Abstract
The purpose of this study was to assess the efficacy of cementoplasty in the treatment of sacral multiple myelomas. We retrospectively reviewed the records of eight patients (four women and four men; age range 47–68 years; mean age 57.8) who underwent cementoplasty for painful osteolytic localization of multiple myeloma between April 2007 and May 2009. The patients had difficulty walking because of increasing pain. Six patients had persistent pain despite other cementoplasties for vertebral and femoral localization, whereas two patients referred at the time of diagnosis had only sacral lesions. The clinical indication for treatment was (1) a pain intensity score ≥5 on visual analogue scale (VAS) and (2) pain totally or partially refractory to analgesic treatment in patients with a life expectancy >3 months. Technical planning was based on computed tomography and/or magnetic resonance imaging. Six patients had previously undergone radiotherapy or chemotherapy and were receiving varying doses of analgesics, whereas sacroplasty represented the first treatment for two patients. Five patients had monolateral local involvement, and the other patients had massive involvement of the sacrum; Technical success was achieved in all cases. We had only one small and asymptomatic foraminal leak. All patients experienced improvement in symptoms after the procedure, as demonstrated by improved VAS scores and performance status (PS) and decreased analgesic dose constant during follow-up. In our experience, percutaneous stabilization can be used effectively and safely in patients with focal or extensive involvement of the sacrum by multiple myeloma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Vertebroplasty is largely being used for metastatic lesions from several neoplasms and from multiple myeloma (MM); however, literature data regarding patients with painful sacral metastases are limited. Furthermore, there is no consensus on the indications or degree of sacral involvement for percutaneous treatment. Sacroplasty was initially used to stabilize sacral-insufficiency fractures [1–3].
Even if the exact mechanism by which sacroplasty causes pain relief is unknown, two theories have been proposed: (1) stabilization obtained with cement injection decreases movement at the fracture site and thus pain by augmenting the strength and stiffness of the sacrum; and (2) the analgesic effect of osteoplasty in vertebral metastases results from reinforcing the trabecular bone, which leads to stabilization of the vertebral body [4], thus obviating deformation of the periostium [5]. This mechanism has been suggested for other skeletal bone, including the sacrum.
Materials and Methods
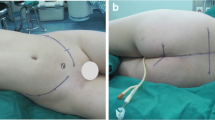
We retrospectively reviewed the records of eight patients (four women, four men; age range 47–68 years; mean age 57.8) who underwent osteoplasty for painful osteolytic localization of MM between April 2007 and May 2009. Patient characteristics are listed in Table 1. Five patients had monolateral lesions (Fig. 1), in particular three of these had small painful lesions (Figs. 2, 3, 4); the other patients had massive involvement of the sacrum (Figs. 5, 6). After evaluating the various treatment options and possible contraindications, the indication for treatment was established by a team of hematologists, radiotherapists, surgeons, and radiologists on the basis of a detailed correlation between clinical history, particular current symptoms (PS), and CT or MRI findings. All patients had difficulty walking because of increasing pain, and patient no. 8 (Fig. 3), also affected by an iliac bone lesion, could not even get out of bed. Six patients had persistent pain despite having had other osteoplasties for vertebral and femur involvement, whereas two patients referred at the time of diagnosis had a sacral lesion only (Table 1).
Patient no. 4. Coronal reformatted CT images showing a focal area of osteolysis with involvement of ipsilateral foramina that was treated by (a) radiofrequency ablation needle (white arrow) coaxially inserted through a (b) vertebroplasty needle (black arrow). c and d Postprocedural coronal and sagittal reformatted CT images
Patient no. 8. a and b Sagittal reformatted CT images showing a focal area of osteolysis in the left sacrum (arrow) with another osteolitic lesion in controlateral iliac bone (asterisk) that was treated by (c and d) insertion of two vertebroplasty needles (arrows). Postprocedural fluoroscopic (e) and CT images (f–h)
The clinical indication for treatment was a pain intensity score ≥5 or higher on VAS and pain totally or partially refractory to analgesic treatment in patients with a life expectancy >3 months. Technical planning was based on computed tomography (CT) and/or magnetic resonance imaging (MRI). Seven patients had previously undergone radiotherapy or chemotherapy and were receiving varying doses of analgesics (Table 2), whereas for patient nos. 4 and 5, osteoplasty, performed after radiofrequency ablation (RFA) in the former case, represented the first treatment. In that case we used an electrode with 1-cm active tip to decrease the risk of neurologic damage due to the cortical invasion operated by the neoplasm. Written informed consent to treatment in this study was obtained from all patients and their families. All procedures were performed with the patient under local anaesthesia or moderate sedation. Osteoplasty was performed with 11- or 13-gauge bevel-tip needles 15 cm in length plus cement (polymethylmethacrylate; Cardinal Health, France). All procedures were carried out under fluoroscopic guidance in the angiographic suite. CT (Brilliance 16; Philips, The Netherlands) was used in all cases for immediate postprocedural evaluation. A subjective assessment of perceived pain intensity was obtained through analysis of VAS scores (on which 0 indicates total absence of pain and 10 indicates the worst pain ever experienced), which were recorded before and immediately after treatment and during the follow-up period (range 3–27 months; mean 12.5) by ambulatory visits or telephone interviews (Table 3). Imaging follow-up was carried out according to the standard follow-up schedule for the tumour and was anticipated in the event of worsening of pain. Technical success was defined as the ability to access the lesion using the approach established at previous CT and MR imaging. Clinical success was defined as a quantitative decrease in analgesic medication and improved VAS score and PS compared with baseline. Complications were classified, based on the standards of the Society of Interventional Radiology, into major and minor according to length of hospitalization after the procedure, where the lowest grade of major complication involved therapy and hospitalization for <48 h.
Results
Technical success was achieved in all cases. A total amount of cement, ranging between 3 and 4 cc for focal monolateral procedures and 8–10 cc for bilateral interventions, was injected. We had only a small and asymptomatic foraminal leak in patient no. 1 (Fig. 6). All patients experienced improvement in symptoms after the procedure as demonstrated by improved VAS scores and PS and decreased analgesic doses (Tables 2, 3). All patients were followed-up for a period ranging from 3 to 27 months (mean 12.5). VAS scores in all patients were significantly lower, between 3 and 8 points (mean 5) within 24 h of the procedure, and they remained substantially unchanged throughout the follow-up.
Discussion
Osteoplasty currently represents one of the standard treatments of vertebral neoplasms, and in recent years its use has been proposed for extraspinal lesions on the basis of the same pathologic mechanism (i.e, activation of pain nerves of the periosteum). Even if vertebroplasty is widely used for localization of MM, reported literature on the use of percutaneous stabilization in extraspinal lesions in such patients is lacking. If we consider three more recent literature series on percutaneous treatment of extraspinal bone neoplasms published in 2008 by Anselmetti et al. [6] (50 patients), by Hoffman et al. [7] (22 patients), and by Basile et al. [8] (13 patients), the investigators reported, respectively, 1, 4, and 5 cases of MM. The localization of MM to the sacrum is rare, as is local lesion or massive involvement. To our knowledge, only 17 cases of sacroplasty for bone metastases have been published up until now in the English literature [6–14] (Table 4). Of these, only two cases of sacroplasty for MM have been published. The first case was published by Butler et al. [12] in a patient with sacral fracture secondary to bilateral MM involvement. The investigators performed a double procedure on the right sacrum because cement distribution during the initial therapy was insufficient; however, they did not specify whether or not the patient had clinical improvement after the first procedure. The second case was published by Wee et al. [14] in a patient with extensive infiltration of the S1 segment, who had already been treated with surgical intervention for a large destructive mass in the S1 and S2 segments, extending to involve the L5 vertebral body and obliterating the sacral thecal sac.
In the largest reported series of extraspinal bone lesions treated percutaneously by cementoplasty alone or after RF ablation, published by Anselmetti et al. [6], the investigators performed eight sacroplasties for seven monolateral and one bilateral metastases without using previous RF ablation, with good results in terms of pain relief and decreased analgesic therapy.
In our patients, sacral lesions were discovered at the exordius of the disease or as a late involvement, and they were treated despite any sign of fracture. All patients experienced almost immediate and dramatic pain relief after osteoplasty for the duration of follow-up, and they were able to leave the hospital few days after the procedure and returned to home care.
In particular, patient no. 4 was treated at the exordius first with percutaneous techniques instead of standard treatment (chemotherapy and radiotherapy), and this represents a new indication. We performed radiofrequency ablation before osteoplasty because there was a large neoplasm involving the bone; we use a 1-cm active-tip electrode to decrease the risk of neurologic damage. In our institution, according to the protocol implemented in collaboration with haematologists, we prefer to perform immediate percutaneous treatment in highly symptomatic patients with MM or at risk of fracture who need immediate therapy and who cannot wait for radiotherapy for those reasons. Frequently we treat patients with proximal long-axis bone lesions, such as the femoral neck, in this way. These patients would otherwise undergo surgical treatment or radiotherapy and have to wait weeks before starting chemotherapy. The important concept of this approach is that such patients undergo a “bridge” percutaneous stabilization, which allows immediate pain relief, decreased risk of fracture, and immediate start up of chemotherapy.
In conclusion, based on our knowledge of English literature, this is the largest series published this far of patients with MM of the sacrum treated by sacroplasty. On the basis of our experience, percutaneous stabilization can be used effectively and safely in patients with focal or extensive involvement of sacrum; however, more patients and longer follow-up are necessary to confirm our experience.
References
Frey ME, DePalma MJ, Cifu DX et al (2007) Efficacy and safety of percutaneous sacroplasty for painful osteoporotic sacral insufficiency fractures: a prospective, multicenter trial. Spine 32:1635–1640
Garant M (2002) Sacroplasty: a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol 13:1265–1267
Pommersheim W, Huang-Hellinger F, Baker M et al (2003) Sacroplasty: a treatment for sacral insufficiency fractures. AJNR Am J Neuroradiol 24:1003–1071
Brien JP, Sims JT, Evans AJ (2000) Vertebroplasty in patients with severe vertebral compression fractures: a technical report. AJNR Am J Neuroradiol 21:1555–15587
Amar AP, Larsen DW, Esnaashari N et al (2001) Percutaneous transpedicular PMMA vertebroplasty for the treatment of spinal compression fractures. Neurosurgery 49(5):1105–1115
Anselmetti GC, Manca A, Ortega C et al (2008) Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Cardiovasc Intervent Radiol 31:1165–1173
Hoffmann RT, Jakobs TF, Trumm C et al (2008) Radiofrequency ablation in combination with osteoplasty in the treatment of painful metastatic bone disease. J Vasc Interv Radiol 19:419–425
Basile A, Giuliano G, Scuderi V et al (2008) Cementoplasty in the management of painful extraspinal bone metastases: our experience. Radiol Med 113:1018–1028
Dehdashti AR, Martin JB, Jean B et al (2000) PMMA cementoplasty in symptomatic metastatic lesions of the S1 vertebral body. Cardiovasc Intervent Radiol 23:235–237
Hierholzer J, Anselmetti G, Fuchs H et al (2003) Percutaneous osteoplasty as a treatment for painful malignant bone lesions of the pelvis and femur. J Vasc Interv Radiol 14:773–777
Uemura A, Matsusako M, Numaguchi Y et al (2005) Percutaneous sacroplasty for haemorrhagic metastases for hepatocellular carcinoma. AJNR Am J Neuroradiol 26:493–495
Butler CL, Given CA II, Michel SJ et al (2005) Percutaneous sacroplasty for the treatment of sacral insufficiency fractures. AJR Am J Roentgenol 184:195
Masala S, Konda D, Massari F et al (2006) Sacroplasty and iliac osteoplasty under combined CT and fluoroscopic guidance. Spine 31:E667–E669
Wee B, Shimal A, Stirling AJ, James SLJ (2008) CT-guided sacroplasty in advanced sacral destruction secondary to tumour infiltration. Clin Radiol 63:906–912
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Basile, A., Tsetis, D., Cavalli, M. et al. Sacroplasty for Local or Massive Localization of Multiple Myeloma. Cardiovasc Intervent Radiol 33, 1270–1277 (2010). https://doi.org/10.1007/s00270-009-9761-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-009-9761-x