Abstract
Introduction
Sagittal imbalance is a spine deformity with multifactorial etiology, associated with severe low back pain and gait disturbance that worsen deeply patients’ quality of life. The amount of correction achievable through PSO is limited by the height of the resection of the posterior wall, causing a ceiling of segmental correction of 30–35°. The aim of this study is to describe and preliminarily evaluate the results of an alternative technique, corner osteotomy (CO), that can increase the amount of correction.
Materials and methods
From March 2012, every patient examined in our Division, diagnosed with sagittal imbalance to be treated with PSO, underwent CO and fusion. This technique consists in removing the posterior vertebral arch, the pedicle and the posterior–superior corner of the vertebral body; the inferior endplate of the vertebra above is prepared and the superior adjacent disc removed to obtain, when closing the osteotomy, a direct interbody fusion. Ten patients undergoing CO were compared with 20 patients undergoing PSO regarding spinopelvic parameters, operative variables, complications and degree of correction.
Results
Patients undergoing CO obtained higher lordotic angle at the osteotomy than patients undergoing PSO (36.6° ± 8.2° vs 16.5° ± 9.5°, p < 0.001) and had lower postoperative PT and SVA and higher average increase in lordosis. Complications were similar between groups. A trend toward longer surgical time, greater bleeding and higher transfusion rate was observed in the CO group, though this finding could be related to higher complexity of cases or incidence of associated anterior approach.
Discussion and conclusions
Corner osteotomy technique was more effective than the PSO in increasing segmental and lumbar lordosis with modest increase in blood loss and similar complication rate. The CO technique, in addition, proved a good reproducibility. Further studies with larger populations should confirm these preliminary results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Global spinal balance and its relationship to the pelvis have received much more attention since recent studies have shown that sagittal plane alignment correlates closely with disability and quality of life [1]. Sagittal misalignment has been shown to be an independent predictor of outcome in almost all scenarios of adult spinal pathology [2–5]. Because of longer expectations of life and demands for better quality of life during aging, adult deformity surgery is an expanding field, associated with an important increase in the number of candidates for deformity correction. For these reasons in the last decade, major effort has been made to increase knowledge in this field. It has been demonstrated that this extensive surgery, previously considered to have poor balance between risk and outcomes, causes a dramatic increase in health-related quality of life [6], with the greatest improvements in health-related quality of life (HRQoL) in the oldest age group.
Recent studies have demonstrated that failure to restore normal sagittal alignment in patients primarily operated for reasons other than deformity results in unacceptably high rates of poor results and revision surgery [7–9]. Thus, surgical planning should consider sagittal alignment in every patient and anticipate the impact of any planned surgery on sagittal balance. Normative values for spinal balance parameters [10, 11], equilibrium between these parameters [12] and outcome follow-up studies regarding the contribution made by the correction of some of these parameters now enable a pre-operative surgical planning that reliably produces good results [6, 13]. PSO is the most frequent procedure in the treatment of patients with severe sagittal misalignment. It has been described to provide corrections on average 25° though technical modifications can increase the amount of correction to 30° or 35°. The ceiling of angular correction of standard PSO depends on the geometrical relationship between the length of the vertebral body and the height of the posterior wall that can be resected within the vertebra, usually from the upper endplate to some millimeters below the inferior edge of the pedicle.
In this paper we describe the corner osteotomy (CO), a modified PSO technique that increases the amount of sagittal correction within the vertebra, and present preliminary results.
Patients and methods
Design
Retrospective cohort with historical controls.
Patients
The first 10 consecutive patients operated with the CO technique in a center with high case load (80 tricolumnar osteotomies per year) formed the study group. The control group was formed by the previous last 20 patients with similar pathologies operated with standard decancellation PSO technique, both for sagittal malalignment.
Analysis
For all patients, the following spinopelvic alignment parameters were measured pre- and post-operatively: pelvic incidence (PI), pelvic tilt (PT), lumbar lordosis (LL), thoracic kyphosis (TK), and sagittal vertical axis (SVA). Changes in PT, LL and SVA were recorded and compared between groups. Blood loss, surgical time, transfusions and complications were obtained from the clinical charts and follow-up visits. The primary outcome measure was the increase in lordosis obtained at the level of the osteotomy between pre- and post-operative. Comparisons between variables with non normal distribution were made with the non-parametric Mann–Whitney U Test. Significance threshold was set at p < 0.05.
Surgical technique
Under general anaesthesia, the patient is placed prone on a Jackson table, allowing for abdominal decompression and for reverse break of the table at the level of the osteotomy, to assist in its closure. Standard skin preparation and exposure are made in the area to be instrumented. Neuromonitoring is performed as dictated by the protocol of the hospital. As usual in any PSO technique, it is advisable to extend the instrumentation at least two levels above and below the osteotomized vertebra. In case the fusion area includes S1, the authors prefer to routinely include iliac bolts in the instrumentation. After complete subperiosteal exposure, reaching bilaterally the tips of the transverse processes, and insertion of pedicle screws, the rods are cut and pre-bent to reduce the time to closure of the osteotomy after it has been performed. The choice of the rod must take into account the high mechanical demand on it, and a large diameter (6 or 6.35 mm) titanium rod or a 5.5 mm CoCr titanium alloy can be preferable. It is also important to avoid damage to the rod, avoiding sharp contouring, repeated contouring and reverse-contouring in the same region and, specially, the use of in situ benders, as they tend to leave marks in the rod that behave as stress risers favoring rod breakage after cycles of load. For better understanding, an L4 CO will be described.
As a ruler of thumb, in an L4 corner osteotomy, the rod usually has to be bent nearly 90° (or even more, depending on the final correction needed) to appropriately engage the iliac, S1, L5, L3 and L2 screws. After contouring, chisels are used to excise the inferior facets of L4 and L3 bilaterally and a rongeur is used to excise the spinous processes of L3, L4 and L5. Complete resection of the arch of L4, yellow ligaments between L3 and L5 and the superior facet joints of L4 and L5 follows. The ventral capsule of the facet joints of L3–L4 and L4–L5 is freed to bilaterally expose the L3 and L4 roots in the foramina. Bleeding usually is intense in the foraminal area and can be controlled by cautious use of bipolar coagulation or with hemostatic agents. Once the exposure is completed, the only remaining posterior elements of L4 are the pedicles that at this point are resected with a rongeur to the point where they meet the posterior wall (Fig. 1). The base of the transverse processes is cut with a Kerrison or an osteotome. With a small Cobb elevator the psoas muscle and the lumbar plexus are carefully dissected laterally from the upper half of the lateral wall of the vertebral body. Care is taken to avoid in this maneuver damage to the segmental vessels and the lumbar plexus. A large leaf of Surgicel is inserted between bone and soft tissue as protection. At this point, the surgeon has control on the lateral wall of the osteotomized vertebra. Then, the ventral dura is mobilized from the posterior longitudinal ligament and again bipolar coagulation is used to control bleeding. Mobilization of the dura to expose medially the L3–L4 disc is possible. The posterior annulus is excised with a scalpel. The posterior annulotomy is extended laterally to the lateral annulus while protecting the exiting L3 root that is retracted cranio-laterally (Fig. 2). This maneuver will allow for easy extraction of the lateral wall fragment after the osteotomy. With shavers and curettes (as usual for PLIF), all the disc is carefully excised bilaterally in all its width and length, and the endplate of L3 is carefully prepared for fusion, with resection of all the endplate cartilage. This will favor fusion between the endplate of L3 and the spongiosa of L4 below the osteotomy. Once this step is completed, a shaver or rongeur is inserted deep into the L3–L4 disc space (Fig. 3). This will serve as a reference for the direction of the endplate and to align the osteotomy plane with the desired angle. At this point the osteotomy is performed. The assistant retracts the L4 root medially and caudally and the lumbar plexus laterally to the vertebral body. A 10–15 mm wide osteotome is placed horizontally usually below the lower margin of the pedicle. Using as a reference the instrument in the disc space, the planned angle of osteotomy is reproduced. This usually results in an osteotomy plane intersecting in the upper endplate of L4. A 30° to 35° osteotomy is performed starting just below the lower limit of the pedicles and reaching the L4 endplate at the union of the posterior 2/3 and the anterior 1/3 of its length. After this first cut, a vertical cut is made medially to the pedicle. This permits mobilizing and extracting the first fragment of bone (Fig. 4). The same procedure is repeated more medially to complete the osteotomy of one-half of the vertebral body. Subsequently, a hemostatic agent is placed in the bone defect and the same procedure is repeated contra laterally. At the end of the contralateral resection a thin bone bridge can remain in the midline. In this case, the surgeon can decide to resect it with the osteotome from one side or by decancellation and impaction of the remaining posterior wall. Once the osteotomy is completed (Figs. 5, 6), it is closed by reverse break of the table and assisted by manual force carefully applied to the spine in anterior direction. The preserved anterior annulus and longitudinal ligament act as a hinge and anterior tension band, and prevent dislocation of the spine. In case additional closure is necessary, a cantilever maneuver can be carefully performed by bilaterally securing the pre-bent rods in L5, S1 and the ilium and applying force simultaneously to both rods. During reduction, the L3 and L4 roots and the sac are visualized bilaterally to avoid impingement. Care must be taken to maintain manual pressure on the rods until at least 2 + 2 proximal screws have been engaged to prevent pullout of screws. A lateral image of S1, the osteotomized vertebra and L1 is taken (by parallel translation of the C-arm to measure the angle of lordosis and to verify that the goal of alignment has been achieved). Thorough lavage, final hemostasis, preparation of the intertransverse fusion bed and application of graft complete the procedure.
After bilateral resection of the corner and excision of the bone bridge remaining between the two defects, a pituitary rongeur can be passed side to side. The completeness and smoothness of the osteotomy plane is verified as well as its angle before closure. Attention to resection of the lateral walls should be paid to avoid difficulties in closure of the osteotomy
The authors prefer to systematically include an interbody fusion below the osteotomized vertebra (in this case at L4-L5) with autologous graft and a cage. Our preference is to perform a direct trans-psoas approach at the end of the procedure in the same anaesthesia. This achieves interbody fusion with a large footprint cage and minimal blood loss. Additionally, implanting the cage after the closure of the posterior construct results in compression between the L3 lower endplate and the spongiosa of L4, increasing the chance of interbody fusion.
Results
Patients in the corner osteotomy and PSO groups had similar spinopelvic parameters pre-operatively (Table 1). The CO group included more revision cases (60 vs 30 %) and was more frequently associated with an anterior approach in the same anaesthesia (40 vs 5 %). Thoracic kyphosis was higher pre-operatively in the PSO group. The diagnoses at the index procedure were similar and are summarized in Table 2.
Patients with corner osteotomy had greater increase in lordosis at the osteotomized level (36.6° vs 16.6°, p < 0.001). They had lower postoperative pelvic tilt, and lower postoperative SVA.
The increase in lumbar lordosis and the decrease in SVA was also greater in the CO compared to the PSO group (Table 3). A trend versus a longer procedure, longer stay, higher blood loss, and higher transfusion rate was observed though differences were not statistically significant (Table 4). Minor complications in the PSO group were two dural tears, one case of temporary unilateral hip flexor weakness, and one case of uniltareral extensor hallucis longus weakness that recovered within 6 months of surgery. In the CO group minor complications included two cases of abdominal pain that resolved spontaneously, one case of temporary unilateral quadricipital weakness and one case of temporary unilateral limitation for ankle dorsiflexion. Almost all patients in both groups presented with postoperative anemia.
Major complications in the PSO group included 2 revisions for misplaced screws within 90 days of surgery, and 2 rod failures requiring revision within a year and 2 years postoperatively, respectively. To date, an additional six patients have undergone revision arthrodesis. In the CO group there was one case of infection that required a revision surgery the same year, one revision for misplaced screws within 10 days of surgery, and one revision surgery for rod breakage. To date, another three patients have undergone revision arthrodesis.
Figures 7, 8 and 9 show three different sample cases.
A 75-year-old female suffering from severe back pain and claudication. Pre-operative full spine radiograms showed severe sagittal imbalance (SVA >200 mm). Correction was achieved by CO in L4 and fixation and fusion T4-pelvis. CO obtained 53° of correction at the osteotomy site; total lumbar correction was 69°
Discussion
Insufficient correction in sagittal realignment procedures is a frequent cause of failure and reoperation. PSO can provide corrections of as much as 30° or 35° in a single vertebra, though in the authors’ experience, in many cases much more modest corrections are effectively achieved. In this study, the average correction with PSO procedures performed by an experienced surgeon that had passed the phase of learning curve was 16.5° ± 9.5, reflecting that it is not uncommon to obtain small corrections. It is interesting to note that the surgical risk in a PSO procedure with poor closure of the osteotomy and modest correction is nearly the same as that in a PSO with high correction.
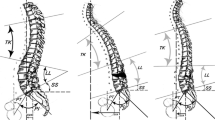
The main limiting factor of the ability to obtain a large correction with PSO is the amount of the posterior wall of the vertebra that can be resected. In fact, though it is easy to resect the posterior wall between the upper endplate and 3–4 mm below the lower edge of the pedicle, extending the resection far below is difficult due to the presence of the exiting roots that run horizontally below the pedicle. The different shape of CO (Fig. 10) determines a substantially greater correction with the same resection in height of the posterior wall. The results of this preliminary description show how the angular correction at the osteotomy is on average 20° higher (with cases of as much as 56° of correction at a single level), resulting in better postoperative alignment that reflects in lower PT and SVA.
Comparison between the shapes of PSO and CO. In a classical PSO, the osteotomy extends from the posterior to the anterior wall of the vertebra. In CO, the osteotomy extends from the posterior wall along the posterior 2/3 of the vertebral body in length. With a posterior height of the same dimensions, the resulting angle is substantially changed. In addition, the CO resects the disc, resulting in an increase in the height of the osteotomy and consequently an increase in angular correction. An anterior hinge is formed by the anterior longitudinal ligament and annulus, preventing sagittal translation
As the patients treated in the CO group were more recent it could be argued that these procedures were performed by more skilled surgeons. Though an historical improvement cannot be excluded, the PSO cases were performed by a single surgeon who had previously performed more than 200 such procedures; whereas the CO were performed by the same surgeon and a less experienced one, and reflect the first CO cases of both, thus including their learning curves in this technique. Surgical time, bleeding and transfusion tended to be higher in the CO, but these cases tended to be more complex with higher proportion of revision cases and combined posterior and anterior procedures.
The CO procedure shows in this preliminary report a similar risk profile to PSO, with matching incidence and type of complications.
One of the potential advantages of CO is that it promotes direct interbody fusion at the upper disc space. Though this aspect has not been assessed in this study, it could correlate with a reduction in the risk of pseudarthrosis and rod breakage [14].
Some alternatives have been proposed to increase the amount of correction of PSO, including cuneiform resection of the disc above or below [15] or closing–opening osteotomies [16]. These techniques require more extensive nerve tissue retraction or direct osteotomy of the anterior wall of the vertebral body that could result in visceral or vascular damage or uncontrolled vertebral translation.
To our knowledge, this is the first detailed description of a modality of PSO that increases sagittal correction by directing the plane of osteotomy to a point posterior to the anterior cortex of the vertebral body and resecting the disc. With this shape, the osteotomy permits gentle anterior opening with a hinge dorsal to the anterior longitudinal ligament, that acts as a stabilizing tension band, and posterior closing, resulting in increased power of correction. This article describes the technique in detail and presents preliminary results that compare favorably to the standard PSO. Since the first case, the authors have performed over 50 cases of CO, and the technique has confirmed to provide excellent correction without increased complications.
In conclusion, corner osteotomy is a valid alternative to classical PSO, allowing easier achievement of the correction goals, direct interbody fusion at the upper disc space and a similar safety profile.
References
Lafage V, Schwab F, Patel A et al (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34:E599–E606
Smith JS, Shaffrey CI, Berven S, Glassman S, Hamill C, Horton W, Ondra S, Schwab F, Shainline M, Fu KM, Bridwell K (2009) Improvement of back pain with operative and non operative in adults with scoliosis. Neurosurgery 65:86–93
Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab FJ, Hamill CL, Horton WC, Ondra SL, Sansur CA, Bridwell KH (2011) Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine 36:817–824
Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ (2009) Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine 34:785–791
Mi Kyung K, Sun-Ho L, Eun-Sang K, Whan E, Sung-Soo C, Chong-Suh L (2011) The impact of sagittal balance on clinical results after posterior interbody fusion for patients with degenerative spondylolisthesis: a pilot study. BMC Musculoskelet Disord 12:69. doi:10.1186/1471-2474-12-69
Lamartina C, Berjano P, Petruzzi M, Sinigaglia A, Casero G, Cecchinato R, Damilano M, Bassani R (2012) Criteria to restore sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J 21:27–31
Jackson RP, McManus AC (1994) Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine 19:1611–1618
Lazennec JY, Ramaré S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9:47–55
Mehta VA, Amin A, Omeis I, Gokaslan ZL, Gottfried ON (2012) Implications of spinopelvic alignment for the spine surgeon. Neurosurgery 70:707–721
Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15:415–422
Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P (2010) Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine 35:1193–1198
Schwab F, Lafage V, Patel A, Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine 34:1828–1833
Roussouly P, Nnadi C (2010) Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19:1824–1836
Berjano P, Bassani R, Casero G, Sinigaglia A, Cecchinato R, Lamartina C (2013) Failures and revisions in surgery for sagittal imbalance: analysis of factors influencing failure. Eur Spine J. doi:10.1007/s00586-013-3024-x
Enercan M, Ozturk C, Kahraman S, Sarıer M, Hamzaoglu A, Alanay A (2012) Osteotomies/spinal column resections in adult deformity. Eur Spine J 22(Suppl 2):S254–S264
Chang K, Cheng C, Chen H, Chang K, Chen T (2008) Closing-opening wedge osteotomy for the treatment of sagittal imbalance. Spine 33(13):1470–1477
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berjano, P., Pejrona, M., Damilano, M. et al. Corner osteotomy: a modified pedicle subtraction osteotomy for increased sagittal correction in the lumbar spine. Eur Spine J 24 (Suppl 1), 58–65 (2015). https://doi.org/10.1007/s00586-014-3618-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3618-y