Abstract
Background
Relapse following hematopoietic stem cell transplantation (HSCT) occurs relatively frequently and is a significant risk factor for mortality in patients with acute myeloid leukemia (AML). Early diagnosis is, therefore, of utmost importance and can provide valuable guidance for appropriate and timely intervention. Here, the diagnostic value of two molecular markers, Wilms tumor 1 (WT1) and tumor suppressor protein p53 (TP53), were studied.
Methods and results
Twenty AML patients undergoing HSCT participated in this investigation. Some had relapsed following HSCT, while others were in remission. Peripheral blood (PB) and bone marrow (BM) samples were collected following relapse and remission. WT1 and TP53 messenger RNA (mRNA) expression was evaluated using reverse transcription-quantitative polymerase chain reaction (RT‒qPCR). The diagnostic value of genes was evaluated by utilizing receiver-operating characteristic (ROC) curve analysis. ROC analysis showed WT1 and TP53 as diagnostic markers for relapse after HSCT in AML patients. The mRNA expression level of WT1 was elevated in individuals who experienced relapse compared to those in a state of remission (p value < 0.01). Conversely, the expression level of TP53 mRNA was lower in individuals who had relapsed compared to those in remission (p value < 0.01).
Conclusions
WT1 and TP53 possess the potential to serve as invaluable biomarkers in the identification of molecular relapse after HSCT in patients with AML. Further studies for a definitive conclusion are recommended.
Highlights
In acute myeloid leukemia disease relapse is a major contributor to mortality.
After transplantation, up to 50% of acute myeloid leukemia patients may relapse.
Making early detection of molecular relapse essential for effective treatment.
WT1 and TP53 emerged as diagnostic biomarkers for early detecting molecular relapse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is a malignancy that impacts hematopoietic stem cells, resulting in abnormal proliferation of immature myeloid cells with abnormal differentiation and forming a clone of cells with a myeloid lineage [1]. In addition to conventional chemotherapy, allogeneic stem cell transplantation (allo-SCT) serves as a fundamental treatment modality for AML patients who meet the necessary criteria. Regardless of its predictive characteristics, allo-SCT possesses the highest potential as a post remission therapy for enduring survival of intermediate- or high-risk diseases and as a salvage therapy for relapsed or resistant disease [2]. Self-renewing leukemic stem cells maintain the malignant clones in leukemia, which are rare and quiescent, making them highly resistant to cytotoxic chemotherapy. This resistance can contribute to relapse and disease progression [3].
In patients with AML, disease relapse and related leukemia-associated complications are major contributors to mortality. The relapse of AML is associated with a notable increase in molecular complexity, as numerous novel subclones and mutations arise that lead to increased resistance to cytotoxic chemotherapy [4]. Up to 50% of AML patients may relapse after transplantation; thus, early molecular relapse diagnosis is crucial for successful treatment. Waiting for hematological relapse, which has a poor prognosis, is less effective than starting treatment at the molecular relapse stage with a modest disease burden [5]. Inactivation of the tumor suppressor protein p53 (TP53) is a strong promoter of AML and Loss or alteration of TP53 is a significant predictor of poor outcomes in AML. However, TP53 mutations are commonly found in AML cases with increased genomic instability. This suggests that additional factors may contribute to the development and progression of AML, highlighting the complex relationship between TP53 mutations and AML [6].
In AML, the overexpression of Wilms tumor 1 (WT1) functions as an oncogene, unlike its expected role in the BM. The effect of WT1 depends on its interactions with multiple protein partners, such as p53 and Fms-related receptor tyrosine kinase 3 (FLT3). However, it is unclear what triggers the overexpression of WT1 in AML or whether it occurs early or late in disease onset. Furthermore, it is still unclear how a pro-apoptotic factor such as WT1 transforms into an oncogene. The conflicting results from multiple studies continue to be a source of discussion about the prognostic significance of WT1 overexpression in AML [7]. WT1 expression levels increase during relapse and decrease in the bone marrow after HSCT, making the WT1 transcript assay highly sensitive for detecting relapse [8].
This study aimed to investigate the diagnostic potential of WT1 and TP53 gene expression as markers for relapse in AML patients who have undergone HSCT using real-time PCR.
Materials and methods
Patients and sample collection
Twenty AML patients who underwent HSCT at Taleghani Hospital transplant center in Tehran were included in the study. All protocols and sampling were performed following the completion of informed consent forms by patients and obtaining confirmation from the ethics committee of Shahid Beheshti University of Medical Sciences (Ethics code No: IR.SBMU.RETECH.REC.1401.360). Peripheral blood (PB) and bone marrow (BM) samples were collected from patients with relapsed AML after HSCT and individuals in remission after HSCT at Taleghani Hospital in Tehran.
mRNA extraction and expression analysis
Using reverse transcription-quantitative polymerase chain reaction (RT‒qPCR), the relative expression levels of WT1 and TP53 messenger RNAs (mRNAs) in PB and BM samples were determined. PB and BM samples were subjected to total RNA extraction using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) in accordance with the manufacturer’s recommendations. Then, agarose gel electrophoresis was used to assess RNA integrity, and the purity of intact RNA was assessed by NanoDrop. According to the manufacturer’s instructions, cDNA synthesis was performed utilizing the ExcelRT™ Reverse Transcriptase kit developed by SMOBio, a company based in South Korea. A Real-time PCR reaction was conducted in a total volume of 13 µl for the expression analysis step. The composition of the reaction mixture consisted of 6.5 µl of 2× Master Mix (Real Q Plus Master Mix, Denmark), 0.5 µl of each primer, 1 µl of synthesized cDNA, and 4.5 µl of nuclease-free water. The Applied Biosystems StepOnePlus™ Real-time PCR System and Thermal Cycler (USA) was used for this purpose. The reactions were performed under the following conditions: an initial denaturation at 95 °C for 15 min, followed by 40 cycles of denaturation at 95 °C for 15 s, annealing at 60–62 °C for 15 s, extension at 72 °C for 15 s, and a final step of 10 min for the melting curve analysis. The ABL geometric mean cycle threshold (CT) was utilized to calculate the relative expression level, represented as 2−ΔCT. The sequences of the housekeeping gene and mRNA primers are provided in Table 1.
Statistical analysis
The data analysis was performed using two software programs: SPSS version 25 and GraphPad Prism version 9. The Shapiro‒Wilk test was used to confirm the normality of the WT1 and TP53 variable distributions. Additionally, a t test was utilized to assess whether there was any discernible difference in the expression of WT1 and TP53 between AML patients who had relapsed following HSCT and those who were in remission. Furthermore, Pearson’s test was used to measure the linear correlation between WT1 and TP53 expression. The diagnostic value of WT1 and TP53 in the diagnosis of relapse was analyzed by receiver operating characteristic (ROC) analysis. A p value less than 0.05 was considered statistically significant.
Results
Patient data
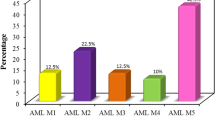
The study included 20 AML patients who underwent HSCT. The average age of the individuals in the study was 51.3 ± 20.5 years, and half of them were of the female gender. Also, the median and age range were 47 and 25–64, respectively. The demographic information was recorded and is presented in Table 2, out of the patients who underwent HSCT, seven experienced relapse, while 13 achieved remission.
mRNA expression
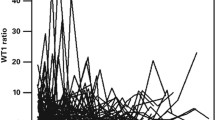
Compared to individuals who experienced remission following HSCT, AML patients who relapsed after HSCT exhibited significantly higher levels of WT1 expression (p value< 0.01). TP53 expression was significantly lower in AML patients who relapsed after HSCT than in the individuals in remission after HSCT (p value < 0.01) (Fig. 1). The analysis of PB samples revealed that individuals who experienced relapse had significantly higher expression levels of WT1 compared to those in remission (p value < 0.05) (Fig. 2A). The analysis further revealed that among individuals who relapsed, those in the age group of 47< exhibited higher expression levels of WT1 compared to those who achieved remission (p value < 0.05) (Fig. 2B).
The analysis of BM samples revealed that individuals who experienced relapse had significantly lower expression levels of TP53 compared to those who achieved remission (p value < 0.05) (Fig. 2C). Furthermore, when considering the age factor, it was observed that among individuals who relapsed, those in the age group of 47 < had lower expression levels of TP53 compared to those who remained in remission (p value < 0.01) (Fig. 2D). Blast percent was significantly higher in the relapse group than in the remission group at diagnosis (p value < 0.05).
Relative expression of WT1 and TP53 in individuals who had relapsed after HSCT and those who had remission after HSCT. a Expression of WT1 in BM and PB samples. b Expression of WT1 in the age < 47 and age > 47 groups. c Expression of TP53 in BM and PB samples. d Expression of TP53 in the age < 47 and age > 47 groups. NS stands for not significant, P < 0.05 *, P < 0.01 **, P < 0.001 ***
ROC analysis results
In our study, we conducted a ROC analysis to assess the diagnostic value of WT1 and TP53 mRNAs in the detection of relapse. The analysis of ROC curves demonstrated that both WT1 and TP53 mRNAs serve as convenient diagnostic markers for relapse after HSCT in AML patients (Fig. 3A and B) (p value: 0.008, 0.008). WT1 had a sensitivity of 0.85 and a specificity of 0.76, and TP53 had a sensitivity of 1 and a specificity of 0.61 for diagnosing relapse after HSCT in AML patients.
Discussion
Recent studies have demonstrated that AML patients who relapse post-HSCT have a poor prognosis. However, it has been increasingly recognized that early intervention at the molecular relapse stage, when the disease burden is minimal, yields more favorable outcomes than waiting for hematological relapse. Therefore, early detection of imminent relapse at the molecular level is crucial for successful therapeutic intervention [9,10,11]. The goal of our study was to examine the potential diagnostic use of WT1 and TP53 gene expression as potential recurrence biomarkers in AML patients who had received HSCT. Real-time PCR and ROC curve analysis were used for the evaluation. The WT1 gene can function as both an oncogene and a tumor suppressor in the development of AML. The tumor suppressive protein p53 plays a crucial role in regulating WT1 activity by physically interacting with it and facilitating its recruitment to the promoter region of WT1 target genes, which modulates their expression. However, the disruption of p53 and WT1 interaction caused by the p53 mutation (p53R248Q) in AML cases can result in the loss of WT1 target gene modulation. Moreover, wild-type p53 is necessary for the antiproliferative activity of WT1 in AML cells, while WT1 promotes AML cell proliferation in the absence of p53 or in the presence of mutated p53. In general, WT1 inhibits AML cell proliferation via a p53-dependent mechanism [12].
According to our findings, patients with relapsed AML had higher levels of WT1 mRNA expression than those in remission. Consistent with our findings, studies on WT1 as a marker for measurable residual disease (MRD) have demonstrated that WT1 expression is generally low in the bone marrow of healthy people but rises in AML patients during diagnosis. After successful treatment for AML, it has been observed that the expression of WT1 decreases but may rise again before clinical relapse [13,14,15,16,17,18,19,20].
In our results, AML patients who had relapsed after HSCT had lower expression of TP53 mRNA compared to the individuals in remission. We did not find any studies that investigated the expression of TP53 mRNA in AML patients who relapsed after HSCT. Nevertheless, a study by Mattsson K et al. revealed upregulation of p53 protein in patients who relapsed compared to relapse-free individuals at 3–6 months post-HSCT, which is in contradiction with our data [21]. It’s difficult to explain. It is anticipated that the expression of TP53 mRNA will be lower in AML patients who relapsed after HSCT than in those who were in remission because TP53 is a tumor suppressor and works in conjunction with WT1 to inhibit proliferation. The WT1 assay is very useful for predicting and managing relapse following allogeneic stem cell transplantation, regardless of the presence of chimeric gene markers [22]. WT1 transcript levels are a more sensitive diagnostic relapse test than the morphologic readout approach utilized in the clinic [23]. WT1 expression post-transplant appears to be a reliable marker of MRD, which is the most important predictor of relapse and survival in AML patients undergoing allogeneic HSCT [24]. In patients with AML undergoing allo-SCT, monitoring of MRDWT1 can be conducted in more than 80% of cases. According to the European LeukemiaNet (ELN) criteria, WT1 overexpression in PB is a highly accurate predictor of post-transplant relapse. Consequently, it is advised to quantify WT1 expression in PB after allo-SCT to identify patients at high risk of poor outcomes. Patients classified as being at very poor risk may benefit from early immunosuppressive drug withdrawal, preemptive donor lymphocyte injection, and/or chemotherapy [25]. These published findings suggest that WT1 can be utilized to detect relapse in AML patients after HSCT at an early stage. Consequently, morphological relapse can be prevented by performing appropriate therapeutic interventions.
So, we decided to evaluate the expression of WT1 and TP53 mRNAs in AML patients who relapsed after HSCT compared to those in remission to study their probable diagnostic potential for relapse after HSCT. On the basis of ROC curve analysis, we determined that WT1 and TP53 expression levels have an excellent capacity for discriminating between relapsed and remission patients. Thus, WT1 and TP53 mRNAs proved to be valuable markers for the diagnosis of relapse in AML patients following HSCT.
We had some limitations in conducting the present study, such as its small sample size. It is of great importance to acknowledge that our sampling procedure was conducted during the COVID-19 pandemic when the frequency of patients visiting medical centers reached its lowest point. This issue had a significant impact on our sampling.
Conclusions
In conclusion, WT1 and TP53 emerged as valuable diagnostic biomarkers for potential early detection of molecular relapse following HSCT in patients with AML. Utilizing these markers can facilitate the timely implementation of appropriate therapeutic interventions to prevent hematological relapse.
Data availability
The data have been incorporated into the manuscript and properly documented and archived under the supervision of the corresponding author.
References
Ganzel C, Manola J, Douer D, Rowe JM, Fernandez HF, Paietta EM et al (2016) Extramedullary Disease in adult acute Myeloid Leukemia is common but lacks Independent significance: analysis of patients in ECOG-ACRIN cancer research group trials, 1980–2008. J Clin Oncol 34(29):3544
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood the Journal of the American Society of Hematology 129(4):424–447
Pollyea DA, Jordan CT (2017) Therapeutic targeting of acute Myeloid Leukemia stem cells. Blood the Journal of the American Society of Hematology 129(12):1627–1635
Short NJ, Rytting ME, Cortes JE (2018) Acute Myeloid Leukemia. The Lancet 392(10147):593–606
Rautenberg C, Germing U, Haas R, Kobbe G, Schroeder T (2019) Relapse of acute Myeloid Leukemia after allogeneic stem cell transplantation: prevention, detection, and treatment. Int J Mol Sci 20(1):228
Barbosa K, Li S, Adams PD, Deshpande AJ (2019) The role of TP53 in acute Myeloid Leukemia: challenges and opportunities. Genes Chromosom Cancer 58(12):875–888
Lazzarotto D, Candoni A (2022) The role of wilms’ Tumor gene (WT1) expression as a marker of minimal residual Disease in acute Myeloid Leukemia. J Clin Med 11(12):3306
Zhao X, Jin S, Zhu H, Xu L, Liu D, Chen H et al (2012) Wilms’ Tumor gene 1 expression: an Independent acute Leukemia prognostic indicator following allogeneic hematopoietic SCT. Bone Marrow Transplant 47(4):499–507
Schmid C, Labopin M, Nagler A, Niederwieser D, Castagna L, Tabrizi R et al (2012) Treatment, risk factors, and outcome of adults with relapsed AML after reduced intensity conditioning for allogeneic stem cell transplantation. Blood the Journal of the American Society of Hematology 119(6):1599–1606
Bejanyan N, Weisdorf DJ, Logan BR, Wang H-L, Devine SM, de Lima M et al (2015) Survival of patients with acute Myeloid Leukemia relapsing after allogeneic hematopoietic cell transplantation: a center for international blood and marrow transplant research study. Biol Blood Marrow Transplant 21(3):454–459
Schroeder T, Rachlis E, Bug G, Stelljes M, Klein S, Steckel NK et al (2015) Treatment of acute Myeloid Leukemia or Myelodysplastic Syndrome relapse after allogeneic stem cell transplantation with azacitidine and donor lymphocyte infusions—a retrospective multicenter analysis from the German Cooperative Transplant Study Group. Biol Blood Marrow Transplant 21(4):653–660
Yao Y, Chai X, Gong C, Zou L (2021) WT1 inhibits AML cell proliferation in a p53-dependent manner. Cell Cycle 20(16):1552–1560
Válková V, Polák J, Marková M, Vítek A, Hájková H, Šálek C et al (2013) Minimal residual Disease detectable by quantitative assessment of WT 1 gene before allogeneic stem cell transplantation in patients in first remission of acute Myeloid Leukemia has an impact on their future prognosis. Clin Transplant 27(1):E21–E9
Polák J, Hájková H, Maalaufová-Soukupová J, Marková J, Šálek C, Schwarz J et al (2012) Estimation of molecular upper remission limit for monitoring minimal residual Disease in peripheral blood of acute Myeloid Leukemia patients by WT1 expression. Experimental and Therapeutic Medicine 3(1):129–133
Weisser M, Kern W, Rauhut S, Schoch C, Hiddemann W, Haferlach T et al (2005) Prognostic impact of RT–PCR-based quantification of WT1 gene expression during MRD monitoring of acute Myeloid Leukemia. Leukemia 19(8):1416–1423
Cilloni D, Renneville A, Hermitte F, Hills RK, Daly S, Jovanovic JV et al (2009) Real-time quantitative polymerase chain reaction detection of minimal residual Disease by standardized WT1 assay to enhance risk stratification in acute Myeloid Leukemia: a European LeukemiaNet study. J Clin Oncol 27(31):5195–5201
Nomdedéu J, Hoyos M, Carricondo M, Bussaglia E, Estivill C, Esteve J et al (2013) Bone marrow WT1 levels at diagnosis, postinduction and postintensification in adult de novo AML. Leukemia 27(11):2157–2164
Rossi G, Minervini MM, Melillo L, Di Nardo F, De Waure C, Scalzulli PR et al (2014) Predictive role of minimal residual Disease and log clearance in acute Myeloid Leukemia: a comparison between multiparameter flow cytometry and Wilm’s Tumor 1 levels. Ann Hematol 93:1149–1157
Paschka P, Marcucci G, Ruppert AS, Whitman SP, Mrózek K, Maharry K et al (2008) Wilms’ Tumor 1 gene mutations independently predict poor outcome in adults with cytogenetically normal acute Myeloid Leukemia: a cancer and Leukemia group B study. J Clin Oncol 26(28):4595
Gray JX, McMillen L, Mollee P, Paul S, Lane S, Bird R et al (2012) WT1 expression as a marker of minimal residual Disease predicts outcome in acute Myeloid Leukemia when measured postconsolidation. Leuk Res 36(4):453–458
Mattsson K, Honkaniemi E, Barbany G, Gustafsson B (2015) Increased p53 protein expression as a potential predictor of early relapse after hematopoietic stem cell transplantation in children with acute myelogenous Leukemia. Pediatr Transplant 19(7):767–775
Ogawa H, Tamaki H, Ikegame K, Soma T, Kawakami M, Tsuboi A et al (2003) The usefulness of monitoring WT1 gene transcripts for the prediction and management of relapse following allogeneic stem cell transplantation in acute type Leukemia. Blood the Journal of the American Society of Hematology 101(5):1698–1704
Israyelyan A, Goldstein L, Tsai W, Aquino L, Forman SJ, Nakamura R et al (2015) Real-time assessment of relapse risk based on the WT1 marker in acute Leukemia and Myelodysplastic Syndrome patients after hematopoietic cell transplantation. Bone Marrow Transplant 50(1):26–33
Pozzi S, Geroldi S, Tedone E, Luchetti S, Grasso R, Colombo N et al (2013) Leukemia relapse after allogeneic transplants for acute Myeloid Leukemia: predictive role of WT 1 expression. Br J Hematol 160(4):503–509
Dulery R, Nibourel O, Gauthier J, Elsermans V, Behal H, Coiteux V et al (2017) Impact of Wilms’ Tumor 1 expression on outcome of patients undergoing allogeneic stem cell transplantation for AML. Bone Marrow Transplant 52(4):539–543
Acknowledgements
We thank the Cellular & Molecular Research Center, Qom University of Medical Sciences, Qom, Iran, and all our colleagues at Shahid Beheshti University of Medical Sciences.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
AA collected the samples, performed the experiments, performed the statistical analyses, and wrote the first version of the manuscript. FF, JG and MM drafted the manuscript and analyzed the data. MM conceived the study, designed and coordinated it, and finalized the manuscript. All authors gave final approval for publication.
Corresponding author
Ethics declarations
Ethics approval
All experimental procedures and protocols were conducted strictly with the ethical guidelines and standards set forth by the institutional and/or national research committee. The present study obtained ethical approval from the ethics committee of Shahid Beheshti University of Medical Sciences, with the assigned ethics code number IR.SBMU.RETECH.REC.1401.360.
Consent to participate
Before participating in the study, all patients provided informed consent by completing the requisite consent form.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Asghari-Ghomi, A., Fallahian, F., Garavand, J. et al. WT1 and TP53 as valuable diagnostic biomarkers for relapse after hematopoietic stem cell transplantation in acute myeloid leukemia. Mol Biol Rep 51, 244 (2024). https://doi.org/10.1007/s11033-023-09185-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-023-09185-8