Abstract
Osteoid osteoma is a relatively common benign skeletal tumor. The traditional standard treatment has been surgical resection of the nidus. Recently, computed tomography (CT)-guided radiofrequency ablation (RFA) has gained favor as a more precise alternative due to potentially less bone destruction. However, CT-guided RFA is limited in treatment for osteoid osteoma involving complex anatomic structures such as cervical spine, pelvis, or scapula because of difficulty in approach and proximity to neurovascular structures. To solve this problem, we investigated RFA using a new real-time three-dimensional fluoroscopic navigation system. We report its technical procedure and use in a rare case of osteoid osteoma of the scapula.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoid osteoma is a relatively common benign skeletal tumor that accounts for 13.5 % of all benign tumors [1]. The male-to-female ratio in one large patient series was reported to be 4:1 [2]. The most common symptom is pain, which often worsens at night, and is usually relieved by non-steroidal anti-inflammatory drugs. The pain may cause arousal from sleep, resulting in sleep deprivation. Osteoid osteoma has a nidus surrounded by sclerotic bone and is usually less than 20 mm in size. It commonly occurs in the long bones of the lower extremity, occurring in the tibia and femur in 50 % of cases [3]. Among other bones, osteoid osteoma generally involves the upper limbs in 25 % of cases and occurs less frequently in the scapula (20 %; 5/25) than in the humerus (68 %; 17/25) [4].
The traditional standard treatment has been surgical resection of the nidus. Recently, potentially serious complications of surgery have made percutaneous radiofrequency ablation (RFA) an attractive alternative due to potentially less bone destruction, shorter hospitalization time, quicker rehabilitation time, and equal safety and efficacy [5]. Moreover, computed tomography (CT)-guided RFA has gained favor as a more precise alternative [6]. However, CT-guided RFA is limited for the treatment for osteoid osteomas involving complex anatomic structures, such as the cervical spine, pelvis, and scapula, because it is not a real-time guide, the treatment time is long, and radiation exposure is excessive for appropriate construction of images [7]. To solve this problem, we investigated RFA using a new three-dimensional (3D) fluoroscopic navigation system. We report its technical procedure and use in a rare case of osteoid osteoma of the scapula.
Technical report
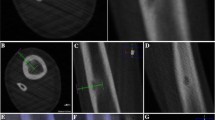
Treatment was performed under general anesthesia and with the patient placed in an appropriate position for the procedure (the entire procedure is shown in the supplementary movie). The reference frame was stabilized with two 1.6-mm-wide Kirschner wires (K-wire) that were inserted into the bone involving the tumor percutaneously. K-wires should be inserted to the point that had enough thickness to stabilize the frame and kept the appropriate distance to the tumor for easy manipulation to ablate the tumor. To acquire a 3D skeletal image, a Ziehm Vision FD Vario 3D (Ziehm Imaging, Orlando, FL, USA) was used to perform cone beam CT. Subsequently, a Stryker Navigation System 2 Cart (Stryker Orthopedics, Mahwah, NJ, USA) was used to create a live 3D fluoroscopic overlay. A 3D skeletal image, which was reconstructed from CT images, was used to plan the wire trajectory from the skin entry point to the nidus of the tumor. After the skin entry point and the wire trajectory were determined, 0.5-cm skin incision was made on the skin entry point and 1.6-mm K-wire and 1.7-mm drill guide were inserted to attach the cortex through the entry point. The determined path was guided by real-time 3D fluoroscopy to allow exact K-wire placement to the tumor and constant monitoring and adjustments during K-wire progression (Fig. 1). CT was performed again to confirm the correct position of the tip of the K-wire. Next, a bone biopsy was performed, in which the K-wire was replaced by a 17 G 15 cm RFA probe, and RFA was performed using a Cool-tip RFA system (Valleylab, Covidien, Mansfield, MA, USA) (Fig. 2). The RFA active tip was heated to 90 °C for 5 min, and 0.5 cm around the tip was ablated. Ablation was performed with 1-cm spacing in the tumor. After the ablation, RFA probe, the reference frame, and two 1.6-mm K-wires were removed and the skin incision on the entry point was sutured by 4-0 nylon.
Case and its result
One case is treated with this procedure. A 40-year-old man had severe pain in his left shoulder for 2 years. He was referred to our institution by another hospital because diagnosis on the basis of radiography alone was difficult. Radiography showed sclerotic changes around the glenoid cavity of the scapula (Fig. 3a), while CT revealed a subcortical cystic lesion with an indistinct nidus (Fig. 3b). Magnetic resonance imaging (MRI) showed a focal hyperintense lesion observed in the glenoid cavity of the scapula on T2-weighted MRI (Fig. 3c). On the basis of these findings, the cause of pain was diagnosed as osteoid osteoma of the scapula. Because of the tumor position, it was considered that the probable damage caused by surgical resection could interfere with normal shoulder function. Therefore, we decided to perform RFA using a new 3D fluoroscopic navigation system. Ablation was performed twice with 1-cm spacing in the tumor. The entire procedure took 59 min, and duration of radiation exposure during CT was 2.5 min. No complications were observed during the procedure. Pathological examination showed an appearance consistent with that of osteoid osteoma. Left shoulder pain totally disappeared immediately after the procedure; visual analog scale (0–10) was improved 7 to 0 two days after the procedure, and the patient experienced no significant complication or recurrence for 18 months.
Radiography, computed tomography (CT), and magnetic resonance imaging (MRI) of the scapula. a Radiograph shows sclerotic changes around the glenoid cavity of the scapula. b CT reveals a subcortical cystic lesion with an indistinct nidus. c T2-weighted MRI with fat suppression shows a focal hyperintense lesion with surrounding bone marrow edema
Discussion
CT-guided techniques for treating osteoid osteoma have emerged recently, and RFA is considered a good alternative to surgery [1]. In a previous study, CT-guided RFA has been suggested to be an effective treatment for most osteoid osteoma of the upper extremities, and 76 % (19/25 cases) of patients have become completely pain free after single treatment [4]. However, the success rate for upper extremities is lower than that for other skeletal areas (89–95 %) [8, 9]. Failure of RFA is considered to be caused by decreased temperature or duration of RFA because of proximity to neurovascular structures [4]. Furthermore, it has been suggested that recurrent pain may be due to inaccurate needle positioning, irritation of adjacent soft tissues, or inadequate ablation of large lesions [1]. On the basis of these reports, precise positioning that provides a safe distance from neurovascular structures may be necessary for effective treatment using RFA.
Real-time fluoroscopic navigation solves the above-mentioned problems. In previous studies, treatment involving planning with 3D images and 2D fluoroscopic navigation had the advantage of allowing access to the nidus from any direction [7], which enabled planning of a safe and effective path that avoided neurovascular structures, and precise positioning guided by real-time navigation may help prevent tumor recurrence. However, we believe that 2D fluoroscopic navigation is more difficult in the treatment for tumors involving complex anatomic structures, such as the pelvis and scapula. It has been suggested that treatment for tumors involving the pelvis or cervical spine, which are difficult to approach, may fail [10], and treatment for tumors in the scapula may have similar problems. The previous report and review suggested that osteoid osteoma of the scapula is a rare and in most cases does not involve the flat bone, which results in the difficulty of the surgery [11]. The new 3D fluoroscopic navigation system may overcome these difficulties because it can provide real-time information on the 3D position of the needle. Furthermore, in our past four cases, RFA using 2D fluoroscopic navigation took longer time for the operation and CT (93.7 min for operation and 4.6 min for CT; not published) and we experienced one failure case of osteoid osteoma in pelvis (not published). Therefore, we believe that the 3D fluoroscopic navigation system may reduce surgery time and the frequency of CT to confirm the needle position compared with those of previous navigation systems, especially for the treatment for osteoid osteoma in complex anatomic structure, such as the scapula.
There have been few previous reports of complications associated with osteoid osteomas. Full-thickness skin necrosis after RFA may occur with superficial thermocoagulation [12]. Nerve injuries have not been previously reported; however, treatment failure related to approach difficulties caused by nerve root proximity has been reported [10]. These reports clarified the problems associated with decisions regarding entry points and wire paths for approach in cases of osteoid osteoma involving complex anatomic structures. On the basis of this case, we believe that the 3D fluoroscopic navigation system may make it easier to determine appropriate entry points and paths in addition to decreasing complications.
Radiofrequency ablation using the new fluoroscopic navigation system resulted in successful treatment for osteoid osteoma in the scapula. Additional cases may show that this procedure is an effective and useful technique for the treatment for osteoid osteoma, especially involving complex anatomic structures.
References
Motamedi D, Learch TJ, Ishimitsu DN, Motamedi K, Katz MD, Brien EW et al (2009) Thermal ablation of osteoid osteoma: overview and step-by-step guide. Radiographics 29:2127–2141
Kransdorf MJ, Stull MA, Gilkey FW, Moser RP Jr (1991) Osteoid osteoma. Radiographics 11:671–696
Virayavanich W, Singh R, O’Donnell RJ, Horvai AE, Goldsby RE, Link TM (2010) Osteoid osteoma of the femur in a 7-month-old infant treated with radiofrequency ablation. Skeletal Radiol 39:1145–1149
Soong M, Jupiter J, Rosenthal D (2006) Radiofrequency ablation of osteoid osteoma in the upper extremity. J Hand Surg Am 31:279–283
Hoffmann RT, Jakobs TF, Kubisch CH, Trumm CG, Weber C, Duerr HR et al (2010) Radiofrequency ablation in the treatment of osteoid osteoma-5-year experience. Eur J Radiol 73:374–379
Mylona S, Patsoura S, Galani P, Karapostolakis G, Pomoni A, Thanos L (2010) Osteoid osteomas in common and in technically challenging locations treated with computed tomography-guided percutaneous radiofrequency ablation. Skeletal Radiol 39:443–449
Busser WM, Hoogeveen YL, Veth RP, Schreuder HW, Balguid A, Renema WK et al (2010) Percutaneous radiofrequency ablation of osteoid osteomas with use of real-time needle guidance for accurate needle placement: a pilot study. Cardiovasc Intervent Radiol 34:180–183
Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelmann W, Wortler K (2001) Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Jt Surg Br 83:391–396
Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ (2003) Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology 229:171–175
Vanderschueren GM, Taminiau AH, Obermann WR, van den Berg-Huysmans AA, Bloem JL (2004) Osteoid osteoma: factors for increased risk of unsuccessful thermal coagulation. Radiology 233:757–762
Mosheiff R, Liebergall M, Ziv I, Amir G, Segal D (1991) Osteoid osteoma of the scapula. A case report and review of the literature. Clin Orthop Relat Res 262:129–131
Lyon C, Buckwalter J (2008) Case report: full-thickness skin necrosis after percutaneous radio-frequency ablation of a tibial osteoid osteoma. Iowa Orthop J 28:85–87
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MPEG 48030 kb)
Rights and permissions
About this article
Cite this article
Okada, K., Myoui, A., Hashimoto, N. et al. Radiofrequency ablation for treatment for osteoid osteoma of the scapula using a new three-dimensional fluoroscopic navigation system. Eur J Orthop Surg Traumatol 24, 231–235 (2014). https://doi.org/10.1007/s00590-013-1180-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-013-1180-7