-term function after an assortment of orthopedic procedures [1, 2]. However, orthopedic surgery has been shown to be among the most painful operations, often warranting opioid medications to achieve satisfactory pain control [3,4,5]. Given the deleterious side effects of opioids such as delirium and respiratory depression, as well as rising rates of opioid use disorder, it is worthwhile to examine multimodal pain control techniques [6]. These include non-narcotic medications, neuraxial analgesia, and peripheral nerve blocks, with the goal of augmenting narcotic medications such that adequate pain control is maintained while reducing total opioid consumption [7, 8].
Prior studies have demonstrated reductions in opioid use after total hip arthroplasty and total knee arthroplasty when incorporating regional anesthesia (RA) [9]. Additionally, RA has been shown to reduce opioid demand and pain scores following ankle arthroplasty, arthrodesis, and other elective foot and ankle procedures [10, 11]. However, the literature on RA use in the acute fracture setting is more divided [12,13,14]. Examining distal tibia and ankle fractures specifically, prior studies have demonstrated a reduction in opioid consumption, pain scores, and length of stay in the post-anesthesia care unit (PACU) setting when incorporating RA [15, 16]. There is one study that examines longer-term impacts, demonstrating a reduction in opioid use through post-operative day (POD) 1 when incorporating RA, with no impact to POD2 or POD3 [17]. Pain scores are not reported.
Additionally, RA is not without its own risks. In addition to the risks of any procedure, such as bleeding, infection, or neurovascular damage, there is the concept of rebound pain. In this instance, patients experience hyperalgesia after the analgesic effects of a nerve block subside, with a subsequent increase in total opioid use post-operatively [18]. Additionally, limited case reports exist in the literature documenting instances of missed compartment syndrome, thought to be related to pain masking in the setting of peripheral nerve blocks [19, 20].
Therefore, we sought to better understand the role of RA after distal tibia and ankle fracture repair and to quantify the specific magnitudes and durations of any changes the therapy may provide regarding post-operative opioid use and pain scores. We hypothesized that the use of peripheral nerve blocks would be associated with decreased opioid use in the immediate post-operative period, as well as decreased pain scores in the immediate post-operative period.
Materials and methods
After receiving institutional review board approval, a retrospective cohort study was performed of patients who underwent open reduction and internal fixation of ankle and pilon fractures at a single academic medical center over a 5-year period between July 1, 2013, and June 30, 2018 treated with and without RA. All patients were identified by Current Procedural Terminology (CPT) codes, including 27766, 27769, 27792, 27814, 27822, 27823, 27826, 27827, and 27828. Patients were excluded from the study if they were under the age of 18, or if they were currently using opioids chronically for a prior, unrelated injury at the time of surgery.
Patient demographic and injury data were recorded, including age, sex, race, body mass index (BMI), smoking status, American Society of Anesthesiologists (ASA) score, injury mechanism, open versus closed injury, and additional injuries and/or surgeries. Total inpatient opioid use in the post-operative period, from 0–24, 24–48, to 48–72 h was recorded. Post-operative opioid use was first converted to morphine milligram equivalents (MMEs) using conversion factors from the Centers for Disease Control and Prevention (CDC), then to 5 mg oxycodone equivalents (OEs) [21]. Maximum visual analog scale (VAS) pain ratings were recorded from 0–24, 24–48, to 48–72 h post-operative. All patients were included in POD1 analysis, then excluded from further analysis based on date of discharge relative to surgery.
The decision whether to receive a peripheral nerve block was made at the discretion of the attending anesthesiologist. Nerve block data, including type, location, contents, and amount, were recorded, if applicable. Preliminary data analysis demonstrated that patients were less likely to receive RA if they were polytrauma patients. Because of the expected differences in total opioid requirements and pain levels for polytrauma patients, patients were placed into one of four groups: non-polytrauma receiving RA, non-polytrauma not receiving RA, polytrauma receiving RA, and polytrauma not receiving RA. OEs and VAS ratings were then compared as follows: non-polytrauma receiving RA versus non-polytrauma not receiving RA and polytrauma receiving RA versus polytrauma not receiving RA.
Statistical analysis was performed using IBM SPSS Statistics, version 28.0.1.1 for MacOS (Chicago, IL). Data were evaluated with Fisher’s Exact Test or Student’s t-test where applicable. An alpha value of 0.05 was used to assess for statistical significance.
Results
Seven hundred and twenty-three patients were included in the study population (n = 400 female; 55.3%), with an average age of 47.5 (range 18 to 91) (Table 1). Five hundred and forty patients were included in the non-polytrauma group (n = 390 received a block; 72.2%), whereas 183 patients were included in the polytrauma group (n = 71 received a block; 38.8%). Baseline characteristics of the study populations aligned well. Non-polytrauma patients who received RA were slightly younger (46.9 ± 17.3 vs. 52.2 ± 17.7; p = 0.002) and had slightly lower BMIs (29.1 ± 6.2 vs. 30.7 ± 7.3; p = 0.020), though the clinical significance of these differences is likely insignificant. Additionally, they had a lower rate of open fracture (n = 19 [4.9%] vs. n = 20 [13.3%]; p = 0.001). Similarly, polytrauma patients receiving RA had a lower rate of open fracture (n = 10 [14.1%] vs. n = 38 [33.9%]; p = 0.003), as well as a lower rate of additional surgeries within the 7-day post-operative period (n = 5 [7.0%] vs. n = 24 [21.4%]; p = 0.012). There were no other significant differences between patient groups regarding sex, race, smoking status, ASA grade, or percentage of high-energy injury mechanism, which included motor vehicle accidents, falls from height, and ballistic wounds.
All blocks were single-shot. The most common block locations were to the sciatic and saphenous nerves (n = 373; 80.9%) and to the sciatic nerve alone (n = 69; 15.0%). Most blocks consisted of 0.5% ropivacaine (n = 452; 98.0%).
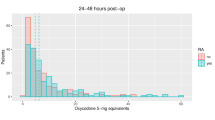
Patients in the non-polytrauma group who received RA required fewer inpatient 5 mg OEs on POD1 compared to the non-RA group (4.8 [95% CI 4.2–5.4] vs. 10.5 [95% CI: 9.2–11.8]; p < 0.001; MME: 7.2 [95% CI 6.3–8.1] vs. 15.8 [95% CI: 13.8–17.7]) (Fig. 1a). There were no differences between these groups on POD2 or POD3. Similarly, maximum VAS pain scores were lower in the group who received RA on POD1 (5.0 [95% CI 4.6–5.4] vs. 7.7 [95% CI: 7.3 – 8.1]; p < 0.001) (Fig. 2a), with no differences between these groups on POD2 or POD3.
a Use of RA was associated with decreased inpatient 5 mg OE use on POD1 in the non-polytrauma group (4.8 [95% CI 4.2 – 5.4] vs. 10.5 [95% CI: 9.2 – 11.8]; p < 0.001; MME: 7.2 [95% CI 6.3 – 8.1] vs. 15.8 [95% CI: 13.8 – 17.7]). There was no effect on POD2 or POD3. b Use of RA had no impact on inpatient 5 mg OE use on POD1, POD2, or POD3 in the polytrauma group. OEs = 5 mg oxycodone equivalents. MMEs = morphine milligram equivalents. RA = regional anesthesia. Error bars represent 95% confidence intervals
a Use of RA was associated with decreased maximum VAS pain scores on POD1 in the non-polytrauma group (5.0 [95% CI 4.6 – 5.4] vs. 7.7 [95% CI: 7.3 – 8.1]; p < 0.001). There was no effect on POD2 or POD3. b Use of RA had no impact on maximum VAS pain scores on POD1, POD2, or POD3 in the polytrauma group. VAS = visual analog scale. RA = regional anesthesia. Error bars represent 95% confidence intervals
Patients in the polytrauma group demonstrated no differences in OEs or VAS pain scores between the RA and non-RA groups at any post-operative time points (Figs. 1b and 2b).
Discussion
Multimodal pain modalities are often used in combination after orthopedic procedures to provide sufficient pain control while reducing post-operative opioid use. Many studies have demonstrated reductions in opioid use following arthroplasty procedures and other elective orthopedic procedures [9,10,11]. However, the literature is more variable and limited when discussing fracture fixation. Given the differences in acuity of injury, mechanism of injury, and extent of soft tissue damage in the trauma setting, it is important to independently analyze these populations. Furthermore, RA is not without its own risks. Therefore, it is worthwhile to quantify the specific impacts to opioid use and pain scores that nerve blocks may provide. We elected to analyze distal tibia and ankle fractures given their high incidence and common use of regional anesthesia.
Our results demonstrate a modest reduction in opioid use and pain scores following distal tibia and ankle fracture surgery only in the non-polytrauma population and only at POD1, with no impact to total opioid consumption or pain scores beyond this time point. These results align well with prior published literature. Cunningham et al. examined distal tibia and ankle fractures and found a reduction in opioid use through POD1, with no impact to POD2 or POD3 [17]. Similarly, Alexander et al. found that preoperative nerve blocks were associated with decreased pain scores, PACU opioid consumption, and PACU length of stay [15]. Christensen et al. reported similar findings [16]. All patients included in our study received single-shot nerve blocks. The observed reductions in opioid consumption through POD1 with no sustained benefit beyond this aligns well with the published 12–24-h duration of action of single-shot peripheral nerve blocks [22].
Additionally, our results expand on the prior literature by including subgroup analyses examining polytraumatized and non-polytraumatized patients independently, with RA demonstrating no reduction to opioid consumption or pain scores in the polytraumatized population. Intuitively, it is understandable that polytraumatized patients may not see the same reductions in total opioid consumption that non-polytraumatized patients experience. Given multiple orthopedic and non-orthopedic injuries, there are likely many drivers of a polytrauma patient’s pain that treatment with RA is unable to address. Therefore, it may not be beneficial to utilize RA in the polytraumatized patient population if the sole goal is opioid reduction. While there may be additional benefits to the use of RA in this group beyond simple reductions in total opioid consumption or pain scores, these benefits are beyond the scope of this study.
There was an increased rate of open fractures in patients who did not receive RA. Given the higher energy typically associated with open fractures and the greater degree of soft tissue damage, it is reasonable to expect higher opioid demands and pain scores in these patients. For this reason, our analysis was performed both with and without open fractures included. There were no differences in results, arguing in favor of true reductions in OE use and VAS values when incorporating RA as opposed to higher baseline measurements in the non-RA population.
Rebound pain is the concept that patients can experience hyperalgesia shortly after the analgesic effects of a peripheral nerve block wear off. This subsequently increases total opioid demand, more than counteracting the early reduction in opioid use that a block may provide [18]. While the pathophysiology of rebound pain is still debated, it is thought to involve both mechanical and chemical irritation from local anesthetics, as well as increased awareness of pain signals [23]. Prior studies have documented the occurrence of rebound pain with peripheral nerve blocks following proximal humerus, pelvic and acetabular, and distal femur fracture repair, and overall rates have been reported to be as high as 40% [13, 14, 24, 25]. However, we did not find conclusive evidence of the rebound pain phenomenon in our results. Both opioid consumption and pain scores were comparable between RA and non-RA groups on POD2 and POD3 in both the polytrauma and non-polytrauma patient groups. Additionally, the differences between pain scores on POD1 and POD2 between RA and non-RA groups were not significantly different. This may be related to patient education regarding rebound pain or the use of scheduled medications such as acetaminophen [18].
It is possible that select patients within our cohort experienced rebound pain, and in fact, 22% of patients treated with RA experienced an increase in maximum VAS pain score between POD1 and POD2 (though 55% experienced a decrease and 23% had no change in maximum VAS pain score). While patients experiencing an increase in pain between POD1 and POD2 were more likely to be older (p = 0.004), there were no differences in sex, smoking status, or BMI. Given the smaller sample size of patients experiencing increases in pain levels, we are unable to draw any firm conclusions regarding risk factors for this occurrence.
There are several limitations to this study. As it was performed at a single academic medical center, our conclusions may not be generalizable to other institutions with differing post-operative pain protocols. However, this is less likely as multiple independent studies have demonstrated early post-operative reductions in opioid use when incorporating regional anesthesia, with waning impacts at later timepoints. Additionally, while the multiple fracture patterns and block types included in our study improve its generalizability, this may mask certain populations that may benefit most from RA as well as which block types may be most effective. Furthermore, an inpatient-only study introduces several biases. In general, these patients may have more severe fracture patterns, may be sicker, may experience more difficulty with pain control, and their access to pain medications is different than in an outpatient setting. We feel that by excluding patients as they are discharged, the accuracy of our data is maintained and any impacts to our results and conclusions are limited. However, this does change our patient population throughout the study period, limiting our ability to comment on day-to-day changes in opioid use. Given this, the conclusions of our manuscript should only be applied to the inpatient treatment of distal tibia and ankle fractures with peripheral nerve blocks, not peripheral nerve blocks in their entirety. Future studies may expand upon these results to the outpatient setting through pain and medication journaling. Finally, peripheral nerve blocks require a trained anesthesiologist and require additional time and financial costs. Our study did not include an assessment of these additional costs in relation to the measured benefits.
Overall, our results demonstrate a modest reduction in opioid use and pain scores when incorporating RA after isolated distal tibia and ankle fractures. However, these benefits are limited to the first post-operative day, with no evidence of sustained reductions. Furthermore, polytrauma patients do not experience these same benefits. Additionally, we found no evidence of rebound pain at any time points. We believe that these findings will help patients and physicians have a better understanding of the degree of opioid use and pain score reductions that RA can provide, as well as the limitations of the procedure. We anticipate that this information will contribute to the shared decision-making process between physicians and patients when discussing the potential benefits and drawbacks of nerve blocks for post-operative pain control after orthopedic trauma.
References
Morrison SR, Magaziner J, McLaughlin MA, Orosz G, Silberzweig SB, Koval KJ, Siu AL (2003) The impact of post-operative pain on outcomes following hip fracture. Pain 103(3):303–311. https://doi.org/10.1016/S0304-3959(02)00458-X
Judkins BL, Hao KA, Wright TW, Jones BK, Boezaart AP, Tighe P, Vasilopoulos T, Horodyski M, King JJ (2022) Early reduction in postoperative pain is associated with improved long-term function after shoulder arthroplasty: a retrospective case series. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-022-03242-x
Chung F, Ritchie E, Su J (1997) Postoperative pain in ambulatory surgery. Anesth Analg 85(4):808–816. https://doi.org/10.1097/00000539-199710000-00017
Ekstein MP, Weinbroum AA (2011) Immediate postoperative pain in orthopedic patients is more intense and requires more analgesia than in post-laparotomy patients. Pain Med 12(2):308–313. https://doi.org/10.1111/j.1526-4637.2010.01026.x
Boddapati V, Padaki AS, Lehman RA, Lenke LG, Levine WN, Riew KD (2021) Opioid prescriptions by orthopaedic surgeons in a medicare population: recent trends, potential complications, and characteristics of high prescribers. J Am Acad Orthop Surg 29(5):e232–e237. https://doi.org/10.5435/JAAOS-D-20-00612
(2021) What is the U.S. Opioid Epidemic? http://www.hhs.gov/opioids/about-the-epidemic/index.html. Accessed 1 October 2022
Sinatra RS, Torres J, Bustos AM (2002) Pain management after major orthopaedic surgery: current strategies and new concepts. J Am Acad Orthop Surg 10(2):117–129. https://doi.org/10.5435/00124635-200203000-00007
Pasero C, McCaffery M (2007) Orthopaedic postoperative pain management. J Perianesth Nurs. 22(3):160–72; quiz 172–3. doi: https://doi.org/10.1016/j.jopan.2007.02.004
Soffin EM, Wu CL (2019) Regional and multimodal analgesia to reduce opioid use after total joint arthroplasty: a narrative review. HSS J 15(1):57–65. https://doi.org/10.1007/s11420-018-9652-2
Chan JJ, Garden E, Chan JC, Poeran J, Zubizarreta N, Mazumdar M, Galatz LM, Vulcano E (2021) Peripheral nerve block use in ankle arthroplasty and ankle arthrodesis: utilization patterns and impact on outcomes. J Anesth 35(6):879–888. https://doi.org/10.1007/s00540-021-02994-w
Gianakos AL, Romanelli F, Rao N, Badri M, Lubberts B, Guss D, DiGiovanni CW (2021) Combination lower extremity nerve blocks and their effect on postoperative pain and opioid consumption: a systematic review. J Foot Ankle Surg 60(1):121–131. https://doi.org/10.1053/j.jfas.2020.08.026
Cunningham DJ, LaRose MA, Zhang GX, Au S, MacAlpine EM, Paniagua AR, Klifto CS, Gage MJ (2022) Regional anesthesia reduces inpatient and outpatient perioperative opioid demand in periarticular elbow surgery. J Shoulder Elbow Surg 31(2):e48–e57. https://doi.org/10.1016/j.jse.2021.08.005
Cunningham DJ, Robinette JP, Paniagua AR, LaRose MA, Blatter M, Gage MJ (2022) Regional anesthesia does not decrease opioid demand in pelvis and acetabulum fracture surgery. Eur J Orthop Surg Traumatol 32(7):1357–1370. https://doi.org/10.1007/s00590-021-03114-w
Cunningham DJ, LaRose MA, Zhang GX, Paniagua AR, Klifto CS, Gage MJ (2021) Beware the rebound effect: regional anesthesia increases opioid utilization after humerus fracture surgery. Shoulder Elbow. https://doi.org/10.1177/17585732211048117
Alexander JC, Sunna M, Minhajuddin A, Liu G, Sanders D, Starr A, Gasanova I, Joshi GP (2020) Comparison of regional anesthesia timing on pain, opioid use, and postanesthesia care unit length of stay in patients undergoing open reduction and internal fixation of ankle fractures. J Foot Ankle Surg 59(4):788–791. https://doi.org/10.1053/j.jfas.2019.05.012
Christensen KP, Møller AM, Nielsen JK, Klausen TW, Sort R (2016) The effects of anesthetic technique on postoperative opioid consumption in ankle fracture surgery. Clin J Pain 32(10):870–874. https://doi.org/10.1097/AJP.0000000000000335
Cunningham DJ, Paniagua A, DeLaura I, Zhang G, Kim B, Kim J, Lee T, LaRose M, Adams S, Gage MJ (2022) Regional anesthesia decreases inpatient but not outpatient opioid demand in ankle and distal tibia fracture surgery. Foot Ankle Spec 19:19386400221088452. https://doi.org/10.1177/19386400221088453
Dada O, Gonzalez Zacarias A, Ongaigui C, Echeverria-Villalobos M, Kushelev M, Bergese SD, Moran K (2019) Does rebound pain after peripheral nerve block for orthopedic surgery impact postoperative analgesia and opioid consumption? A narrative review. Int J Environ Res Public Health 16(18):3257. https://doi.org/10.3390/ijerph16183257
Ganeshan RM, Mamoowala N, Ward M, Sochart D (2015) Acute compartment syndrome risk in fracture fixation with regional blocks. BMJ Case Rep. https://doi.org/10.1136/bcr-2015-210499
Tran AA, Lee D, Fassihi SC, Smith E, Lee R, Siram G (2020) A systematic review of the effect of regional anesthesia on diagnosis and management of acute compartment syndrome in long bone fractures. Eur J Trauma Emerg Surg 46(6):1281–1290. https://doi.org/10.1007/s00068-020-01320-5
National Center for Injury Prevention and Control (2018) CDC compilation of benzodiazepines, muscle relaxants, stimulants, zolpidem, and opioid analgesics with oral morphine milligram equivalent conversion factors. https://www.cdc.gov/drugoverdose/modules/data-files.html. Accessed 1 October 2022
Joshi G, Gandhi K, Shah N, Gadsden J, Corman SL (2016) Peripheral nerve blocks in the management of postoperative pain: challenges and opportunities. J Clin Anesth 35:524–529. https://doi.org/10.1016/j.jclinane.2016.08.041
Sort R, Brorson S, Gögenur I, Nielsen JK, Møller AM (2019) Rebound pain following peripheral nerve block anaesthesia in acute ankle fracture surgery: an exploratory pilot study. Acta Anaesthesiol Scand 63(3):396–402. https://doi.org/10.1111/aas.13290
Lavand’homme P (2018) Rebound pain after regional anesthesia in the ambulatory patient. Curr Opin Anaesthesiol 31(6):679–684. https://doi.org/10.1097/ACO.0000000000000651
Cunningham DJ, Paniaugua AR, LaRose MA, DeLaura IF, Blatter MK, Gage MJ (2022) Regional anesthesia does not decrease inpatient or outpatient opioid demand in distal femur fracture surgery. Arch Orthop Trauma Surg 142(8):1873–1883. https://doi.org/10.1007/s00402-021-03892-2
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MAL, WMN, and SRY. The first draft of the manuscript was written by MAL and SRY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All components of this study met institutional review board approval and comply with the current laws of the United States of America.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lantieri, M.A., Novicoff, W.M. & Yarboro, S.R. Regional anesthesia provides limited decreases in opioid use following distal tibia and ankle fracture surgery. Eur J Orthop Surg Traumatol 33, 2633–2638 (2023). https://doi.org/10.1007/s00590-023-03486-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03486-1