Abstract
Study design
A systematic review and meta-analysis.
Objective
The purpose of this study was to evaluate the clinical outcome and safety of sacroplasty for patients with secondary metastatic lesions to the sacrum.
Methods
Several databases, including the Cochrane library, PubMed and EMBASE, were systematically searched to identify potentially eligible articles in English language. All the above databases were searched until December 2019. The search strategy was based on the combination of the following keywords: sacroplasty AND secondary tumours OR metastasis OR metastases. The reference list of the selected literature was also reviewed and a standard PRISMA template utilised.
Results
From a total of 102 articles initially identified, a final seven studies were identified as meeting the inclusion criteria. A total of 107 patients from these studies were included. The follow-up ranged from immediate post-operatively to 30.5 months. The mean preoperative VAS was 8.38 (range 6.9–9.3), which improved significantly to 3.01 (range 1.12–4.7) post-operatively (p < 0.001). The most frequent complication reported was cement leakage, which occurred in 26 patients (25.4%), but without any neurological or other adverse sequelae.
Conclusions
Sacroplasty in the management of secondary sacral tumours is a safe procedure that can achieve a significant reduction in pain, as quantified by VAS scores, and low complication rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The skeleton is the third most common site of metastasis after the lung and liver, with the axial skeleton most frequently involved [1,2,3]. Primary spinal tumours are uncommon, but, of these, 31.5% involve the sacrum [4]. The most common primary sites for metastatic tumours of bones include the breast, lung, kidney, thyroid and prostate [2, 5]. Symptomatic spinal metastases are estimated to occur in 10–20% of all cancer patients, with the thoracic spine being involved in 70% of these, the lumbar in 20% and the sacrum in a small minority of cases [5]. Up to 50% of spinal metastases require some form of treatment and 5–10% require surgical management [6].
For sacral metastatic lesions, the treatment is typically palliative, aiming at pain control and salvage of neurologic function [7]. Currently, the two main methods of treating sacral tumours are radiotherapy and surgery. Radiotherapy is the procedure of choice for tumours without spinal instability or neurological compromise [2]. Surgical intervention for sacral tumours is a complex endeavour. En bloc sacrectomy is a procedure with a high rate of major complications, regardless of tumour histology, often requiring readmissions and secondary interventions [8]. Surgical options for pathological sacral fractures are limited given the invasiveness and potential morbidity of open instrumented sacropelvic stabilization [9].
Sacroplasty involves the injection of Polymethyl methacrylate (PMMA) cement into the sacral ala in the tumour area or around the fracture zone. In the context of insufficiency fractures of the sacrum, sacroplasty has been shown to provide a significant improvement in pain as measured by the visual analogue scale (VAS) [10]. The procedure is also evolving as a treatment for sacral tumours; it can provide a minimally invasive alternative to other surgical procedures in cases without neurological deficit or instability, the main improvements being in pain and mobility [2]. The evidence for this has been largely based on level IV studies. Here, we review the published literature on sacroplasty for spinal tumours and summarize the clinical outcomes.
Materials and methods
Search strategy
Several databases, including the Cochrane library, PubMed and EMBASE, were systematically searched to identify potentially eligible articles. All the above databases were searched up to December 2019. The search strategy was based on the combination of the following keywords: sacroplasty, cement augmentation, secondary tumours, and sacral metastases. The reference list of selected literatures was also reviewed.
Inclusion and exclusion criteria
Inclusion criteria were established before the search, and the following criteria were used.
We limited our results to articles published in the English language that reported on and included clinical outcomes of sacroplasty in patients with secondary sacral tumours.
Exclusion criteria: (1) non-English language, (2) case reports and expert opinions, (3) no reported outcome measures, (4) sacroplasty for reasons other secondary tumours, (5) lower than 4 cases of sacroplasty and (6) repetitive studies.
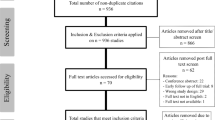
A flow chart outlining the search is provided in (Fig. 1). For the assessment of evidence quality, the Oxford Centre for Evidence-Based Medicine (CEBM) grading system was utilized.
Data extraction
Each article from the primary search was individually assessed for inclusion, based on its title and abstract, according to these parameters. A second review, which included assessing the full article, was performed by the main author to further discriminate the primary findings.
For each study included in the analysis, the main author, year of publication, level of evidence and patient characteristics (per reported cohort) were tabulated, along with the follow-up data, imaging method and technique used. The clinical outcomes as presented in the papers are shown in (Table 1), including any improvement in pain documented using the VAS and the rate and nature of any complications.
Institutional review board approval was not necessary.
Results
Type of study
Seven papers were published in the English language literature between 1996 and 2019. There was no level I, II or III evidence available to include in our study. Four papers were retrospective case series, and three papers were prospective case series. The follow-up ranged between immediate post-operative and 30.5 months.
Sun et al. [11] studied seven patients who underwent sacroplasty for severe painful sacral metastases. Significant pain relief was reported with VAS reduction ≥ 4 points in all seven patients at 1 month after the procedure, six out of seven at 3 months and five out of seven at 6 months of follow-up. Pain relief was considered good if the score was 0–3, partial if the score was 4–6 and insufficient or null if the score was 7–10. A good level of pain relief was observed in five out of seven patients, and partial pain relief was observed for two out of seven patients, insufficient pain relief was not noticed at 1 month after the procedure. Good and partial pain relief was observed in six out of seven patients at 3 months and five out of six patients at 6 months, respectively. Cement leakage at S1 foramina was noticed in one case without clinical significance.
Andresen et al. [12] studied 10 patients who had sacroplasty for metastatic involvement of the sacrum. A significant (p < 0.001) reduction in pain according to the VAS occurred in all patients from 9.3 ± 0.67(8–10) preoperatively to 2.7 ± 1.28 (1–5) on the second post-operative day and 2.9 ± 0.81 (2–5) 6 months after the intervention. No significant complications were reported.
Georgy et al. [13] studied 12 patients with malignant metastatic lesions of the sacrum and pelvis who underwent percutaneous cement augmentation. All treated patients reported decreased pain level by VAS (except for 1 patient) within 2–4 weeks of follow-up. Average VAS score was 8.6 before the procedure and improved to 3.8 after the procedure. Three patients had minimal clinically insignificant leakage.
Basile et al. [14] studied eight patients who underwent sacroplasty for sacral multiple myelomas. All patients experienced improvements in symptoms after the procedure, as demonstrated by improved VAS scores pre-op: 7.5 ± 1.1, post-op: 1.12 ± 1.2 and performance status and decreased analgesic dose during follow-up. One case of a small and asymptomatic foraminal leak was reported.
Kortman et al. [15] studied 39 patients with symptomatic sacral lesions. The average pre-treatment VAS score of 9.0 ± 0.9 in patients with sacral lesions was significantly improved after sacroplasty to 2.6 ± 2.4 (p < 0.001). There were no major complications or procedure-related deaths.
Moussazadeh et al. [9] studied 25 patients with cancer-associated sacral insufficiency fractures. Twenty of 25 patients (80%) had reduction in their visual analogue pain score at a median follow-up of 6.5 months; no patients were worsened. The mean visual analogue scale score decreased from 8.8 to 4.7 post-procedurally (p < .001). Extravertebral cement migration was noted in 18 procedures without being clinically significant. Six repeat or contralateral procedures were performed.
Tian et al. [16], studied 10 patients who underwent percutaneous sacroplasty for painful sacral metastases. The mean VAS declined significantly (p < 0.01) from 6.9 ± 1.2 before the procedure to 2.7 ± 1.34 after the procedure reflected by significant reduction (p < 0.01) in opioids use before and after the surgery. Extraosseous cement leakage occurred in 3 cases out of 10 without causing any clinical complications.
Clinical outcome assessment
VAS score was reported as a clinical outcome measure in all patients. The mean preoperative VAS was 8.38 (range 6.9–9.3), and the mean post-operative VAS was 3.01 (range 1.12–4.7) (p < 0.001, two-tailed paired t test). The improvement appeared to be maintained in all series at the latest follow-up, which ranged from immediate post-op to 30.5 months.
Complications
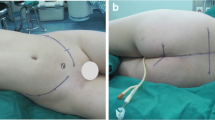
The only complication reported was cement leakage, which occurred in 26 patients and was without clinical significance. Figure 2 is a case illustration of sacroplasty performed for a sacral metastasis in our unit.
Discussion
This systematic review and meta-analysis shows that sacroplasty in the management of secondary lesions of the sacrum is a safe procedure and can result in significant reduction in pain as quantified by VAS scores and with low complication rates. Metastatic tumours of the sacrum, although less frequent than metastatic lesions of the thoracic or lumbar spine, have a devastating impact on an individual’s quality of life by causing pain, functional disability, sensory/motor deficits and, eventually, bladder and bowel dysfunction [2].
Vertebroplasty was first introduced in Amiens in 1984 by Gailbert and Deramond [17]. After a 50-year-old patient underwent laminectomy of the L2 vertebra for a haemangioma, three millilitres of bone cement were injected into the L2 vertebral body for reinforcement. Following surgery, the patient experienced complete pain relief. Since then, the procedure has been used for osteoporotic and metastatic vertebral fracture and has proven to be safe and effective in providing pain relief and improving functional outcomes in patients with vertebral body fractures [18, 19].
The main treatment options for sacral metastasis are radiotherapy and surgery. Radiotherapy is indicated in patients without spinal instability or acute neurological deterioration. There are several limitations of radiotherapy when used in the treatment of spinal metastasis. Radiosensitivity varies among tumours types. In general, prostate and lymphoid tumours are radiosensitive, breast cancer is 70% sensitive and 30% resistant, and gastrointestinal tumours, renal cell tumours and melanomas are radioresistant [2].
Pain response also varies among patients. A study by Chow assessed pain scores after radiotherapy and found that partial response (PR) rates at 2, 4, 8 and 12 weeks occurred in 44, 42, 30 and 38% of the patients, respectively, whereas complete response rates were 24, 32, 31 and 29% [20]. Complete response was defined as zero on the VAS, whereas PR was defined as a reduction of VAS score of two or more points, or a ≥ 50% reduction of the pre-treatment pain score. Pain flare is also common among patients, lasting for three days on average and occurring in nearly 40% of the patients receiving palliative radiotherapy for symptomatic bone metastases [21]. In the context of sacral insufficiency fractures, sacroplasty was found to produce significant improvements in VAS scores and was recommended as an alternative to analgesia and rehabilitation [10].
Injection of the cement seems to be related to the analgesic effect, but the exact mechanism of pain relief is not well understood. Various authors have postulated that stabilization of microfractures, the tumouricidal effect of cement through cytotoxic activity or thermal necrosis can play a role in pain reduction [22,23,24,25]. In any case, in our literature review, we found immediate, significant and sustained pain relief after sacroplasty for sacral metastasis. Sacroplasty could offer an alternative approach to treating painful sacral lesions where neurological deficit or instability is not present [2].
The largest series to date is presented by Pereira, who reports the results of sacroplasty in 42 patients with sacral metastasis, nine patients with insufficiency fractures and seven patients with primary sacral tumours [26]. Unfortunately, the authors did not differentiate between groups, although they performed a statistical analysis which shows no difference in clinical outcome between the three groups (p = 0.50). Statistically significant differences were observed between pre- and post-sacroplasty mean VAS scores (Student’s t test, p < 0.05). They concluded that percutaneous sacroplasty for metastatic and osteoporotic fractures is a safe and effective technique in terms of pain relief and functional outcome.
Good imaging quality is a crucial factor in the success of sacroplasty. The sacrum is different from the cuboidal shape of the vertebral body in terms of its three-dimensional anatomy. In the majority of the analysed studies, fluoroscopy appears to be the main technique used, either alone or in combination with CT. The fluoroscopy visualization seems to be the preferred imaging technique during the cement injection in order to ensure maximal bone penetration and to prevent leakage. The relationship between the cement and sacral foramina can be difficult to ascertain with standard fluoroscopy due to the oblique configuration of the sacrum and its foramina. Consequently, some authors preferred to first place the needle under CT guidance and then, visualize the cement injection under fluoroscopy [11, 13].
The most frequent complication encountered in our review was cement extravasation, which occurred in 26 patients but was asymptomatic and without clinical significance in all of them. More than half of them were reported in one study in which Moussazadeh et al. [9] reported extravertebral cement migration in 18 out of 31 sacroplasties done. However, none were clinically significant.
Conclusion
Sacroplasty in the management of secondary lesions of the sacrum is a safe procedure and can result in significant reduction in pain as quantified by VAS scores and low complication rates. This is a review of level IV studies and we cannot provide clear recommendation in favour of this procedure. However, given the significant benefits of sacroplasty noted in this series, we feel that further studies on sacroplasty would be of great interest.
References
Aaron AD (1994) The management of cancer metastatic to bone. JAMA 272(15):1206–1209
Quraishi NA, Giannoulis KE, Edwards KL et al (2012) Management of metastatic sacral tumours. Eur Spine J 21(10):1984–1993
Quraishi NA, Giannoulis KE, Manoharan SR et al (2013) Surgical treatment of cauda equina compression as a result of metastatic tumours of the lumbosacral junction and sacrum. Eur Spine J 22(1):S33–S37
Kelley SP, Ashford RU, Rao AS et al (2007) Primary bone tumours of the spine: a 42-year survey from the Leeds Regional Bone Tumour Registry. Eur Spine J 16(3):405–409
Vialle LR (2015) AOSpine Masters Series. Thieme Medical Publishers, New York
Bilsky MH, Lis E, Raizer J et al (1999) The diagnosis and treatment of metastatic spinal tumor. Oncologist 4(6):459–469
Raque GH Jr, Vitaz TW, Shields CB (2001) Treatment of neoplastic diseases of the sacrum. J Surg Oncol 76(4):301–307
Verlaan JJ, Kuperus JS, Slooff WB et al (2014) Complications, secondary interventions and long term morbidity after en bloc sacrectomy. Eur Spine J 24(10):2209–2219
Moussazadeh N, Laufer I, Werner T et al (2015) Sacroplasty for cancer-associated insufficiency fractures. Neurosurgery 76(4):446–450 discussion 50
Bayley E, Srinivas S, Boszczyk BM (2009) Clinical outcomes of sacroplasty in sacral insufficiency fractures: a review of the literature. Eur Spine J 18(9):1266–1271
Sun G, Jin P, Li M et al (2012) Three-dimensional C-arm computed tomography reformation combined with fluoroscopic-guided sacroplasty for sacral metastases. Support Care Cancer 20(9):2083–2088
Andresen R, Radmer S, Ludtke CW et al (2014) Balloon sacroplasty as a palliative pain treatment in patients with metastasis-induced bone destruction and pathological fractures. Rofo 186(9):881–886
Georgy BA (2009) Percutaneous cement augmentations of malignant lesions of the sacrum and pelvis. AJNR Am J Neuroradiol 30(7):1357–1359
Basile A, Tsetis D, Cavalli M et al (2010) Sacroplasty for local or massive locaization of multiple myeloma. Cardiovasc Intervent Radiol 33(6):1270–1277
Kortman K, Ortiz O, Miller T et al (2013) Multicenter study to assess the efficacy and safety of sacroplasty in patients with osteoporotic sacral insufficincey fractures or pathologic sacral lesions. J Neurointerv Surg 5(5):461–466
Tian QH, Liu HF, Wang T et al (2019) Percutaneous sacroplasty for painful sacral metastases involving multiple sacral vertebral bodies: initial experience with an interpedicular approach. Korean J Radiol 20(6):939–946
Galibert P, Deramond H, Rosat P et al (1987) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 33(2):166–168
Mendel E, Bourekas E, Gerszten P et al (2009) Percutaneous techniques in the treatment of spine tumors: what are the diagnostic and therapeutic indications and outcomes? Spine (Phila Pa 1976) 34(22 Suppl):S93–100
Barr JD, Barr MS, Lemley TJ et al (2000) Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine (Phila Pa 1976) 25(8):923–928
Chow E, Wong R, Hruby G et al (2001) Prospective patient-based assessment of effectiveness of palliative radiotherapy for bone metastases. Radiother Oncol 61(1):77–82
Gomez-Iturriaga A, Cacicedo J, Navarro A et al (2015) Incidence of pain flare following palliative radiotherapy for symptomatic bone metastases: multicenter prospective obsevational study. BMC Palliat Care 14:48
Pilitsis JG, Rengachary SS (2001) The role of vertebroplasty in metastatic spinal disease. Neurosurg Focus 11(6):e9
Whitlow CT, Yazdani SK, Reedy ML et al (2007) Investigating sacroplasty: technical considerations and finite element analysis of polymethylmethacrylate infusion into cadaveric sacrum. AJNR Am J Neuroradiol 28(6):1036–1041
Roedel B, Clarencon F, Touraine S et al (2015) Has the percutaneous vertebroplasty a role to prevent progression or local recurrence in spinal metastases of breast cancer? J Neuroradiol 42(4):222–228
Nelson DA, Barker ME, Hamlin BH (1997) Thermal effects of acrylic cementation at bone tumour sites. Int J Hyperthermia 13(3):287–306
Pereira LP, Clarencon F, Cormier E et al (2013) Safety and effectiveness of sacroplasty: a large single-centre experience in 58 patients with tumours or osteoporotic insufficient fractures treated under fluoroscopic guidance. Eur Radiol 23(10):2764–2772
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tarawneh, A.M., Sabou, S., AlKalbani, S. et al. Clinical outcomes of sacroplasty for metastatic sacral tumours: a systematic review and meta-analysis. Eur Spine J 29, 3116–3122 (2020). https://doi.org/10.1007/s00586-020-06562-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06562-w