Abstract
Purpose
Temporary internal distraction (TID) is a surgical technique used to correct severe scoliosis. We sought to evaluate the long-term outcomes associated with temporary internal distraction (TID) for severe scoliosis.
Methods
Scoliosis patients who underwent TID from 2006 to 2019 at a single institution were identified. Patients with coronal Cobb angles ≥ 90° or congenital scoliosis, and ≥ 2-year follow-up were included. Clinical and imaging data were reviewed for patient and operative characteristics and complications. Patient-reported outcomes were also analyzed.
Results
51 patients (37 female) were included. Mean age at surgery was 14.3 ± 3.5 years. Mean follow-up was 5.8 ± 3.0 years. Eighteen (35%) curves were idiopathic, 24 (47%) were cerebral palsy (CP) related, and 9 (18%) were congenital. Mean Cobb angle was 103° preoperatively and 20° at final follow-up, with an intermediate angle of 55º in staged procedures. Intraoperative neuromonitoring changes occurred in 13 (25.4%) cases, but all returned to baseline with immediate lessening of distraction. Overall, three (5.8%) cases of wound dehiscence, five (9.7%) cases of deep infections, one (2%) case of screw protrusion, and one (2%) case of delayed extremity weakness occurred. Patient-reported outcomes significantly improved at final follow-up.
Conclusion
Our findings suggest that TID is a valuable adjunct for correcting severe scoliosis. The mean Cobb reduction achieved (81%) was higher than that reported for halo-traction and was sustained over long-term follow-up. TID also allowed a shorter a hospital stay. While intraoperative neuromonitoring changes were not uncommon, they were reversible. However, care must always be exercised as major corrections may rarely result in delayed neurologic deficits despite intact neuromonitoring.
Level of evidence
Therapeutic—Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Severe scoliosis can have a major impact on patient health and quality of life. Surgical correction of large curves is difficult as it associated with a high risk of neurologic injury, particularly when a large amount of correction is attempted in a single procedure [1,2,3]. Halo-traction is considered the gold standard adjunct for treatment of large curves; nonetheless, it has several disadvantages including restriction of mobility, prolonged hospital stay, risk of cranial nerve injuries, and pin tract problems [1, 2]. Halo-traction may be also contraindicated in certain conditions such as cervical instability.
Temporary internal distraction (TID), first described by Buchowski et al. in 2006, is an alternative surgical technique used to correct severe scoliotic deformities [4]. By utilizing iterative distractions, it allows for correction of severe curves while minimizing the risk of neurologic injury associated with large “en bloc” corrections [5]. TID can be performed during a single procedure or in stages [6]. In the first step, cephalad anchors are placed on the spine or ribs, and caudad anchors placed on the spine or pelvis. Temporary distraction rods are inserted, osteotomies/releases are completed, and small, iterative distractions are attempted over the course of the procedure. If adequate correction is achieved, the final fusion may be completed at this time. If not, a staged approach may be performed, and the wound is closed. The patient returns to the operating room 1–3 weeks later where the temporary rods are removed, further distraction is performed, and the final fusion instrumentation is placed [6].
Although evidence supporting the benefits of TID for severe scoliosis is promising, current studies are limited by short-term follow-ups [4, 5]. Over the past 15 years, the senior author (PDS) has consistently utilized this technique and become more experienced with it. In this study, we sought to evaluate the corrective magnitude and long-term outcomes (including complications and patient reported outcomes) associated with TID for severe scoliosis.
Materials and methods
The study design was a retrospective case series. After institutional review board (IRB) approval, electronic medical records from a single institution were retrospectively reviewed to identify scoliosis patients who underwent TID and subsequent spinal fusion for either primary or secondary deformity correction from 2006 to 2019. We included patients with coronal Cobb angles ≥ 90° or congenital scoliosis. Minimum 2-year follow-up was required. Patients were further stratified by scoliosis etiology: idiopathic, congenital, or cerebral palsy (CP) related.
Clinic and operative notes were reviewed for patient characteristics (e.g., age, sex, etiology), visual analogue scale (VAS) pain scores, and operative details (e.g., TID method, definitive fusion levels). Pre- and postoperative imaging was used to determine coronal and sagittal Cobb angle changes over time. Other outcomes including intraoperative neuromonitoring (IONM) changes, patient reported outcomes, and complications (including surgical site infection or wound issues, new neurologic deficits, mechanical complications, revision surgery, and medical complications) were recorded. Patient-reported outcomes were analyzed through the scoliosis research society 22 questionnaire (SRS-22) for idiopathic scoliosis patients and the CPCHILD questionnaire for CP patients [7, 8]. These were prospectively collected for all patients and analyzed retrospectively. Patient-reported outcomes were not available for congenital scoliosis patients.
We also analyzed for differences in preoperative kyphosis, percent change in kyphosis, preoperative coronal Cobb angle, percent change in coronal Cobb angle, and deformity angular ratio (DAR) in patients who had IONM changes compared to those who did not. Independent t test was used for these comparisons while the paired t test was used to analyze for changes in SRS-22 and CPCHILD scores. All analyses were performed using Microsoft Excel (version 16.46, Microsoft Corporation).
Results
Baseline and operative characteristics and radiographic outcomes
A total of 51 patients (14 male; 37 female) were included (Table 1). Mean age at surgery was 14.4 ± 3.3 years. Mean follow-up duration was 5.0 ± 2.9 years. The etiology of 18 (35.3%) curves was idiopathic, 9 (17.6%) were congenital, and 24 (47.1%) were CP-related. Three patients were revision cases, and all others were primary fusions. Eleven patients were treated with staged TID (using temporary rods) and 40 were treated with single-stage TID (27 using outrigger distractor and 13 using temporary rods) (Table 2). The outrigger distractor is a custom-made distraction instrument used to perform temporary distraction through typical cephalad and caudal anchors but without the need to insert a temporary rod.
Time between surgeries for staged TID ranged from 11 to 31 days. Mean Cobb angle of main curves was 103° preoperatively and 20° at final follow-up, with an intermediate angle of 55º in staged procedures (Table 3). Initial coronal DAR was 9.95 ± 2.18 (Table 1) [9]. Preoperative T1–T12 kyphosis and L1–L5 lordosis angles were 42º (5º–100º) and 51º (20º–95º), respectively, compared to 33º (9º–74º) and 46º (10º–75º) postoperatively (Table 3). Final coronal correction ranged from 80 to 88% depending on etiology (Fig. 1).
Complications
Mean postoperative pain score was 1.2 ± 2.6 compared to 1.6 ± 2.9 preoperatively. Only two patients (5%) had persistent pain (> 5 out of 10 VAS) at 6 months and both resolved at 2-year follow-up. During Stage 1 of staged procedures, IONM changes occurred in three (27.3%) cases, but these changes were transient and did not correlate with any neurological deficit (Table 4). During definitive PSF, IONM changes occurred in ten (19.6%) cases (only one of these instances occurred in a revision case). All but one (2%) case returned to baseline with immediate lessening of distraction, although this patient did not have any clinical neurologic deficit. Separately, one neuromuscular (2%) patient developed lower extremity weakness > 12 h after definitive fusion despite stable neuromonitoring. This resolved after reoperation to decrease correction (Table 4).
Five (9.8%) patients (including 1 idiopathic, 1 congenital, and 3 CP-related) developed deep surgical site infection (2 acute and 3 late) (Table 4). Both acute infections were treated by debridement, and all three late infections were treated by debridement and exchange of instrumentation. Late infections occurred at 3, 5, and 7 years after index surgery. By procedure type, 3/40 (7.5%) single-stage patients (1 idiopathic, 1 congenital, 1 CP patient) had a surgical site infection compared to 2/11 (18%) staged patients (both CP patients). Superficial wound dehiscence occurred in one idiopathic and two CP patients, and all resolved with observation and dressing changes. One CP patient had proximal pedicle screw protrusion causing brachial plexus irritation 1-year postoperatively. This was treated with reoperation and revision of proximal anchors. No other mechanical or implant-related complications occurred. With regards to medical complications, one CP patient had intraoperative cardiac arrest which occurred before incision. Surgery was postponed until the patient was medically stable. Two CP patients had pneumonia, and two other CP patients had postoperative urinary tract infections. All resolved with appropriate medical management (Table 4). None of the three revision cases had any complication.
Patient-reported outcomes
At final follow-up, idiopathic patients had significantly improved SRS-22 scores compared to preoperatively for the self-image/appearance domain (2.8 ± 0.4 vs 4.4 ± 0.8; P < 0.01), satisfaction domain (3.3 ± 0.8 vs 4.6 ± 0.9; P = 0.04), and total scores (3.6 ± 0.3 vs 4.1 ± 0.6; P = 0.05) (Table 5). Meanwhile, CP patients had improved CPCHILD scores for the positioning, transferring and mobility domain (29.8 ± 7.2 vs 52 ± 8.4; P < 0.01), comfort and emotions domain (48.3 ± 10.2 vs 87.5 ± 12.0; P < 0.01), communication and social interaction domain (44.1 ± 18.2 vs 65 ± 6.6; P = 0.03), overall quality of life domain (64.0 ± 20.1 vs 87.1 ± 7.5; P < 0.01), and total scores (40.6 ± 5.7 vs 64.5 ± 3.5; P = 0.04) (Table 5).
Predictors of IONM changes
Compared to patients with no IONM changes, patients who had IONM changes had higher mean preoperative kyphosis (41.0 ± 15.8 vs 39.2 ± 23.7; P = 0.80), higher mean percent kyphosis correction (15.2 ± 14.9 vs 4.9 ± 31.6; P = 0.27), higher mean preoperative coronal Cobb angle (107.3 ± 14.9 vs 102.4 ± 17.9; P = 0.38), higher mean coronal Cobb correction (81.3 ± 7.5 vs 79.1 ± 7.3; P = 0.37), and higher mean coronal DAR (10.6 ± 2.4 vs 9.5 ± 2.5; P = 0.18). However, none of these differences reached statistical significance. Further, there was no significant difference in scoliosis etiology in those with IONM changes compared to those with no IONM changes (P = 0.08) (Table 4).
Discussion
In 1971, Nachemson and Elfstrom analyzed telemetry recordings across Harrington rods in scoliosis patients and noted that the tension across the construct rapidly decreases in the hours and days following distraction [10, 11] This highlighted the viscoelastic nature of the spine and paraspinal soft tissues, suggesting that spacing out distractive forces over time would potentially decrease the stress on the spine. Almost 35 years later, utilizing these same principles, Buchowski et al. described TID using modern segmental instrumentation and showed that it maintained good corrective capacity while minimizing the risk of neurologic injury associated with large distractions [4, 5].
In this ≥ 2 year follow-up series of 51 patients with severe scoliosis, we found that TID achieved 55% intermediate curve correction and 81% final curve correction, consistent with the original report by Buchowski et al. also demonstrating 50 and 80% curve correction, respectively [4]. With a mean follow-up of 5 years, we also found that correction was maintained at final follow-up and patient reported outcomes were significantly improved. Notably, mean preoperative DAR was low to moderate. This likely reflects our preferential utilization of TID primarily for large, multisegmented curves (Fig. 2). In our experience, TID works best for curves with low DARs as opposed to short, rigid curves which might be better treated with osteotomies and releases. Nonetheless, we have found TID to be useful in revision causes with stiff curves where strong distraction is required (Fig. 3).
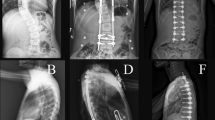
A Preoperative AP and lateral radiographs of 12-year-old female with idiopathic scoliosis (115° curve) treated with a staged temporary internal rod distraction. B AP and lateral radiographs after stage 1 and C after stage 2 (performed 13 days after stage 1). D AP and lateral radiographs at 7-year follow-up
A Preoperative AP and lateral radiographs of 17-year-old male with congenital scoliosis and other associated congenital abnormalities who had prior spinal instrumentation but still had trouble with posture (99° curve). He had a single lung, so we avoided intrathoracic procedures. B AP and lateral radiographs post-stage 1 of distraction, C post-stage 2 of distraction (performed 6 weeks after stage 1), and at D 3-year follow-up. E Clinical images preoperatively (left two panels) and at 3-month postoperatively (right two panels)
Halo-traction followed by spinal fusion is a well-established strategy for many cases of severe scoliosis [1, 2, 12]. Nonetheless, TID is a valuable alternative when the risks of traction-related complications are elevated or when halo-traction is contraindicated [1, 2]. TID also has several other advantages in our experience. First, it requires a much shorter hospital stay compared to halo-traction. This is important as patients and families are often averse to halo-traction, considering its mobility restrictions, interference with daily activities, and requirement of longer hospital stays. In this series, most TID cases were done as a single-stage procedure, while time between staged procedures averaged 18 days. This is considerably shorter compared to the mean treatment duration of 6 weeks for halo-traction [3, 12, 13]. Second, we have found halo-traction to be less effective for caudal deformities, where it achieves limited tensile strength. TID overcomes this by applying corrective forces directly to the region of deformity. Third, TID achieved a higher mean curve correction (81%) compared to that reported for halo-traction followed by spinal fusion, which ranges from 50 to 60% [3, 13]. This likely reflects the ability of TID to combine with intraoperative releases and focus corrective forces directly on the spine. Despite these advantages, it is important to note that our study design prevents us from making any conclusive claims about the overall efficacy of TID compared to halo-traction. We have only highlighted certain scenarios where TID provides advantages over halo-traction.
A vertebral column resection (VCR) is another well-recognized option for severe deformities [14]. In our experience, VCRs or extensive osteotomies may be preferred in short rigid curves. Such resections may allow protection of the spinal cord against focal bony compression as the deformity is corrected. However, TID is suitable for longer curves as it deals with the musculo-ligamentous envelope and offers a lower risk of complications and neurologic injury [15,16,17,18]. We have found the single-stage outrigger distractor to be especially useful in idiopathic patients for avoiding staging or more complex procedures such as a VCR (as demonstrated by that only three idiopathic scoliosis patients underwent staged distraction in our series). In contrast to VCR, wherein only further resection or realignment can be performed if neuromonitoring signals are lost, TID is reversible at every stage, and neuromonitoring changes can be immediately reversed by lessening distraction in most cases. This is reflected in our series by the return of neuromonitoring signals in all but one patient with signal loss. Skaggs et al. similarly reported a 41% incidence of neuromonitoring changes in a series of 22 patients treated with TID, with all but one case resolving upon lessening of distraction [5]. Undeniably, the risk of neurologic insult is still present, as seen in one patient in our series who developed a delayed motor weakness after surgery and required return to the operating room to decrease distraction. This occurred despite stable intraoperative neuromonitoring throughout the initial procedure. The weakness resolved with reoperation to decrease distraction and the patient did well afterwards, again reflecting the advantageous reversibility of TID during both the intraoperative and early postoperative periods. In our experience, TID in conjunction with posterior mobilization techniques has rendered VCR rarely needed in our pediatric spinal deformity practice.
As a staged procedure, TID also offers two other advantages. First, it allows testing of the intended lower instrumented vertebrae as well as confirmation of trunk balance with the patient standing and moving before the definitive fusion is performed. This permits better planning of the definitive fixation. Second, it allows testing of neurologic function through a complete motor and sensory physical exam between procedures. Such neurologic evaluation is especially valuable for high cervicothoracic scoliosis where intraoperative monitoring of upper extremity function may be less reliable. We did have 2/11 (18%) infections in the staged group (both in CP patients), which is undesirable. However, it is unclear whether staging increases the risk of infection, or this is secondary to the underlying pathology and large curve. This remains an opportunity for improvement and future research.
This study is limited by its retrospective design, sample size, and lack of matched controls. Since severe scoliosis correction is not common, we did not limit our series to a specific etiology and had a heterogenous population. As such, our results are better interpreted by examining the outcomes of each patient population, and not the overall aggregated results. Moreover, since this is a case series, it is only able to offer descriptive analyses with no true comparative power. It is also worth noting that our complication rates may have been inflated due to inclusion of only severe curves and analysis of long-term follow-up, since patients who did well were more likely to be lost to follow-up early on. Further, due to the retrospective nature of this series, we may have missed other complications treated at other institutions after loss-to-follow-up. While we highlighted some advantages of TID, we are unable to make conclusive claims about its efficacy compared to halo-traction. Finally, our sub-analysis of predictors of IONM changes was limited by sample size, and a larger sample may be able to demonstrate significant differences. Despite these limitations, this study constitutes, to our knowledge, the largest reported series of TID for severe scoliosis as well as the first analysis of long-term outcomes after TID.
Conclusion
TID is effective in improving the muscular and ligamentous contractures present in large curves. In this case series of 51 patients with large curves, TID achieved and maintained an 81% corrective magnitude over a mean follow-up of 5 years. Advantages of TID include eliminating the need for long hospital stays and facilitating safer distractions with a low risk of neurologic injury, largely owing to its reversibility at all stages. When performed as a staged procedure, TID also allows for testing of intended lower instrumented vertebrae and trunk balance prior to definitive fixation, as well as verification of intact motor and sensory function. Although these results are encouraging, we emphasize that TID must always be performed with accurate neuromonitoring and utilized only for curves low DAR, as over-distraction of more angular curves may increase the risk of neurologic injury. Further, neurologic deficits may occur despite intact neuromonitoring when severe correction is attempted.
References
O’Brien JP, Yau AC, Smith TK et al (1971) Halo pelvic traction. A preliminary report on a method of external skeletal fixation for correcting deformities and maintaining fixation of the spine. J Bone Joint Surg Br 53(2):217–229
Kumar K (1996) Spinal deformity and axial traction. Spine (Phila Pa 1976) 21(5):653–655
Sink EL, Karol LA, Sanders J et al (2001) Efficacy of perioperative halo-gravity traction in the treatment of severe scoliosis in children. J Pediatr Orthop 21(4):519–524
Buchowski JM, Bhatnagar R, Skaggs DL et al (2006) Temporary internal distraction as an aid to correction of severe scoliosis. J Bone Joint Surg Am 88(9):2035–2041
Skaggs DL, Lee C, Myung KS (2014) Neuromonitoring changes are common and reversible with temporary internal distraction for severe scoliosis. Spine Deform 2(1):61–69
Buchowski JM, Skaggs DL, Sponseller PD (2007) Temporary internal distraction as an aid to correction of severe scoliosis. Surgical technique. J Bone Joint Surg Am 89(Suppl 2):297–309
Narayanan U. CPCHILD: Caregiver priorities & child health index of life with disabilities. Available at https://lab.research.sickkids.ca/pscoreprogram/wp-content/uploads/sites/72/2017/09/CPCHILD_English_Parent_5.0_Watermarked.pdf. Accessed 23 Apr 2020
Narayanan UG, Fehlings D, Weir S et al (2006) Initial development and validation of the Caregiver priorities and child health index of life with disabilities (CPCHILD). Dev Med Child Neurol [Internet] 48(10):804–812. https://doi.org/10.1111/j.1469-8749.2006.tb01227.x/pdf
Lewis NDH, Keshen SGN, Lenke LG et al (2015) The deformity angular ratio: does it correlate with high-risk cases for potential spinal cord monitoring alerts in pediatric 3-column thoracic spinal deformity corrective surgery? Spine (Phila Pa 1976) 40(15):E879–E885
Nachemson A, Elfström G (1971) Intravital wireless telemetry of axial forces in Harrington distraction rods in patients with idiopathic scoliosis. J Bone Joint Surg Am 53(3):445–465
Elfström G, Nachemson A (1973) Telemetry recordings of forces in the Harrington distraction rod: a method for increasing safety in the operative treatment of scoliosis patients. Clin Orthop Relat Res 93:158–172
Edgar MA, Chapman RH, Glasgow MM (1982) Pre-operative correction in adolescent idiopathic scoliosis. J Bone Joint Surg Br 64(5):530–535
Letts RM, Palakar G, Bobecko WP (1975) Preoperative skeletal traction in scoliosis. J Bone Joint Surg Am 57(5):616–619
Saifi C, Laratta JL, Petridis P et al (2017) Vertebral Column Resection for Rigid Spinal Deformity. Glob spine J 7(3):280–290
Lenke LG, Newton PO, Sucato DJ et al (2013) Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine (Phila Pa 1976) 38(2):119–132
Suk S-I, Chung E-R, Kim J-H et al (2005) Posterior vertebral column resection for severe rigid scoliosis. Spine (Phila Pa 1976) 30(14):1682–1687
Hamzaoglu A, Alanay A, Ozturk C et al (2011) Posterior vertebral column resection in severe spinal deformities: a total of 102 cases. Spine (Phila Pa 1976) 36(5):E340–E344
Xie J, Wang Y, Zhao Z et al (2012) Posterior vertebral column resection for correction of rigid spinal deformity curves greater than 100°. J Neurosurg Spine 17(6):540–551
Funding
No funding was received in support of this work.
Author information
Authors and Affiliations
Contributions
Conception and design, analysis of data, manuscript drafting, manuscript revision: DB, AG, DLS, PDS, IRB. Acquisition of data: DB, AG. Interpretation of data: DB, DLS, PDS. We declare that all authors have met all four authorship criteria: (1) Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work. (2) Drafted the work or revised it critically for important intellectual content. (3) Approved the version to be published. (4) Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
David Skaggs received grants or contracts from NuVasive, royalties or licenses from Wolters Kluwer Health and Zimmer Biomet, consulting fees from ZimmerBiomet, Top Doctors, and Orthobullets, payment or honoraria from ZimmerBiomet, leadership or fiduciary roles in Pediatric Spine Study Group, Pediatric Spine Foundation, Spine Deformity, Orthopedics Today, Journal of Children’s Orthopedics, Stock or Stock option in Zipline Medical, Green Sun Medical, Orthobullets. Paul Sponseller received consulting fees from Orthopediatrics, Johnson and Johnson, and Nuvasive, payment or honoraria from Johnson and Johnson, and Nuvasive, support for attending meetings/travel from Johnson and Johnson, leadership or fiduciary role in Scoliosis Research Society and Marfan Foundation. All other authors have no disclosures.
Ethical approval
This study was approved by the Johns Hopkins Institutional Review Board (IRB).
Informed consent
Informed consent or a waiver of informed consent was obtained where applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Badin, D., Gupta, A., Skaggs, D.L. et al. Temporary internal distraction for severe scoliosis: two-year minimum follow-up. Spine Deform 11, 341–350 (2023). https://doi.org/10.1007/s43390-022-00602-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00602-9