Abstract
Study design
Technical report on the surgical technique of asymmetric osteotomy of the spine for coronal imbalance.
Objective
To describe a successful method of performing asymmetrical pedicle subtraction osteotomy (APSO) through a posterior only approach.
Summary of background
Rigid coronal deformity of the spine can be sharply angulated and can create significant coronal imbalance. Surgical correction is the only definitive treatment of restoring the balance as bracing is unhelpful. Corrective surgery can be anterior or posterior. The literature on the methods of surgical correction of rigid coronal deformities of the spine is limited. Unlike osteotomies for sagittal imbalance, blunt dissection of the anterior cortex is necessary in asymmetrical osteotomy to allow resection of the anterior cortex for closure of the wedge. We describe a method by which we performed this in the thoracic and lumbar spine with case examples.
Method
After insertion of pedicle screws, laminectomy and unilateral facetectomy of the proposed level of osteotomy is performed. Next, dissection lateral to the pedicle and vertebral body is performed bluntly with mastoids to reach the front of the anterior cortex and confirmed with fluoroscopy. An oblique osteotomy including the lateral and posterior cortex is performed above and below the pedicle under imaging. The osteotomy site is closed through unilateral compression.
Conclusion
Satisfactory correction of coronal deformity can be achieved with APSO from an isolated posterior approach. In contrast to sagittal osteotomies, blunt dissection along the anterior cortex is necessary to allow safe resection of anterior cortical bone for closure of the wedge.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Subtraction osteotomy procedures have become a mainstay of spinal deformity surgery. Pedicle subtraction osteotomies (PSO) and Smith Peterson osteotomies (SPO) are well-established techniques for the correction of adult sagittal plane deformities [1–6]. Pedicle subtraction osteotomies allow significant correction through removal of a wedge tapering towards the anterior cortex [6, 7].
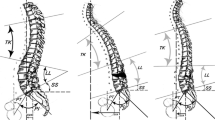
Coronal plane deformities are less common. This, in contrast to sagittal correction via PSO, requires a lateral convexity based wedge with resection of the anterior cortex tapering towards the concavity [4]. Traditionally, this is accomplished with a combined anterior and posterior approach in the form of vertebral column resection (VCR) [8, 9].
We describe an asymmetrical pedicle subtraction osteotomy (APSO) technique for the treatment of coronal plane deformity through an isolated posterior approach which we have used successfully in two cases.
Case description
Case 1 is a young lady of 28 with VATER syndrome. She had a past h/o Rt L5 hemi-vertebra which was fused without resection from L3 to S1 when she was eight. Her main complaint was coronal imbalance to her left and back pain. She compensated for this deformity by walking on tip-toes on her left side. A whole spine X-ray and CT reconstruction showed a coronal angular deformity of 25° and imbalance of 21 cm (Fig. 1a–d).
Through a posterior approach a single level right-sided APSO of L3 and fusion from L1 to sacrum was performed.
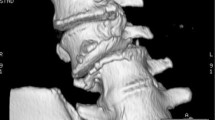
Case 2 is a 51-year-old paraplegic who leads a near independent life using a wheel chair. He presented with a mal-aligned type C fracture of the thoracic spine at T6 and a Charcot joint articulation at T11 (Fig. 2). His main complaint was costo-pelvic impingement and sitting imbalance in his wheel chair. A sitting X-ray showed a coronal angular deformity of 31° across the thoracic spine.
A right-sided T12 APSO through an isolated posterior approach with fusion from T5 to L2 was performed.
Surgical technique
Principle of surgical technique of asymmetrical pedicle subtraction osteotomy
The procedure was performed on a radiolucent table in the prone position. Pre-operatively, the angles of osteotomy that were required in both the cases were determined by visual estimation of angles alone without navigational aid. Spinal cord monitoring is recommended, but was not used in our cases as the first patient had an implanted sacral stimulator and the second patient was a complete paraplegic. A standard posterior exposure of the spine is performed extending to two levels above and below the intended site of the osteotomy with pedicle screw placement at these levels. A temporary rod can be mounted across the concavity of the deformity (used in case 2). The entire lamina and unilateral pedicle are resected on the side of the intended osteotomy. The lateral cortex of the vertebral body is dissected to the anterior circumference using small-sized swabs (mastoid swabs). Using osteotomes a lateral wedge is fashioned and removed with the exception of the anterior cortex which is resected with Kerrison rongeurs. The wedge is closed though compression on the side of the osteotomy.
Technical details
Asymmetric PSO case 1: lumbar spine
The lamina of L3 including the pedicle pars and articular processes was removed on the right (osteotomy) side. The transverse process on the osteotomy side was subsequently removed by breaking it at its base and resecting it with Kerrison rongeurs. This allowed blunt dissection lateral to the L3 vertebral body using swabs. The lateral cortex of L3 was exposed including the anterior circumference and confirmed under fluoroscopy (Fig. 3a). A malleable retractor was inserted for additional protection of para-vertebral tissue. The L3 nerve root was carefully retracted medially. Using osteotomes under image guidance, two cuts were made into the vertebral body through the posterior wall. The first was placed above the pedicle parallel to the superior endplate; the second was placed below the pedicle at the desired angle to the first cut (see Fig. 4a, b of case 2). Both cuts included the lateral cortex and extended just beyond the midline of the posterior wall. The osteotomes were tapped forward up to but not beyond the anterior cortex under lateral imaging. The lateral edges of the osteotomes were well visualised due to the previous lateral dissection. The osteotomy cuts of the posterior vertebral wall were completed from the left side by retracting the L3 root to the right and extending the cuts from the midline to the medial cortex of the left pedicle. The wedge was then broken away from the anterior cortex with curettes. The remaining anterior cortex was removed using Kerrison rongeurs and curettes, carefully avoiding injury to the anterior vessels (Fig. 3a, b). The osteotomy was closed by compressing the convex side (Fig. 3c). The inferior facet on the left was removed to facilitate mobilisation and easy closure of the osteotomy. Inter-laminar fusion of the instrumented segments was done with auto-graft.
Case 1. Intra-operative lateral fluoroscopy view showing mastoid swabs (radio-opaque strips) and malleable retractor anterior to L3 (a); a curette is visible working on the anterior cortex. AP fluoroscopy demonstrates the extent of bone resection in the shape of a wedge (b). Closure of the osteotomy side on the convex side (c)
Asymmetric PSO case 2: thoracic spine
A laminectomy of T12 and resection of adjacent facet joints on the right (osteotomy) side of the vertebra was performed. A costotransversectomy of T12 and resection of the right pedicle allowed retro-pleural dissection of the lateral vertebral wall with swabs. Osteotomies were performed in a similar way to the lumbar PSO described above, from the lateral cortex towards the contra-lateral side above and below the T12 pedicle in an oblique fashion (Fig. 4a, b). This step was done under fluoroscopic control to avoid the anterior wall of the vertebral body. The resultant wedge was removed using curettes, leaving behind the anterior vertebral cortex. The anterior cortex was subsequently removed using Kerrison rongeurs, carefully avoiding the anterior vessels (Fig. 4c). The osteotomy was then closed by connecting the remaining rod and alternatively compressing the convex side and distracting the concave side. This was followed by intra-laminar fusion.
Results
Case 1: Pre-operative coronal angular deformity of 25° was reduced to 3° after the osteotomy. Coronal imbalance of 21 cm pre-operatively was reduced to zero in the last follow-up X-ray at the end of 1 year (Fig. 5a, b). A sacral stimulator was implanted in the interim for bowel control.
Case 2: Pre-operative coronal angular deformity of 31° was reduced to 6° after the osteotomy restoring his sitting balance and relieving the costo-pelvic impingement. At the last follow-up at 1 year the correction was maintained with fusion across the site (Fig. 6a, b).
Complications: There was a small dural tear in case 2, which was repaired intraoperatively. Both patients were mobilised post-operatively without brace.
Discussion
Coronal deformities of the spine [1] frequently require surgical correction to restore spinal balance. For sharp, angular deformity an APSO offers significant correction through a limited approach [6, 7]. Most literature on asymmetrical correction of angular deformities is on hemi-vertebra excision in the paediatric group [10, 11]. Bakaloudis et al. [4] have recently described their results of treatment of a group of paediatric patients with severe kypho-scoliosis of varied aetiologies with APSO. They included patients whose deformity was reducible in a Risser cast by about 20–40%, demonstrating a role for APSO in intermediate degree of coronal deformity.
Literature on coronal plane osteotomy for adult deformity, however, is scarce. Our two adult cases had rigid sharp angular deformities in the setting of previous fusion (surgical in one case and post-traumatic in the other). In the absence of sagittal imbalance as in our cases, an isolated lateral wedge needs to be resected to correct the deformity [1]. The base of the wedge includes the pedicle on the convexity with the anterior and posterior vertebral cortex making up the sides of the wedge. While it is reasonably easy to access the posterior vertebral wall, exposure of the anterior vertebral cortex poses greater challenges from posterior [4, 12]. The careful dissection of the vertebral cortex with swabs (in our experience mastoid swabs worked best) across the anterior cortex allowed well-visualised resection of the anterior cortex with Kerrison rongeurs. In our cases the anterior vessels were easily displaced with the swabs. Care would obviously need to be taken to avoid injury in a setting where the vessels prove to be adherent [12]. The use of osteotomes in the formation of the wedge provided a cleaner geometrical cut than the traditional method of de-cancellation through the pedicle and de-bulking the vertebral body before using the Lexell Rongeur or osteotome to shape the wedge on the lateral wall [6, 7].
References
Bridwell KH (2006) Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs vertebral column resection for spinal deformity. Spine 31:S171–S178
Thomasen E (1985) Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop 194:142–152
Dorward IG, Lenke LG (2010) Osteotomies in the posterior-only treatment of complex adult spinal deformity: a comparative review. Neurosurg Focus 28(3):E4
Bakaloudis G, Lolli F, Di Silvestre M, Greggi T, Astolfi S, Martikos K, Vommaro F, Barbanti-Brodano G, Cioni A, Giacomini S (2011) Thoracic pedicle subtraction osteotomy in the treatment of severe pediatric deformities. Eur Spine J 20(Suppl):S95–S104
Wang Y, Lenke LG (2011) Vertebral column decancellation for the management of sharp angular spinal deformity. Eur Spine J 20:1703–1710
Bridwell KH, Lewis SJ, Rinella A, Lenke LG, Baldus C, Blanke K (2004) Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance surgical technique. J Bone Joint Surg Essent Surg Tech 86(Suppl):1
Wang MY, Sigurd BH (2007) Lumbar pedicle subtraction osteotomy. Neurosurgery 60(2):p140–p146
Suk S, Chung E, Lee S, Lee J, Kim S, Kim J (2005) Posterior vertebral column resection in fixed lumbosacral deformity. Spine 30:E703–E710
Bradford DS, Tribus CB (1997) Vertebral column resection for the treatment of rigid coronal decompensation. Spine 22:1590–1599
Polly DW, Rosner MK, Monacci W, Moquin RR (2003) Thoracic hemivertebra excision in adults via a posterior-only approach. Report of two cases. Neurosurg Focus 14:1–4
Halm H (2011) Transpedicular hemivertebra resection and instrumented fusion for congenital scoliosis. Eur Spine J 20:993–994
Arun R, Dabke HV, Mehdian H (2011) Comparison of three types of lumbar osteotomy for ankylosing spondylitis: a case series and evolution of a safe technique for instrumented reduction. Eur Spine J 20:2252–2260
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thambiraj, S., Boszczyk, B.M. Asymmetric osteotomy of the spine for coronal imbalance: a technical report. Eur Spine J 21 (Suppl 2), 225–229 (2012). https://doi.org/10.1007/s00586-012-2171-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2171-9