Abstract
Purpose
Ankle arthrodesis and total ankle arthroplasty (TAA) are often associated with significant postoperative pain. While this may be mitigated by the use of peripheral nerve blocks (PNB), large-scale data are lacking. Using national data, we aimed to evaluate PNB utilization pattern and its impact on outcomes.
Methods
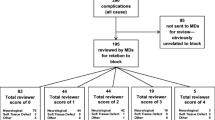
This retrospective cohort study utilized data from the nationwide database (2006–2016) on TAA (n = 5,290) and ankle arthrodesis (n = 14,709) procedures. PNB use was defined from billing; outcomes included opioid utilization, length and cost of stay, discharge to a skilled nurse facility, and opioid-related complications. Mixed-effects models estimated the association between PNB use and outcomes, separate by procedure type and inpatient/outpatient setting. We report odds ratios and 95% confidence intervals (CI).
Results
Overall, PNB was utilized in 8.7% of TAA and 9.9% of ankle arthrodesis procedures, with increased utilization from 2006 to 2016 of 2.6% to 11.3% and 5.2% to 12.0%, respectively. After adjustment for relevant covariates, PNB use was significantly associated with decreased total opioid utilization specifically in the inpatient setting in TAA ( − 16.9% CI − 23.9%; − 9.1%) and ankle arthrodesis procedures ( − 18.9% CI − 24.4; − 13.0%), this was particularly driven by a decrease in opioid utilization on the day of surgery. No clinically relevant effects were observed for other outcomes.
Conclusion
PNB utilization is associated with substantial reductions in opioid utilization, particularly in the inpatient setting. Our study is in support of a wider use of this analgesic technique, which may translate into more benefits in terms of clinical outcomes and resource utilization.
Level of Evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Both ankle arthrodesis and total ankle arthroplasty (TAA) are currently utilized treatments for ankle arthritis, a debilitating condition that leads to diminished quality of life by causing substantial pain and limited ankle function [1,2,3,4,5]. Controlling post-operative pain is crucial for optimal recovery and patient satisfaction [6]. While adequate post-operative pain control is often achieved through various opioid and non-opioid agents, peripheral nerve blocks (PNB) are an increasingly utilized mode of analgesia, particularly continuous popliteal sciatic nerve blocks [7,8,9]. With the increasing shift toward outpatient foot and ankle surgery, avoidance of sedation, opioids, or general anesthesia in the management of immediate post-operative pain has become increasingly important [10].
Various different types of PNB have also been described for foot and ankle procedures and all demonstrated decreased opioid consumption and improved post-operative pain control [10,11,12]. However, the existing literatures on PNB in foot and ankle surgery are single institutional studies with small sample sizes; therefore, generalizability of these data is lacking [13, 14]. Given the potential benefits of PNB, a population-level study is needed. Therefore, the purpose of this study was to examine population-level utilization pattern of PNB and the effect of PNBs on outcomes —specifically, total opioid utilization, length of stay (LOS), hospitalization costs, and complications in patients who underwent TAA or ankle arthrodesis. We hypothesized that there is an increase in PNB utilization over the past decade, and that PNB use is associated with decreased opioid utilization, LOS, and costs while not altering odds of complications.
Materials and methods
Data source, study design, and study sample
The study used data from the Premier Healthcare database (Premier Healthcare Solutions, Inc., Charlotte, NC) [1, 2], a national all-payer database which contains detailed billing information on hospital stays from 20 to 25% of US hospitals. The cohort was defined using the International Classification of Disease, Ninth Revision (ICD-9) procedure codes for TAA (81.11) and ankle arthrodesis (81.56) procedures for the years 2006–2016. Patients were excluded if they met one of the following criteria: unknown gender (n = 256), and unknown discharge status (n = 204), non-elective procedure (n = 3,308). The Mount Sinai Hospital Review Board considers this study exempt from review based on the de-identified HIPAA-compliant nature of the data (project#14–0067).
Study variables
An analysis plan was created a priori where all study variables, including the main effects of interest and outcomes were defined. Our main effect of interest was the use of a PNB, which was extracted from billing data in line with previous studies [3, 4]. Outcomes of interest were total opioid utilization (in oral morphine equivalents (milligrams [mg]); during the full hospital stay), opioid utilization on the day of surgery (‘Day 0’), cost of hospitalization, length of stay, discharge to a skilled nursing facility (SNF), opioid-related complications [5] (combination of respiratory, gastrointestinal, genitourinary, central nervous system, and ‘other’ [bradycardia, rash or itching, fall from bed, adverse drug effects] complications) and 30-day readmission. Opioid utilization was extracted from billing for opioids (fentanyl, hydrocodone, hydromophone, meperidine, morphine, oxycodone, and propoxyphene) and was converted into oral morphine equivalents using the Lexicomp® “opioid agonist conversion” [15] and the GlobalRPH “opioid analgesic converter” [16] calculator. Cost of hospitalization was adjusted for inflation and reported as 2016 US dollars. 30-day readmission was defined as any readmission within the study period to the same hospital where the primary surgical procedure was performed.
Patient demographic variables included age, gender, race/ ethnicity (White, Black, Other). Healthcare-related variables were insurance type (Commercial, Medicaid, Medicare, uninsured, unknown), hospital location (rural, urban), hospital size (< 300 beds, 300–499 beds, ≥ 500 beds), hospital teaching status, and number of annual TAA/ankle arthrodesis procedures per hospital. The procedure-related variables were year of procedure, type of surgeon (orthopedic foot/ankle surgeon, podiatrist, other/missing), setting of procedure (inpatient, outpatient), and diagnosis of osteoarthritis. Comorbidity burden was quantified using the Quan adaptation of the Charlson–Deyo Comorbidity Index [17]. Additionally, smoking and obesity (≥ 30 kg/m2) were also included.
Statistical analysis
TAA and ankle arthrodesis were analyzed as separate cohorts. Univariable associations between use of a PNB and the above-mentioned study variables were assessed using standardized differences, instead of p values as univariable group differences easily reach statistical significance in large sample sizes. A standardized difference of 0.1 (or 10%) generally indicates a meaningful difference in covariate distribution between groups [18]. Mixed-effects models measured associations between the use of PNB and outcomes, separately for patients having their surgery in an inpatient or outpatient setting. Mixed-effects models account for the correlation between patients treated at the same hospital/clinic, on the assumption that they will receive similar treatment and care. Here, separate regression lines are fitted for each hospital [7]. We report adjusted odds ratios (OR) and 95% confidence intervals (CI) for the binary outcomes. The continuous outcomes of opioid utilization, cost of hospitalization, and length of stay were modeled using the gamma distribution and log link function because of their skewed distribution [8, 9]. For these outcomes, we report the percent (%) change compared to the reference. All multivariable analyses were performed using the PROC GLIMMIX procedure in SAS v9.4 statistical software (SAS Institute, Cary, NC).
Results
Overall, 5290 and 14,709 TAA and arthrodesis procedures were included, respectively. PNB was utilized in 8.7% of TAA and 9.9% of ankle arthrodesis procedures.
Among TAA procedures, PNB use increased from 2.6% in 2006 to 11.3% in 2016 (Table 1). Higher PNB use was particularly seen in large (≥ 500 beds, 10.6%) and teaching (11.5%) hospitals and among procedures performed by orthopedic foot/ankle surgeons (10.0% compared to podiatrists); all with standardized differences > 0.1. When looking at unadjusted outcome differences between groups, the most pronounced effect was seen for ‘Day 0’ opioid use: 128 compared to 144 oral morphine equivalents for those with and without a PNB, respectively. While not always as pronounced, similar patterns were observed in patients undergoing ankle fusion surgery (Table 2), except for a higher PNB use in medium-sized hospitals (300–499 beds).
After adjustment for relevant covariates, PNB use was significantly associated with decreased opioid utilization during the total hospital stay for both TAA and ankle arthrodesis procedures (− 16.9%, CI − 23.9%; − 9.1% and − 18.9%, CI − 24.4%; − 13.0%, respectively), but only for inpatient procedures. This was particularly driven by a decrease in opioid utilization on the day of surgery: − 23.8% (CI − 30.4%; − 16.6%) and − 24.5% (CI − 29.5%; − 19.2%) in TAA and ankle arthrodesis, respectively. Other than an 11.3% reduction in opioid use on the day of surgery among patients undergoing outpatient ankle arthrodesis, no clinically relevant effects of PNB use were seen for other outcomes (Table 3).
When looking at trends of PNB use against opioid utilization on the day of surgery, no consistent pattern emerged of lower opioid utilization among patients receiving a PNB compared to those that did not (Fig. 1). However, in the ankle arthrodesis cohort, a slight overall trend (independent of PNB use) towards decreasing opioid use was seen.
Opioid utilization (in oral morphine equivalents [mg]) on the day of surgery by patients receiving a PNB and those that did not; total ankle arthroplasty (upper) and ankle arthrodesis cohort (lower). Given the low use of PNBs before 2008, the trend lines in the total ankle arthroplasty cohort represent the 2008–2016 cohort
Discussion
In this first nationwide study on PNB use in TAA and ankle arthrodesis, we found that only a minority of patients received PNBs. Moreover, hospital factors (size and teaching status) and healthcare-related factors (surgeon type) appeared to be associated with PNB utilization. Importantly, PNB use was associated with significant opioid-sparing effects, specifically on the day of surgery, while no significant effects were seen for length of stay, discharge to SNF, and opioid-related complications. Trend analyses demonstrated a slight overall decrease in opioid utilization on the day of surgery, independent of PNB use, particularly in the ankle arthrodesis cohort.
Recent studies have demonstrated impact of regional anesthesia on a wide variety of perioperative outcomes including decreased blood loss [19], improved pain management [20], and reduced mortality [21]. Despite its proven efficacy and increase in popularity in the past 5 years, regional blocks are still in minority for most orthopedic procedures [3, 22]. Cozowicz et al. demonstrated that in only 8.7% of total hip arthroplasty and 20.4% of total knee arthroplasty procedures, a PNB was used up till 2016 with a slight increasing trend using the same national database [3]. Compared to the hip and knee arthroplasty literature, PNB utilization studies in foot and ankle surgery has been lacking [3, 4]. Similar trends as found in the hip and knee arthroplasty literature are reflected in our dataset; for both TAA and ankle arthrodesis, only a fraction of patients in the dataset received peripheral nerve blocks (8.7% and 9.9%, respectively), but there is a general upward trend in PNB usage from 2006 to 2016.
Hospital factors, such as size and teaching status, were associated with PNB use with particularly higher use seen in teaching hospitals and medium- and large-sized hospitals. One possible explanation is that larger academic hospitals are more likely to be on the forefront of regional anesthetics than non-teaching hospitals. This finding is also evident in hip and knee research [4]. Recent studies have shown that hospital factors may contribute to patient and financial outcomes. Beck et al. recently published their data comparing TAA performed at an orthopedic specialty hospital versus at an academic teaching hospital [23]. They found no differences in patient safety and clinical outcomes, but noted significant discrepancies in length of stay. They postulated that the specialized staffing in addition to familiarity of ancillary services with the patients and procedures allows for higher efficiency in orthopedic specialty hospitals. Although this implies that academic and larger hospitals typically have dedicated services and staff with standardized protocols to facilitate and manage patients’ expectations (more so than smaller non-academic hospitals), this has not been validated in the current literature. Therefore, hospital factors cannot be ignored when considering what may contribute to the differential employment of PNB.
In a similar vein, a surgeon’s training background may influence peripheral block usage, as our data illustrated that orthopedic surgeons are significantly more likely than podiatrists to use this method of anesthesia for both procedures. In significant parts of the U.S., both foot and ankle surgeons (MD and DO) and podiatrists can perform surgical procedures in the foot and ankle regions. Both professions specialize in management of disorders of the foot and ankle, but their educational backgrounds differ in several ways. Orthopedic foot/ankle surgeons are medical doctors (MDs or DOs) trained in the diagnosis and management of diseases of the musculoskeletal system who specialize in the foot and ankle, while podiatrists are doctors of podiatric medicine (DPMs) trained exclusively on management of the foot, ankle, and lower leg. Both professions have similar undergraduate training requirements. Additionally, both require four years of postgraduate training, but the former must do so at an accredited medical school, while the latter must do so at a podiatric medical school. Upon completion of postgraduate training, orthopedic surgeons are then required to complete a five-year residency covering training in generalized orthopedic surgery, followed by an optional year of sub-specialized fellowship training devoted exclusively to disorders of the ankle and foot. In contrast, podiatrists must complete three years of foot and ankle surgical residency training after obtaining their postgraduate degrees. Differences in training focuses between the two provider types in combination with the fact that orthopedists are more likely to practice in an academic facility, orthopedic surgeons are more likely to go forth with a PNB than podiatrists.
Most importantly, our study demonstrates that after adjusting for covariates, PNB usage is associated with reduction in total opioid utilization for both TAA and ankle arthrodesis (-16.9% and -18.9%, respectively), mostly driven by reductions on the day of surgery. This trend has been identified in similar studies assessing a variety of orthopedic procedures [3, 4]. A prospective randomized study showed that implementation of lumbosacral plexus blocks in total hip arthroplasties resulted in decreased opioid consumption [24]. The authors found that adequate PNB with light sedation had lower incidences of postoperative delirium and postoperative cognitive decline with earlier discharge readiness times. A randomized controlled trial assessing efficacy of PNBs in total knee arthroplasty patients found a 50% reduction in morphine consumption during the immediate postoperative phase [25]. Young et al. retrospectively reviewed 78 patients underwent TAA, and they found patients who received continuous PNB consumed approximately half of the opioid medication within the first 48 h post-operatively compared to the non-continuous PNB group [26]. We also found that the largest decrease in opioid utilization was seen on the day of surgery for both TAA and ankle arthrodesis. The first day of surgery is also the day that coincides with the highest opioid consumption. Therefore, this result suggests that PNB was successful in mitigating acute post-operative pain and hence reducing overall opioid consumption. Considering the ongoing national public health crisis surrounding opioid consumption [27], this correlation highlights one of many potential avenues to curb over-prescription of opioids.
When assessing the limitations of this study, it is important to consider that this observational study can only describe correlations, not causations. Regarding our database, information on certain potentially confounding variables (e.g., patient socioeconomic status, preoperative opioid utilization, etc.) and important outcome variables (e.g., pain scores) was not available. Additionally, the reliability of this study relies on minimal variation in data collection between participating hospitals. Finally, these data were sourced from billing records precludes us from analyzing important details surrounding PNBs performed (i.e., anesthetic choice and dose, specialty of the provider performing the PNB, institutional variations in post-PNB opioid administration policies, etc.). Furthermore, many surgeons provide local infiltration anesthesia as part of their pain control protocol, but this part of the practice is largely not coded in healthcare database. Due to these limitations, further studies are required utilizing alternative sources of data to definitively determine the outcomes arising from use of PNBs.
In conclusion, this study assessed the effect of regional block usage on resource consumption and patient outcomes in patients undergoing TAA and ankle arthrodesis. Our study demonstrates that there are no significant demographic differences in patients receiving PNBs; however, orthopedic surgeons in teaching hospitals more commonly provide this form of anesthesia/analgesia. Moreover, our data suggest that regional block utilization is associated with a substantial relative reduction in postoperative opioid use for both TAA and ankle arthrodesis. Given the increasing the demand for TAA and ankle arthrodesis surgery and the current low use of PNBs, our study provides evidence of beneficial effects on the population level with a wider implementation of PNB use in these surgical cohorts.
References
Makadia R, Ryan PB. Transforming the premier perspective hospital database into the observational medical outcomes partnership (OMOP) common data model. Egems. 2014;2(1):1110. https://doi.org/10.13063/2327-9214.1110.
Premier Healthcare Database White Paper: Data that Informs and Performs. 2020. Online: https://products.premierinc.com/downloads/PremierHealthcareDatabaseWhitepaper.pdf (accessed 8/22/2021).
Cozowicz C, Poeran J, Zubizarreta N, Mazumdar M, Memtsoudis SG. Trends in the use of regional anesthesia: neuraxial and peripheral nerve blocks. Reg Anesth Pain Med. 2016;41(1):43–9. https://doi.org/10.1097/AAP.0000000000000342.
Memtsoudis SG, Poeran J, Cozowicz C, Zubizarreta N, Ozbek U, Mazumdar M. The impact of peripheral nerve blocks on perioperative outcome in hip and knee arthroplasty-a population-based study. Pain. 2016;157(10):2341–9. https://doi.org/10.1097/j.pain.0000000000000654.
Kessler ER, Shah M, Gruschkus K, S, Raju A. . Cost and quality implications of opioid-based postsurgical pain control using administrative claims data from a large health system: Opioid-related adverse events and their impact on clinical and economic outcomes. Pharmacotherapy. 2013;33(4):383–91.
Srikumaran U, Stein BE, Tan EW, Freehill MT, Wilckens JH. Upper-extremity peripheral nerve blocks in the perioperative pain management of orthopaedic patients: AAOS exhibit selection. J bone Jt Surg Am. 2013;95(24):e197. https://doi.org/10.2106/JBJS.L.01745.
Witte JS, Greenland S, Kim LL, Arab L. Multilevel modeling in epidemiology with GLIMMIX. Epidemiology. 2000;11(6):684–8.
Moran JL, Solomon PJ, (2012) Outcome ACf, Resource Evaluation of the A, New Zealand Intensive Care S. A review of statistical estimators for risk-adjusted length of stay: analysis of the Australian and new Zealand Intensive Care Adult Patient Data-Base, 2008–2009. BMC Med Res Methodol.;12:68. doi: https://doi.org/10.1186/1471-2288-12-68.
Rascati KL, Smith MJ, Neilands T. Dealing with skewed data: an example using asthma-related costs of medicaid clients. Clin Ther. 2001;23(3):481–98.
Lee KT, Park YU, Jegal H, Roh YT, Kim JS, Yoon JS. Femoral and sciatic nerve block for hindfoot and ankle surgery. J Orthop Sci: Off J Jpn Orthop Assoc. 2014;19(4):546–51. https://doi.org/10.1007/s00776-014-0576-5.
Hansen E, Eshelman MR, Cracchiolo A 3rd. Popliteal fossa neural blockade as the sole anesthetic technique for outpatient foot and ankle surgery. Foot Ankle Int. 2000;21(1):38–44. https://doi.org/10.1177/107110070002100107.
Myerson MS, Ruland CM, Allon SM. Regional anesthesia for foot and ankle surgery. Foot Ankle. 1992;13(5):282–8.
Henningsen MJ, Sort R, Moller AM, Herling SF. Peripheral nerve block in ankle fracture surgery: a qualitative study of patients’ experiences. Anaesthesia. 2018;73(1):49–58. https://doi.org/10.1111/anae.14088.
Stefani KC, Ferreira GF, Pereira Filho MV. Postoperative analgesia using peripheral anesthetic block of the foot and ankle. Foot Ankle Int. 2018;39(2):196–200. https://doi.org/10.1177/1071100717739670.
Seaworth CM, Do HT, Vulcano E, Mani SB, Lyman SL, Ellis SJ. Epidemiology of total ankle arthroplasty: trends in New York state. Orthopedics. 2016;39(3):170–6. https://doi.org/10.3928/01477447-20160427-12.
McAuley D, Pharm.D.: GlobalRPH Opioid Analgesic Converter http://globalrph.com/narcoticonv.htm (accessed 07–21–2017). http://globalrph.com/narcoticonv.htm Accessed 19–09–2016.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424. https://doi.org/10.1080/00273171.2011.568786.
Modig J, Karlstrom G. Intra- and post-operative blood loss and haemodynamics in total hip replacement when performed under lumbar epidural versus general anaesthesia. Eur J Anaesthesiol. 1987;4(5):345–55.
Elkassabany N, Cai LF, Mehta S, Ahn J, Pieczynski L, Polomano RC, Picon S, Hogg R, Liu J. Does regional anesthesia improve the quality of postoperative pain management and the quality of recovery in patients undergoing operative repair of tibia and ankle fractures? J Orthop Trauma. 2015;29(9):404–9. https://doi.org/10.1097/BOT.0000000000000344.
Basques BA, Toy JO, Bohl DD, Golinvaux NS, Grauer JN. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am. 2015;97(6):455–61. https://doi.org/10.2106/JBJS.N.00662.
Cozowicz C, Poeran J, Memtsoudis SG. Epidemiology, trends, and disparities in regional anaesthesia for orthopaedic surgery. Br J Anaesth. 2015;115(Suppl 2):57–67. https://doi.org/10.1093/bja/aev381.
Beck DM, Padegimas EM, Pedowitz DI, Raikin SM. Total ankle arthroplasty: comparing perioperative outcomes when performed at an orthopaedic specialty hospital versus an academic teaching hospital. Foot Ankle Spec. 2017;10(5):441–8. https://doi.org/10.1177/1938640017724543.
Mei B, Zha H, Lu X, Cheng X, Chen S, Liu X, Li Y, Gu E. Peripheral nerve block as a supplement to light or deep general anesthesia in elderly patients receiving total hip arthroplasty: a prospective randomized study. Clin J Pain. 2017;33(12):1053–9. https://doi.org/10.1097/AJP.0000000000000502.
Allen HW, Liu SS, Ware PD, Nairn CS, Owens BD. Peripheral nerve blocks improve analgesia after total knee replacement surgery. Anesth Analg. 1998;87(1):93–7.
Young DS, Cota A, Chaytor R. Continuous infragluteal sciatic nerve block for postoperative pain control after total ankle arthroplasty. Foot Ankle Spec. 2014;7(4):271–6. https://doi.org/10.1177/1938640014537303.
Knaul FM, Farmer PE, Krakauer EL, De Lima L, Bhadelia A, Jiang Kwete X, Arreola-Ornelas H, Gomez-Dantes O, Rodriguez NM, Alleyne GAO, Connor SR, Hunter DJ, Lohman D, Radbruch L, Del Rocio Saenz Madrigal M, Atun R, Foley KM, Frenk J, Jamison DT, Rajagopal MR, Lancet Commission on Palliative C, Pain Relief Study G. (2018) Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: the Lancet Commission report. Lancet (London, England).391(10128):1391–454. doi: https://doi.org/10.1016/S0140-6736(17)32513-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Chan, J.J., Garden, E., Chan, J.C. et al. Peripheral nerve block use in ankle arthroplasty and ankle arthrodesis: utilization patterns and impact on outcomes. J Anesth 35, 879–888 (2021). https://doi.org/10.1007/s00540-021-02994-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-02994-w