Abstract
Chronic myeloid leukemia (CML) is a clonal hematopoietic stem cell disorder characterized by the presence of Philadelphia (Ph) chromosome. Wilms’ tumor gene 1 (WT1) plays an important role in leukemogenesis and can be useful as a molecular marker to detect minimal residual disease (MRD). The goal of this study was to evaluate WT1 expression and compare it with BCR-ABL1 expression in peripheral blood (PB) of CML patients, in order to explore the utility of WT1 as an alternative marker for MRD detection. Eighteen newly diagnosed CML patients (BCR-ABL1-p210-positive), 16 chronic CML patients with a history of imatinib therapy, and 18 normal individuals (BCR-ABL1-p210-negative) as controls were enrolled in this study. WT1 and BCR-ABL1 expression was evaluated by quantitative real-time polymerase chain reaction (Q-RT-PCR). Analysis of RT-PCR data was performed using REST Software (2009, QIAGEN, Valencia, USA). Data were analyzed by SPSS software (v.16.0) using Spearman’s rho and Kruskal-Wallis methods. WT1 expression in all PB samples of newly diagnosed CML patients was significantly higher than that of the normal individuals (P = 0.003). WT1 expression was not different in patients on imatinib therapy compared to normal individuals (P = 0.6), but it was significantly lower than that of the newly diagnosed CML patients (P = 0.001). There was no significant correlation between expression of WT1 and BCR-ABL1 and hematological findings in newly diagnosed CML patients. We confirm the oncogenic role of WT1 by WT1 upregulation in CML. Due to lack of significant correlation between BCR-ABL1 and WT1 expression, using WT1 as an additional marker for CML monitoring could not be applicable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic myeloid leukemia (CML) is a clonal hematopoietic stem cell (HSC) disorder and is characterized by the Philadelphia (Ph) chromosome as a result of reciprocal translocation between long arms of chromosomes 9 and 22 [t(9;22)(q34;q11)](Zheng et al. 2006; Babashah et al. 2012), which leads to generation of BCR-ABL1 fusion oncogene and translation into a constitutively active tyrosine kinase protein(Smith et al. 2003). BCR-ABL1 protein promotes cell proliferation and survival through activating different pathways, including JAK/STAT, Ras/Raf/MEK/ERK, and PI3/Akt (Fig. 1) (Jabbour and Kantarjian 2014).
The role of WT1 in regulation of involved signaling pathways in CML pathogenesis. BCR-ABL protein promotes proliferation and survival of a cell through activating different signaling pathways such as JAK/STAT, MAPKinase, and PI3/Akt. The expression of WT1 is induced by these pathways. On the other hand, WT1 activates MAPK and JAK/STAT pathway-related genes. WT1 downregulates and upregulates IRF-8 and NDRG2, respectively. WT1 upregulation increases ABCB1 expression through Wnt/β-catenin. ABCB1 is involved in drug resistance in CML. WT1 Wilms’ tumor 1, IRF-8 interferon regulatory factor 8, NDRG2 N-myc downstream-regulated gene 2, MAPK mitogen-activated protein kinase, JAK/STAT Janus kinase/Signal transducer and activator of transcription
Wilms’ tumor gene 1 (WT1) was first recognized as a tumor suppressor (TS) gene involved in the pathogenesis of Wilms’ tumor, a pediatric renal neoplasm (Call et al. 1990; Yang et al. 2007). WT1 gene is located on the short arm of chromosome 11 (11p13). Its product is a zinc finger transcription factor that regulates the expression of different genes, including PDGF-α (platelet-derived factor) chain, CSF-1 (colony-stimulating factor 1), IGF-II (insulin growth factor II), IGF-1R (insulin growth factor receptor), C-myc, RAR-α (retinoic acid receptor alpha), and Bcl-2 (B cell lymphoma 2)(Inoue et al. 1998). WT1 controls the proliferation and differentiation of several cells such as HSC (Menssen et al. 1997). The pattern of WT1 expression is restricted to CD34+ progenitor cells and early hematopoietic precursors, which is downregulated following differentiation (Heesch et al. 2010; Maurer et al. 1997). WT1 is highly expressed in early myeloid progenitors, but it is downregulated during differentiation (Nomdedéu et al. 2013). According to WT1 over-expression in leukemic cells, it is recently considered as an oncogene (Sugiyama 2010; Hatta et al. 2005). High expression of WT1 has been reported in hematological malignancies, including acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), and acute lymphocytic leukemia (ALL) (Tamaki et al. 1999; Cilloni et al. 2009; Asgarian Omran et al. 2008). Therefore, it is a useful and good marker for detecting minimal residual disease (MRD) and can be applicable as a prognostic marker for treatment monitoring and predicting the relapse in leukemic and MDS patients (Sakamoto et al. 2009). There is a high expression of WT1 in the blastic phase rather than the chronic phase of CML (Inoue et al. 1994). According to recent studies related to the usefulness of WT1 as a marker for MRD in other leukemias, we decided to evaluate its expression and possible utility in CML patients in Iran. The goal of our study was to evaluate the expression pattern of WT1 in peripheral blood of CML patients at diagnosis (BCR-ABL1-p210-positive) and during imatinib therapy by sensitive real-time quantitative polymerase chain reaction (PCR) method compared to normal individuals (BCR-ABL1-p210-negative), and we have tried to study the relationship between BCR-ABL1 and WT1 gene, in order to demonstrate WT1 as a prognostic and additional marker for monitoring CML in parallel with BCR-ABL1 expression.
Materials and methods
Patients and controls
Eighteen newly diagnosed CML patients (BCR-ABL1-p210-positive) at the Shafa Hospital of the Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran, were enrolled in this study between January 2013 and January 2014 among patients with suspected myeloproliferative disorders referred for the first time. They were nine males and nine females, randomly. All the patients were in the first chronic phase of CML according to the WHO criteria (Swerdllow et al. 2008) and before the start of treatment. Sixteen chronic CML patients (nine males, seven females) with a history of imatinib therapy which were referred to our Laboratory for treatment monitoring were also chosen. Peripheral EDTA blood samples (5 mL) were obtained from all patients. Diagnosis was based on morphological examination of peripheral blood (PB) and bone marrow (BM) films. CML was confirmed by the presence of the BCR-ABL1-p210 fusion gene by PCR. Eighteen normal individuals without any history of hematological disease which were referred for health checkup were also selected as controls. Their BCR-ABL1-p210 fusion test was also negative.
This study was approved by the local ethics committee of the Ahvaz Jundishapur University of Medical Sciences (ajums.REC.1392, 341), and written informed consent was obtained from all patients and normal individuals.
Cell lines
The K562 cell line was used as a positive control of Ph+ CML and WT1 expression. The Jurkat cell line was used for BCR-ABL1 expression, and the U937 cell line was used as negative control for BCR-ABL1 fusion. The cell lines were purchased from the Pasteur Institute of Iran and cultured in RPMI-1640 medium (Gibco, Carlsbad, CA, USA) containing 10 % fetal calf serum (FCS), 50 U/mL penicillin, 50 g/mL streptomycin, 2 mM/L l-glutamine (Sigma-Aldrich, St. Louis, MO, USA), and 25 mM/L HEPES (4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid) at 37 °C in 5 % CO2.
Isolation of mononuclear cells
PB EDTA samples were layered onto Ficoll-Paque (Lymphodex, inno-Train, Germany) gradient. Isolated mononuclear cells were washed twice with phosphate buffer saline (PBS).
RNA extraction and cDNA synthesis
Total RNA was extracted from 106 isolated cells from PB EDTA samples as well as from the mentioned cell lines using RNeasy Mini Kit (RIBO-prep, Russia) based on the manufactures’ instructions. RNA was spectrophotometrically quantified at 260 nm. Complementary DNA (cDNA) was synthesized from 2 μg of total RNA in 20 mL reaction mixture using a cDNA synthesis kit (Bioneer, Korea) according to the manufactures’ instructions. The mixture was incubated at 20 °C for 30 s, 42 °C for 4 min, and 55 °C for 30 s, followed by 95 °C for 5 min performed at 8 cycles.
Quantitative real-time polymerase chain reaction
HPRT gene was used as a reference gene because it was validated according to our experimental conditions. In addition, its expression was invariant and stable by experimental factors. The use of a reference gene as an internal control is essential for normalizing real-time data (messenger RNA (mRNA) concentration of target gene/reference genes), and it should be experimentally validated for specific cell types or tissues (Bustin et al. 2009). For BCR-ABL1 fusion, the ABL gene was used as the reference gene. The expression level of genes was determined by the Step One Plus Real-Time RT-PCR system (ABI, USA) using SYBR Green Master Mix (Takara, Japan) according to the manufacturers’ instructions. The following specific primers were used: WT1 forward (F): 5′-AGGGTACGAGAGCGATAACCACAC-3′; WT1 reverse (R): 5′-CTCAGATGCCGACCGTACAAGA-3′; HPRT1 F: 5′-CCTGGCGTCGTGATTAGTG-3′; and HPRT1 R: 5′-TCAGTCCTGTCCATAATTAGTCC-3′. Twenty-two microliters reaction mixture of PCR was prepared containing 11 μL SYBR Green, 0.5 μL each primer, 2 μL cDNA, and 8 μL DEPC water. WT1 real-time polymerase chain reaction (RT-PCR) was performed in 40 cycles, and each cycle consisted of 95 °C for 20 s, 95 °C for 3 min, and 60 °C for 30 s. BCR-ABL1 RT-PCR was performed according to NanoGene kit (Alert, Italy) in 50 cycles, and each cycle consisted of 50 °C for 2 min, 95 °C for 2 min, and followed by 95 °C for 15 s and 60 °C for 1 min.
The data of RT-PCR were analyzed by the 2−∆∆CT method and were presented as fold change in gene expression (Livak and Schmittgen 2001). The results were presented as a relative index of the WT1/HPRT1 ratio. BCR-ABL1 expression was presented as a copy number. All samples were tested in duplicate.
Statistical analysis
Analysis of RT-PCR data was performed using REST Software (2009, QIAGEN, Valencia, USA). Data were analyzed by SPSS software for Windows v.16.0. Spearman’s rho method was used to examine the correlation between quantitative data. The Kruskal-Wallis method was used to compare quantitative data between three groups of CML patients. P value <0.05 was considered statistically significant.
Results
WT1 expression in newly diagnosed CML patients
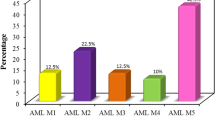
WT1 expression level was evaluated in PB EDTA samples of 18 newly diagnosed CML patients (9 females and 9 males) with a mean age of 48.12 ± 18.77 years. The WT1/HPRT ratio was calculated for each patient in comparison to normal individuals with REST software, separately. WT1 was upregulated and downregulated in 13 (72.2 %) and 2 (11.1 %) newly diagnosed CML patients in comparison to the control group, respectively (P < 0.05).There was no difference of WT1 expression in three (16.6 %) newly diagnosed CML patients compared to the control group (P > 0.05) (Fig. 2). Taken together, WT1 expression in all PB samples of newly diagnosed CML patients was significantly higher than that of the normal individuals (P = 0.003). WT1 expression was not related to BCR-ABL1 fusion copy number (Spearman’s correlation coefficient = −0.205; P = 0.414).
The demographic and clinical characteristics of chronic-phase CML patients are listed in Table 1. There was no significant correlation between WT1 expression and hematological findings (P values >0.05) (Table 2). Moreover, there was no significant correlation of hematological findings and BCR-ABL1 fusion copy number between three groups of patients according to WT1 expression level (P values >0.05) (Table 1).
WT1 expression in CML patients on imatinib therapy
WT1 expression level was evaluated in PB EDTA samples of 16 CML patients on imatinib therapy. WT1 expression was downregulated, upregulated, and not different in three (18.75 %), three (18.75 %), and ten (62.5 %) of these patients in comparison to normal individuals, respectively (Fig. 3). Taken together, WT1 expression was not different in CML patients on imatinib therapy in comparison to normal individuals (P = 0.6). WT1 expression in these patients was significantly lower than that of the newly diagnosed CML patients (P = 0.001), which was downregulated on imatinib therapy (Table 3.).There was no significant correlation between WT1 and BCR-ABL1 in newly diagnosed CML patients, so it was not evaluated in patients on imatinib therapy.
WT1 expression in cell lines
WT1 is highly expressed in K562 (b3a2) and Jurkat cell lines. Its expression in the Jurkat cell line is less than that in the K562 cell line. There was no expression of WT1 in the U937 cell line. No significant difference was observed for WT1/HPRT ratio between the K562 cell line and newly diagnosed CML patients (P = 0.06).
Discussion and future directions
CML is a myeloproliferative disorder associated with the presence of Philadelphia chromosome and elevated tyrosine kinase activity of BCR-ABL1 fusion protein (Jabbour and Kantarjian 2014). The presence of oncogenes as molecular indexes of tumor or absence of tumor suppressors in combination with BCR-ABL1 is likely the reason for CML development. Therefore, recognition and evaluation of these markers could be helpful for better diagnosis, treatment, and control of disease. The research for understanding the involved molecules participating in CML development and CML monitoring continues. MRD monitoring is based on molecular markers which are present in leukemic but not in normal cells. Recent progress in molecular techniques has led to identification of leukemic genes known as tumor-associated antigens (TAA). They play a role in the development of leukemia and can be used as molecular markers for diagnosis and monitoring. WT1 is one of these genes (Asgarian Omran et al. 2008; Asgarian et al. 2005; Dong et al. 2014). Overexpression of WT1 has been reported in several hematological malignancies and acts as a good marker for detecting MRD in AML, ALL, MDS, and the blastic phase of CML; however, its role in leukemogenesis is yet unclear (Asgarian Omran et al. 2008; Siehl et al. 2004). The important role of WT1 in proliferation and survival of leukemic cells and antileukemic effect of its inhibition has been indicated. Glienke et al. identified downregulation of WT1 by siRNA which led to proliferation reduction and increased apoptosis of K562 and HL-60 cell lines (Glienke et al. 2007). In the study of Yamagami et al., downregulation of WT1 by WT1 antisense oligomers led to inhibition of cell growth in both K562 cell lines and fresh leukemic cells (Yamagami et al. 1996). Therefore, WT1 expression can be an appropriate molecular marker for malignant hematopoiesis (Mao et al. 2013) but its biologic function in hematopoietic cells and hematological malignancies is still controversial (Siehl et al. 2004).
Our study confirmed the previous studies, which have indicated that WT1 expression is increased as an oncogene in hematological malignancies such as CML (Tamaki et al. 1999; Cilloni et al. 2009; Asgarian Omran et al. 2008). There was no significant association between WT1 expression and BCR-ABL1 fusion expression in the present study, while there was an association between them in the bone marrow samples in Cao et al.’s study (Cao et al. 2007). This difference may be related to presence of accelerated and blastic-phase patients and WT1 evaluation in BM samples.
As all of our patients were BCR-ABL1-positive, the presence of the BCR-ABL1 fusion can induce CML in cooperation with WT1 overexpression. This may be the effect of tyrosine kinase activity of BCR-ABL1 on cellular signaling pathways (Jabbour and Kantarjian 2014). For example, BCR-ABL1 tyrosine kinase leads to overexpression of WT1 gene as well as increased mRNA and protein levels through PI3K-Akt pathway (Svensson et al. 2007a). BCR-ABL1 transfection leads to increased expression of WT1, and it was decreased after imatinib incubation (Cilloni et al. 2004). Also, incubation of K562 cells with imatinib caused inhibition of BCR-ABL1 tyrosine kinase activity and downregulation of WT1 expression (Cilloni and Saglio 2003). Therefore, inhibition of BCR-ABL1 tyrosine kinase activity can be responsible for WT1 reduction; otherwise, WT1 overexpression is related to increased BCR-ABL1 tyrosine kinase activity. According to overexpression of WT1 in BCR-ABL1-negative leukemias such as AML, BCR-ABL1-activated signaling pathway is not the only mechanism and reason for WT1 overexpression (Yang et al. 2007). Nishida et al. indicated that AML-ETO gene, which is recognized as a common chimeric gene in AML, performs its leukemogenesis activity in cooperation with WT1 expression and AML-ETO could not induce AML by itself (Nishida et al. 2006).
The oncogenic activity of WT1 is mediated through regulation of different genes and signaling pathways (Fig. 1). Li et al. (Li et al. 2014a) reported upregulation of molecules associated with MAPK and JAK/STAT signaling pathways in WT1-isoform-transfected U937 cell lines. Interferon regulatory factor 8 (IRF-8) and N-myc downstream-regulated gene 2 (NDRG2) are recognized as WT1 target genes. WT1 downregulates and upregulates IRF-8 and NDRG2 expression, respectively (Vidovic et al. 2010; Svensson et al. 2007b). IRF-8 leads to BCR-ABL1 antagonization and downregulation of antiapoptotic protein Bcl-2, increasing the expression of tumor suppressor p15 (Burchert et al. 2004; Schmidt et al. 2004). Therefore, deregulation of IRF-8 and NDRG2 expression by WT1 can be one of the oncogenic mechanisms in CML development. There was downregulation of β-catenin, Wnt/β-catenin pathway-related gene, and β-catenin target genes (including CCND1 and MYC in WT1-specific shRNA) in transfected K562 cells (Li et al. 2014b). In Corrêa et al.’s study (Corrêa et al. 2012), increased Wnt/β-catenin activity regulates ABCB1 gene expression, which is involved in drug resistance in CML (Corrêa et al. 2012). Therefore, WT1 gene has an oncogenic role by Wnt/β-catenin regulation in leukemogenesis.
Progression mechanism and molecular events involved in CML development are still unknown (Calabretta and Perrotti 2004). According to WT1 overexpression in most chronic CML patients in our study and higher expression of it in the blastic phase than the chronic phase in Inoue et al.’s and Varma et al.’s studies (Inoue et al. 1994; Varma et al. 2011), the value of WT1 as a possible and effective factor in progression of disease is indicated, and it can be used for predicting disease prognosis and progression. In the current study, there was also a significant reduction in WT1 in CML patients on imatinib therapy in comparison with newly diagnosed CML patients. No difference in WT1 expression was observed in patients on imatinib therapy compared to the control group. There are related studies about the effects of imatinib on WT1 expression in vitro (Table 4). For example, incubation of BM samples of pretreatment patients with imatinib for 18 h in vitro leads to decreased tyrosine kinase activity and eventual downregulation of WT1 in imatinib-responsive patients, while this was not observed in imatinib-resistant patients. Therefore, in vitro testing with imatinib to evaluate the inhibition level of WT1 expression before treatment can be the basis of a valuable test for predicting the response of patients to imatinib. It can also be used to recognize imatinib-resistant patients (Cilloni et al. 2004; Otahalova et al. 2008). Inhibition of BCR-ABL1 tyrosine kinase activity and downregulation of WT1 expression were also seen after imatinib incubation in K562 cell lines (Cilloni and Saglio 2003). In vivo study of Varma et al. (Varma et al. 2011) also demonstrated WT1 downregulation in 76 % of patients on imatinib therapy (decreased in 78.95 % of complete hematologic response (CHR) patients and increased in 66.67 % of non-CHR patients). The limitation of our study was inaccessibility of complete data of our patients and their paraclinical tests. So, we could not compare WT1 expression with other parameters.
Conclusion
Our data confirmed the previous studies, which have indicated the oncogenic role of WT1 by its upregulation in hematologic malignancies, but this expected role was not seen in all cases. However, we could not demonstrate its relation to BCR-ABL1 expression at diagnosis and in patients on imatinib therapy. Overall, according to current and previous studies, imatinib can be effective in downregulating WT1 expression, but due to WT1 upregulation in just 72.2 % of CML patients at diagnosis and lack of significant correlation between BCR-ABL1 and WT1 expression, using WT1 as an additional marker for CML monitoring could not be applicable, although a longer follow-up of CML patients may validate the results. Therefore, future studies are required in which WT1 expression will be evaluated in combination with other molecular markers during treatment, after remission, or after the relapse phase of CML in order to optimize its possible role in CML, therapy efficiency, disease stage determination, WT1 peptide vaccination, and target therapy.
References
Asgarian Omran H, Shabani M, Vossough P, Sharifian R, Tabrizi M, Khoshnoodi J et al (2008) Cross-sectional monitoring of Wilms’ tumor gene 1 (WT1) expression in Iranian patients with acute lymphoblastic leukemia at diagnosis, relapse and remission. Leuk Lymphoma 49(2):281–290
Asgarian H, Shabani M, Vosoogh P, Ali R, Sharifian SG, Khoshnoodi J et al (2005) Over-expression of Wilm’s Tumor Gene 1 (WT1) in Iranian patients with acute myeloblastic leukemia. Iran J Immunol 2(4):182
Babashah S, Rezaei-Tavirani M, Zamanian-Azodi M, Saki N (2012) Chronic myeloid leukemia as a stem cell-derived malignancy. J Paramedical Sci. 3(2)
Burchert A, Cai D, Hofbauer LC, Samuelsson MK, Slater EP, Duyster J et al (2004) Interferon consensus sequence binding protein (ICSBP; IRF-8) antagonizes BCR/ABL and down-regulates bcl-2. Blood 103(9):3480–3489
Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M et al (2009) The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem 55(4):611–622
Calabretta B, Perrotti D (2004) The biology of CML blast crisis. Blood 103(11):4010–4022
Call KM, Glaser T, Ito CY, Buckler AJ, Pelletier J, Haber DA et al (1990) Isolation and characterization of a zinc finger polypeptide gene at the human chromosome 11 Wilms’ tumor locus. Cell 60(3):509–520
Cao XS, Gu WY, Chen ZX, Hu SY, He J, Cen JN (2007) Bone marrow WT1 gene expression and clinical significance in chronic myelogenous leukemia. Zhonghua Nei Ke Za Zhi 46(4):277–279
Cilloni D, Saglio G, editors (2003) Usefulness of quantitative assessment of Wilms tumor suppressor gene expression in chronic myeloid leukemia patients undergoing imatinib therapy. Seminars in Hematology: Elsevier
Cilloni D, Messa F, Gottardi E, Fava M, Arruga F, Defilippi I et al (2004) Sensitivity to imatinib therapy may be predicted by testing Wilms tumor gene expression and colony growth after a short in vitro incubation. Cancer 101(5):979–988
Cilloni D, Renneville A, Hermitte F, Hills RK, Daly S, Jovanovic JV et al (2009) Real-time quantitative polymerase chain reaction detection of minimal residual disease by standardized WT1 assay to enhance risk stratification in acute myeloid leukemia: a European LeukemiaNet study. J Clin Oncol 27(31):5195–5201
Corrêa S, Binato R, Du Rocher B, Castelo-Branco MT, Pizzatti L, Abdelhay E (2012) Wnt/β-catenin pathway regulates ABCB1 transcription in chronic myeloid leukemia. BMC Cancer 12(1):303
Dong W, Zhang J, Shao N, Tian T, Li L, Jian J et al (2014) Development and immunological evaluation of HLA-specific chronic myeloid leukemia polyepitope vaccine in Chinese population. Vaccine 32(28):3501–3508
Glienke W, Maute L, Koehl U, Esser R, Milz E, Bergmann L (2007) Effective treatment of leukemic cell lines with wt1 siRNA. Leukemia 21(10):2164–2170
Hatta Y, Takeuchi J, Saitoh T, Itoh T, Ishizuka H, Iriyama N et al (2005) WT1 expression level and clinical factors in multiple myeloma. J Exp Clin Cancer Res 24(4):595
Heesch S, Goekbuget N, Stroux A, Tanchez JO, Schlee C, Burmeister T et al (2010) Prognostic implications of mutations and expression of the Wilms tumor 1 (WT1) gene in adult acute T-lymphoblastic leukemia. Haematologica 95(6):942–949
Inoue K, Sugiyama H, Ogawa H, Nakagawa M, Yamagami T, Miwa H et al (1994) WT1 as a new prognostic factor and a new marker for the detection of minimal residual disease in acute leukemia. Blood 84(9):3071–3079
Inoue K, Tamaki H, Ogawa H, Oka Y, Soma T, Tatekawa T et al (1998) Wilms’ tumor gene (WT1) competes with differentiation-inducing signal in hematopoietic progenitor cells. Blood 91(8):2969–2976
Jabbour E, Kantarjian H (2014) Chronic myeloid leukemia: 2014 update on diagnosis, monitoring, and management. Am J Hematol 89(5):547–556
Li X, Li Y, Yuan T, Zhang Q, Jia Y, Li Q, et al. (2014) Exogenous expression of WT1 gene influences U937 cell biological behaviors and activates MAPK and JAK-STAT signaling pathways. Leuk Res
Li Y, Wang J, Li X, Jia Y, Huai L, He K et al (2014b) Role of the Wilms’ tumor 1 gene in the aberrant biological behavior of leukemic cells and the related mechanisms. Oncol Rep 32(6):2680–2686
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2− ΔΔCT method. Methods 25(4):402–408
Mao X, Zhang B, Liu L-L, Bai X-L, Zhang D-H (2013) Interaction of human genes WT1 and CML28 in leukemic cells. J Huazhong Univ Sci Technol Med Sci 33:37–42
Maurer U, Brieger J, Weidmann E, Mitrou P, Hoelzer D, Bergmann L (1997) The Wilms’ tumor gene is expressed in a subset of CD34+ progenitors and downregulated early in the course of differentiation in vitro. Exp Hematol 25(9):945–950
Menssen HD, Renkl H-J, Entezami M, Thiel E (1997) Wilms’ tumor gene expression in human CD34+ hematopoietic progenitors during fetal development and early clonogenic growth. Blood 89(9):3486
Nishida S, Hosen N, Shirakata T, Kanato K, Yanagihara M, Nakatsuka S-i et al (2006) AML1-ETO rapidly induces acute myeloblastic leukemia in cooperation with the Wilms tumor gene, WT1. Blood 107(8):3303–3312
Nomdedéu J, Hoyos M, Carricondo M, Bussaglia E, Estivill C, Esteve J, et al. (2013) Bone marrow WT1 levels at diagnosis, post-induction and post-intensification in adult de novo AML. Leukemia
Otahalova E, Ullmannova-Benson V, Klamova H, Haskovec C (2008) WT1 expression in peripheral leukocytes of patients with chronic myeloid leukemia serves for the prediction of Imatinib resistance. Neoplasma 56(5):393–397
Sakamoto Y, Mariya Y, Sasaki S, Teshiromori R, Oshikiri T, Segawa M et al (2009) WT1 mRNA level in peripheral blood is a sensitive biomarker for monitoring minimal residual disease in acute myeloid leukemia. Tohoku J Exp Med 219(2):169–176
Schmidt M, Bies J, Tamura T, Ozato K, Wolff L (2004) The interferon regulatory factor ICSBP/IRF-8 in combination with PU. 1 up-regulates expression of tumor suppressor p15Ink4b in murine myeloid cells. Blood 103(11):4142–4149
Siehl JM, Reinwald M, Heufelder K, Menssen HD, Keilholz U, Thiel E (2004) Expression of Wilms’ tumor gene 1 at different stages of acute myeloid leukemia and analysis of its major splice variants. Ann Hematol 83(12):745–750
Smith DL, Burthem J, Whetton AD (2003) Molecular pathogenesis of chronic myeloid leukaemia. Expert Rev Mol Med 5(27):1–27
Sugiyama H (2010) WT1 (Wilms’ tumor gene 1): biology and cancer immunotherapy. Jpn J Clin Oncol 40(5):377–387
Svensson E, Vidovic K, Lassen C, Richter J, Olofsson T, Fioretos T et al (2007a) Deregulation of the Wilms’ tumour gene 1 protein (WT1) by BCR/ABL1 mediates resistance to imatinib in human leukaemia cells. Leukemia 21(12):2485–2494
Svensson E, Vidovic K, Olofsson T, Vallon-Christersson J, Borg Å, Gullberg U (2007b) The Wilms’ tumor gene 1 (WT1) induces expression of the N-myc downstream regulated gene 2 (NDRG2). DNA Cell Biol 26(8):589–597
Swerdllow S, Campo E, Harris NL (2008) WHO classification of tumours of haematopoietic and lymphoid tissues. IARC Press, France
Tamaki H, Ogawa H, Ohyashiki K, Ohyashiki J, Iwama H, Inoue K et al (1999) The Wilms’ tumor gene WT1 is a good marker for diagnosis of disease progression of myelodysplastic syndromes. Leukemia 13(3):393–399
Varma N, Anand MS, Varma S, Juneja SS (2011) Role of hTERT and WT1 gene expression in disease progression and imatinib responsiveness of patients with BCR-ABL positive chronic myeloid leukemia. Leuk Lymphoma 52(4):687–693
Vidovic K, Svensson E, Nilsson B, Thuresson B, Olofsson T, Lennartsson A et al (2010) Wilms’ tumor gene 1 protein represses the expression of the tumor suppressor interferon regulatory factor 8 in human hematopoietic progenitors and in leukemic cells. Leukemia 24(5):992–1000
Yamagami T, Sugiyama H, Inoue K, Ogawa H, Tatekawa T, Hirata M et al (1996) Growth inhibition of human leukemic cells by WT1 (Wilms tumor gene) antisense oligodeoxynucleotides: implications for the involvement of WT1 in leukemogenesis. Blood 87(7):2878–2884
Yang L, Han Y, Saiz FS, Minden M (2007) A tumor suppressor and oncogene: the WT1 story. Leukemia 21(5):868–876
Zheng C, Li L, Haak M, Brors B, Frank O, Giehl M et al (2006) Gene expression profiling of CD34+ cells identifies a molecular signature of chronic myeloid leukemia blast crisis. Leukemia 20(6):1028–1034
Acknowledgments
This work was financially supported by grant TH92/13 from the Vice Chancellor for Research Affairs of the Ahvaz Jundishapur University of Medical Sciences. This paper is issued from the thesis of Saeideh Hajizamani.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the local ethics committee of the Ahvaz Jundishapur University of Medical Sciences (ajums.REC.1392, 341) and with the 1964 Helsinki declaration. Written informed consent was obtained from all patients and normal individuals.
Rights and permissions
About this article
Cite this article
Hajizamani, S., Mohammadi-asl, J., Malehi, A.S. et al. Is Wilms’ tumor gene 1 a useful biomarker for detecting minimal residual disease in chronic myeloid leukemia (BCR-ABL1-p210-positive) patients?. Comp Clin Pathol 25, 713–720 (2016). https://doi.org/10.1007/s00580-016-2252-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-016-2252-y