Abstract
Objective
To report our experience in percutaneous sacroplasty (PSP) for tumours and insufficiency fractures of the sacrum.
Methods
Single-centre retrospective analysis of 58 consecutive patients who underwent 67 PSPs for intractable pain from sacral tumours (84.5 %) or from osteoporotic fractures (15.5 %). The following data were assessed: visual analogue scale (VAS) before and after the procedure for global pain; short-term (1-month) clinical follow-up using a four-grade patient satisfaction scale (worse, unchanged, mild improvement and significant improvement); modification in analgesics consumption; referred short-term walking mobility. Minor and major complications were systematically assessed.
Results
The mean VAS score was 5.3 ± 2.0 in pre-procedure and 1.7 ± 1.8 in post-procedure. At 1-month follow-up, 34/58 (58.5 %) patients experienced a mild improvement; 15/58 (26 %) presented a significant improvement while 4/58 (7 %) and 5/58 (8.5 %) patients had unchanged or worse pain, respectively. Decreased analgesic consumption was observed in 34 % (20/58) of the patients. Eighty percent of patients with walking limitation experienced improvement, 16 % remained unchanged and 4 % were worse. We noted minor complications in 2/58 patients (3.4 %) and major complications in 2/58 patients (3.4 %).
Conclusion
Percutaneous sacroplasty for metastatic and osteoporotic fractures is a safe and effective technique in terms of pain relief and functional outcome.
Key points
• Percutaneous sacroplasty provides pain relief and functional improvement for insufficiency sacral fractures.
• Percutaneous sacroplasty provides pain relief and function improvement for sacral tumours.
• The major complication rate is acceptable (3.4 %), and is higher in sacral tumours.
• Posterior wall/cortical sacral bone disruption is not statistically associated with more complications.
• However, osteolytic tumours seem to be associated with higher risk of complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sacral metastases and insufficiency fractures are disabling causes of severe low back pain, leading patients to bed rest with increased risk of comorbidities, such as pneumonia, urinary tract infections, deep vein thrombosis, pulmonary embolism, muscle atrophy and sacral decubitus ulcers [1]. Moreover, these patients usually require high doses of opiates, especially for sacral metastasis, that may be responsible for major side effects [2].
Percutaneous vertebroplasty (PV) has gained acceptance in recent years for stabilising traumatic and osteoporotic fractures and as a palliative treatment of metastatic painful lesions [3–6]. The cementoplasty of the sacrum (percutaneous sacroplasty [PSP]), a variant of vertebroplasty, is used for the same purpose. However, there are several technical considerations that are unique to PSP, mainly the risk of cement leakage into the sacral foramina [1]. The effectiveness and safety of this technique has been poorly reported, until recently in small series or case reports [7–12], most of these being focused on insufficiency fractures.
The aim of our study was to retrospectively report our experience of 67 consecutive PSPs in 58 patients treated for osteoporotic lesions or tumours of the sacrum.
Materials and methods
Patients
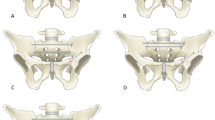
Patients’ demographics are summarised in Table 1 and Fig. 1.
We retrospectively review the data of 58 consecutive patients that underwent 67 PSP procedures in our institution for intractable pain from sacral tumours or from osteoporotic fractures, from January 2002 to July 2011. Procedures were performed in 42 women and 16 men (mean age 62 years, range 27–88), on an outpatient basis. Of these patients, 72.5 % (42/58, 28 women and 14 men) had metastatic lesions (from breast cancer, n = 19; lung cancer, n = 5; thyroid cancer, n = 4; endometrium cancer, n = 2; oesophagus cancer, n = 1; rectum cancer, n = 1; bladder cancer, n = 2; carcinoma of unknown origin, n = 8), 15.5 % (9/58, 7 women and 2 men) osteoporotic fractures and 12 % (7/58, all females) had sacral primitive tumours (plasmocytoma/myeloma, n = 4; haemangioma, n = 1; chondrosarcoma, n = 1; chordoma, n = 1). All patients presented with a history of lower back pain that was minimally responsive to analgesic treatment or had adverse effects (constipation, urinary retention and/or confusion) from opioid treatment with controlled pain. In case of osteoporosis, failure of conservative treatment was considered after a period of at least 4 weeks. None of the patients with sacral insufficiency fracture had other concomitant symptomatic vertebral compression fracture. Thirty-four patients with sacral metastasis had undergone previous chemotherapy and/or local radiotherapy.
All patients had pre-procedure imaging focusing on the sacrum area, including computed tomography (CT) (bone and soft tissue windowing), 1.5-T magnetic resonance (MR) imaging (at least T1-weighted images [WI], T2-WI and T1 fat-saturated-WI after gadolinium injection in at least two orthogonal planes). The CT findings enabled us to classify spinal metastases as osteolytic, osteoblastic, or mixed lesions. Epidural or soft tissue extensions were assessed on MR images; cortical bone disruption (of the posterior wall and of sacral foramina) was evaluated on CT.
Lesion characteristics
Lesion characteristics are summarised in Table 2.
In patients presenting tumoral lesions, the lesion was osteolytic in 21/49 cases (43 %); mixed in 24/49 cases (49 %) and osteoblastic in 4/49 cases (8 %). Sacral foramen cortical disruption was observed in 23/49 cases (47 %) and epidural extension was depicted on MRI in 5/49 cases (10 %). All osteoporotic lesions had radiological evidence of acute or sub acute fractures on CT and MR images.
Inclusion/exclusion criteria
Inclusion criteria were: patient older than 18 years with intractable (visual analogue scale [VAS] > 4) sacral pain related to imaging-proven insufficiency fracture of the sacrum or a sacral tumour. Patients with VAS ≤ 4 under opiates but with severe side effect of the analgesic treatment were also included in the study.
Exclusion criteria were: major sacral canal extension, nerve root or cauda equina compression related to the lesion, local cutaneous or subcutaneous infection, uncorrectable coagulopathy, active systemic infection or leucopaenia or history of allergy to polymethylmethacrylate (PMMA) bone cement used for vertebro/sacroplasty.
PSP technique
Percutaneous sacroplasty was bilateral in 38/58 patients (66 %) and unilateral in 20/58 patients (34 %) with a total of 67 procedures. Most of the procedures (82/96; 85.4 %) were performed under conscious sedation that was achieved with IV propofol (Diprivan; Astra-Zeneca, Rueil-Malmaison, France) alone or in combination with IV alfentanyl (Rapifen; Janssen-Cilag, Issy-les-Moulineaux, France) and midazolam hydrochloride (Hypnovel; Roche, Neuilly, France). Local anaesthesia (1 % lidocaine, Xilocaine; Astra, Södertälje, Sweden) was administered subcutaneously under fluoroscopic guidance and 1 g intravenous cefazolin (or other broad-spectrum antibiotic) was also administered at the beginning of the procedure in order to minimise any risk of infection. All procedures were performed by three operators with experience in cementoplasty of 20, 15 and 10 years, respectively. PSP was performed in an angiographic suite with a C-arm digitalised X-ray system (Angiostar; Siemens, Erlangen, Germany) for patients treated before 2007 (18/58 patients) and with a C-arm flat panel (Axiom Artis; Siemens, Erlangen, Germany) for those treated after 2007 (40/58 patients). The patient was placed in the prone position; the lumbo-sacral region prepped and draped to ensure sterility. General anaesthesia with oro-tracheal intubation was performed only for young patients, in patients with osteoblastic lesions, or when the positioning of the bone needle was suspected by the operator to be difficult. The sterile draped flat panel system was positioned at the anteroposterior (AP) view, centred on the sacral bone. Bevelled 11-gauge bone needles (Thiebaud, Margencel, France) were inserted into the sacrum and advanced with the aid of a mallet towards the centre of the lesion for the tumour lesions and into the fracture site for insufficiency sacral fractures. On average, 2.3 ±1 bone needles were used (range 1–5).
A posterior approach was performed in 85 % of the cases (57/67 procedures), whereas a transiliac approach was used in 25 % of the cases (17/67 procedures). In 10 % of the cases (7/67) both approaches were performed at the same time. When the imaging findings were not conclusive as to the cause of the lesion, a bone biopsy was performed before PMMA injection by using a coaxial system with a 13-gauge, long bone biopsy needle (Thiebaut). Then, PMMA cement (Biomet Bone Cement V; Biomet, Warsaw, IN, USA) mixed with tungsten powder (Balt, Montmorency, France), which enhances the cement’s radiopacity, was injected under fluoroscopic guidance until homogeneous filling of the target lesion was achieved. The goal of the cement injection was to fill the lesion as much as possible without extravasation of cement (Fig. 2).
A 66-year-old patient presenting a painful mixed metastatic lesion of the upper portion of the sacrum from a lung carcinoma. a Pre-operative axial CT, bone windowing showing a mixed lesion of the sacral bone. b MRI, axial T1-fat-saturated-weighted image (WI) after gadolinium injection. Foci of contrast media enhancement are seen within the upper segment of the sacrum, as well as in the ilion bones. c, d Plain X-rays in anteroposterior (AP) (c) and lateral (d) projections after the positioning of the bone needles. e Plain X-ray after injection of 10 cc polymethyl methacrylate (PMMA) bone cement, showing satisfactory filling of the bone lesion. f Post-percutaneous sacroplasty (PSP) axial CT confirming the satisfactory filling of the lesion and the absence of foraminal or intracanal cement leakage
Immediately after PMMA injection, standard anteroposterior (AP) and lateral control plain X-rays were performed. Sacral bone multidetector CT (Somatom Sensation 16; Siemens, Erlangen, Germany) with multiplanar reconstructions was also systematically performed in order to evaluate the filing of the lesion by the bone cement and to depict cement leakage.
Clinical outcome assessment
Patients’ records were assessed for pain and functional status, before and 30 days after the procedure. A VAS was used for pain evaluation, based on its subjective perception of pain, ranging between 0 and 10, where 0 corresponds to pain absence and 10 represents the worst pain imaginable. Overall improvement of clinical status was evaluated using a four-grade patient satisfaction scale: 1 = worse, 2 = unchanged, 3 = mild improvement and 4 = significant improvement. The comparison between analgesic drug consumption before and after PSP was systematically evaluated using the following semi-quantitative scale: 1 = increased oral narcotic analgesics, 2 = same drug treatment and 3 = reduced oral narcotic analgesics. Finally, the ambulation was evaluated with a three-grade scale: 1 = worse, 2 = unchanged and 3 = improvement of ambulation.
Complications were systematically assessed and divided into minor and major complications. Cement leakage leading to transient neurological deficit that resolved spontaneously or under medical treatment was considered as minor complication. Major complications were: cement leakage leading to permanent neurological deficit, neurological deficit requiring surgical decompression, or cauda equina syndrome, general complications after PSP (e.g. pulmonary embolism, pulmonary infection) or procedure-related death.
Statistical analysis
Analyses were performed to search for statistically significant associations among pain relief (decrease of 2 points or more on VAS between pre and post-PSP), decreased analgesic drug consumption (decrease of the dose of the analgesic drugs previously used or in case of switching to an analgesic drug of a lower level in the WHO scale), functional outcome (patient’s referral of mild or significant improvement of overall clinical status) as well as complications (major and minor complications) versus clinically or imaging-relevant characteristics of lesions. According to this rationale, the following paired dichotomous variables were tested: differences in terms of pain relief/functional outcome and patients with: (1) a sacral tumour or an insufficiency fracture; (2) a malignant or a benign tumour; (3) a bilateral or an unilateral lesion; (4) a lytic or a mixed/blastic lesion; (5) the presence or absence of posterior wall/cortical disruptions. The differences in terms of complication rates depending on the type of the lesion or depending on cortical/posterior wall disruption were also evaluated. Statistical analysis was performed with Medcalc software (Medcalc, Mariakerke, Belgium). We used a chi-squared test for categorical variables and Fisher exact tests when the expected values in the 2 × 2 contingency table for the chi-squared test were less than 5 in at least one cell. For continuous variables, the Student t-test for independent samples was used. A P value of less than 0.05 was considered to indicate a significant difference.
Ethical statement
Neither approval of the institutional review board nor patient informed consent was required by the ethics committee of our institution for retrospective analyses of patients’ records and imaging data.
Results
The results of pain and functional status are summarised in Table 3 and Figs. 3, 4 and 5).
Technical success with adequate distribution of cement was achieved in 49/58 patients (84 %) after the first procedure; technical success was achieved in the remaining 9 patients (16 %, 2 osteoporotic lesions and 7 tumours) after a second intervention. The mean VAS score was 5.3 ± 2.0 (range 1.0–9.0) pre-procedure and 1.7 ± 1.8 (range 0–6) post-procedure (Table 4). At the 1-month follow-up, 34/58 (59 %) patients experienced a mild improvement in overall clinical status; 15/58 (26 %) presented a major improvement, while 4/58 (6.3 %) and 5/58 (8.6 %) patients had unchanged or worse clinical status, respectively (Fig. 3). Decreased analgesic drug consumption was observed in 34 % (20/58, 18 patients presenting tumoral lesions and 2 with osteoporotic fractures) of the patients (Fig. 4). Almost half of the patients had pre-procedure walking limitation (25/58). At the 1-month clinical follow-up, 80 % (20/25) experienced improvement, 16 % (4/25) remained unchanged and 4 % (1/25) referred to worsening (Fig. 5).
Statistically significant differences were observed between pre- and post-PSP mean VAS scores (Student t-test, P values < 0.05).
Statistically significant lower pain relief was obtained in patients with lesions that presented posterior wall/cortical disruption than in patients with not (VAS ≤ 2 vs VAS > 2, P value < 0.01). No statistically significant difference in terms of functional outcome was however observed between these groups of patients (P = 0.35).
No statistically significant difference in terms of pain relief, functional status and decrease in analgesic drug consumption was observed between patients with insufficiency sacral fracture and those with a tumour (P = 0.50, 0.48 and 0.89, respectively), between patients with unilateral and bilateral sacral lesion (P = 0.29 and 0.28, respectively) or between patients presenting lytic, or mixed/osteoblastic lesions (P = 0.08 and 0.17, respectively).
No procedure-related deaths were recorded. Minor complications were observed in 2/58 patients (3.4 %) (Table 5). These two patients experienced transient neurological deficit due to local extravasation of PMMA, which resolved under anti-inflammatory medication. Two other patients (2/58; 3.4 %) experienced a major complication: cement leakages were reported within the vertebral canal and S1 foramen respectively (Fig. 6) that subsequently required surgical decompression for symptomatic relief of the radicular pain. Both patients had a good outcome with no permanent deficit. Major complication rate was higher in the tumour group than in the osteoporotic group (3.4 % vs 0 %). However, this difference was not statistically significant (Fisher’s exact test, P = 1). Complication rates of patients with posterior wall/cortical bone disruption and those without such imaging findings were not statistically different (P = 0.16). A statistically significant complication rate was found in the group harbouring lytic lesions (20 %, 5/30) versus mixed/osteoblastic ones (0 %, 0/28) (Fisher’s exact test, P = 0.046). Biopsy results were assessed in 39 patients (5 osteoporotic fractures and 34 tumours) with malignant cells found in 31 % (12/39), absence of malignant cells in 59 % (23/39) and samples from 10 % of the patients (4/39) were considered insufficient or unsuitable by the pathologist for evaluation (1 insufficiency fracture and 4 tumours). No malignant cells were found in presumed osteoporotic lesions.
A 80-year-old man with a painful osteolytic lesion of the S1 segment of the sacrum from an adenocarcinoma of the rectum. a Unenhanced axial CT, bone windowing showing an osteolytic lesion of the upper segment of the sacrum with anterior extension (arrows). b, c Plain X-rays after PMMA bone cement injection in AP (b) and lateral (c) projections. Satisfactory filling of the lesion is seen. However, a tubular shape image is seen at the level of the left S1 sacral foramen (b, arrow), with a posterosuperior orientation on lateral projection (c, arrow) suggestive of a cement leakage into the left S1–S2 sacral foramen. d, e Post-PSP CT, bone windowing; (d) axial slice, (e) coronal reconstruction. Cement leakage into the left S1–S2 sacral foramen is seen (d, arrow and e, arrowheads). Contact between the cement leakage and the S1 nerve root is seen (d, arrow). The patient underwent surgical removal of the bone cement fragment and clinically completely recovered
Discussion
Spinal tumours and insufficiency fractures due to osteoporosis are important causes of severe lower back pain, leading to chronic disability and a devastating impact on quality of life [13, 14].
It is estimated that osteoporosis affects approximately 10 million people, causing more than 700,000 fractures annually only in the United States [15] and spinal metastasis develop in 5–10 % of all cancer patients during the course of their disorder, predominantly in the thoracic region, followed by the lumbar spine and lumbosacral junction [16].
Currently, the mainstay of management for sacral metastatic tumours is palliation: bed rest, medical analgesia, radiotherapy, chemotherapy and endovascular embolisation in cases of highly vascular tumours [2, 16]. Surgical correction is associated with prolonged postoperative recovery time with high mortality rates [17] and is mainly indicated for locally advanced tumours that compromise spinal stability and neurological status [16].
Since the introduction of PV by Galibert et al. in 1987 [18], its use has been gradually increased as a treatment for osteolytic pathological fractures and osteoporotic vertebral compression fractures, and from early 2000 this technique has extended its application by many researchers, not only for cylinder-shaped vertebral bodies but also for shield-shaped sacral bones [19].
Some authors studied the mechanical and analgesic effects of PMMA injection in vertebral osteoporotic fractures and metastatic lesions, demonstrating mechanical stabilisation, which prevents painful micromotion and restores pelvic strength [20] and an analgesic effect in pathological lesions due to its thermal property [2, 21].
In the past years, several case reports and series have been published discussing PSP as an alternative to traditional medical therapy for sacral insufficiency fractures [8, 19, 22–25]. Our study showed the effectiveness of PSP in pain relief and functional recovery. Indeed, 84 % of the patients experienced pain reduction, whereas 80 % presented an improvement of their ability to walk. Average VAS decrease was 3.6 (from 5.3 to 1.7).
Most of the previously published series seem to agree that PSP is associated with durable pain relief and good rehabilitation, and with low complication rates [2, 7, 9, 12, 19, 24, 26, 27]. Bayley et al. [28]. reviewed 15 papers about the subject, with same conclusions Frey et al. [27], in a prospective multicentre study, one of the largest series about osteoporotic fractures treated with PSP (52 patients), showed a decrease in the mean VAS score from 8.1 pre-procedure to 0.8 at 52 weeks’ follow-up. They reported one case of transient S1 radiculitis that resolved completely with foraminal epidural steroid injection (complication rate, 2 %).
Even though the effectiveness of this technique has been demonstrated for osteoporotic fractures, the use of PSP for painful sacral tumours has been poorly reported, probably because tumours are more challenging to treat. Only eight studies reported the effectiveness of PSP for tumour sacral lesions [2, 29–35]. A recent multicentre study by Kortman et al. [35] assessed the efficacy and safety of PSP in 243 patients, in which only 39 patients had symptomatic sacral tumours. These authors demonstrated positive results (mean VAS ranging from 8.9 to 2.6), reporting no complications in this group of patients. In our study, 49 patients presented with sacral tumours, which to the best of our knowledge makes our series the largest in the literature on tumours treated with PSP. Results in term of pain relief were not statistically different from those obtained for osteoporotic sacral fractures. However, in our series, the complication rate was higher in the tumour group (8 %, 4/49) than in the group of insufficiency fractures (0 %, 0/9). Nevertheless, this difference was not statistically significant. We also observed that patients with more aggressive tumour lesions, with posterior wall and cortical disruption, had statistically significant less pain relief compared with lesions limited to the sacral bone. Although this could be expected, it should be reminded when dealing with this type of lesions.
Sacroplasty is technically similar to vertebroplasty; however, there are a few differences between the two techniques that need to be noted. Firstly, it can be challenging to know when the tip of the needle has reached the inner cortical margin of the sacrum and has not traversed into the pelvic side. Secondly, it may be difficult to see the sacral foramina when using only fluoroscopic guidance, but this can be overcome by placement of needles in the sacral foramina before cement injection.
Potential complications of PSP include venous cement leakage, which may migrate into the pulmonary circulation (and lead to pulmonary embolism), infection and leakage into the neural foramina or the spinal canal [27]. We experienced two major complications (3.4 %), due to cement extravasation that required surgical decompression in patients with metastatic lesions. It is noteworthy that after surgical decompression, none of the patients had residual neurological deficit. In the literature, complication rates range from 0 to 20 %, depending on the total number of patients, with most of the papers reporting one or a maximum of two patients with complications [1, 7, 27, 28, 35]. This slightly higher number of complications in our study (four patients, two minor and two major complications) may be because most of our patients had tumours; some of them were complex lesions, with posterior wall and cortical bone disruption. Interestingly, in our study, contrary to previously published series on vertebroplasty in which the complication rate was higher in sclerotic lesions [36], PSP-related complications occurred more frequently in osteolytic lesions than in blastic or mixed lesions. We had a relatively high rate of repeated procedures (16 %) compared with other series [1, 37, 38], but again this can be due to our larger series of tumoral complex lesions. We think that this should be discussed with all patients prior to the procedure.
In our series, all the PSPs were performed under fluoroscopic guidance. Even if this technique presents some difficulties for the positioning of the bone needles in the sacral bone and requires experience, it allows for better visualisation of the progression of the cement within the lesion and for earlier depiction of cement leakage. Case reports have been published on the interest in using CT guidance for PSP, especially for a more accurate positioning of the bone needles [37]. However, despite its helpfulness for the bone needles’ setting, CT guidance provides poor visualisation of the cement injection, without the possibility of having continuous fluoroscopy. In order to overcome the limitations of both the sole fluoroscopic guidance and the sole CT guidance, some authors have proposed the combination of CT and fluoroscopic guidance during PSP for better visualisation of bone landmarks and to monitor live cement extravasation during injection [1, 2, 28]. However, this combined technique is difficult to organise in daily practice. Improvements in CT fluoroscopy may be a solution to overcome these technical limitations, but it delivers a higher X-ray dose to the patient. Finally, the recently developed hybrid angiographic suite, which combines C-arm flat panel and CT in the same room, can be an interesting tool in increasing the safety of PSP. Indeed, in these hybrid angiographic suites, the needle(s) can be positioned under CT guidance, and then, by a simple translation of the table towards the C-arm flat panel without any mobilisation of the patient, the PMMA injection can be performed under fluoroscopic guidance, allowing for live visualisation of the progression of the cement.
In conclusion, PSP is a safe and effective technique in terms of pain relief and functional outcome for both sacral osteoporotic fractures and tumours, with an acceptable complication rate. Even if more challenging to treat by PSP, tumour bone lesions are not statistically associated with a higher complication rate. However, the treatment of osteolytic lesions is more frequently associated with neurological complications.
Abbreviations
- PSP:
-
Percutaneous sacroplasty
- PV:
-
Percutaneous vertebroplasty
- PMMA:
-
Polymethyl methacrylate
References
Strub WM, Hoffmann M, Ernst RJ et al (2007) Sacroplasty by CT and fluoroscopic guidance: is the procedure right for your patient? AJNR Am J Neuroradiol 28:38–41
Zhang J, Wu CG, Gu YF et al (2008) Percutaneous sacroplasty for sacral metastatic tumours under fluoroscopic guidance only. Korean J Radiol 9:572–576
Klazen CAH, Lohle PNM, de Vries J et al (2010) Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 376:1085–1092
Saliou G, Kocheida EM, Lehmann P et al (2010) Percutaneous vertebroplasty for pain management in malignant fractures of the spine with epidural involvement. Radiology 254:882–890
Mailli L, Filippiadis DK, Brountzos EN et al (2013) Clinical Outcome and Safety of Multilevel Vertebroplasty: Clinical Experience and Results. Cardiovasc Intervent Radiol 36:183–191
Masala S, Mastrangeli R, Petrella MC et al (2009) Percutaneous vertebroplasty in 1,253 levels: results and long-term effectiveness in a single centre. Eur Radiol 19:165–171
Whitlow CT, Mussat-Whitlow BJ, Mattern CWT et al (2007) Sacroplasty versus vertebroplasty: comparable clinical outcomes for the treatment of fracture-related pain. AJNR Am J Neuroradiol 28:1266–1270
Trouvin A-P, Alcaix D, Somon T et al (2012) Analgesic effect of sacroplasty in osteoporotic sacral fractures: a study of six cases. Joint Bone Spine 79:500–503
Kang S-S, Kim H-C, Park J-H et al (2009) Three-dimensional C-arm computed tomography-guided sacroplasty for the treatment of sacral body fracture. Spine 34:309–311
Naderi S, Ilaslan H, Aslan A et al (2010) Sacroplasty: report of three cases. Turk Neurosurg 20:418–422
Kang SE, Lee JW, Kim JH et al (2011) Percutaneous sacroplasty with the use of C-arm flat-panel detector CT: technical feasibility and clinical outcome. Skeletal Radiol 40:453–460
Jayaraman MV, Chang H, Ahn SH (2009) An easily identifiable anatomic landmark for fluoroscopically guided sacroplasty: anatomic description and validation with treatment in 13 patients. AJNR Am J Neuroradiol 30:1070–1073
Ehrlich GE (2003) Low back pain. Bull World Health Organ 81:671–676
Katsanos K, Sabharwal T, Adam A (2010) Percutaneous cementoplasty. Semin Intervent Radiol 27:137–147
Riggs BL, Melton LJ 3rd (1995) The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone 17:505S–511S
Quraishi NA, Giannoulis KE, Edwards KL et al (2012) Management of metastatic sacral tumours. Eur Spine J 21:1984–1993
Pascal-Moussellard H, Broc G, Pointillart V et al. Complications of vertebral metastasis surgery. Eur Spine J 7:438–444
Galibert P, Deramond H, Rosat P et al (1987) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 33:166–168
Choi K-M, Song J-H, Ahn S-K et al (2010) Therapeutic considerations of percutaneous sacroplasty for the sacral insufficiency fracture. J Korean Neurosurg Soc 47:58–63
Kayanja M, Tsai E, Yamashita T et al (2006) The Biomechanics of Insufficiency Fractures and Augmentation of the Sacrum. Spine J 6:96S
Belkoff SM, Molloy S (2003) Temperature measurement during polymerization of polymethylmethacrylate cement used for vertebroplasty. Spine 28:1555–1559
Vilmarsson V, Schnabel K, Wikholm G (2010) Osteoporotic sacral fracture—a painful condition, easy to miss. Sacroplasty a new treatment with quick pain relief. Lakartidningen 107:251–254
Lyders EM, Whitlow CT, Baker MD et al (2010) Imaging and treatment of sacral insufficiency fractures. AJNR Am J Neuroradiol 31:201–210
Ehara S (2006) Percutaneous sacroplasty for osteoporotic insufficiency fractures. AJR Am J Roentgenol 186:580, author reply 580–581
Garant M (2002) Sacroplasty: a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol 13:1265–1267
Cho CH, Mathis JM, Ortiz O (2010) Sacral fractures and sacroplasty. Neuroimaging Clin N Am 20:179–186
Frey ME, Depalma MJ, Cifu DX et al (2008) Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: a prospective, multicenter, observational pilot study. Spine J 8:367–373
Bayley E, Srinivas S, Boszczyk BM (2009) Clinical outcomes of sacroplasty in sacral insufficiency fractures: a review of the literature. Eur Spine J 18:1266–1271
Nebreda C, Vallejo R, Aliaga L et al (2011) Percutaneous sacroplasty and sacroiliac joint cementation under fluoroscopic guidance for lower back pain related to sacral metastatic tumours with sacroiliac joint invasion. Pain Pract 11:564–569
Wee B, Shimal A, Stirling AJ et al (2008) CT-guided sacroplasty in advanced sacral destruction secondary to tumour infiltration. Clin Radiol 63:906–912
Valencia-Anguita J, Juliá-Narváez M, Rodríguez-Burgos F et al (2007) Percutaneous sacroplasty for relieving pain caused by sacral metastases. Neurocirugia (Astur) 18:247–249
Uemura A, Matsusako M, Numaguchi Y et al (2005) Percutaneous sacroplasty for hemorrhagic metastases from hepatocellular carcinoma. AJNR Am J Neuroradiol 26:493–495
Sun G, Jin P, Li M et al. (2011) Three-dimensional C-arm computed tomography reformation combined with fluoroscopic-guided sacroplasty for sacral metastases. Support Care Cancer. Available at: http://www.ncbi.nlm.nih.gov/pubmed/22081116
Basile A, Tsetis D, Cavalli M et al (2010) Sacroplasty for local or massive localization of multiple myeloma. Cardiovasc Intervent Radiol 33:1270–1277
Kortman K, Ortiz O, Miller T et al (2012) Multicenter study to assess the efficacy and safety of sacroplasty in patients with osteoporotic sacral insufficiency fractures or pathologic sacral lesions. J Neurointervent Surg. doi:10.1136/neurintsurg-2012-010347
Laredo J-D, Hamze B (2005) Complications of percutaneous vertebroplasty and their prevention. Semin Ultrasound CT MRI 26:65–80
Brook AL, Mirsky DM, Bello JA (2005) Computerized tomography guided sacroplasty: a practical treatment for sacral insufficiency fracture: case report. Spine 30:E450–E454
Gjertsen O, Schellhorn T, Nakstad PH (2008) Fluoroscopy-guided sacroplasty: special focus on preoperative planning from three-dimensional computed tomography. Acta Radiol 49:1042–1048
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pereira, L.P., Clarençon, F., Cormier, É. et al. Safety and effectiveness of percutaneous sacroplasty: a single-centre experience in 58 consecutive patients with tumours or osteoporotic insufficient fractures treated under fluoroscopic guidance. Eur Radiol 23, 2764–2772 (2013). https://doi.org/10.1007/s00330-013-2881-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2881-3