Abstract
Introduction
Degenerative scoliosis is a three-dimensional deformity that can present in some instances with fixed sagittal and coronal imbalance. Pedicle subtraction osteotomy (PSO) is an effective technique that allows correction with a posterior approach. When a combined coronal and sagittal imbalance is present, asymmetric PSOs could be an optimal choice to correct deformity on both planes.
Methods
The asymmetric wedge resected from the vertebral body has to be shorter in the side of coronal imbalance, while a higher side cut has to be performed in the site opposite to the coronal imbalance. This allows to restore both coronal and sagittal alignment after osteotomy closure. An adequate preoperative planning is mandatory to correctly assess the geometry of the wedge to obtain the necessary correction.
Conclusions
The few studies present in literature show good results in terms of correction, even if the difficulty of this technique is certain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vertebral osteotomies are becoming frequently used to treat spinal deformities and restore a correct alignment of the thoracolumbar region. Wedge osteotomies like pedicle subtraction osteotomy (PSO) or Smith–Petersen osteotomy (SPO) are commonly used when a sagittal imbalance occurs, causing a decrease in patients’ quality of life due to back pain, radiculopathies, and walking impairment. Lumbar disc degeneration is the first cause of such imbalance, with a loss of lordosis of the lumbar region and a consequent disruption of the normal alignment of the spine. Lumbar kyphosis can also depend from previous vertebral fractures, previous surgery, spondylodiscitis, and other conditions that alter the normal shape of the spinal segment of motion.
Combined sagittal and coronal imbalance is less frequent than sagittal balance alone, and is mainly caused by the asymmetrical degeneration of discs, with inability to compensate for the primary deformity at levels above or below the original deformity. Coronal imbalance or combined sagittal and coronal malalignment can also be the consequence of a previous surgery with an improper correction of a pre-existing deformity. In some cases of isolated sagittal imbalance, the lack of control of the coronal plane during operations that dramatically increase the flexibility of the spine (as PSO itself) can result in postoperative fixed coronal or combined coronal and sagittal imbalance. Finally, failure to identify different degrees of stiffness in two areas of a scoliotic curve can lead to a different degree of correction in the coronal plane that results in postoperative coronal imbalance of a previously coronal balanced spine.
The three-column posterior osteotomy, or PSO, was first described by Thomasen in 1985 for patients with ankylosing spondylitis [1]. It is usually performed in the lumbar spine and is typically used to correct a fixed sagittal deformity that requires a correction of as much as 30°–35° at a single level. When a combined sagittal and coronal malalignment is present, an asymmetric PSO can correct the spine on both the planes and restore satisfactory alignment. The aim of the present paper is to describe this specific technique and discuss on it with case studies.
Preoperative evaluation
Preoperative planning is mainly based upon full spine, standing frontal and lateral X-rays of the patient. Measurement of the pelvic incidence (PI) is the basis to calculate the ideal lumbar lordosis (LL), lower lumbar lordosis (LL4-S1), thoracic kyphosis (TK), and pelvic tilt (PT) of the patient. An appropriate classification of the deformity is useful to determine the levels that should be treated and to assess the correct surgery [2, 3]. In the frontal plane, a C7 plumbline passing more than 4 cm lateral to the center of the sacrum is usually the criterion to define coronal imbalance. Sagittal imbalance can be defined as a C7 plumbline more than 5 cm anterior to the posterior S1 corner or increased pelvic tilt with kyphotic deformity of the lumbar spine or the thoracolumbar junction (in this case, kyphotic deformity means more kyphosis or less lordosis than predicted). Though beyond the scope of this article, the correction goal in the sagittal plane matches the ideal sagittal shape of the spine in this calculation and is based on different preoperative calculations [4]. Lateral bending films are used to evaluate the flexibility of each segment of the spine. Though bending films can underestimate the reducibility of the curve, they permit to verify the mobility of spinal segments, and thus some potential of correction. In some cases, an MRI or CT scan can provide additional information on alignment, bone stock, neural compression, and fusion or ankylosis (Fig. 1).
CT 3D reconstruction of a lumbar spine of a 56-year-old female suffering from degenerative scoliosis. Fusion between L4 and L5 with a coronal tilt of the segment causes the inferior half of the lumbar curve being stiffer than the upper one. Underestimation of this differential stiffness caused postoperative coronal imbalance (same patient as in Fig. 5)
Preoperative planning regarding the sagittal plane correction follows standard rules. In the case of coronal plane, the most important aspects of correction when a rigid coronal deformity exists are determining the level at which the osteotomy should be performed and calculating the necessary degree of correction of coronal imbalance.
Regarding the level of the osteotomy, the key factor regarding coronal plane is the direction of the coronal imbalance with respect to the lumbar scoliotic curve. When the coronal imbalance is toward the convexity of the main lumbar curve, the asymmetrical PSO should be performed at the base of the main lumbar curve. When the coronal imbalance is toward the concavity of the main lumbar curve, the asymmetrical osteotomy should be performed in the apical area of the lumbar deformity.
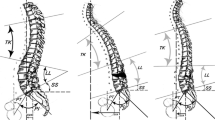
The magnitude of the osteotomy can be separately calculated in both planes (sagittal and coronal). Starting with the sagittal plane, the degrees of correction at the level of the osteotomy are calculated. A simple trigonometric calculation is made (or a graphical simulation) to translate in millimeters of height the amount of resection of the posterior wall of the osteotomized vertebra (Fig. 2). This height (H1) will be the height of the osteotomy in the side of the vertebra where the shorter resection will be performed. After this, a calculation of the angle of acute coronal correction at the level of the osteotomy is made and the angle is translated in millimeters of height of coronal resection (H2). The planned osteotomy will have a height at the side of the coronal imbalance equal to H1 and at the opposite side equal to H1 + H2. The cranial osteotomy line will be parallel to the disc space. The caudal osteotomy line will run from H1 below the cranial osteotomy line at the side of the coronal decompensation to H1 + H2 below the cranial osteotomy line at the opposite side of the vertebra. Closure of such an osteotomy will result in simultaneous correction in the coronal and lateral plane equal to the planned angulations (Fig. 2).
For the rest of the procedure, the technique is equivalent to standard PSO that is described in another article of this supplement.
Surgical technique
The patient is placed in a prone position on a Jackson table or a Wilson frame. The abdomen should be left hanging to avoid any compression that could increase the venous blood return and consequent intraoperative bleeding. A longitudinal skin incision corresponding to the planned instrumented vertebrae is followed by a deep dissection of the paravertebral muscles, until a complete exposition of the bony structures is obtained. Pedicle screws are inserted in the planned fusion area, except for the vertebra where the osteotomy will be performed. A complete laminectomy is then performed at the osteotomy level, including a partial removal of the cranial and caudal laminae and spinous processes. Dura is exposed and the four roots exiting from the upper and lower foramens are identified. The transverse processes are removed and the lateral walls isolated. Osteotomy starts with a deep insertion of taps of increasing sizes, until a cavity in the vertebral body is obtained. An asymmetric wedge is then resected; the characteristics of the wedge should be the following: the upper cut line should be parallel to the superior endplate of the osteotomized vertebra; the lower cut line should be oblique going from cephalad to caudal from the side of the coronal imbalance to the opposite side. From both sides, the inferior cut progresses from posterior/caudal to anterior/cephalad, to correct the sagittal imbalance after osteotomy closure. The difference between the heights of the two lateral resections of the wedge gives approximately the coronal correction. Once the asymmetric wedge is obtained, the corresponding lateral walls are removed with a rongeur or with appropriate chisels, and the posterior vertebral wall is resected or imploded between the osteotomy lines. The closure of the osteotomy can now be performed through the flexion of the table, in case a Jackson table is used, or gently pushing on the pedicle screws immediately cranial and caudal to the osteotomy level. This last technique is, however, the less preferable, since the risk of pull-out is high especially in old osteoporotic patients. New techniques to close osteotomies have been proposed, as sublaminar band-assisted closure, to reduce the risk of hardware mobilization [5]. In case a cantilever maneuver is deemed necessary, it should be performed loading simultaneously groups of anchors and not individual anchors at both sides of the osteotomy. The domino technique (two independent rods), one in the caudal and one in the cephalad side of the osteotomy engage as many screws as possible in the side opposite to the coronal imbalance; each rod permits manipulation of a segment of the spine. Connecting them with a domino connector and compressing simultaneously corrects coronal and sagittal imbalance. The contralateral rod is inserted thereafter to complete the construct. After osteotomy closure, a lateral fluoroscopy can be compared with a similar fluoroscopy obtained before the osteotomy to calculate the degrees of sagittal correction, while an AP full spine film can evaluate the coronal correction. In case a full spine radiograph is not feasible, an inverted cross made with two metallic rods, one parallel to the sacral endplate or iliac crests (with c-arm verification) and the second perpendicular to it at the midpoint of the sacrum can be used as a reference; when a correct coronal alignment is obtained, the vertical rod passes on the T1 spinous process, that can easily be palpated.
Case studies
Three cases are here reported on combined coronal and sagittal malalignments in which an asymmetric PSO were performed in the lumbar region to restore a correct balance of the spine.
The first case (Fig. 3a–d) is represented by a 51-year-old female suffering from disabling low back pain. Preoperative full standing X-rays (Fig. 3a–b) showed a coronal imbalance with a shift of C7 plumbline of 10 cm to the right side associated to a positive C7 plumbline of 17 cm on the sagittal plane. The apex of the kyphotic deformity corresponded to L1. Pelvic parameter measurements showed a pelvic incidence (PI) of 44°, a pelvic tilt (PT) of 24°, and a sacral slope (SS) of 10°. These values underlined dramatic pelvic retroversion, since the ideal value of PT should have been of 9°, according to Vialle’s rule [6]. The spinal parameters were lumbar lordosis (LL) 12° and thoracic kyphosis (TK) 11°. Both these values were diminished in respect to their theoretic values, since LL should have been of 54° and thoracic kyphosis of 44. This patient was enclosed in the Lumbar Kyphosis category, according to Lamartina–Berjano sagittal imbalance classification [2]. An asymmetric L3 PSO and a T9-pelvis fusion were indicated. An anterior support below the osteotomized vertebra was obtained through an XLIF approach. The authors routinely perform interbody fusion with cages and autologous graft below, above, or on both the adjoining levels when performing a PSO, to increase the stiffness of the anterior column and reduce the risk of pseudarthrosis. When the surgery was completed, a complete correction of the coronal and sagittal balance was obtained (Fig. 3c, d). PT was reduced to 3°; LL reached a value of 70°, and thoracic kyphosis spontaneously increased to 65°. Since a large correction was obtained, a four-rod technique was used to increase the resistance of the instrumentation. The patient was able to walk in postoperative day (POD) #2, and was discharged in POD #8.
AP and lateral preoperative X-rays (a, b) of a 51-year-old female suffering from combined sagittal and coronal malalignment. Observe in postoperative X-rays (c, d) how a T9-pelvis fusion with an L3 asymmetric PSO and an intersomatic XLIF fusion at L3–4 level corrected spinal alignment on both planes. A four-rod technique was applied
The second case (Fig. 4a–d) is a 63-year-old female with a coronal and sagittal imbalance (Fig. 4a, b), suffering from back pain and neurogenic claudication. The AP full standing X-ray shows a left coronal imbalance due to a lumbar scoliosis, while the lateral X-ray underlines a thoracolumbar kyphosis with a significative pelvic retroversion (PI = 64°, PT = 38°, ideal PT = 17°). This patient was classified as a Lumbar Kyphosis, according to Lamartina–Berjano’s classification, and a short fusion with an asymmetric PSO was indicated. A T9-pelvis fusion with an asymmetric PSO of L3 was performed, with a correction of both the coronal and the sagittal alignments. After the surgery (Fig. 4c, d), PT reached the value of 17°, LL was 72°, and thoracic kyphosis spontaneously increased to 64°. The patient was standing at POD #2 and discharged at POD #10. No intraoperative or postoperative complications occurred.
Preoperative (a, b) and postoperative (c, d) AP and lateral X-rays of a 63-year-old female with a coronal and sagittal imbalance, suffering from back pain and neurogenic claudication. A T9-pelvis fusion with an asymmetric PSO of L3 was performed, with a correction of both the coronal and the sagittal alignments
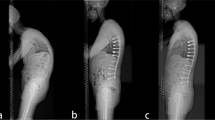
The third case regards a 56-year-old female that had a lumbar degenerative scoliosis with sagittal imbalance. The patient was first with a T10-S1 instrumented fusion (Fig. 5a, b), with new onset of coronal imbalance despite partial correction of the scoliosis and persistence of sagittal imbalance. This was due to a partial fusion of the lower lumbar spine and an insufficient correction of the lumbar lordosis. With a PI of 44°, the patient still had a pelvic retroversion (PT = 15°, ideal PT = 9°) and a hypolordosis of the lumbar region (LL = 39°, ideal LL = 54°). The preoperative planning was the following: a correction of the coronal and sagittal alignment through a revision of the instrumented fusion with an L4 asymmetric PSO and an L3-4 XLIF, as L4-L5 was fused. This surgery allowed a complete restoration of the coronal balance, an increase of the lumbar lordosis to 53° and a complete correction of the PT to a value of 8° (Fig. 5c, d).
Discussion
When combined fixed coronal and sagittal imbalance is present, asymmetric PSOs are an optimal choice to correct deformity on both planes. In a prospective paper, Toyone et al. [7] analyzed 14 patients who underwent corrective asymmetric PSO. The findings were that this technique provided an appreciable correction of the scoliosis and a correction of lumbar lordosis using a convex-sided posterolateral wedge resection. The mean reduction of lumbar curves was of 28° and the average restoration of lordosis was 39°, underlining the efficacy of the procedure. Further on, a significant improvement in back pain scores was noticed, since the values passed from an average score of 61 ± 28 before surgery to 9 ± 4 at the final follow-up. Very few papers in literature managed asymmetric osteotomies, because of the relatively infrequence of combined sagittal and coronal imbalance and the technical difficulty in performing this particular kind of osteotomy. Asymmetric PSO is, however, a valid alternative to vertebral column resection (VCR), a technique reserved for complex deformities, like those on both coronal and sagittal planes. VCR is a powerful technique, providing a huge correction on both planes, but needs great technical capacities and presents greater risks in terms of neurological injury, intraoperative complications, showing at the same time the highest length of surgery [8, 9]. VCR can also need a double anterior and posterior approach, since the posterior VCR (PVCR) is a demanding procedure also in expert hands. In both cases, VCR or PVCR require an anterior support like an expandable cage to restore the integrity of the anterior column, with all the possible related complications such as hardware failure or subsidence and pseudarthrosis. For these reasons, asymmetric PSO is considered a valid alternative to such an invasive procedure as VCR, showing, however, adequate corrective properties of deformities on both sagittal and coronal planes. Some papers on asymmetric PSO series and technical description [7, 10] and an interesting OOT video [11] can further illustrate this particular and rarely performed osteotomy.
Conclusion
When a combined coronal and sagittal deformity disrupts the normal alignment of the spine, asymmetric PSO is a valid technique to restore an adequate balance. The asymmetric wedge has to be lower in the side of coronal imbalance. This allows the restoration of both coronal and sagittal alignment after osteotomy closure. An adequate preoperative planning and intraoperative verification of the correction achieved are mandatory, to obtain the necessary correction. The few studies present in literature show good results in terms of correction, even if the difficulty of this technique is certain.
References
Thomasen E (1985) Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res 194:142–152
Lamartina C, Berjano P (2014) Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J 23:1177–1189
Berjano P, Lamartina C (2014) Classification of degenerative segment disease in adults with deformity of the lumbar or thoracolumbar spine. Eur Spine J 23(9):1815–1824
Lamartina C, Berjano P, Petruzzi M, Sinigaglia A, Casero G, Cecchinato R, Damilano M, Bassani R (2012) Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J 21(Suppl 1):S27–S31
Berjano P, Cucciati L, Damilano M, Pejrona M, Lamartina C (2013) A novel technique for sublaminar-band-assisted closure of pedicle subtraction osteotomy. Eur Spine J 22(12):2910–2914
Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. JBJS 87(2):260–267
Toyone T, Shiboi R, Ozawa T et al (2012) Asymmetrical pedicle subtraction osteotomy for rigid degenerative lumbar kyphoscoliosis. Spine (Phila Pa 1976) 37(21):1847–1852
Gill JB, Levin A, Burd T et al (2008) Corrective osteotomies in spine surgery. J Bone Joint Surg Am 90:2509–2520
Suk SI, Chung ER, Kim JH et al (2005) Posterior vertebral column resection for severe rigid scoliosis. Spine 2(30):1682–1687
Thambiraj S, Boszczyk BM (2012) Asymmetric osteotomy of the spine for coronal imbalance: a technical report. Eur Spine J 21(Suppl 2):S225–S229
Obeid I, Laouissat F, Vital JM (2013) Asymmetric T5 pedicle subtraction osteotomy (PSO) for complex posttraumatic deformity. Esut Spine J 22:2130–2135
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cecchinato, R., Berjano, P., Aguirre, MF.I. et al. Asymmetrical pedicle subtraction osteotomy in the lumbar spine in combined coronal and sagittal imbalance. Eur Spine J 24 (Suppl 1), 66–71 (2015). https://doi.org/10.1007/s00586-014-3669-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3669-0