Abstract
Purpose
To present in a single source the relevant information needed to assess spinopelvic balance and alignment, and to estimate the amount of correction needed in a patient during surgical treatment.
Methods
Narrative literature review
Results
Sagittal balance can be evaluated by global balance estimates (sagittal vertical axis and T1 tilt). Other important parameters are the relationship between pelvic incidence and lumbar lordosis (spinopelvic harmony), between pelvic incidence and difference of thoracic kyphosis and lumbar lordosis (spinopelvic balance), excess of pelvic tilt, knee flexion and thoracic compensatory hypokyphosis. Different methods to calculate the amount of surgical correction needed in patients with sagittal imbalance have been based on combinations of these parameters.
Conclusions
Relevant parameters of sagittal imbalance have been identified and correlated with clinical outcomes. Methods for calculation of surgical correction of imbalance have been proposed, but not validated in patients with mid-term follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sagittal imbalance is a complex clinical entity causing pain and disability. Surgical correction of sagittal imbalance is technically challenging, and burdened by frequent and often significant complications. Calculation of the amount of correction needed by a given patient has been addressed in different ways, and is based on the comprehension of spinopelvic morphology, the relationships among its parameters, and of compensating mechanisms. The present paper aims to present in a single source the relevant information needed to assess spinopelvic balance, alignment and compensatory mechanisms and to estimate the amount of correction needed in a patient during surgical treatment.
Design
Current concepts review.
Methods
Literature review included Medline database search (1970–2011) with the following search strategy: (sagittal [All Fields] AND “balance” [All Fields]) OR (sagittal [All Fields] AND imbalance [All Fields]) AND (“spine” [MeSH Terms] OR “spine” [All Fields]).
One author reviewed the titles and abstracts of the 565 papers identified, and selected articles containing relevant information to define parameters for assessment of sagittal balance, methods to calculate the amount of needed correction and clinical validation data of both. Relevant papers in the authors’ database and from other relevant papers’ reference list were also included.
Results
Definition of sagittal balance
Sagittal balance is a situation where the individual is able to maintain a stable standing position with minimal muscle effort. Sagittal balance is the result of the interaction of bone morphology (mainly pelvic and vertebral morphology), disc and ligaments mechanical behavior, muscle strength and resistance, and ability to introduce compensating mechanisms.
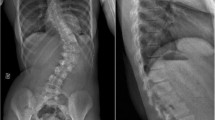
Sagittal balance can be evaluated by a number of metric or angular parameters. Global sagittal balance is more frequently evaluated by sagittal vertical axis (SVA) [1] measuring the distance from the C7 plumb line to the posterior corner of the S1 endplate. Patients with SVA more than 50 mm from S1 are more likely symptomatic and have higher disability scores than patients with SVA < 50 mm [1]. Another global alignment parameter is T1 spinopelvic inclination, which, though is less frequently used in clinical setting, correlates even better than SVA with patients outcomes [1].
Pelvic parameters and compensatory mechanisms
There is a continuum from the normal condition of sagittal balance, through sagittal compensated imbalance to the pathological condition of sagittal imbalance. The balanced extreme of this line is represented by a subject with such an alignment that allows for standing with no muscle effort. The imbalanced extreme is represented by an individual failing to maintain the standing position without a cane, because his muscle strength or resistance are not enough to, within the positions allowed by his joints’ range of motion, keep standing. Subjects with less efficient alignment, requiring active compensation (which relies always on muscular effort) through compensatory lordosis, hypokyphosis, pelvic retroversion or knee flexion are intermediate points in the continuum.
Pain emerging from diseased joints or discs or from nerve encroachment is well known. Other than this causes of pain, subjects with imperfect sagittal balance can present pain and disability due to the excessive muscle effort needed to keep the upright position. When the muscle effort necessary to keep the standing position is low as compared to the individual’s ability to exert muscle activity for a time, we can expect the subject to be relatively asymptomatic. When the effort needed to compensate is high compared to the physical condition of the subject, symptoms from muscle overload will probably develop.
That a sagittally balanced spine should have enough lordosis and not too much kyphosis is rather intuitive. Attempts to determine normative data for the amount of lumbar lordosis or thoracic kyphosis have soon shown that these parameters are highly variable and that it is not possible to establish an interval for what normal lordosis or kyphosis is [2]. Introduction of the shape of the pelvis as a key parameter in an individual’s sagittal alignment evaluation has allowed us to better understand what a normal alignment is. The key parameter to describe pelvic shape related to sagittal balance is pelvic incidence (PI) [3]. Pelvic incidence is an angular parameter which reflects the sagittal length of the pelvis from the sacral endplate to the center of the hips. It is an anatomical constant for each individual that cannot be modified after skeletal maturity (unless the shape of the pelvis is modified by trauma or surgery). Pelvic incidence values show a high variability between individuals, ranging from 30° to 80° both in symptomatic and asymptomatic individuals [2, 4]. The amount of pelvic incidence is not a predictor of clinical outcomes. Instead, the amount of pelvic incidence has demonstrated a good correlation with lumbar lordosis [4].
Whereas pelvis sagittal morphology is defined by pelvic incidence, pelvic orientation in the sagittal plane (depending of the amount of forward or backward rotation of the pelvis around the hip joints) can be measured by pelvic tilt (PT) [3]. A higher pelvic tilt means that the pelvis is more retroverted. A lower pelvic tilt means that the pelvis is anteverted. An anteverted pelvis is energy saving because it brings the loading axis of the trunk on the pelvis (through the sacral endplate) closer to the loading axis of the pelvis on the lower limbs (through the hip joints), diminishing the torque [5] of both vectors (ground reaction force through the hips and trunk weight through the sacrum), which must be neutralized by muscle contraction.
As pelvic retroversion causes a more horizontal sacral endplate and a more posterior basement of the spine, it helps to compensate a forward displacement of the spine. So, pelvic retroversion is an energy consuming mechanism of compensation of imperfect sagittal balance.
A third pelvic angular parameter, sacral slope (SS), is a measure of pelvic orientation [3]. There is an arithmetic relationship between sacral slope and pelvic tilt for a given subject: PI = SS + PT. Thus, pelvic tilt and sacral slope are two equivalent ways to measure pelvis orientation in the sagittal plane.
The concept of spinopelvic balance
Although pelvic incidence, pelvic tilt and lumbar lordosis are extremely variable between subjects, for a given individual, there is a close relationship between these parameters. Lumbar lordosis can be very exactly predicted for an asymptomatic individual as a function of pelvic incidence, sacral slope and thoracic kyphosis [4]. Another study [6] on asymptomatic adults, proposed that lumbar lordosis could be predicted by the formula LL = PI + 9°. The same group of researchers demonstrated on a study on 125 operated subjects that those with lumbar lordosis not matching their own pelvic incidence (LL < PI + 9°) had higher probability of having poor clinical outcomes [1]. This concept has been referred to as “spino-pelvic harmony”. Spinopelvic harmony, as an alignment in which lumbar and thoracic shapes are proportional to pelvic shape has shown to better interpret how a normal sagittal alignment is achieved.
When describing pelvic retroversion, we stated that higher pelvic retroversion is more energy consuming and that increased muscle effort for standing is a cause of pain and disability. If this was true, one could expect worse clinical results in patients with increased pelvic retroversion. This has been experimentally demonstrated by Schwab et al. who in 125 subjects with adult deformity found a correlation of higher pelvic tilt with poorer health related quality of life [1]. The threshold for improved clinical outcomes was identified at 20° of pelvic tilt, with lower pelvic tilt corresponding to better clinical outcomes.
Clinical impact of sagittal imbalance
Sagittal imbalance is a significant cause of morbidity in adults and elderly. In unoperated adult deformity patients, sagittal imbalance correlates better with pain and disability than coronal deformity or coronal imbalance do [7]. Postoperative sagittal balance has been demonstrated to be an independent predictor of surgical result in adult deformity cases [8] and in short spinal fusion for degenerative disease [9], in terms of health related quality of life. Surgical correction of adult deformity, and specifically in the elderly, has demonstrated to improve health related quality of life and pain, being final sagittal balance a strong predictor of outcome, opposed to the lower predictive value of residual coronal misalignment [10–12]. Clinical outcomes improvement has also been demonstrated after surgical correction of sagittal imbalance [13].
Still, adult sagittal deformity surgery is challenging [14], with frequent complications and postoperative events [10, 11]. Insufficient correction of the sagittal deformity [8], decompensation [15] or even excessive correction [16] can jeopardize clinical result and make necessary repeat surgery. Insufficient correction of the C7 plumbline has been reported to be as high as 45% at 2-year follow-up [13]. One of the most challenging aspects of adult deformity surgery is preoperative calculation of the amount of necessary correction to be achieved during surgery.
Recently, Neal et al. [17] have suggested a new parameter to evaluate spinopelvic balance. They calculated from normative values in literature a spinopelvic constant, which is the quotient between pelvic incidence and the number of degrees that lumbar lordosis exceeds thoracic kyphosis. The value resulting from asymptomatic adult patients (18–60 years old) was different from the value for asymptomatic elderly patients (over 60), reflecting natural trend toward loss of lumbar lordosis. Spinopelvic balance was measured as the difference between the excess of lordosis measured in a patient and the predicted excess of lordosis, calculated from pelvic incidence and age-related spinopelvic constant. Interestingly, when they compared the outcomes of operated patients, they found that patients with spinopelvic balance in the interval (0°, +10°) had better outcomes in SRS score, ODI score and SF12 PCS score. Best scores were found in patients with both spinopelvic balance and sagittal balance (measured as deviation of C7 plumbline from S1). Patients with both spinopelvic and sagittal imbalance had the worst scores, while patients with either sagittal or spinopelvic balance had intermediate scores.
Methods for calculation the amount of correction needed
Several methods have been proposed to preoperatively estimate the amount of needed correction. Ondra et al. [18] defined a trigonometric method to calculate the amount of required correction to displace the C7 plumbline to the posterior corner of S1 endplate, and found it reliable in all but 2 patients out of a series of 15 patients. The method did not consider pelvic parameters and the calculation proposed was a sort of approximation to the true geometry of correction by pedicle subtraction osteotomy (PSO), were the rotation hinge for correction is placed at the anterior wall of the vertebra (instead, they calculated the amount of needed correction with an angle with apex in the posterior aspect of the vertebra). Although the method seemed to be reliable in the reviewed patients, length of follow-up was not reported. Long-term loss of correction has been observed in other series and could be a reason to consider that the reported accuracy of the trigonometric method is overestimated.
The same year, Yang and Ondra [19] published a second paper (submitted second, published first), addressing the error of the first trigonometric method, and suggesting an exact method to calculate the needed degree of correction. Apex of the estimated angle was placed at the apex of operative correction for PSO, so that the calculation can be exact. The method did not consider pelvic parameters (pelvic incidence or compensation suggested by pelvic tilt). In the cases analyzed, they found that the error of the trigonometric method was within few (<3°) degrees of the exact method.
Less intuitive is the method proposed by Aurorer et al. [20]. They introduced several important refinements: after first calculating the amount of required correction by osteotomy (or osteotomies) to translate the head over the sacrum, they calculated the amount of increased pelvic tilt (difference between measured pelvic tilt and predicted pelvic tilt, following the criteria of Vialle et al. [21], and added extra lordosis to correct this parameter, as they did for the angle of femur obliquity (reflecting increased pelvic tilt after full hip extension). Finally, if the patient had a flexible thoracic spine compensating by hypokyphosis, they suggested to plan an extra increase of lumbar lordosis as a postoperative increase of thoracic kyphosis could be anticipated in such cases.
Le Huec [22] proposed a different approach to calculate the amount of correction needed. The full balance integrated (FBI) method is based in calculation of the sum of three angles:
-
Angle of C7 translation (C7TA). Is equivalent to the angle of translation calculated in Ondra’s exact method (defined by three points: C7 center, apex of the osteotomy and C7 corrected position in the plumbline through the posterior angle of S1 endplate).
-
Femoral obliquity angle (FOA). Angle between the femoral axis and the vertical line.
-
Pelvic tilt excess. Set based on author’s experience to 10° when pelvic tilt is more than 25° and 5° when it is <25°.
The FBI method has been preliminarily validated by the authors in a short series of cases [22]. Limitations of the FBI method are gross estimation of the amount of pelvic tilt excess and lack of consideration of thoracic hypolordosis which has been shown to jeopardize the accuracy of final correction in patients with flexible thoracic spine [20]. In addition, it underestimates the amount of needed correction in those patients with normal SVA, no knee flexion and extreme pelvic tilt, a scenario that can present clinically.
Discussion
The authors’ preferred method: the spinofemoral angle method
We propose a method of calculation of the amount of correction needed that can avoid potential lack of accuracy in the FBI method, while keeping its simplicity.
The method is based on the measurement of a single angle, the spino femoral angle (SFA). This is the angle formed by the femoral axis and the line drawn from the center of C7 to the point where the vertical line from of the posterior end of the S1 plate intersects the level of the planned osteotomy. As shown by Yang and Ondra [19], the angle of this line with the vertical is equivalent to Le Huec’s angle of C7 translation with an error of <3°. With this approximation, the SFA equals the sum of the femoral obliquity angle plus the angle of C7 translation, and can easily be calculated on digital radiographs or on conventional radiographs with an electronic clinometer (the authors use the smartphone application CobbMeter, R2MobileStudio, France, with gives a precision within 0.1°) or with image processing software.
To increase the accuracy of the method, two modifier parameters must be added to SFA in the calculation: hip extension reserve and thoracic hypokyphosis.
When we measure femoral obliquity angle, we are really estimating the excess of pelvic tilt in that patient. We can assume that when compensating imbalance by increasing pelvic tilt, the patient first completely extends his hips (hip extension reserve usually equals 10°) and then flexes his knees to further retrovert the pelvis (with an additional increase in pelvic tilt equal to femoral obliquity angle). Therefore, the best estimate of excess of pelvic tilt is the sum of hip extension reserve and femoral obliquity angle.
Finally, in patients with an hypokyphotic, flexible thoracic spine, that will not be included in the instrumentation, a postoperative increase in thoracic kyphosis (ITK) after surgery can be anticipated, and some correction will be lost for this reason. To our knowledge, no study has shown a method to predict the amount of increase of thoracic kyphosis after surgery for sagittal balance. We propose calculation based on flexion radiographs of the thoracic spine, assuming that final thoracic kyphosis will equal to active flexion kyphosis in a worst case scenario. Lumbar lordosis should be additionally increased by the expected ITK, calculated as the difference between acrive flexion thoracic kyphosis (ATK) and standing thoracic kyphosis (TK)
Thus, the final needed correction angle would be calculated as
Needed correction angle = SFA + 10° + ITK
where
If thoracic spine flexion radiographs are not available, final thoracic kyphosis can estimated to be close to final lumbar lordosis.
Although our method has not yet been validated, it has been preliminarily used in our clinical practice.
Conclusions
Sagittal imbalance causes pain and decrease in health related quality of life and function. Although it is the result of complex interactions, currently there exist sufficient information to interpret the key aspects of sagittal imbalance in a given patient. A model interpreting sagittal imbalance should include global alignment (measured with C7 plumbline), spinopelvic balance (calculated from lumbar lordosis, thoracic kyphosis, pelvic incidence and age related spinopelvic constant) and adaptative knee flexion. Several methods exist to calculate the amount of correction needed. Those including all the relevant parameters should be preferred.
References
Schwab F, Patel A, Ungar B, Farcy JP, Lafage V (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 35:2224–2231
Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P (2010) Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine 35:E1193–E1198
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15:415–422
Lamartina C, Zavatsky JM, Petruzzi M, Specchia N (2009) Novel concepts in the evaluation and treatment of high-dysplastic spondylolisthesis. Eur Spine J 18:133–142
Schwab F, Lafage V, Patel A, Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine 34:1828–1833
Mac-Thiong JM, Transfeldt EE, Mehbod AA, Perra JH, Denis F, Garvey TA, Lonstein JE, Wu C, Dorman CW, Winter RB (2009) Can C7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine 34:E519–E527
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30:682–688
Videbaek TS, Bünger CE, Henriksen M, Neils E, Christensen FB (2011) Sagittal spinal balance after lumbar spinal fusion: the impact of anterior column support results from a randomized clinical trial with an eight- to thirteen-year radiographic follow-up. Spine 36:183–191
Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab FJ, Hamill CL, Horton WC, Ondra SL, Sansur CA, Bridwell KH, Spinal Deformity Study Group (2011) Risk–benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine 36:817–824
Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR (2008) Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976) 33:2243–2247
Bridwell KH, Baldus C, Berven S, Edwards C 2nd, Glassman S, Hamill C, Horton W, Lenke LG, Ondra S, Schwab F, Shaffrey C, Wootten D (2010) Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine 35:1849–1854
Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ (2009) Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine 34:785–791
Roussouly P, Nnadi C (2010) Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19:1824–1836
Lee SH, Kim KT, Suk KS, Lee JH, Seo EM, Huh DS (2011) Sagittal decompensation after corrective osteotomy for lumbar degenerative kyphosis: classification and risk factors. Spine 36:E538–E544
Lewis SJ, Gray R, David K, Kopka M, Magana S (2010) Technique of reverse smith petersen osteotomy (RSPO) in a patient with fixed lumbar hyperlordosis and negative sagittal imbalance. Spine 35:E721–E725
Neal CJ, McClendon J, Halpin R, Acosta FL, Koski T, Ondra SL (2011) Predicting ideal spinopelvic balance in adult spinal deformity. J Neurosurg Spine 15:82–91
Ondra SL, Marzouk S, Koski T, Silva F, Salehi S (2006) Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine 31:E973–E979
Yang BP, Ondra SL (2006) A method for calculating the exact angle required during pedicle subtraction osteotomy for fixed sagittal deformity: comparison with the trigonometric method. Neurosurgery 59:ONS458–ONS463
Aurouer N, Obeid I, Gille O, Pointillart V, Vital JM (2009) Computerized preoperative planning for correction of sagittal deformity of the spine. Surg Radiol Anat 31:781–792
Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am 87:260–267
Le Huec JC, Leijssen P, Duarte M, Aunoble S (2011). Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J 20:669–680
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lamartina, C., Berjano, P., Petruzzi, M. et al. Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J 21 (Suppl 1), 27–31 (2012). https://doi.org/10.1007/s00586-012-2236-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2236-9