Abstract
Purpose
This review summarizes the recommendations for the prophylaxis of nausea and vomiting in adults receiving highly emetogenic chemotherapy (HEC) which includes cisplatin, mechlorethamine, streptozocin, cyclophosphamide >1500 mg/m2, carmustine, dacarbazine, and the combination of an anthracycline and cyclophosphamide (AC) administered to women with breast cancer, as agreed at the MASCC/ESMO Antiemetic Guidelines Update meeting in Copenhagen in June 2015.
Methods
A systematic review of the literature using PubMed and the Cochrane Database from 2009 to June 2015 was performed.
Results
The NK1-receptor antagonists netupitant (300 mg given in combination with palonosetron 0.5 mg as NEPA) and rolapitant have both completed phase II and III programs and were approved by FDA (both) and EMA (NEPA) in 2014–2015. Addition of one of these agents (or of (fos)aprepitant) to a combination of a serotonin (5-HT)3-receptor antagonist and dexamethasone improved the number of patients with a complete response (no emesis and no rescue medication) days 1–5 after AC HEC with 8–9 % and after non-AC HEC by 8–20 %. Olanzapine has improved control of delayed nausea as compared to aprepitant in a randomized open designed study. In the prophylaxis of delayed nausea and vomiting, metoclopramide is an option instead of aprepitant in patients receiving cisplatin-based chemotherapy and dexamethasone is an option instead of aprepitant in patients receiving AC chemotherapy.
Conclusions
Two new NK1-receptor antagonists (netupitant and rolapitant) have been included in the updated recommendations as additional options to aprepitant or fosaprepitant. Addition of one of these NK1-receptor antagonists to a combination of a 5-HT3-receptor antagonist and dexamethasone is recommended in both non-AC HEC and AC HEC. Olanzapine is included as an option in HEC in particular if nausea is the main symptom.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This manuscript is an update of the recommendations published after the last MASCC/ESMO antiemetic consensus conference in 2009 [1–3]. It summarizes evidence-based recommendations for the prophylaxis of nausea and vomiting in adult patients receiving high emetic risk chemotherapy.
High emetic risk is defined as a risk of vomiting within the first 24 h after start of chemotherapy of >90 % in patients who do not receive prophylactic antiemetics. In 2009, high emetic risk chemotherapy (HEC) included cisplatin, mechlorethamine, streptozocin, cyclophosphamide >1500 mg/m2, carmustine, and dacarbazine. At that point, the combination of an anthracycline (A) and cyclophosphamide (C) was classified as moderate emetic risk chemotherapy [2], but in the recent MASCC/ESMO update of the emetic risk classification, AC chemotherapy was included in the HEC category [4] and recommendations for AC chemotherapy are included in this review. The recommendations for dose and schedule of antiemetics are given in Table 1 and updated guidelines for the use of antiemetics in HEC in Table 2.
Methods
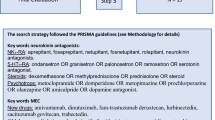
A literature search was done from January 01, 2009, through June 01, 2015, in PubMed and in the Cochrane Database. The keywords included were: (cisplatin OR anthracycline OR cyclophosphamide OR mechlorethamine OR streptozocin OR carmustine OR dacarbazine) AND clinical trial. A supplementary search through PubMed was also completed using the key words: (ondansetron OR granisetron OR dolasetron OR tropisetron OR palonosetron OR ramosetron OR azasetron OR metoclopramide OR domperidone OR metopimazine OR prochlorperazine OR olanzapine OR aprepitant OR fosaprepitant OR netupitant OR rolapitant OR casopitant) AND chemotherapy. The first search resulted in 511 “hits” the second in 819 “hits,” a total of 1330 references. The flow diagram for the literature search is summarized in Fig. 1.
Findings
Since the 2009 update [1–3], numerous studies involving the serotonin (5-HT)3-receptor antagonist, palonosetron, were published; the new neurokinin (NK)1-receptor antagonists netupitant and rolapitant have been approved by the FDA (netupitant as NEPA and rolapitant) and the EMA (netupitant as NEPA), and an intravenous formulation of aprepitant, fosaprepitant, has been marketed. Another NK1-receptor antagonist, casopitant was evaluated in phase III studies [5, 6]; however, it did not receive FDA approval and hence data on this agent will not be included in this review. In addition, the antiemetic effect of olanzapine, an agent targeting multiple receptors, has been further investigated and data will be reviewed. This paper will also review the dose, the schedule, and the route of administration of dexamethasone, the 5-HT3-, and NK1-receptor antagonists.
Recommendations for the use of these agents are given indicating the MASCC level of evidence and consensus and the ESMO type of evidence and grade of recommendation (Table 2).
Dose, schedule, and route of administration of antiemetics
5-HT3-receptor antagonists
ECG changes, particularly QTc prolongation, are a class effect of the 5-HT3-receptor antagonists. The risk may differ between these agents and palonosetron seems to induce the lowest risk [7]. Due to cardiac adverse effects, FDA warnings against both the intravenous dose of dolasetron (Drug Safety Communication, December 2010) and the high 32-mg intravenous dose of ondansetron (Drug Safety Communication, June 2012) have been released. These formulations have therefore been withdrawn [7]. Antiemetic dose recommendations to prevent nausea and vomiting induced by HEC in adults are given in Table 1.
Ondansetron
The 32-mg intravenous dose has been withdrawn. There are no other changes in dose and schedule.
Dolasetron
The intravenous dose has been withdrawn. There are no changes in dose and schedule of the oral formulation.
Granisetron
A randomized, double-blind study (n = 582) found that a transdermal formulation of granisetron was as effective as daily oral granisetron (2 mg/day for 3–5 days) in patients receiving multiple-day moderately or highly emetogenic chemotherapy [8]. A patch providing 3.1 mg granisetron/24 h for up to 7 days has been marketed. There are no other changes in dose and schedule.
Tropisetron
There are no changes in dose and schedule.
Palonosetron
Since the last update, two large randomized, double-blind studies confirmed non-inferiority of the oral 0.5-mg dose compared to the intravenous 0.25-mg dose in patients receiving cisplatin-based chemotherapy [9] or different antineoplastic agents with a moderate emetic potential [10]. The oral formulation of palonosetron 0.5 mg has also been combined with the NK1-receptor antagonist netupitant (see below).
NK1-receptor antagonists
Aprepitant and fosaprepitant
A large randomized, double-blind study (n = 2.247) demonstrated that a single intravenous dose of fosaprepitant 150 mg is non-inferior to a 3-day oral regimen of apepitant (125/80/80 mg) in patients receiving their initial cycle of cisplatin-based (≥70 mg/m2) chemotherapy [11]. A study in young, healthy volunteers (n = 16) showed that the 5-day NK1-receptor binding affinity of a single dose of oral aprepitant 165 mg was as high as a single intravenous dose of fosaprepitant 150 mg [12]. It is unknown if the results can be extrapolated to cancer patients, who are older than the healthy volunteers in the study and typically require 4–6 different drugs each day, running into a risk of drug-drug interaction with the oral formulation. Nevertheless, the single oral dose was approved by the EMA, but not the FDA. No clinical trial has investigated the 165-mg single oral dose.
Netupitant
NEPA, an oral combination of the NK1-receptor antagonist, netupitant, and the 5-HT3-receptor antagonist, palonosetron, was investigated in a randomized, double-blind, dose-ranging phase II study [13]. In a total of 694 chemotherapy-naive, cisplatin-treated patients (≥50 mg/m2) three different oral doses of netupitant (100, 200, and 300 mg) plus oral palonosetron 0.50 mg were compared with oral palonosetron 0.50 mg, all given on day 1. A standard 3-day oral aprepitant regimen plus a single intravenous dose of ondansetron 32 mg was included as an exploratory arm. In the NEPA- and aprepitant arms, patients received 12 mg oral dexamethasone on day 1 and 4 mg twice daily on days 2–4 and in the palonosetron arm the dose of dexamethasone was 20 mg orally day 1 followed by 8 mg twice daily on days 2–4. Aprepitant 125 mg on day 1 and 80 mg on days 2 and 3 was added in the aprepitant arm. The primary parameter was complete response (no emesis and no use of rescue antiemetics) days 1–5. All NEPA doses showed statistically significant superior complete response rates days 1–5 compared with palonosetron (87.4 % NEPA100, 87.6 % NEPA200, and 89.6 % NEPA300 and 76.5 % with palonosetron, p = 0.004–0.018), while 86.6 % of patients receiving aprepitant and ondansetron achieved a complete response. Complete response days 2–5 was also statistically significant superior in the NEPA (and aprepitant) arms compared to palonosetron (p < 0.05). On day 1, the complete response was 93.3, 92.7, and 98.5 %, respectively, versus 89.7 % with palonosetron and 94.8 % with aprepitant and ondansetron. On day 1, only NEPA 300 mg and aprepitant plus ondansetron were significantly superior to palonosetron alone (p < 0.05). Based on these results, a dose of 300 mg NEPA was selected for phase III trials.
Rolapitant
A randomized, double-blind, dose-finding study investigated four different oral doses of rolapitant (9, 22.5, 90, and 180 mg, respectively) in comparison with placebo all combined with intravenous ondansetron 32 mg and oral dexamethasone 20 mg on day 1 followed by dexamethasone 8 mg twice daily on days 2–4. A total of 454 patients receiving cisplatin-based (≥70 mg/m2) chemotherapy were included [14]. The primary endpoint was complete response in the overall phase (days 1–5). All doses of rolapitant statistically significantly improved complete response days 1–5. The greatest benefit was observed with rolapitant 180 mg (62.5 versus 46.7 % on days 1–5, p = 0.032; 87.6 versus 66.7 % on day 1, p = 0.001, and 63.6 versus 48.9 % on days 2–5, p = 0.045). Rolapitant 180 mg (corresponding to 200 mg of rolapitant hydrochloride monohydrate) was subsequently selected for phase III studies.
Dexamethasone and other corticosteroids
No dose-ranging studies with dexamethasone have been completed since the last update of the guidelines [1–3]. Only the day 1 dose of dexamethasone in cisplatin and in anthracycline-cyclophosphamide chemotherapy has been established [15, 16], whereas no randomized trials have investigated the dexamethasone dose on days 2–4. The dose of dexamethasone in combination with an NK1-receptor antagonist has been of particular interest (see paragraph about differences between NK1-receptor antagonists).
Two studies have investigated whether the administration of dexamethasone in patients receiving either AC or moderate risk chemotherapy can be limited to day 1 (steroid-sparing studies), when given in combination with palonosetron [17, 18]. Neither of these studies included an NK1-receptor antagonist as recommended by the guidelines and other 5-HT3-recptor antagonists (than palonosetron) were not investigated; hence, it is uncertain whether the results are restricted to concomitant use with palonosetron or could be extended to all 5-HT3-receptor antagonists. A recent meta-analysis of individual patient data examining the effect of age on outcome in a pooled sample of 405 patients with breast cancer receiving AC chemotherapy support these findings [19]. The overall conclusion is that the benefit of administering dexamethasone beyond day 1 in patients treated with AC chemotherapy and palonosetron is modest. This does not change the guidelines, because the recommendation in AC patients is to use a combination of a 5-HT3-receptor antagonist, dexamethasone, and an NK1-receptor antagonist on day 1 only (aprepitant days 2–3, if the NK1-receptor antagonist chosen day 1 is aprepitant at 125 mg).
New studies
5-HT3-receptor antagonists
No studies with the potential to change the guidelines in AC or cisplatin-treated patients have been published since 2009. Two studies compared granisetron and palonosetron in different settings and did not find major differences [20, 21].
NK1-receptor antagonists
Aprepitant and fosaprepitant in cisplatin-based chemotherapy
The current recommendations in cisplatin-based chemotherapy from 2009 were based on two double-blind phase III trials with identical design comparing standard therapy with ondansetron 32 mg intravenous plus oral dexamethasone 20 mg on day 1, followed by oral dexamethasone 8 mg twice a day on days 2–4 with ondansetron 32 mg intravenous, oral dexamethasone 12 mg, and oral aprepitant 125 mg on day 1, followed by oral dexamethasone 8 mg daily on days 2–4 and oral aprepitant 80 mg on days 2 and 3 [22, 23]. A third study used the same design, but ondansetron was continued in the control arm days 2–4 in an oral dose of 8 mg twice daily [24]. The dexamethasone dose was reduced in the aprepitant arms because one pharmacokinetic study found that aprepitant increased dexamethasone plasma concentrations resulting in approximately twofold increase in area under the curve (AUC). In all three studies, the primary endpoint (complete response, defined as no emesis and no use of rescue antiemetics 0–120 h after the initiation of chemotherapy) was significantly superior with the addition of aprepitant (73 versus 52 %, p < 0.001, 63 versus 43 %, p < 0.001, and 72 versus 61 %, p < 0.003) [22–24].
Subsequently, a double-blind, randomized, non-inferiority study compared the efficacy and tolerability of a single 150-mg intravenous dose of fosaprepitant (a prodrug of aprepitant), with the 3-day oral aprepitant administration in 2247 cancer patients submitted to cisplatin-based chemotherapy [11]. All patients received ondansetron on day 1 and dexamethasone on days 1–4. Complete response rate was not significantly nferior with fosaprepitant with respect to aprepitant. Complete response was achieved in 89.0 versus 88.0 % of patients on day 1, in 74.3 versus 74.2 % on days 2–5, and in 71.9 versus 72.3 % on days 1–5, respectively. Therefore, a single fosaprepitant dose is not inferior to the 3-day oral aprepitant regimen and can be recommended in the prevention of cisplatin-induced emesis. Subsequent studies confirmed the efficacy of the 150-mg single intravenous dose of fosaprepitant [25] and the 3-day oral regimen of aprepitant in cisplatin-based chemotherapy [26].
Aprepitant in women with breast cancer receiving anthracycline-cyclophosphamide chemotherapy
The current recommendations were based on a double-blind, randomized phase III study carried out in 866 breast cancer patients treated with cyclophosphamide plus anthracyclines [27]. The study compared orally administered ondansetron (8 mg twice daily on days 1–3) and dexamethasone (20 mg) versus orally administered ondansetron (8 mg twice daily on day 1), dexamethasone (12 mg), and aprepitant (125 mg on day 1 and 80 mg on days 2–3) (9). Complete response on days 1–5 (the primary endpoint) was significantly superior with aprepitant (51 versus 42 %, p = 0.015) as well as on day 1 (76 versus 69 %, p = 0.034), whereas no significant difference was seen on days 2–5 (55 versus 49 %, p = 0.064). A subsequent study, in which nearly 50 % of the patients received AC chemotherapy and the same antiemetics as in the first study, confirmed these results [28].
Netupitant in cisplatin-based chemotherapy
The phase II NEPA study in cisplatin-treated patients is described within the “Dose, schedule, and route of administration of antiemetics” paragraph [13]. In a phase III study including 413 patients of which 24 % received highly emetogenic chemotherapy (primarily cisplatin), netupitant plus palonosetron plus dexamethasone was investigated during six cycles of chemotherapy [29]. The study focused on safety and in particular no cardiac safety concerns were raised based on cardiac adverse effects and ECGs. In the first cycle of this study [29], 81 % of the patients treated with netupitant 300 mg plus palonosetron and dexamethasone obtained a complete response on days 1–5 as compared to 89.6 % of the patients treated with netupitant 300 mg plus palonosetron and dexamethasone in the phase II study [13].
Netupitant in women with breast cancer receiving anthracycline-cyclophosphamide chemotherapy
A double-blind phase III study including 1455 patients undergoing anthracycline-cyclophosphamide chemotherapy compared NEPA (oral netupitant 300 mg and palonosetron 0.5 mg) plus oral dexamethasone 12 mg with oral palonosetron 0.5 mg plus oral dexamethasone 20 mg [30]. The primary endpoint was the complete response achieved during the delayed phase. The complete response on days 2–5 was significantly superior with netupitant 76.9 versus 69.5 % (p = 0.001) as well as on day 1 (88.4 versus 85.0 %, p = 0.047) and on day 1–5 (74.3 versus 66.6 %, p = 0.001). Addition of netupitant significantly increased the antiemetic effect of palonosetron and dexamethasone in women (98 %) with breast cancer (97–98 %). Although the benefit was less than 10 % as concerns both the primary and secondary efficacy parameters, these differences seems to be clinically relevant, because a significantly higher number of patients in the NEPA arm reported that nausea and vomiting had no impact on daily living as compared to patients in the palonosetron arm.
Rolapitant in cisplatin-based chemotherapy
Rolapitant was approved by the FDA (September 2, 2015) for prevention of delayed nausea and vomiting associated with initial and repeat courses of emetogenic cancer chemotherapy.
Two phase III studies (HEC-1 and HEC-2) have evaluated rolapitant in cisplatin-treated patients. The studies were initially presented separately in abstract form [31, 32], but combined in the full publication [33]. The two phase III studies had the same design and compared the standard antiemetic treatment (granisetron 10 μg/kg iv and oral dexamethasone 20 mg on day 1 and 8 mg twice daily on days 2–4) with granisetron and dexamethasone in the same doses and schedules plus rolapitant 180 mg orally (equivalent to 200 mg rolapitant hydrochloride monohydrate). The dose of dexamethasone was not reduced in the experimental arm because rolapitant is not an inducer or inhibitor of CYP3A4. The primary endpoint of these studies was the complete response on days 2–5 which was significantly superior in the rolapitant arms in both studies (HEC-1 73 versus 58 %, p = 0.0006 [31], and HEC-2 70 versus 62 %, p = 0.043 [32]). Complete responses on day 1 and days 1–5 were 84 versus 74 % (p = 0.0051) and 70 versus 56 % (p = 0.0013), respectively, in HEC 1 and 83 versus 79 % and 68 versus 60 % (both not statistically significant) in HEC-2 [33]. Combining data from these two trials (n = 1.087) [33], the addition of rolapitant significantly improved the effect of granisetron plus dexamethasone compared to placebo in all primary and secondary parameters.
Rolapitant in women with breast cancer receiving anthracycline-cyclophosphamide chemotherapy
A randomized, double-blind phase III study (n = 1369) evaluated rolapitant in patients receiving a combination of anthracycline-cyclophosphamide (AC) or non-AC moderately emetogenic chemotherapy [34]. Oral granisetron (2 mg daily on days 1–3) and dexamethasone (20 mg on day 1) were compared with oral rolapitant (180 mg on day 1) plus oral granisetron and dexamethasone in the same doses and schedules as in the control arm. The primary endpoint was complete response on days 2–5. Protocol-specified subanalysis in women with breast cancer receiving AC (53 %) and patients of different diagnosis receiving non-AC (47 %) chemotherapy were planned. Rolapitant significantly improved the effect of granisetron and dexamethasone both in the entire population and in women with breast cancer receiving AC chemotherapy with respect to complete response days 2–5 (total population 71 versus 62 %, p = 0.0002, and AC population 67 versus 60 %, p = 0.0465). Also, the number of patients obtaining a complete response days 1–5 was significantly improved by rolapitant in the entire population and in the AC subgroup, whereas no significant difference was seen day 1 in either group [34].
Are there differences among the NK1-receptor antagonists in the prevention of nausea and vomiting following high emetic risk chemotherapy?
Differences in pharmacokinetics including risk of drug-drug interactions
Aprepitant is a CYP3A4 substrate and is a moderate inhibitor of CYP3A4 [35, 36]. The AUC and half-life of aprepitant is increased following co-administration with ketoconazole, and decreased following co-administration with rifampicin.
Netupitant has a half-life of approximately 90 h and is also primarily metabolized by CYP3A4 [37]. In vitro data suggest that netupitant inhibits CYP3A4 and is a substrate for and a weak inhibitor of P-glycoprotein (P-gp) [38]. As a consequence, both aprepitant and netupitant significantly increase the exposure of dexamethasone; hence, reduction of dexamethasone doses is recommended during co-administration.
Rolapitant has a half-life of 180 h and is not an inhibitor or inducer of CYP3A4 [39]. It is therefore unlikely that it interacts with drugs metabolized through the CYP3A4 system, and therefore there is no need to reduce the dose of dexamethasone during co-administration [39]. Rolapitant is a moderate inhibitor of CYP2D6 and should not be used concomitantly with CYP2D6 substrates such as thioridazine.
There are a few differences, in terms of DDI profiles of aprepitant and netupitant. For example, aprepitant may reduce the efficacy of hormonal contraception, while netupitant did not significantly affect the exposures to contraceptives [37]. Aprepitant is also a mild inducer of CYP2C9, which can affect the metabolism of tolbutamide [40]. Netupitant, conversely, has not been shown to induce CYP2C9 [38].
Aprepitant has also been shown to exert an inductive effect on CYP3A4; in a study using intravenous midazolam as a probe, administration of a standard 3-day regimen of aprepitant was associated with weak CYP3A4 inhibition on day 4 and weak induction on day 8, with no effect on day 15 [40]. Netupitant and its metabolites have not shown any inductive effects on CYP3A4 [38].
Clinical differences
At present, no comparative studies have been carried out to identify differences in efficacy and toxicity between the three NK1-receptor antagonists. Therefore, when available, choice may be dependent on respective convenience and cost.
Conclusion cisplatin-based and AC-based chemotherapy
Cisplatin-based chemotherapy
The addition of an NK1-receptor antagonist in patients receiving cisplatin chemotherapy increased the complete response on day 1 between 4 and 14 %, on days 2–5 between 8 and 21 %, and on days 1–5 between 8 and 20 % [13, 22–24, 33]. This increase is not only statistically significant but also clinically relevant because of the potential positive impact on the rates of complete response in the first cycle on the subsequent cycles of chemotherapy. The magnitude of the differences observed between the studies could be affected by differences in the control arm, (e.g. differences in 5-HT3-receptor antagonist use). Furthermore, part of the antiemetic effect days 2–5 could also be due to a dependence effect from day 1 (the better results obtained on day 1, the higher chance of complete responses on days 2–5).
The updated MASCC/ESMO guidelines include recommendations for the use of NEPA and rolapitant (Table 2).
AC-treated female patients with breast cancer
The addition of an NK1 receptor antagonist in patients receiving AC chemotherapy for breast cancer increased the complete response on day 1 between 0 and 7 %, on days 2–5 between 6 and 9 % and, on days 1–5 between 8 and 9 % [27, 30, 34]. The improvement in the delayed and overall phases is not only statistically significant but also clinically relevant because of the potential positive impact on the complete response rates in the subsequent cycles of chemotherapy. Similar to the cisplatin studies, the differences in the magnitude of benefit could be influenced by differences in the control arm. Also, as with the cisplatin-based studies, none of the AC chemotherapy studies were designed specifically for the investigation of delayed nausea and vomiting, and a carry-over effect of a day 1 difference cannot be excluded.
Other high emetic risk chemotherapy
These agents include mechlorethamine, streptozocin, cyclophosphamide >1500 mg/m2, carmustine, and dacarbazine. Since the last update in 2009, a few randomized clinical trials have been published. These studies primarily investigated high dose chemotherapy used in connection with stem cell transplantation and are reviewed elsewhere [41]. The recommendation is to add a NK1 receptor antagonist to the combination of a 5-HT3-receptor antagonist and dexamethasone.
Are other antiemetics useful in the prevention of nausea and vomiting following HEC?
Olanzapine
Three recent studies [42–44] of low to moderate quality have investigated the use of olanzapine and are summarized in Table 3.
A randomized, double-blind, phase III trial (published as an abstract only) was performed in 109 (100 evaluable) chemotherapy and radiation therapy naïve patients receiving concurrent local radiation and cisplatin, ≥70 mg/m2 based chemotherapy [45]. Patients were randomized to antiemetic prophylaxis with 10 mg of oral olanzapine, 0.25 mg of intravenous palonosetron and intravenous dexamethasone 20 mg on day 1, and 10 mg/day of oral olanzapine on days 2–4 post-chemotherapy or to 150 mg of intravenous fosaprepitant, 0.25 mg of intravenous palonosetron and intravenous dexamethasone 12 mg on day 1, and 4 mg of oral dexamethasone twice daily on days 2 and 3. Distribution of patients in different groups was similar with respect to gender, types of cancer, and radiotherapy regimens. Complete response (CR) (no emesis, no rescue) was 88 % for the acute period (24 h post-chemotherapy), 76 % for the delayed period (days 2–5 post-chemotherapy), and 76 % for the overall period (0–120 h) for 51 patients receiving the olanzapine regimen. CR was 84 % for the acute period, 73 % for the delayed period, and 73 % for the overall period in 49 patients receiving the fosaprepitant regimen (no significant differences). Patients without nausea (0, scale 0–10, visual analogue scale) were as follows: 86 %, acute; 71 %, delayed; and 71 %, overall for the olanzapine regimen and 77 %, acute; 41 %, delayed; and 41 %, overall for the fosaprepitant regimen (p < 0.01). No grade 3 or 4 toxicities were documented.
A phase II study [46] and a recent randomized, double-blind phase III study published as an abstract only [47], both reported high CR rates and high protection rates against nausea in patients receiving cisplatin-based [46, 47] or AC chemotherapy [47], when olanzapine was combined with a three-drug combination of a 5-HT3-receptor antagonist, dexamethasone, and the NK1 receptor antagonist, aprepitant.
In conclusion, olanzapine seems to be useful in the prophylaxis of delayed nausea (superior to (fos)aprepitant) and equal to (fos)aprepitant in the prevention of acute symptoms. The studies published to date are of low to moderate quality (small sample sizes and/or open design, poorly described patient populations).
Dexamethasone and metoclopramide for delayed nausea and vomiting
Two randomized, double-blind studies, specifically designed to investigate delayed nausea and vomiting, compared the effect of aprepitant with metoclopramide [48] and with dexamethasone [49], respectively.
In the first study [48], 303 chemotherapy-naïve patients received cisplatin-based chemotherapy and intravenous palonosetron 0.25 mg, dexamethasone 12 mg, and oral aprepitant 125 mg as antiemetic prophylaxis (day 1). Patients were randomized to oral dexamethasone 8 mg (days 2–4) plus oral aprepitant 80 mg (days 2–3) or to oral metoclopramide 20 mg four times daily plus oral dexamethasone 8 mg twice daily (both days 2–4). No significant differences were observed on day 1. On days 2–5, the complete response rates (primary parameter, defined as no vomiting and no rescue antiemetics) were 80.3 % (aprepitant plus dexamethasone) versus 82.5 % (p = 0.38). Also, no significant differences were observed with respect to the secondary efficacy parameters and toxicity. The conclusion is that in patients receiving cisplatin-based chemotherapy and the same antiemetic prophylaxis on day 1 (including aprepitant 125 mg), patients could receive either aprepitant (days 2–3) plus dexamethasone (days 2–4) or metoclopramide plus dexamethasone days 2–4.
The other study [49] investigated 580 chemotherapy-naïve women with breast cancer, who received adjuvant anthracycline plus cyclophosphamide and intravenous palonosetron 0.25 mg, dexamethasone 8 mg, and oral aprepitant 125 mg as antiemetic prophylaxis (day 1). Patients were randomized to oral dexamethasone 4 mg twice daily (days 2–3) or oral aprepitant 80 mg (days 2–3). No significant differences were observed on day 1. On days 2–5, the complete response rates (primary parameter, defined as no vomiting and no rescue antiemetics) were identical in both arms (79.5 %). Also, no significant differences were observed with respect to the secondary efficacy parameters, but significantly more patients complained of heartburn and insomnia in the dexamethasone group on days 2–5. The conclusion is that in patients receiving AC chemotherapy and the same antiemetic prophylaxis on day 1 (including aprepitant 125 mg), patients could receive either aprepitant (days 2–3) or dexamethasone days 2–3.
Overall conclusion
Since the last MASCC/ESMO consensus conference in 2009, the most important achievements have been the FDA (netupitant and rolapitant) and the EMA (netupitant) approval of two new NK1-receptor antagonists. These approvals were based on large phase II and III investigational programs. In addition, the combination of an anthracycline and cyclophosphamide in women with breast cancer is now recognized to be highly emetogenic. Olanzapine, a multiple receptor targeting agent, seems useful in the prevention of HEC-induced delayed nausea, but higher quality studies are warranted.
References
Kris MG, Tonato M, Bria E, Ballatori E, Espersen B, Herrstedt J, Rittenberg C, Einhorn LH, Grunberg S, Saito M, Morrow G, Hesketh P (2011) Consensus recommendations for the prevention of vomiting and nausea following high-emetic-risk chemotherapy. Support Care Cancer 19(Suppl 1):S25–S32
Herrstedt J, Rapoport B, Warr D, Roila F, Bria E, Rittenberg C, Hesketh PJ (2011) Acute emesis: moderately emetogenic chemotherapy. Support Care Cancer 19(Suppl):S15–S23
Roila F, Herrstedt J, Aapro M et al (2010) Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol 21(suppl 5):v232–v243
Jordan K, Chan A, Gralla RJ, Jahn F, Rapoport B, Warr D, Hesketh PJ (2016) Emetic risk classification and evaluation of the emetogenicity of antineoplastic agents. Support Care Cancer 24 (in review)
Grunberg SM, Rolski J, Strausz J, Aziz Z, Lane S, Russo MW, Wissel P, Guckert M, Wright O, Herrstedt J (2009) Efficacy and safety of casopitant mesylate, a neurokinin 1 (NK1)-receptor antagonist, in prevention of chemotherapy-induced nausea and vomiting in patients receiving cisplatin-based highly emetogenic chemotherapy: a randomised, double-blind, placebo-controlled trial. Lancet Oncol 10:549–558
Herrstedt J, Apornwirat W, Shaharyar A, Aziz Z, Roila F, Van Belle S, Russo MW, Levin J, Ranganathan S, Guckert M, Grunberg SM (2009) Phase III trial of casopitant, a novel neurokinin-1 receptor antagonist, for the prevention of nausea and vomiting in patients receiving moderately emetogenic chemotherapy. J Clin Oncol 27:5363–5369
Brygger L, Herrstedt J (2014) 5-Hydroxytryptamine3 receptor antagonists and cardiac side effects. Expert Opin Drug Saf 13:1407–1422
Boccia RV, Gordan LN, Clark G, Howell JD, Grunberg SM, Sancuso Study Group (2011) Efficacy and tolerability of transdermal granisetron for the control of chemotherapy-induced nausea and vomiting associated with moderately and highly emetogenic multi-day chemotherapy: a randomized, double-blind, phase III study. Support Care Cancer 19:1609–1617
Karthaus M, Tibor C, Lorusso V et al (2015) Efficacy and safety of oral palonosetron compared with IV palonosetron administered with dexamethasone for the prevention of chemotherapy-induced nausea and vomiting (CINV) in patients with solid tumors receiving cisplatin-based highly emetogenic chemotherapy (HEC). Support Care Cancer 23:2917–2923
Boccia R, Grunberg S, Franco-Gonzales E, Rubenstein E, Voisin D (2013) Efficacy of oral palonosetron compared to intravenous palonosetron for the prevention of chemotherapy-induced nausea and vomiting associated with moderately emetogenic chemotherapy: a phase 3 trial. Support Care Cancer 21:1453–1460
Grunberg S, Chua D, Maru A, Dinis J, DeVandry S, Boice JA, Hardwick JS, Beckford E, Taylor A, Carides A, Roila F, Herrstedt J (2011) Single-dose fosaprepitant for the prevention of chemotherapy-induced nausea and vomiting associated with cisplatin therapy: randomized, double-blind study protocol—EASE. J Clin Oncol 29:1495–1501
Van Laere K, De Hoon J, Bormans G, Koole M, Derdelinckx I, De Lepeleire I, Declercq R, Sanabria Bohorquez SM, Hamill T, Mozley PD, Tatosian D, Xie W, Liu Y, Liu F, Zappacosta P, Mahon C, Butterfield KL, Rosen LB, Murphy MG, Hargreaves RJ, Wagner JA, Shadle CR (2012) Equivalent dynamic human brain NK1-receptor occupancy following single-dose i.v. fosaprepitant vs. oral aprepitant as assessed by PET imaging. Clin Pharmacol Ther 92:243–250
Hesketh PJ, Rossi G, Rizzi G, Palmas M, Alyasova A, Bondarenko I, Lisyanskaya A, Gralla RJ (2014) Efficacy and safety of NEPA, an oral combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy: a randomized dose-ranging pivotal study. Ann Oncol 25:1340–1346
Rapoport B, Chua D, Poma A et al (2015) Study of rolapitant, a novel, long-acting, NK1 receptor antagonist, for the prevention of chemotherapy-induced nausea and vomiting due to highly emetogenic chemotherapy. Support Care Cancer 23:3281–3288
The Italian group for Antiemetic Research (1998) Double-blind, dose-finding study of four intravenous doses of dexamethasone in the prevention of cisplatin-induced acute emesis. J Clin Oncol 16:2937–2942
The Italian group for Antiemetic Research (2004) Randomized, double-blind, dose-finding study of dexamethasone in preventing acute emesis induced by anthracyclines, carboplatin, or cyclophosphamide. J Clin Oncol 22:725–729
Celio L, Frustaci S, Denaro A et al (2011) Palonosetron in combination with 1-day versus 3-day dexamethasone for prevention of nausea and vomiting following moderately emetogenic chemotherapy: a randomised, multicenter, phase III trial. Support Care Cancer 19:1217–1225
Aapro M, Fabi A, Nole F et al (2010) Double-blind, randomised, controlled study of the efficacy and tolerability of palonosetron plus dexamethasone for 1 day with or without dexamethasone on days 2 and 3 in the prevention of nausea and vomiting induced by moderately emetogenic chemotherapy. Ann Oncol 21:1083–1088
Celio L, Bonizzoni E, Bajetta E, Sebastiani S, Perrone T, Aapro MS (2013) Palonosetron plus single-dose dexamethasone for the prevention of nausea and vomiting in women receiving anthracycline/cyclophosphamide-containing chemotherapy: meta-analysis of individual patient data examining the effect of age on outcome in two phase III trials. Support Care Cancer 21:565–573
Raftopoulos H, Cooper W, O’Boyle E, Gabrail N, Boccia R, Gralla RJ (2015) Comparison of an extended-release formulation of granisetron (APF530) versus palonosetron for the prevention of chemotherapy-induced nausea and vomiting associated with moderately or highly emetogenic chemotherapy: results of a prospective, randomized, double-blind, noninferiority phase 3 trial. Support Care Cancer 23:723–732
Roscoe JA, Heckler CE, Morrow GR et al (2012) Prevention of delayed nausea: a University Of Rochester Cancer Center Community Clinical Oncology Program study of patients receiving chemotherapy. J Clin Oncol 30:3389–3395
Hesketh PJ, Grunberg SM, Gralla RJ et al (2003) The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin—the Aprepitant Protocol 052 Study Group. J Clin Oncol 21:4112–4119
Poli-Bigelli S, Rodrigues-Pereira J, Carides AD et al (2003) Addition of the neurokinin 1 receptor antagonist aprepitant to standard antiemetic therapy improves control of chemotherapy-induced nausea and vomiting. Results from a randomized, double-blind, placebo-controlled trial in Latin America. Cancer 97:3090–3098
Schmoll HJ, Aapro MS, Poli-Bigelli S et al (2006) Comparison of an aprepitant regimen with a multiple-day ondansetron regimen, both with dexamethasone, for antiemetic efficacy in high-dose cisplatin treatment. Ann Oncol 17:1000–1006
Saito H, Yoshizawa H, Yoshimori K, Katakami N, Katsumata N, Kawahara M, Eguchi K (2013) Efficacy and safety of single-dose fosaprepitant in the prevention of chemotherapy-induced nausea and vomiting in patients receiving high-dose cisplatin: a multicentre, randomised, double-blind, placebo-controlled phase 3 trial. Ann Oncol 24:1067–1073
Hu Z, Cheng Y, Zhang H, Zhou C, Han B, Zhang Y et al (2014) Aprepitant triple therapy for the prevention of chemotherapy-induced nausea and vomiting following high-dose cisplatin in Chinese patients: a randomized, double-blind, placebo-controlled phase III trial. Support Care Cancer 22:979–987
Warr DG, Hesketh PJ, Gralla RJ, Muss HB, Herrstedt J, Eisenberg PD, Raftopoulos H, Grunberg SM, Gabriel M, Rodgers A, Bohidar N, Klinger G, Hustad CM, Horgan KJ, Skobieranda F (2005) Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breast cancer after moderately emetogenic chemotherapy. J Clin Oncol 23:2822–2830
Rapoport BL, Jordan K, Boice JA et al (2010) Aprepitant for the prevention of chemotherapy-induced nausea and vomiting associated with a broad range of moderately emetogenic chemotherapies and tumor types: a randomized, double-blind study. Support Care Cancer 18:423–431
Gralla RJ, Bosnjak SM, Hontsa A, Balser C, Rizzi G, Rossi G, Borroni ME, Jordan K (2014) A phase III study evaluating the safety and efficacy of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting over repeated cycles of chemotherapy. Ann Oncol 25:1333–1339
Aapro M, Rugo H, Rossi G, Rizzi G, Borroni ME, Bondarenko I, Sarosiek T, Oprean C, Cardona-Huerta S, Lorusso V, Karthaus M, Schwarcbrszberg L, Grunberg S (2014) A randomized phase III study evaluating the efficacy and safety of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy. Ann Oncol 25:1328–1333
Rapoport B, Poma A, Hedley ML, Martell RE, Navari RM (2014) Phase 3 trial results for rolapitant, a novel NK-1 receptor antagonist, in the prevention of chemotherapy-induced nausea and vomiting in subjects receiving highly emetogenic chemotherapy. J Clin Oncol 32(suppl 5):636, A 9638
Schnadig ID, Modiano MR, Poma A, Hedley ML, Martell RE, Schwartzberg LS (2014) Phase 3 trial results for rolapitant, a novel NK-1 receptor antagonist, in the prevention of chemotherapy-induced nausea and vomiting (CINV) in subjects receiving moderately emetogenic chemotherapy (MEC). J Clin Oncol 32(suppl 5):635, A9633
Rapoport BL, Chasen MR, Gridelli C, Urban L, Modiano MR, Schnadig ID, Poma A, Arora S, Kansra V, Schwartzberg LS, Navari RM (2015) Safety and efficacy of rolapitant for prevention of chemotherapy-induced nausea and vomiting after administration of cisplatin-based highly emetogenic chemotherapy in patients with cancer: two randomised, active-controlled, double-blind, phase 3 trials. Lancet Oncol 16:1079–1089
Schwartzberg LS, Modiano MR, Rapoport BL, Chasen MR, Gridelli C, Urban L, Poma A, Arora S, Navari RM, Schnadig ID (2015) Safety and efficacy of rolapitant for prevention of chemotherapy-induced nausea and vomiting after administration of moderately emetogenic chemotherapy or anthracycline and cyclophosphamide regimens in patients with cancer: a randomised, active-controlled, double-blind, phase 3 trial. Lancet Oncol 16:1071–1078
Sanchez RI, Wang RW, Newton DJ, Bakhtiar R, Lu P, Chiu S-H, Evans DC, Huskey SE (2004) Cytochrome P450 3A4 is the major enzyme involved in the metabolism of the substance P receptor antagonist, aprepitant. Drug Metab Dis 32:1287–1292
Majumdar AK, McCrea JB, Panebianco DL et al (2003) Effects of aprepitant on cytochrome P450 3A4 activity using midazolam as a probe. Clin Pharmacol Ther 74:150–156
Calcagnile S, Lanzarotti C, Rossi G et al (2013) Effect of netupitant, a highly selective NK1 receptor antagonist, on the pharmacokinetics of palonosetron and impact of the fixed dose combination of netupitant and palonosetron when coadministered with ketoconazole, rifampicin, and oral contraceptives. Support Care Cancer 21:2879–2887
Natale JJ, Spinelli T, Calcagnile S, Lanzarotti C, Rossi G, Cox D, Kashef K (2015) Drug–drug interaction profile of components of a fixed combination of netupitant and palonosetron: review of clinical data. J Oncol Pharm Pract. doi:10.1177/1078155215586824
Rojas C, Slusher BS (2015) Mechanisms and latest clinical studies of new NK1 receptor antagonists for chemotherapy-induced nausea and vomiting: rolapitant and NEPA (netupitant/palonosetron). Cancer Treat Rev 41(10):904–913
Sanchez RI, Wang RW, Newton DJ et al (2004) Cytochrome P450 3A4 is the major enzyme involved in the metabolism of the substance P receptor antagonist aprepitant. Drug Metab Dispos 32:1287–1292
Einhorn LH, Rapoport B, Navari R, Herrstedt J, Brames MJ (2016). Antiemetic therapy for multiple-day chemotherapy, high dose chemotherapy, and breakthrough nausea and vomiting: review and consensus statements. Support Care Cancer 24.
Tan L, Liu J, Liu X et al (2009) Clinical research of olanzapine for prevention of chemotherapy-induced nausea and vomiting. J Exp Clin Cancer Res 28:131. doi:10.1186/1756-9966-28-131
Navari RM, Gray SE, Kerr AC (2011) Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol 9:188–195
Mizukami N, Yamanchi M, Koike K et al (2014) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting in patients receiving highly or moderately emetogenic chemotherapy: a randomized, double-blind, placebo-controlled study. J Pain Symptom Manag 47:542–550
Navari RM, Nagy CK (2015). Olanzapine versus fosaprepitant for the prevention of nausea and vomiting in patients receiving concurrent chemoradiation treatment. J Clin Oncol 33: (suppl; abstr 9502).
Abe M, Hirashima Y, Kasamatsu Y et al (2016) Efficacy and safety of olanzapine combined with aprepitant, palonosetron, and dexamethasone for preventing nausea and vomiting induced by cisplatin-based chemotherapy in gynecological cancer: KCOG-G1301 phase II trial. Support Care Cancer 24:675–682
Navari RM, Qin R, Ruddy KJ et al (2015) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting (CINV) in patients receiving highly emetogenic chemotherapy (HEC): alliance A221301, a randomized, double-blind, placebo-controlled trial. J Clin Oncol 33(suppl 29S):abstract 176
Roila F, Ruggeri B, Ballatori E et al (2015) Aprepitant versus metoclopramide, both combined with dexamethasone, for the prevention of cisplatin-induced delayed emesis: a randomized, double-blind study. Ann Oncol 26:1248–1253
Roila F, Ruggeri B, Ballatori E, Del Favero A, Tonato M (2013) Aprepitant versus dexamethasone for preventing chemotherapy-induced delayed emesis in patients with breast cancer: a randomized double-blind study. J Clin Oncol 32:101–106
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jørn Herrstedt: Consultant Tesaro and remuneration SOBI.
Fausto Roila: No conflict of interest.
David Warr: Consultant Helsinn, Merck, Tesaro.
Luigi Celio: Consultant Helsinn.
Rudolp M Navari: Consultant Tesaro.
Paul J Hesketh: No conflict of interest.
Alexandre Chan: Consultant and remuneration MSD.
Matti S Aapro: Consultant Helsinn, Merck/MSD, Tesaro, remuneration Helsinn, Tesaro, Roche, Esai, Merk/MSD and funding Helsinn.
Rights and permissions
About this article
Cite this article
Herrstedt, J., Roila, F., Warr, D. et al. 2016 Updated MASCC/ESMO Consensus Recommendations: Prevention of Nausea and Vomiting Following High Emetic Risk Chemotherapy. Support Care Cancer 25, 277–288 (2017). https://doi.org/10.1007/s00520-016-3313-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3313-0