Abstract
Purposes
We sought to verify the efficacy and safety of RFA in spinal OO and osteoblastomas (OB) (Enneking Stage 2, S2).
Methods
We retrospectively reviewed patients treated in our hospital. Surgical resection was indicated for Enneking Stage 3 OB. RFA indications for spinal OO and OB (S2) were no neurological deficits, complete bone cortex around the lesion on computed tomography (CT), and cerebrospinal fluid between a lesion and the spinal cord/nerve root on magnetic resonance imaging. Abundant cerebrospinal fluid (more than 1.0 mm) between the lesion and nerve root/spinal cord was preferred to prevent neurological damage by heat. Otherwise, surgery was recommended. The minimum follow-up was 24 months.
Results
Ten patients were treated with CT-guided percutaneous RFA, including three with OB and seven with OO. No patients had neurological deficits or scoliosis. In OO patients, the average visual analog scale (VAS) scores were 7.6/10 (range 6–10) before RFA. In OB cases, the VAS scores were 8, 7, and 9 before RFA. Nine patients had a one-stage biopsy and then RFA, and one patient had a two-stage procedure (biopsy before RFA). The average RFA time for OO was 10 min (range 4–12). In the three OB cases, the RFA time was 12, 12, and 24 min. The time of the whole produce was 98 min (range 65–130 min). All 10 patients were followed-up. The average follow-up time of OO was 46.6 months (range 24–66). Six patients were free of pain, except one who suffered occasional pain with VAS 2/10. The three OB cases were free of pain at 24, 26, and 26 months.
Conclusion
CT-guided percutaneous RFA is a safe and effective treatment for spinal OO and S2 OB, especially in lesions with no neurological deficits and intact cortical bone. Cerebrospinal fluid around the lesion is an appropriate indication for percutaneous RFA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoid-producing primary bone tumors are rare lesions, with the most prevalent being osteoid osteomas (OO) and osteoblastomas (OB). Less than 10% of these lesions are located in the spine [1]. A particular challenge is OB’s histologic resemblance to OO. In the current study, we used tumor size of less than 1.5 cm to indicate an OO and anything larger as a marker for OB [2, 3]. It has been reported that OO may progress to OB, which is thought to be rare [4]. Most OO lesions and some OB lesions are active (Enneking stage 2, S2), and other OB lesions are aggressive (Enneking stage 3, S3) [5,6,7].
Nonsteroidal anti-inflammatory drugs (NSAIDs) are an optional conservative treatment for OO. The historical standard treatment has been surgical resection [2, 8, 9]. Potential surgical complications have made percutaneous radiofrequency ablation (RFA) an attractive alternative due to less bone destruction and shorter hospitalization, with equal safety and efficacy [10,11,12,13,14]. Intralesional curettage is recommended for S2 OB [2, 6]. To the best of our knowledge, only two spine OB cases treated by RFA have been reported in the English-language literature [13, 15]. In this retrospective study, we evaluated the safety and efficacy of RFA for spine OO and OB (S2) cases treated in our hospital.
Materials and methods
The hypothesis we hold is that RFA is efficient and safe in spinal OO and osteoblastomas (OB) (Enneking Stage 2, S2). The medical records of patients who underwent treatment or consultation with the spinal surgery team in our hospital between November 2007 and May 2014 for OO or OB were retrospectively reviewed. A retrospective review of hospital charts, operating room reports, office charts, pathology reports, and radiographs was performed. The data collected included the patient’s age, gender, symptoms, neurological function, radiological features, pathology, details of RFA, outcome, and complications of treatment. The modified Frankel Grade and visual analog scale (VAS) were used to evaluate patients’ neurological function and pain. The minimum follow-up was 24 months. Cases with surgical treatment and/or without definitive pathological diagnosis were excluded from this study. This study was approved by the Ethical Committee of our hospital and conducted according to the principles of Declaration of Helsinki. Because this was a retrospective review, informed consent was waived.
Patient cohort
Twenty-three spinal OO and 39 spinal OB cases (including four S2 and 35 S3) were treated in our department. Among these 62 cases, 10 were treated with computed tomography (CT)-guided percutaneous RFA, including three patients with OB (all male; 9, 13, and 21 years old) and seven with OO (one female, six males; median age 30.1 years old; range 16–55).
Imaging and biopsy
We routinely performed posterior-anterior and lateral spinal radiography, CT, and magnetic resonance imaging (MRI). For patients with typical radiographic results of OO and OB (Stage 2), we performed percutaneous CT-guided trocar biopsy and then percutaneous RFA in one stage. Typical lesions have a distinct radiolucent, round, or oval nidus with variable internal calcification and sclerotic rim seen on fine-section CT. For patients with untypical radiographic features, a bone scan and percutaneous CT-guided trocar biopsy were indicated. Once the pathology was confirmed, percutaneous RFA was the first treatment option.
Treatment protocol
Surgical resection was indicated for S3 OB. We have been performing RFA since 2011. The indications for RFA for spinal OO and OB (S2) were no neurological deficits, the existence of complete bone cortex around the lesion on CT, and the existence of cerebrospinal fluid between the lesion and the spinal cord or nerve root seen on MRI. If there was abundant cerebrolspinal fluid between the lesion and nerve root or spinal cord (more than 1.0 mm), the heat usually did not damage them. Otherwise, surgery was recommended. The benefits and risks of RFA and the surgical alternatives were discussed with the patients or their parents if the patient was a child.
In cases with typical radiological findings, we performed one-stage biopsy and then RFA. If the radiological findings were not diagnostic, biopsy was carried out first, followed by RFA several days later after achieving a definitive pathological diagnosis. The patients underwent percutaneous CT-guided biopsy and RFA under local anesthesia with lidocaine and intravenous conscious sedation with remifentanil and propofol. General anesthesia was indicated if the patient was a child or could not tolerate local pain during RFA. Local anesthesia and moderate sedation were preferred, especially for lesions close to the nerve root or dural sac, which might be endangered during RFA. If the patient complained of aggravation of neurological symptoms during RFA, surgery was indicated.
Patients were placed in the prone position or lateral recumbent position according to the tumor’s location. The RFA procedure was performed with a multi-detector CT, and multiplanar reconstructions were used to guide the coaxial bone biopsy system and define the optimal path(s) to cover the whole nidus.
The entry point and trocar trajectory were planned on CT scan with skin markers. After the skin entry point was made with a 0.5 cm stab incision, the trocar (T-LokTM, Angiotech, Vancouver, BC) was inserted into the cortex of the lesion, which was additionally infiltrated with local anesthetics. CT was performed again to confirm the appropriate tip position and the trocar trajectory. The nidus was then penetrated with the penetration cannula. After achieving an ideal specimen, we replaced the puncture needle with an RFA needle through the trocar. The needle was usually inserted into the lesions along its longitudinal axis to its outer rims, and its tip sat in the sclerotic rim, which was confirmed by CT. The length of the ablation electrode needle was chosen according to the size of the lesion with two different lengths of the active tip (1.0 cm and 2.0 cm). RFA was performed using a Cool-tip RFA system (Valleylab, Covidien, Mansfield, MA, USA). The RFA active tip was heated to 90 °C for 12 min, and 0.5–1.0 cm around the tip (the radius from the probe tip) of the RFA needle was ablated. In case of OB or oval-shaped OO, if the needle could not be placed along the lesion’s longitudinal axis, a single RF ablation might not have been sufficient, and repeated RFA would have been performed immediately (case 3, Fig. 3). If the patients had intolerable discomfort, the RFA might be intermittent, or the procedure might change to general anesthesia.
If the lesion had an intact cortical bone, RFA could be performed safely, since the cortex could be an ideal insulator between the lesion and the thecal sac or spinal nerves. In case of a “missing” cortical layer (too thin to observe on CT, but could still be observed under a microscope) with regard to the neuroforamen or the spinal canal, a sensor might be needed to measure the temperature next to the ablation area. In the case of OB or eclipse OO, two tips were recommended to cover the volume of the whole nidus. First, the access trajectory was planned in all dimensions with regard to the shape of the nidus. RFA was then repeated with different electrode positions to increase the ablation volume and efficacy.
Once RFA was finished, the trocar was pulled out with a needle. Patients, especially their neurological symptoms, were closely monitored during the procedure. They were usually discharged within 48 h after RFA. NSAIDs were administered for only a few days after the procedure. All the cases were performed by senior surgeons.
Follow-up
We obtained X-ray and CT at 3, 6, 12, and 24 months after the index procedure, and then every two years thereafter. VAS and neurological deficits were recorded. Long-term success was assessed using VAS regarding the effect of RFA on the severity of night pain and pain throughout the day. If the patient displayed symptoms indicative of local recurrence, immediate CT and MRI scans were suggested. If suspected recurrence could be neither confirmed nor ruled out, bone scintigraphy was indicated. If a technetium bone scan confirmed intense radionucleotide uptake at the suspected lesion, repeated RFA was suggested.
Results
There were three S2 spinal OB cases and nine spinal OO cases underwent treatment in our hospital since we started RFA in 2011. All of the three OB cases underwent RFA. Two of the OO cases did not meet the indications for RFA after radiological evaluation because the lesions were too close to the neurological structures. Three OB cases and seven OO cases treated by RFA were reviewed.
In the three OB cases, the lesions involved the posterior arch of the atlas, C5 lamina, and T3 vertebral body. In the seven OO cases, the involved segments were cervical in three, thoracic in two, lumbar in one, and sacral vertebra in one. The lesion locations were odontoid process of C2 in one patient and the appendix in six.
No patients had neurological deficits or obvious scoliosis (Cobb angle greater than 10°). In addition, no one had a previous surgical intervention. In the seven OO patients, the average duration of symptoms before diagnosis was 21.7 months (range 8–30 months). The average VAS was 7.6/10 (range 6–10), and all patients suffered from night pain. Six OO patients took NSAIDs; five had partial relief and one had no effect. The durations of the symptoms of the three OB patients were 12, 12, and 60 months. Their VAS scores were 8, 7, and 9. Only one patient (case 3) suffered from night pain.
In nine cases with typical radiological findings, we performed one-stage biopsy and then RFA. But in one case (case 3), its radiological features were not diagnostic, so we did biopsy first, and RFA seven days later after achieving the pathological diagnosis. We used the exactly the same entry point and trajectory. We did not feel any difficulty during the second procedure.
The average RFA time for OO was 10 min (range 4–12 min). One patient (case 10) had RFA for only 4 min due to severe pain and refused general anesthesia. No complications were observed and their pain was relieved immediately after the procedure. Patients were discharged within 48 h after surgery, with the exception of one patient who was discharged three days after RFA due to persistent pain, which disappeared before discharge. In the three OB cases, the RFA time was 12, 12, and 24 min (case 3, two positions). The time of the whole produce was 98 min (range 65–150 min). No complications were observed. These patients were discharged at one, one, and two days after surgery. The pathological diagnoses of biopsy were OB or OO in all the patients (Figs. 1, 2, 3, 4).
Case 1, a 9-year-old boy had local pain for 12 months, and his VAS was 8/10. a, b Axial and sagittal CT showed a lytic and expansive lesion with dotted central calcification and with clear boundary in the center of the posterior arch of atlas. The inner cortex of C1 lamina seems blurry. The lesion’s maximum diameter was 22 mm. c, d Axial and sagittal MRI showed hybrid signal in lesion. e After the pathology was confirmed by CT guide biopsy, percutaneous radiofrequency ablation (RFA) was carried out under general anesthesia in lateral recumbent position along the longitudinal axis of the lesion. f CT at 6-month follow-up showed interval healing of the nidus. He was pain-free at 24 months after the index procedure
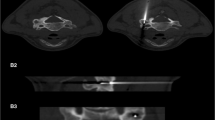
Case 2, a 24-year-old male had local pain for 5 years, and his VAS was 7/10. a, b Posterioanterior and lateral radiography showed sclerosis in C4–6, centered in the right lateral process of C5. c, d Axial and coronial CT showed a lesion in right lateral process of C5. The maximum diameter is 28 mm. e Axial T2-weighted MRI demonstrated decreased signal intensity. f Percutaneous RFA along the lesion’s longitudinal axis. g Axial CT at 6-month follow-up. h At 15-month follow-up, the patient was pain-free and axial CT showed interval healing of the lesion
Case3, a 13-year-old boy suffered back pain and night pain for 12 months. His VAS was 9/10. a Lateral radiography showed increased density on T3 (arrow). b Bone scan showed increased intake on T3. c–e Axial, coronal, and sagittal CT showed osteolytic bone destruction. The outer cortical bone of the right vertebral body became blurry with sclerosis on adjacent T2 and T3 vertebral bodies. f, g Axial and sagittal MRI. h CT-guided biopsy followed by percutaneous RFA. i, j At 6- and 12-month follow-up, the patient was pain-free and the lesion’s outer layer got scelerosis
Case 6, a 23-year-old man had local pain for 24 months, and his VAS was 8/10. a Axial CT showed a lytic and expansive lesion with central nidus and with surrounding sclerosis in left T7 pedicle, which was adjacent to nerve root. The maximum diameter is 10 mm. b Axial MRI. c, d Percutaneous radiofrequency ablation was carried out under local anesthesia in lateral recumbent position along the longitudinal axis of the lesion. e, f At 6- and 12-months follow-up, the patient was pain-free and axial CT showed sclerosis of the internal cortex of the lamina
All 10 patients were followed up. The average follow-up time of OO was 46.6 months (range 24–66 months). Six patients were free of pain, except one who suffered occasional pain, with a VAS score of 2/10 (case 9). The follow-up time in the three OB cases was 24, 26, and 26 months. All three were free of pain (Table 1).
Discussion
For spinal OO and OB in S2, the primary objective of treatment is pain relief. Surgical resection is effective for spinal OO [8, 9]. Boriani et al. [6] recommended intralesional curettage for spinal S2 OB and en bloc resection for S3, which is aggressive and has a higher recurrence rate. Complete excision of the lesion often involves extensive bony removal, which usually leads to local spinal instability. Extensive excision might endanger the spine cord or nerve root. While incomplete excision will lead to recurrence, the recurrence rates have been reported as high as 5 and 80% for OO and OB, respectively [9, 16].
RFA of spinal OO has chiefly been reported in small case series [10, 11, 13,14,15, 17,18,19], and the largest report included 24 cases. In our seven cases, percutaneous RFA showed good results in treating spinal OO with short hospitalization and no bone resection, which is consistent with another report [13]. Although percutaneous CT-guided radiofrequency ablation is accepted as the standard treatment for OO in the extremities, [2, 15] this technique is limited in spinal applications because of the risk of thermal damage to adjacent neurovascular structures. Radiofrequency heating at around 45 °C has been shown to be cytotoxic to the spinal cord and peripheral nerves, and the temperature effects of radiofrequency heating on the adjacent neural structures must be considered before the application of RFA [20]. In the OO lesions with missing cortex seen on CT, a thin layer of cortical bone could still be observed under a microscope, which could provide an insulation effect to prevent cytotoxic temperature elevations in the spinal canal. The rich epidural venous plexus and cerebrospinal fluid pulsations could provide additional local heat sinks [10].
OB lesions are often more expansive and have less sclerotic borders, and may have a more aggressive imaging and histological pattern when compared with OO. Given the fact that surgery is considered the gold standard, to the best of our knowledge, only two spinal OB cases treated with RFA have been reported in the English-language literature. In addition, RFA has often been used in the treatment of OB of the extremities [13, 15]. In our study, RFA was applied in three cases of spinal S2 OB lesions, with no recurrence at the final follow-up. In the case of spinal OB or oval-shaped OO, the lesions required longer RFA time, multiple needle positions, or needle along the longitudinal axis of the lesion.
The major complication of spine RFA is thermal damage to the spinal cord or nerve roots. It is generally believed that cortical bone has an insulation effect on heat transmission [20]. An ex vivo experiment by Greenberg et al. [21] showed that the insulation effect of cortical bone is better than that of cancellous bone, and with the increase in tumor size, the RFA temperature does not have an impact on the surrounding tissues. Yamane et al. [22] reported that 44 °C in the epidural space is the highest tolerable temperature for normal spinal cord function. Klass et al. [18] reported that a bolus of sterile water, injected through a spinal needle into the exit foramen and adjacent epidural space before ablation, is a safe and effective procedure when performing RFA, without potential neurological thermal injury. In addition, Rybak et al. [19] reported that special thermal protection techniques involving the epidural injection of gas or cooled fluid add safety, with the closest distance between the lesion and the neural element of 4.3 mm. Weber et al. [13] reported using thermal protection methods (gas injection) and found that even tumors adjacent to the nerve roots or the spinal canal can be treated safely with satisfactory clinical success.
On the other hand, Vanderschueren et al. [10] reported the heat sink effects of the spinal fluid and venous plexus, which may protect the nerve roots and spinal cord, and found that 2 mm is the minimum safe distance in RFA. This is also mentioned by Yamane et al. [22], who thought that RFA could be used with spinal fluid in cases of incomplete bone cortex around the tumor. We concur that the minimum safe distance is 2 mm; however, if there is cerebrospinal fluid between the lesion and spinal cord/nerve root, the minimum safe distance could be 1 mm. In this situation, we prefer moderate sedation with local anesthesia. If the patient complains of neurological symptom(s) during the procedure, RFA would be abandoned and surgical treatment would be indicated, although we have not faced this problem in our clinical practice.
The major limitations of our study are that it has a retrospective design, the number of cases is small, and the follow-up time was not long enough. Future prospective studies are needed to examine RFA in a larger group of patients with a longer period of follow-up.
CT-guided percutaneous RFA is safe and effective in the treatment of spinal OO and S2 OB in experienced hands, especially in lesions with no neurological deficits and cases of intact cortical bone. The presence of cerebrospinal fluid around the lesion is an appropriate indication for percutaneous RFA.
References
Barlow E, Davies AM, Cool WP, Barlow D, Mangham DC (2013) Osteoid osteoma and osteoblastoma: novel histological and immunohistochemical observations as evidence for a single entity. J Clin Pathol 66(9):768–774. doi:10.1136/jclinpath-2013-201492
Atesok KI, Alman BA, Schemitsch EH, Peyser A, Mankin H (2011) Osteoid osteoma and osteoblastoma. J Am Acad Orthop Surg 19(11):678–689
Berry M, Mankin H, Gebhardt M, Rosenberg A, Hornicek F (2008) Osteoblastoma: a 30-year study of 99 cases. J Surg Oncol 98(3):179–183. doi:10.1002/jso.21105
Chotel F, Franck F, Solla F, Dijoud F, Kohler R, Berard J, Abelin Genevois K (2012) Osteoid osteoma transformation into osteoblastoma: fact or fiction? Orthop Traumatol Surg Res 98(6 Suppl):S98–S104. doi:10.1016/j.otsr.2012.03.017
Enneking WF (1986) A system of staging musculoskeletal neoplasms. Clin Orthop Relat Res 204:9–24
Boriani S, Amendola L, Bandiera S, Simoes CE, Alberghini M, Di Fiore M, Gasbarrini A (2012) Staging and treatment of osteoblastoma in the mobile spine: a review of 51 cases. Eur Spine J 21(10):2003–2010
Boriani S, Weinstein JN, Biagini R (1997) Primary bone tumors of the spine. Spine (Phila Pa 1976) 22(9):1036–1044
Etemadifar MR, Hadi A (2015) Clinical findings and results of surgical resection in 19 cases of spinal osteoid osteoma. Asian Spine J 9(3):386
Gasbarrini A, Cappuccio M, Bandiera S, Amendola L, van Urk P, Boriani S (2011) Osteoid osteoma of the mobile spine. Spine (Phila Pa 1976) 36(24):2089–2093
Vanderschueren GM, Obermann WR, Dijkstra SPD, Taminiau AHM, Bloem JL, van Erkel AR (2009) Radiofrequency ablation of spinal osteoid osteoma. Spine (Phila Pa 1976) 34(9):901–903
Martel J, Bueno Á, Nieto-Morales ML, Ortiz EJ (2009) Osteoid osteoma of the spine: CT-guided monopolar radiofrequency ablation. Eur J Radiol 71(3):564–569
Okada K, Myoui A, Hashimoto N, Takenaka S, Moritomo H, Murase T, Yoshikawa H (2014) Radiofrequency ablation for treatment for osteoid osteoma of the scapula using a new three-dimensional fluoroscopic navigation system. Eur J Orthop Surg Traumatol 24(2):231–235
Weber MA, Sprengel SD, Omlor GW, Lehner B, Wiedenhöfer B, Kauczor HU, Rehnitz C (2015) Clinical long-term outcome, technical success, and cost analysis of radiofrequency ablation for the treatment of osteoblastomas and spinal osteoid osteomas in comparison to open surgical resection. Skeletal Radiol 44(7):981–993
Morassi LG, Kokkinis K, Evangelopoulos DS, Karargyris O, Vlachou I, Kalokairinou K, Pneumaticos SG (2014) Percutaneous radiofrequency ablation of spinal osteoid osteoma under CT guidance. Br J Radiol 87(1038):20140003
Rehnitz C, Sprengel SD, Lehner B, Ludwig K, Omlor G, Merle C, Kauczor H-U, Ewerbeck V, Weber MA (2012) CT-guided radiofrequency ablation of osteoid osteoma and osteoblastoma: clinical success and long-term follow up in 77 patients. Eur J Radiol 81(11):3426–3434
Jiang L, Liu XG, Wang C, Yang SM, Liu C, Wei F, Wu FL, Zhou H, Dang L, Liu ZJ (2015) Surgical treatment options for aggressive osteoblastoma in the mobile spine. Eur Spine J 24(8):1778–1785
Hadjipavlou AG, Lander PH, Marchesi D, Katonis PG, Gaitanis IN (2003) Minimally invasive surgery for ablation of osteoid osteoma of the spine. Spine (Phila Pa 1976) 28(22):E472–E477
Klass D, Marshall T, Toms A (2009) CT-guided radiofrequency ablation of spinal osteoid osteomas with concomitant perineural and epidural irrigation for neuroprotection. Eur Radiol 19(9):2238–2243
Rybak LD, Gangi A, Buy X, La Rocca Vieira R, Wittig J (2010) Thermal ablation of spinal osteoid osteomas close to neural elements: technical considerations. Am J Roentgenol 195(4):W293–W298
Dupuy DE, Hong R, Oliver B, Goldberg SN (2000) Radiofrequency ablation of spinal tumors. Am J Roentgenol 175(5):1263–1266
Greenberg A, Berenstein Weyel T, Sosna J, Applbaum J, Peyser A (2014) The distribution of heat in bone during radiofrequency ablation of an ex vivo bovine model of osteoid osteoma. Bone Jt J 96-B(5):677–683
Yamane T, Tateishi A, Cho S, Manabe S, Yamanashi M, Dezawa A, Yasukouchi H, Ishioka K (1992) The effects of hyperthermia on the spinal cord. Spine (Phila Pa 1976) 17(11):1386–1391
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Author LJ has received grants from Peking University Third Hospital. There is no other conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Funding
This study was funded by Peking University Third Hospital (Y71508-01).
Rights and permissions
About this article
Cite this article
Wang, B., Han, S.B., Jiang, L. et al. Percutaneous radiofrequency ablation for spinal osteoid osteoma and osteoblastoma. Eur Spine J 26, 1884–1892 (2017). https://doi.org/10.1007/s00586-017-5080-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5080-0