Abstract
Aim
To investigate the efficacy and safety of temporary internal distraction corrective surgery for extremely severe scoliosis.
Methods
Eleven scoliosis patients (3 males and 8 females) with curves ≥130° (mean 148.8°; range 130°–157°) who underwent a two-stage surgery, including a posterior temporary internal distraction correction and definitive posterior spinal correction with posterior pedicle screw instrumentation from 2008 to 2011 were retrospectively reviewed. Minimum follow-up was 2-years (mean 41.8 months; range 27.0–63.0 months). The analysis focused on the impact of temporary internal distraction on curve correction, pulmonary function tests (PFTs), complications and surgical outcomes. Neurosurveillance of sensory (somatosensory-evoked potentials) and motor (motor-evoked potentials) potential was performed in all cases. Posterior instrumentation was used in all patients.
Results
After the use of internal distraction, the preoperative major curve (mean 148.8°; range 130°–157°) was corrected to a mean of 79° (range 63°–87°), the T5–T12 kyphosis Cobb angle (mean 79°; range 30°–97°) was corrected to a mean of 59° (range 20°–75°), the coronal imbalance (mean 0.8 cm; range −3.6 to 2.8 cm) was improved to a mean of 0.6 cm (range −1.5 to 2.0 cm), the forced vital capacity percentage (FVC%) was improved from 59.3 ± 11.6 to 68.7 ± 13.7, and the forced expiratory volume in 1 s (FEV1%) was improved from 61.4 ± 13.6 to 71.3 ± 9.3. The average increase in body height was 6.7 cm, and the dorsum razor was corrected to 3–5 cm. During definitive surgery, the final major curves were corrected to a mean of 55° (range 32°–72°), the T5–T12 kyphosis Cobb was corrected to 35° (range 15°–68°), the coronal imbalance was improved to 0.5 cm (range −1.2 to 1.8 cm), the FVC% was improved to 71.2 ± 8.3, the FEV1% was improved to 76.3 ± 16.7, the increase in body height was 3.1 cm, and the dorsum razor was corrected to 1–3 cm. The mean interval time between the two surgeries was 3.5 months. None of the patients exhibited postoperative neurologic deficits or infections. No instrument complications were found during the final follow-up.
Conclusions
Temporary internal distraction in a two-stage corrective surgery provided patients who had extremely severe and rigid scoliosis, an effective and safe solution for scoliosis without significant complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Severe spinal deformities can cause compression of the spinal cord and thoracoabdominal structures [1, 2], which can lead to neurological and cardiopulmonary anomalies. It also affects the patient’s daily activities, growth, development, and appearance [3].
Posterior circumferential vertebral column resection (PVCR) produces a better correction rate (correction rate of 51–59 %) for severe and rigid scoliosis [1, 4–6]. Although it obviates a circumferential approach, a one-stage PVCR is associated with a high risk of neurological compromise during the acute correction, especially if there are significant kyphotic components, a history of intraspinal pathology or a history of previous spinal surgery [6–8]. Meanwhile, intraoperative massive bleeding and operative trauma might result in the deterioration of neurological and/or cardiopulmonary function. Thus, a one-stage PVCR may not be an ideal choice for patients with severe and rigid scoliosis [9–15].
The usual strategy employed to manage severe and rigid scoliosis includes halo-traction devices (e.g., halo-pelvic, halo-femoral, and halo-tibial) that gradually straighten the spine before fusion surgery to retain the position of the correction [16]. Halo-gravity traction (HGT) provides gradually significant corrective forces and it can be used in the patient’s bed, a wheelchair, with a walking frame, and during an operation [17], However, it is associated with complications and contraindications in the presence of fixed cervical instability, kyphosis, or stenosis. In addition, HGT involves the use of a bulky device that often requires the patient to stay in the hospital for the full duration of the procedure. These limitations led to the consideration of temporary internal distraction as an alternative.
To date, only a few studies have used internal distraction devices for deformity correction [17–21]. Some adopted the use of conventional growing rods, and another study reported a case that used a novel magnetically controlled growing rod as an internal distraction device for deformity correction. However, more studies are needed on the use of internal distraction for severe scoliosis (i.e., ≥130°).
The purpose of our study was (1) to assess the safety and efficacy of temporary internal distraction in treating complex, severe and rigid scoliosis of various aetiologies, (2) to observe the effects of temporary internal distraction on pulmonary function, and (3) to identify the complications associated with temporary internal distraction in perioperative and long-term time periods.
Materials and methods
Patients and evaluation
Retrospective analysis carried out in 11 consecutive patients (3 male and 8 female) with severe and rigid scoliosis (major curve Cobb angle ≥130 on anteroposterior radiograph, made with the patient standing; flexibility <15 % on lateral-bending radiograph, made with the patient supine) treated by a two-stage surgery in our hospital from June 2008 to February 2011. The procedure included the initial posterior temporary internal distraction correction following by the second stage posterior spinal correction with posterior pedicle screw instrumentation for the correction of extremely severe and rigid scoliosis. Neurosurveillance with sensory (somatosensory-evoked potentials) and motor (motor-evoked potentials) potential was performed in all cases.
All patients were reviewed with a minimum follow-up of 24 months (mean 41.8; range 27–63 months). No patient was lost during the follow-up. To evaluate surgical effectiveness, the clinical records were reviewed for demographic data, pulmonary function tests (PFTs), radiographic outcomes, operating time, average amount of blood loss and complications. PFTs analysis included percent forced vital capacity (FVC%) and percent volume expelled in one second (FEV1%). Radiographic analysis consisted of Cobb angle measurements of coronal curves, apical vertebral translation (AVT), coronal balance, sagittal balance, thoracic kyphosis, and lumbar lordosis. All measurements were taken preoperatively, after temporary internal distraction surgery, after the definitive surgery, and during the final follow-up period.
Deformity measurements were based on Cobb’s method. Flexibility was calculated according to the Cobb angle obtained from supine bending films. AVT for thoracic curves was measured as the distance between the C7 plumb line and the center of the apical vertebral body or disk. AVT for thoracolumbar and lumbar curves was measured as the distance between the central sacral line and the center of the apical vertebral body or disk. Coronal balance was measured as the distance between the C7 plumb line and the central sacral line. Sagittal balance was measured as the distance between the C7 plumb line and the posterosuperior corner of S1. Thoracic kyphosis was measured by the Cobb method from the superior end plate of T5 to the lower end plate of T12, and lumbar lordosis from the superior end plate of T12 to the end plate of S1.
Pulmonary function tests (PFTs) were assessed using a standard ultrasound spirometer in the sitting position (Spiroson, v1.2D, Germany). The pulmonary function value reported were forced vital capacity (FVC), which is expressed as a percentage of the predicted value (FVC%), and the volume expelled in one second (FEV1), which is expressed as a percentage of the predicted value (FEV1%) [22].
According to the American Thoracic Society’s guidelines for the severity of pulmonary impairment, ‘no’ pulmonary impairment was considered when the FVC% is >80 % of the predicted value, ‘mild’ when the FVC% is ≤80 % but >65 %, ‘moderate’ when the FVC% is ≤65 % but >50 %, and ‘severe’ when the FVC% is ≤50 %. For all the time observed, a negative FVC% change during the treatment period indicated a decline in FVC%.
Patients were defined as ‘pulmonary responders’ to temporary internal distraction if their pulmonary function (in terms of the FVC%) improved by at least 5 % and as ‘non-responders’ if there was an improvement or decrease of 0–5 %; a decline was noted if the FVC% dropped more than 5 % after 2 months of temporary internal distraction. Likewise, the impact of definitive posterior spinal correction on PFTs results was analyzed by comparing the FVC% performed after temporary internal distraction 2 months with FVC% performed after the definitive posterior spinal correction 2 months. Patients were classified as having improved (>5 % FVC% increase), stable (±5 % FVC% change) or worsened (>5 % FVC% decrease).
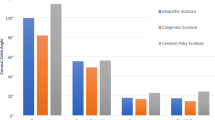
The mean age was 17.8 years (15–23 years); the mean preoperative rigid scoliosis measured 149°, flexibility <15 %. Average kyphosis Cobb is 79°, Risser Stage ≥4 (the French Risser staging systems) and closed triradiate cartilage in all cases. Diagnoses were neuromuscular scoliosis (n = 7), idiopathic (n = 3), and congenital (n = 1). Neuromuscular scoliosis patient diagnoses included spina bifida (type II, n = 3), syringomyelia (n = 2), and chiari malformation (n = 2), one of whom also had syringomyelia. Firstly, a posterior sub occipital craniectomy was performed to enlarge the foramen occipital magnum, and then the patients underwent the scoliosis correction with the two-stage surgery. All patients were ambulatory and with mild limit of daily living activity prior to surgery. All patients had a decrease in pulmonary function with an average of 61 % of normal FEV1 and 59 % of normal FVC (Fig. 1).
Surgical techniques and postoperative management
Patients were placed in the prone position after induction of general anesthesia with tracheal intubation. Two minimally invasive skin incisions (5 cm each) were made at the locations of the upper and lower end of the vertebra. The fascia adjacent to the spinous process in the concavity of the curve was divided and the paraspinous muscles partially mobilized, leaving a thin muscle cuff over the laminae. The periosteum and laminae were not exposed. Markers were placed on the spinous processes to radiographically identify the preplanned levels for instrumentation. Two-level pedicle screws were typically inserted in the upper and lower end vertebra, respectively (two pedicle screws at the cephalad end and two at the caudad end of the major coronal curve on the concave side). If it is too difficult to put in pedicle screws, laminar hooks can be used. Two rods were then measured (left 4–6 cm long above or below the upper or lower construct), cut, contoured for frontal and sagittal plane alignment. A longer distraction rod connected to the cephalad fixation points was inserted subcutaneously, and a shorter distraction rod was connected to the caudad fixation points. These two rods were connected with a side-by-side connector and were distracted and rotated by repeatedly loosening and tightening alternating screw nuts. This is usually a 4–6 cm distraction, depending on the flexibility of the scoliosis. Spinal cord monitoring (both somatosensory-evoked potentials and motor-evoked potentials) was used for all patients during the distraction maneuver throughout each procedure. A wake-up test was performed, and the patients were able to move all four limbs. Within several days after surgery, the patients were fitted with either a Milwaukee (cervical-thoracic-lumbar spinal orthosis) or a total contact (thoracic–lumbar spinal orthosis). The orthoses were worn at all times except when they were sleeping. The patients were allowed activities, as tolerated, after surgery. They were evaluated clinically and radiographically over 3-month intervals.
At 12–15 weeks after the initial surgery or distraction, a definitive posterior spinal fusion was performed when the patient’s medical status was good enough to receive a deformity correction. Patients were placed prone after induction of general anesthesia with tracheal intubation. Following posterior exposure and dissection of the paravertebral tissues to allow the rigid spine to become more flexible, using persuasion and rod derotation, the deformity was corrected. The temporary internal distraction rods were replaced with contoured permanent rods on the convex and concave sides. When there was a lack of scoliosis correction because of severe scoliosis, the Smith-Petersen osteotomy (SPO) [23] was also conducted. The pedicle screws from the previous implant were either retained or partially removed, according to the requirements for further correction. After the cross-link was tightened, the wound was irrigated copiously. Decortication was performed on all levels of planned fusion, and the bone graft was placed along the spine for posterior fusion. The wound was then closed in layers over subfascial drains. After posterior surgery, a wake-up test was performed in all patients. Patients were allowed to sit up in bed after the wound drainage was removed 48 h after the operation. They were then gradually allowed to get out of bed for exercise, although a plastic thoracolumbar sacral brace was prescribed for 3 months (Figs. 2, 3, 4).
a, b The patient underwent temporary internal distraction, postoperatively, the major curves of 137° was corrected to 75°, T5–T12 kyphosis Cobb angle of 92° was corrected to 55°. c, d During definitive surgery, the final major curves was corrected to 63°, T5–T12 kyphosis Cobb was corrected to 35°. e, f At the 24-month follow-up, no relevant loss of correction in the thoracic curve was observed
a Two minimally invasive skin incisions (5 cm each) were made at the locations of the upper and lower end vertebra.b A two-level pedicle screws and two rod were placed. c, d Two rods were connected with a side-by-side connector and were distracted and rotated by repeatedly loosening and tightening alternating screw nuts. e During definitive surgery, the deformity was corrected, and the temporary internal distraction rods were replaced with contoured permanent rods. f Decortication was done to all levels of planned fusion, and bone graft was placed along the spine for posterior fusion
Statistical analysis
Paired student’s t tests were used to test for the level of significance. P < 0.05 was considered statistically significant. The analyses were performed using SPSS11.0.
Results
A total of 11 consecutive patients were enrolled in this study. No patient was lost to follow-up. Demographic details and surgical parameters for all the patients are shown in Table 1. Radiographic parameters for the coronal and sagittal planes, and changes in forced vital capacity percentage (FVC%) and forced expiratory volume in 1 s (FEV1%) are shown in Table 2.
During internal distraction, the mean operating time was 118 min (range 90–135 min) and the mean total blood loss was 210 ml (range 140–300 ml). After the internal distraction, the preoperative major curves (mean 149°, range 130°–157°) were corrected to a mean of 79° (range 63°–87°), the T5–T12 kyphosis Cobb angle (mean 79°, range 30°–97°) was corrected to a mean of 59° (range 20°–75°), the imbalance (mean 0.8 cm, range −3.6 to 2.8 cm) was improved to 0.6 cm (range −1.5 to 2.0 cm) in the coronal plane and was improved to 0.5 cm (range −2.8 to 3.0 cm) in the sagittal plane (mean 1.4 cm, range −3.5 to 4.7 cm), the FVC% was improved from 59.3 to 68.7, the FEV1% was improved from 61.4 to 71.3, the average increase in body height was 6.7 cm, and correction of the dorsum razor was 3–5 cm. No neurologic deficits or infections resulted from the procedure. None of the patients reported breakdown of the skin.
During definitive surgery, the mean operating time was 303 min (range 250–400 min), the mean total blood loss was 1512 ml (range 650–2500 ml), the mean final major curves were corrected to 55° (range 32°–72°), the T5–T12 kyphosis Cobb was corrected to 35°(range 15°–68°), the coronal imbalance was improved to 0.5 cm (range −1.2 to 1.8 cm), the sagittal imbalance was improved to 0.2 cm (range −2.3 to 2.7 cm), the FVC% was improved to 71.2, the FEV1% was improved to 76.3, the mean increase in body height was 3.1 cm, and the correction of the dorsum razor was 1–3 cm.
During the most recent follow-up, there was neither significant loss of correction of the scoliotic curvature nor of the pulmonary function tests (PFTs) between the postoperative measurements and the last follow-up. The mean interval time between the two surgeries was 3.5 months.
All patients in our series recovered well following the surgery without major complications or death. There was a smooth transition from no spontaneous breathing to spontaneous breathing during the immediate postoperative period in the operating room in all patients. All of the patients were successfully extubated in the operating room. None developed respiratory complications, including postoperative pneumonia or required reintubation or tracheotomy. Postoperatively, none of the patients showed neurological deficits or infections. No instrumentation complications were found during the final follow-up. One complication, a paralytic ileus, occurred immediately after surgery. We observed the patient, and the complication cleared within 48 h after surgery. The patient did not require the use of medication.
Discussion
Severe scoliotic spinal deformities can cause compression of the spinal cord and thoracoabdominal structures [1–3], affect the thoracic cage; disturb skeletal, muscular and diaphragmatic function; and reduce respiratory system compliance [24, 25]. To date, a series of long-term studies on the natural course of pulmonary impairment and severe scoliosis have shown that there is no spontaneous resolution but rather a slight decline of PFT over time [26], and this is especially the case with curves >100°, in which respiratory system compliance is decreased to levels comparable to those of adult respiratory distress syndrome, which lead to patients suffering long-term sequelae. This includes reduced pulmonary endurance with an increased mortality rate compared with those who experience respiratory failure in adulthood [27–30]. Untreated severe (kypho-) scoliosis has a poor prognosis, accounting for up to 5 % of chronic ventilator failures in adulthood [31, 32]. Hence, pulmonary function in patients with severe scoliosis was seriously diminished, which can increase the risk of corrective surgery and affect the patient’s daily activities, growth and development and appearance [33].
The current PVCR approach has been a viable option for severe and rigid scoliosis, and it can achieve acute correction (a correction rate of 51–59 %) [12, 34–38]. In such situations, the risk of postoperative neurologic complications is further increased. Acute correction during PVCR, in cases with significant kyphotic components, a history of intraspinal pathology or previous spinal surgery, was reported to bring high risk for neurological compromise [39]. A long operation time, substantial blood loss and operative complications might cause the neurological and cardiopulmonary anomalies to worsen. Therefore, in patients with severe and rigid scoliosis and low pulmonary function, a one-stage PVCR may not always be the ideal choice.
Preoperative traction can correct severe spinal deformities before definitive spinal fusion. It allows for safer, partial and a less aggressive correction of a severely deformed spine and additional spinal deformities that may appear during gradually increased traction so that definitive surgical correction is performed on a less pronounced spinal deformity. This could allow for better and easier overall correction of the deformity without the risk of neurological and cardiopulmonary complications associated with major operations. Halo-traction devices (e.g., halo-femoral, halo-pelvic, and halo-gravity) have been employed to manage these severe and rigid scoliosis cases [15, 17, 40]. HGT can gradually provide significant corrective forces, but this involves the use of a bulky device and patients are often required to stay in the hospital during the entire procedure. The constant, high traction forces are associated with several long-term complications; for instance, pin loosening and superficial, deep pin tract infections (cranial osteomyelitis, intradural and extradural infections), a loss of cervical lordosis and cervical degenerative changes, and avascular necrosis of the proximal tip of the dens [41–46]. These limitations led us to consider the use of temporary internal distractions as an alternative.
To date, only a few studies have used internal distraction devices for deformity correction. Buchowski [19, 20] reported the use of internal distraction devices that accompanied anterior and/or posterior release for deformity correction. Cheng [3] adopted the use of conventional growing rods, and another [18] group reported a case that used novel magnetically controlled growing rods for correction. However, more studies are required on the use of internal distraction to adapt and optimize the techniques for severe scoliosis (≥130°) correction. We aimed to understand the safety and efficacy of temporary internal distraction in treating complex, severe and rigid scoliosis of various aetiologies; to observe the effects of temporary internal distraction on pulmonary function; and to identify the complications associated with temporary internal distractions during perioperative and long-term time periods.
There are studies [28] that have indicated a strong correlation between curve correction and pulmonary function improvement. Preoperative medical and pulmonary improvement in a patient with severe deformity can reduce surgical risks [47, 48]. Since the 1970s, HGT has been recommended for patients whose pulmonary function was so poor that immediate surgery might have been lethal [49]. In Koller’s study, the change from the pre-halo-traction FVC% to the follow-up FVC% averaged 3 %. In Rizzi’s study [28] on severe spinal curves, it was reported that pre-op-HGT was beneficial for the improvement of FVC that averaged 7 %. In a study by Nepple [50], the FVC% improved from 31 to 47 % after 4 weeks of HGT. Smiljanic [32] used an anterior open approach for instrumented derotation and reported on 31 cases of scoliosis of 108° corrected to 37°. He noted an improvement in the FVC% from 66 to 78 % at the 12-month follow-up. Similarly, Kim [51] used a segmental pedicle screw to treat moderate scoliosis and the results demonstrated a significantly increased respiratory function compared with the use of less rigid constructs. We found similar results showing there are ‘pulmonary responders’ to temporary internal distraction. The pulmonary function (represented by FVC%) in patients with pulmonary impairment were improved by 9 %, thus improving from moderate to mild. Temporary internal distraction significantly improved the patients’ postoperative pulmonary evolution with minimally invasive procedures. During the final surgery, pulmonary function (represented by FVC%) improved by 3 %, and these patients were considered to be ‘non-responders’. These stable results emphasize that interdistraction correction might also be decisive for pulmonary improvement in severe scoliosis. In summary, temporary internal distraction is a useful tool to improve a patient’s pulmonary condition.
In terms of halo distraction, Bonnett et al. [52] reported a series of halo-femoral traction with paralytic scoliosis patients who achieved an average of 53 % correction with an additional 12 % correction after posterior instrumentation. Rinella [53] demonstrated less overall curve correction (reduced by 38° or 46 %) than that in the report by Kane et al. and Bonnett et al. [52]. This may be partially due to lower relative traction forces associated with HGT than those associated with halo-femoral traction. However, the results of other experiments were significantly different and sometimes contradictory. Heiko et al. [24] showed that pre-op-HGT did not induce a meaningful release effect for rigid curves, and that the difference in flexibility between HGT radiographs and bending or traction radiographs was not significant. In studies by Seller [54] and Flierl [55], HGT did not improve surgical outcomes for scoliosis. These studies indicated that the real effect of HGT on rigid curves might be overestimated. It is interesting to note that Tokunaga [56] reported improved curve correction (>80°) with HGT and final posterior correction after anterior column release. He also emphasized that HGT gains more importance after an aggressive release. After anterior release, the correction due to HGT increased from 24 to 38 % after 1 week, to 42 % after 2 weeks and to 45 % after 3 weeks. Most of the final correction (49 %) was achieved by the anterior release and the first week of HGT. In our study, internal distraction occurred without posterior or anterior release and the mean operating time was 118 min, the mean total blood loss was 210 ml, the curve correction was 49 % (from 149° to 79°), and the T5–T12 kyphosis Cobb angle correction was 26 % (from 79° to 59°). The mean final curve correction was 64 % (from 149° to 55°). The curve correction rate after internal distraction was better than that achieved with conventional halo distraction and similar to that obtained from corrective surgery with posterior or anterior release. The final curve correction rate was better than that achieved with conventional halo distraction and less than that obtained from surgery with VCR. The concept of using an internal distraction rod to correct the coronal and sagittal planes before definitive fusion was suggested by the report published by Buchowski et al. [19, 20]. The authors implanted conventional growing rods into patients with severe curves and used two distraction procedures to perform a staged correction of the deformities. Curve correction after use of initial posterior release (with six also having anterior release) and internal distraction, and before definitive fusion averaged 53 % (from 104° to 49°); correction was 6 % after the second distraction procedure; and the mean final curve correction was 80 % (from 104° to 20°). We should also note the correction of the scoliotic curve can be obtained progressively by iterative lengthening the growing rod to treat evolutive scoliosis in young children [57–61]. Miladi et al. [57] showed the average improvement in Cobb angle after each rod-lengthening of the growing rod was 12.9, which includes two parts, the loss of correction due to spine growth between two rod lengthenings (10°) and the improvement of correction (2.9°). Moreover, the main scoliotic curve was corrected from 68° ± 32° (range 31°–142°) before surgery and preoperative reduction to 33° (range 11°–71°) after surgery, and 29° (range 15°–63°) on average at the last follow-up. This represents a 57 % improvement. By comparing the average improvement in Cobb angle after each rod-lengthening procedure in Miladi’s study and in Buchowski’s study, it can be seen that Miladi’s technique had the advantage of better curve correction after the rod-lengthening procedure.
This phenomenon exists for a number of reasons. First, submuscular placement of the rod in Miladi’s study avoided a long and unique incision and muscle release that provided fibrosis and bone auto fusion, whereas the viscoelasticity feature of soft tissues was preserved. Second, a growing rod has been proposed for those patients with an immature spine to halt scoliosis progression and delay the definitive surgical procedure until spinal growth was sufficient. Therefore, the mean age at initial surgery in Miladi’s study (average 9 years, range 2–13 years) was younger than in Buchowski’s study (average 13 years, range 8–16 years). The younger children possessed enviable flexibility and future development potential, which are beneficial for iterative lengthening of the growing rod in curve correction. Third, there were more severe and rigid main scoliotic curves in Buchowski’s study (average 104°, range 70°–131°) than in Miladi’s study (average 68°, range 31°–142°), which meant the curve correction was more difficult.
Our study differed from Buchowski’s and Miladi’s studies. First, we did not perform a second distraction procedure and a posterior or anterior release, and only a small difference in correction rate was found after the internal distraction procedure. Second, we did not perform VCR during final correction or fusion surgery. Finally, our study included older patients with more severe and rigid main scoliotic curves. These considerations are important in the assessment of the approach’s effectiveness in treating scoliosis and may limit the efficacy of repetitive distractions with growing rods. During internal distraction with a mini-invasive approach, the viscoelasticity feature of soft tissues is preserved, so results may be better if some iterative distractions are added to improve curve correction before definitive fusion. However, considering the patients’ more advanced ages and more severe and rigid main scoliotic curves in our series than those in Miladi’s series, and the increased cost of the operation, we did not perform repetitive distractions in our series. Certainly, this is an area that should be explored in future studies.
There are conflicting data as to whether maximizing curve correction is required for severe scoliosis. Problems arise with the lack of uniform definitions of severe and rigid curves [62–66]. Generally, severe curves have a Cobb angle >80°–90°, are rigid when the flexibility is <20–30 % and bend down to 70°–80° at best. Silvestre [63] stated that in severe scoliosis, the aim should be not to maximize the correction but rather to obtain an acceptable balance. This strategy was also followed in our study. After use of internal distraction, the imbalance of 0.8 cm (range −3.6 to 2.8 cm) was improved to 0.6 cm (range −1.5 to 2.0 cm) in the coronal plane, and the imbalance of 1.4 cm (range −3.5 to 4.7 cm) was improved to 0.5 cm (range −2.8 to 3.0 cm) in the sagittal plane. The average increase in body height was 6.7 cm, and the correction of the dorsum razor was 3–5 cm. During definitive surgery, the coronal imbalance was improved to 0.5 cm (range −1.2 to 1.8 cm), the sagittal imbalance was improved to 0.2 cm (range −2.3 − 2.7 cm), the mean increase in body height was 3.1 cm, and the correction of the dorsum razor was 1~3 cm. The spinal balance of patients showed good recovery.
Compared to PVCR and HGT results reported in the literature, temporary internal distraction seems to be much safer for improving pulmonary function and correcting spinal curves. Our results showed that all patients recovered well following the surgery with no major complications or death. All of the patients were successfully extubated in the operating room. None of the patients developed any respiratory complications, such as postoperative pneumonia, required reintubation or tracheotomy. Postoperatively, none of the patients showed neurological deficits or infections. No complication of instrumentation was found during the final follow-up. No one reported breakdown of the skin. Even with the advantages described above, internal distraction surgery was not perfect and one complication, a paralytic ileus, occurred immediately after surgery. This case was treated with observation and without oral intake, and it cleared within 48 h. In fact, there were tremendous force exerted on the pedicle screw during internal distraction surgery; therefore, surgeon should pay special attention to prevent screw pull out and neurologic injury.
Conclusion
The use of temporary internal distraction in two-stage corrective surgical treatment for extremely severe and rigid scoliosis can improve pulmonary function and correct deformity. Internal distraction is a safe and effective alternative treatment for severe and rigid scoliosis.
References
Inal-Ince D, Savci S, Arikan H, Saglam M, Vardar-Yagli N, Bosnak-Guclu M, Dogru D (2009) Effects of scoliosis on respiratory muscle strength in patients with neuromuscular disorders. Spine J 9:981–986. doi:10.1016/j.spinee.2009.08.451
Fletcher ND, Larson AN, Richards BS, Johnston CE (2011) Current treatment preferences for early onset scoliosis: a survey of POSNA members. J Pediatr Orthop 31:326–330. doi:10.1097/BPO.0b013e31820f77a0
Cheng X, Ma H, Tan R, Wu J, Zhou J, Zou D (2012) Two-stage posterior-only procedures for correction of severe spinal deformities. Arch Orthop Trauma Surg 132:193–201. doi:10.1007/s00402-011-1415-1
Xie JM, Zhang Y, Wang YS, Bi N, Zhao Z, Li T, Yang H (2014) The risk factors of neurologic deficits of one-stage posterior vertebral column resection for patients with severe and rigid spinal deformities. Eur Spine J 23:149–156. doi:10.1007/s00586-013-2793-6
Jeszenszky D, Haschtmann D, Kleinstuck FS, Sutter M, Eggspuhler A, Weiss M, Fekete TF (2014) Posterior vertebral column resection in early onset spinal deformities. Eur Spine J 23:198–208. doi:10.1007/s00586-013-2924-0
Leatherman KD (1973) The management of rigid spinal curves. Clin Orthop Relat Res:215–224
Charry O, Koop S, Winter R, Lonstein J, Denis F, Bailey W (1994) Syringomyelia and scoliosis: a review of twenty-five pediatric patients. J Pediatr Orthop 14:309–317
Farley FA, Song KM, Birch JG, Browne R (1995) Syringomyelia and scoliosis in children. J Pediatr Orthop 15:187–192
Bridwell KH (2006) Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine 31:S171–S178. doi:10.1097/01.brs.0000231963.72810.38
Lenke LG, O’Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM (2009) Posterior vertebral column resection for severe pediatric deformity: minimum two-year follow-up of thirty-five consecutive patients. Spine 34:2213–2221. doi:10.1097/BRS.0b013e3181b53cba
Papadopoulos EC, Boachie-Adjei O, Hess WF, Sanchez Perez-Grueso FJ, Pellise F, Gupta M, Lonner B, Paonessa K, Faloon M, Cunningham ME, Kim HJ, Mendelow M, Sacramento C, Yazici M (2013) Early outcomes and complications of posterior vertebral column resection. Spine J. doi:10.1016/j.spinee.2013.03.023
Xie J, Li T, Wang Y, Zhao Z, Zhang Y, Bi N (2012) Change in Cobb angle of each segment of the major curve after posterior vertebral column resection (PVCR): a preliminary discussion of correction mechanisms of PVCR. Eur Spine J 21:705–710. doi:10.1007/s00586-011-1985-1
Lu GH, Wang XB, Wang B, Li J, Kang YJ, Deng YW, Liu WD (2010) Complications of one stage posterior vertebral column resection for the treatment of severe rigid spinal deformities. Zhonghua wai ke za zhi [Chinese Journal of Surgery] 48:1709–1713
Li C, Fu Q, Zhou Y, Yu H, Zhao G (2012) Posterior extrapleural intervertebral space release combined with wedge osteotomy for the treatment of severe rigid scoliosis. Spine 37:E647–E654. doi:10.1097/BRS.0b013e318250042b
Xie J, Wang Y, Zhao Z, Zhang Y, Si Y, Yang Z, Liu L, Lu N (2011) One-stage and posterior approach for correction of moderate to severe scoliosis in adolescents associated with Chiari I malformation: is a prior suboccipital decompression always necessary? Eur Spine J 20:1106–1113. doi:10.1007/s00586-011-1717-6
Sponseller PD, Takenaga RK, Newton P, Boachie O, Flynn J, Letko L, Betz R, Bridwell K, Gupta M, Marks M, Bastrom T (2008) The use of traction in the treatment of severe spinal deformity. Spine 33:2305–2309. doi:10.1097/BRS.0b013e318184ef79
Lewis SJ, Gray R, Holmes LM, Strantzas S, Jhaveri S, Zaarour C, Magana S (2011) Neurophysiological changes in deformity correction of adolescent idiopathic scoliosis with intraoperative skull-femoral traction. Spine 36:1627–1638. doi:10.1097/BRS.0b013e318216124e
Cheung JP, Samartzis D, Cheung KM (2014) A novel approach to gradual correction of severe spinal deformity in a pediatric patient using the magnetically-controlled growing rod. Spine J 14:e7–e13. doi:10.1016/j.spinee.2014.01.046
Buchowski JM, Bhatnagar R, Skaggs DL, Sponseller PD (2006) Temporary internal distraction as an aid to correction of severe scoliosis. J Bone Joint Surg Am 88:2035–2041. doi:10.2106/JBJS.E.00823
Buchowski JM, Skaggs DL, Sponseller PD (2007) Temporary internal distraction as an aid to correction of severe scoliosis. Surgical technique. J Bone Joint Surg Am 89 (Suppl 2) Pt.2:297–309. doi: 10.2106/JBJS.G.00163
Tan R, Ma HS, Zou DW, Wu JG, Chen ZM, Zhou XF, Zhou JW (2012) Surgical treatment of severe scoliosis and kyphoscoliosis by stages. Chin Med J (Engl) 125:81–86
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC (1993) Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl 16:5–40
Smith-Petersen MN, Larson CB, Aufranc OE (1969) Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res 66:6–9
Koller H, Zenner J, Gajic V, Meier O, Ferraris L, Hitzl W (2012) The impact of halo-gravity traction on curve rigidity and pulmonary function in the treatment of severe and rigid scoliosis and kyphoscoliosis: a clinical study and narrative review of the literature. Eur Spine J 21:514–529. doi:10.1007/s00586-011-2046-5
Gonzalez C, Ferris G, Diaz J, Fontana I, Nunez J, Marin J (2003) Kyphoscoliotic ventilatory insufficiency: effects of long-term intermittent positive-pressure ventilation. Chest 124:857–862
Burrows B, Cline MG, Knudson RJ, Taussig LM, Lebowitz MD (1983) A descriptive analysis of the growth and decline of the FVC and FEV1. Chest 83:717–724
Pehrsson K, Larsson S, Oden A, Nachemson A (1992) Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine 17:1091–1096
Rizzi PE, Winter RB, Lonstein JE, Denis F, Perra JH (1997) Adult spinal deformity and respiratory failure. Surgical results in 35 patients. Spine 22:2517–2530 discussion 2531
Vitale MG, Matsumoto H, Bye MR, Gomez JA, Booker WA, Hyman JE, Roye DP Jr (2008) A retrospective cohort study of pulmonary function, radiographic measures, and quality of life in children with congenital scoliosis: an evaluation of patient outcomes after early spinal fusion. Spine 33:1242–1249. doi:10.1097/BRS.0b013e3181714536
Weinstein SL (1999) Natural history. Spine 24:2592–2600
Koumbourlis AC (2006) Scoliosis and the respiratory system. Paediatr Respir Rev 7:152–160. doi:10.1016/j.prrv.2006.04.009
Smiljanic I, Kovac V, Cimic M (2009) Changes in pulmonary functional parameters after surgical treatment of idiopathic scoliosis. Coll Antropol 33(Suppl 2):145–152
Zhou C, Liu L, Song Y, Liu H, Li T, Gong Q (2013) Two-stage vertebral column resection for severe and rigid scoliosis in patients with low body weight. Spine J 13:481–486. doi:10.1016/j.spinee.2012.07.008
Enercan M, Ozturk C, Kahraman S, Sarier M, Hamzaoglu A, Alanay A (2013) Osteotomies/spinal column resections in adult deformity. Eur Spine J 22(Suppl 2):S254–S264. doi:10.1007/s00586-012-2313-0
Wang Y, Zhang Y, Zhang X, Huang P, Xiao S, Wang Z, Liu Z, Liu B, Lu N, Mao K (2008) A single posterior approach for multilevel modified vertebral column resection in adults with severe rigid congenital kyphoscoliosis: a retrospective study of 13 cases. Eur Spine J 17:361–372. doi:10.1007/s00586-007-0566-9
Lenke LG, Sides BA, Koester LA, Hensley M, Blanke KM (2010) Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res 468:687–699. doi:10.1007/s11999-009-1037-x
Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH (2002) Posterior vertebral column resection for severe spinal deformities. Spine 27:2374–2382. doi:10.1097/01.BRS.0000032026.72156.1D
Wang Y, Xie J, Zhao Z, Zhang Y, Li T, Si Y (2013) Changes in CSF flow after one-stage posterior vertebral column resection in scoliosis patients with syringomyelia and Chiari malformation type I. J Neurosurg Spine 18:456–464. doi:10.3171/2013.1.SPINE12366
Akhtar OH, Rowe DE (2008) Syringomyelia-associated scoliosis with and without the Chiari I malformation. J Am Acad Orthop Surg 16:407–417 16/7/407 [pii]
Watanabe K, Lenke LG, Bridwell KH, Kim YJ, Hensley M, Koester L (2010) Efficacy of perioperative halo-gravity traction for treatment of severe scoliosis (≥100°). J Orthop Sci 15:720–730. doi:10.1007/s00776-010-1523-8
Letts RM, Palakar G, Bobecko WP (1975) Preoperative skeletal traction in scoliosis. J Bone Joint Surg Am 57:616–619
Tindall GT, Flanagan JF, Nashold BS Jr (1959) Brain abscess and osteomyelitis following skull traction. A report of three cases. Arch Surg 79:638–641
Papagelopoulos PJ, Sapkas GS, Kateros KT, Papadakis SA, Vlamis JA, Falagas ME (2001) Halo pin intracranial penetration and epidural abscess in a patient with a previous cranioplasty: case report and review of the literature. Spine 26:E463–E467
Soyer J, Iborra JP, Fargues P, Pries P, Clarac JP (1999) Brain abscess following the use of skull traction with Gardner-Wells tongs. Chirurgie 124:432–434 S0001400100800173 [pii]
Sharma BS, Khosla VK, Pathak A, Mathuriya SN, Kak VK (1988) Brain abscess following insertion of skull traction. Clin Neurol Neurosurg 90:361–363
Kaye AH, Briggs M (1982) Brain abscess after insertion of skull traction. J Bone Joint Surg Br 64:500–502
Wazeka AN, DiMaio MF, Boachie-Adjei O (2004) Outcome of pediatric patients with severe restrictive lung disease following reconstructive spine surgery. Spine 29:528–534 00007632-200403010-00009 [pii], discussion 535
Sink EL, Karol LA, Sanders J, Birch JG, Johnston CE, Herring JA (2001) Efficacy of perioperative halo-gravity traction in the treatment of severe scoliosis in children. J Pediatr Orthop 21:519–524
Winter RB, Lonstein JE (2010) The Moe maximal correction test to determine true curve flexibility: a historical note with current application. Spine 35:1733–1735. doi:10.1097/BRS.0b013e3181c65179
Nepple JJ, Lenke LG (2009) Severe idiopathic scoliosis with respiratory insufficiency treated with preoperative traction and staged anteroposterior spinal fusion with a 2-level apical vertebrectomy. Spine J 9:e9–e13. doi:10.1016/j.spinee.2009.01.009
Kim YJ, Lenke LG, Bridwell KH, Cheh G, Whorton J, Sides B (2007) Prospective pulmonary function comparison following posterior segmental spinal instrumentation and fusion of adolescent idiopathic scoliosis: is there a relationship between major thoracic curve correction and pulmonary function test improvement? Spine 32:2685–2693. doi:10.1097/BRS.0b013e31815a7b17
Bonnett C, Brown JC, Perry J, Nickel VL, Walinski T, Brooks L, Hoffer M, Stiles C, Brooks R (1975) Evolution of treatment of paralytic scoliosis at Rancho Los Amigos Hospital. J Bone Joint Surg Am 57:206–215
Rinella A, Lenke L, Whitaker C, Kim Y, Park SS, Peelle M, Edwards C 2nd, Bridwell K (2005) Perioperative halo-gravity traction in the treatment of severe scoliosis and kyphosis. Spine 30:475–482 00007632-200502150-00017 [pii]
Seller K, Haas S, Raab P, Krauspe R, Wild A (2005) Preoperative halo-traction in severe paralytic scoliosis. Z Orthop Ihre Grenzgeb 143:539–543. doi:10.1055/s-2005-836750
Flierl S, Carstens C (1997) The effect of halo-gravity traction in the preoperative treatment of neuromuscular scoliosis. Z Orthop Ihre Grenzgeb 135:162–170. doi:10.1055/s-2008-1039574
Tokunaga M, Minami S, Kitahara H, Isobe K, Nakata Y, Moriya H (2000) Vertebral decancellation for severe scoliosis. Spine 25:469–474
Miladi L, Journe A, Mousny M (2013) H3S2 (3 hooks, 2 screws) construct: a simple growing rod technique for early onset scoliosis. Eur Spine J 22(Suppl 2):S96–105. doi:10.1007/s00586-012-2379-8
Thompson GH, Akbarnia BA, Campbell RM Jr (2007) Growing rod techniques in early-onset scoliosis. J Pediatr Orthop 27:354–361. doi:10.1097/BPO.0b013e3180333eea
Pratt RK, Webb JK, Burwell RG, Cummings SL (1999) Luque trolley and convex epiphysiodesis in the management of infantile and juvenile idiopathic scoliosis. Spine 24:1538–1547
Akbarnia BA, Breakwell LM, Marks DS, McCarthy RE, Thompson AG, Canale SK, Kostial PN, Tambe A, Asher MA, Growing Spine Study G (2008) Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine 33:984–990. doi: 10.1097/BRS.0b013e31816c8b4e
Emans JB, Caubet JF, Ordonez CL, Lee EY, Ciarlo M (2005) The treatment of spine and chest wall deformities with fused ribs by expansion thoracostomy and insertion of vertical expandable prosthetic titanium rib: growth of thoracic spine and improvement of lung volumes. Spine 30:S58–S68
Zhang JG, Wang W, Qiu GX, Wang YP, Weng XS, Xu HG (2005) The role of preoperative pulmonary function tests in the surgical treatment of scoliosis. Spine 30:218–221 00007632-200501150-00011 [pii]
Di Silvestre M, Bakaloudis G, Lolli F, Vommaro F, Martikos K, Parisini P (2008) Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80 degrees: pedicle screws versus hybrid instrumentation. Eur Spine J 17:1336–1349. doi:10.1007/s00586-008-0731-9
Yamin S, Li L, Xing W, Tianjun G, Yupeng Z (2008) Staged surgical treatment for severe and rigid scoliosis. J Orthop Surg Res 3:26. doi:10.1186/1749-799X-3-26
Suh SW, Modi HN, Yang J, Song HR, Jang KM (2009) Posterior multilevel vertebral osteotomy for correction of severe and rigid neuromuscular scoliosis: a preliminary study. Spine 34:1315–1320. doi:10.1097/BRS.0b013e3181a028bc
Lonner BS, Murthy SK, Boachie-Adjei O (2005) Single-staged double anterior and posterior spinal reconstruction for rigid adult spinal deformity: a report of four cases. Spine J 5:104–108
Conflict of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Hu, HM., Hui, H., Zhang, HP. et al. The impact of posterior temporary internal distraction on stepwise corrective surgery for extremely severe and rigid scoliosis greater than 130°. Eur Spine J 25, 557–568 (2016). https://doi.org/10.1007/s00586-015-4013-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4013-z