Abstract
Purpose
Rolapitant is a novel, long-acting neurokinin-1 (NK-1) receptor antagonist. This study evaluated the safety and efficacy of four different doses of rolapitant for prevention of chemotherapy-induced nausea and vomiting (CINV) due to highly emetogenic chemotherapy (HEC).
Methods
This randomized, double-blind, active-controlled, global study was conducted in patients receiving cisplatin-based chemotherapy ≥70 mg/m2. Patients received a 9, 22.5, 90, or 180 mg oral dose of rolapitant or placebo with ondansetron and dexamethasone on day 1 of chemotherapy. The primary end point was complete response (CR; no emesis and no use of rescue medication) in the overall (0 to 120 h) phase of cycle 1. Other assessments were CR in delayed (24–120 h) and acute (0–24 h) phases, no emesis, no significant nausea, and no nausea.
Results
Four hundred fifty-four patients were randomized. All doses of rolapitant improved CR with the greatest benefit observed with rolapitant 180 mg vs. active control in the overall phase (62.5 and 46.7 %, p = 0.032) and in the acute (87.6 vs. 66.7 %, p = 0.001) and delayed (63.6 vs. 48.9 %, p = 0.045) phases. Rates for no emesis and no significant nausea were significantly (p < 0.05) higher with rolapitant 180 mg vs. active control in the overall, acute, and delayed phases. Treatment-related adverse events were largely considered related to the chemotherapy and included constipation, headache, fatigue, and dizziness which were mostly mild or moderate and were similar across treatment groups.
Conclusion
All doses of rolapitant were well tolerated and showed greater CR rates than active control. Rolapitant 180 mg demonstrated significant clinical efficacy for preventing CINV in the overall, delayed, and acute phases for patients receiving HEC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced nausea and vomiting (CINV) can affect up to 90 % of patients receiving chemotherapy, reduce treatment adherence over multiple chemotherapy cycles, and ultimately impact treatment success [1–3]. Patients are at risk of developing CINV for up to 120 h following chemotherapy, necessitating protection for this entire 5-day period. This 120-h at-risk period for CINV includes an acute phase (0 to <24 h), a delayed phase (24 to 120 h), and an overall phase (0 to 120 h). Delayed emesis occurs in up to 50 % of patients post-chemotherapy [4] and is not adequately addressed by most standard therapies. Young age, female gender, history of nausea, and lack of response to previous therapy may place patients at greater risk for CINV [5, 6]. Prevention of CINV is essential for increasing patient adherence to chemotherapy and optimizing opportunities for treatment success [7, 8].
Greater understanding of the physiological and molecular pathways underlying CINV has resulted in recently revised treatment guidelines [2, 9–12]. Guidelines now recommend a multimodal approach that incorporates a prophylactic regimen prior to chemotherapy, consisting of a neurokinin-1 (NK-1) receptor antagonist with a serotonin-3 (5-HT3) receptor antagonist and dexamethasone for highly emetogenic chemotherapy (HEC), such as cisplatin or anthracycline/cyclophosphamide [1, 2, 10–13]. As other existing treatment guidelines for CINV are revised, they likely will include recommendations that follow this multimodal approach. Improvement in the management of patients experiencing CINV has been demonstrated with NK-1 receptor antagonists [14], which are approved for prevention of acute and delayed nausea and vomiting associated with HEC and MEC [10, 15–18].
Rolapitant is a potent, selective, high-affinity, competitive NK-1 receptor antagonist with an extended half-life of approximately 180 h [19]. Positron emission tomography (PET) imaging performed in healthy volunteers 5 days (120 h) after a single oral 180-mg dose of rolapitant (equivalent to 200 mg rolapitant hydrochloride monohydrate) demonstrated greater than 90 % NK-1 receptor occupancy in the brain [20], suggesting that a single dose may be sufficient to prevent CINV during the entire risk period of 0 to 120 h. Rolapitant is not an inhibitor or inducer of CYP P450 3A4 (CYP3A4) and, consequently, is unlikely to interact with drugs metabolized through the CYP3A4 system; many drugs metabolized via this system are administered to cancer patients undergoing chemotherapy [19].
We describe here the results of a global, multicenter, randomized, double-blind, active-controlled pivotal study to evaluate whether the administration of rolapitant, ondansetron, and dexamethasone prevents CINV in the combined acute and delayed phase (0 to 120 h) compared with the administration of an active control therapy of ondansetron and dexamethasone in patients receiving cisplatin-based HEC.
Methods
This was a pivotal phase 2, global, multicenter, randomized, double-blind, active-controlled, parallel-group, dose-ranging study conducted at 75 sites in 21 countries. Prior to study initiation, the clinical study protocol and amendments and the written informed consent form were reviewed and approved by Independent Ethics Committees. The study was conducted in accordance with good clinical practice (GCP). Written informed consent was obtained from each patient prior to any study-related activity. This study was registered at clinicaltrials.gov: NCT00394966.
Patient selection
Male and female patients were considered eligible if they were ≥18 years with a Karnofsky Performance Status (KPS) score ≥60; had a predicted life expectancy ≥3 months; had adequate bone marrow, kidney, and liver function; and were scheduled to receive HEC (≥70 mg/m2 cisplatin-based chemotherapy). Patients were excluded if they had previously received cisplatin or had received within 5 days prior to the study 5-HT3 receptor antagonists, NK-1 receptor antagonists, or other drugs that could interfere with the study; if they were scheduled to receive any radiation therapy to the abdomen or pelvis from day 5 to day 6; and if they had received systemic corticosteroids within 72 h of day 1 of the study, except as premedication for taxane-based chemotherapy. Patients who were receiving chronic daily steroid therapy could be enrolled provided that the daily steroid dose was ≤10 mg of prednisone or equivalent. Patients who had ongoing vomiting caused by any etiology were also excluded.
Study treatments
Eligible patients were randomized to receive rolapitant 9, 22.5, 90, or 180 mg (equivalent to 10, 25, 100, or 200 mg rolapitant hydrochloride monohydrate) or placebo administered approximately 2 h prior to the first dose of chemotherapeutic agent on day 1 of cycle 1 (Fig. 1). Randomization was stratified by gender and concomitant emetogenic chemotherapy use. Intravenous (IV) ondansetron 32 mg and oral dexamethasone 20 mg were administered to all patients 0.5 h before initiation of chemotherapy on day 1. Dexamethasone 8 mg twice daily was administered on days 2, 3, and 4. At the end of cycle 1, patients were eligible to continue the same treatment regimen for up to five additional cycles. Patients who experienced intolerable nausea and/or vomiting during the study were permitted to take rescue medication. The rescue medication regimen was at the discretion of the investigator. A patient who required rescue medication in cycle 1 was allowed to continue participating in the study but was considered to have failed the primary end point of complete response (CR).
Study assessments
In cycle 1, patients recorded nausea, emesis, and use of rescue therapy daily in a study diary from days 1 to 6. Nausea was self-assessed using a 100-mm horizontal 10-point visual analog scale (VAS) in the study diary. Emesis, use of rescue medication, and nausea data were used to assess response rates in the overall (0 to 120 h), acute (0 to 24 h), and delayed (>24 to 120 h) phases of CINV following initiation of emetogenic chemotherapy. CR was defined as no emesis and no rescue medication. No emesis was defined as no vomiting, retching, or dry heaves, regardless of rescue medication use. No nausea was a maximum VAS <5 mm, and no significant nausea was a maximum VAS score <25 mm. Complete protection was no emesis, no rescue medication use, and a maximum VAS score <25 mm. Total control was no emesis, no rescue medication, and a maximum nausea VAS score of <5 mm. Quality of life (QoL) was measured by the Functional Living Index-Emesis (FLIE) questionnaire [21] and reported as a total score derived from 18 questions on a 7-point scale. No impact on daily life was defined as total FLIE score of more than 108. Safety and tolerability were assessed from adverse event (AE) reporting (relationship to study treatment was determined by study investigator), physical examinations, vital signs, electrocardiograms (ECGs), and clinical laboratory values.
Statistical analysis
This study planned to randomize approximately 450 patients to one of five treatment arms to achieve a total of 425 evaluable patients. With 85 patients per group, the study had 80 % power to detect a 21 % difference in CR rate between the rolapitant arm and placebo at an alpha = 0.049 level of significance (two-sided), assuming a placebo response rate of 50 %. The primary analysis was based on all randomized patients who received cisplatin-based chemotherapy and a dose of study medication and had at least one post-treatment efficacy assessment in cycle 1 recorded.
The primary objective of this study was to determine if the administration of rolapitant with ondansetron and dexamethasone in patients receiving HEC improved outcomes in the combined acute and delayed phases of CINV compared with the administration of placebo with ondansetron and dexamethasone. The primary assessment of efficacy was CR overall during cycle 1.
The primary analysis was conducted using a logistic regression model with terms for treatment, sex, and use of concomitant chemotherapy. To control for multiple comparisons, CR overall was analyzed in a stepwise manner starting with the highest dose of rolapitant compared with active control, followed by the next lower dose, and so forth sequentially. Sequential testing for the next lower dose occurred only if the previous comparison was statistically significant. Likewise, secondary end points of CR for the delayed and acute phase were tested in a stepwise fashion, starting with the highest dose that met significance for the primary end point. No adjustment for multiplicity was performed for the remaining secondary efficacy end points. Dichotomous response variables were analyzed using the same logistic regression model as described for CR. The time to first emesis or to rescue medication use was summarized using Kaplan-Meier (K-M) curves, and each dose comparison with active control used the log-rank test.
Results
A total of 454 patients were randomized to study treatment. Of these patients, 416 (91.6 %) completed cycle 1. The most common reason for discontinuation during cycle 1 was adverse events (8.4 %) (Fig. 1). Baseline demographic and clinical characteristics were similar across treatment groups (Table 1). Overall, 85.7 % of patients received concomitant emetogenic chemotherapy (CEC), and 99.1 % had a KPS of >60. The median duration of each cycle ranged from 26 to 28 days.
Efficacy
The rolapitant 180 mg group demonstrated significantly greater CR compared with active control (62.5 and 46.7 %, p = 0.032) in the overall phase, the primary end point of the study (Fig. 2). In addition, the rolapitant 180 mg group achieved statistically significant improvement compared with active control for CR in the acute phase (87.6 and 66.7 %, p = 0.001) and the delayed phase (63.6 and 48.9 %, p = 0.045). CR rates across all phases of CINV were consistently higher for all other rolapitant dose groups compared with active control, except for the 9 mg group in the acute phase, but did not achieve statistical significance.
Rolapitant 180 mg was also statistically superior to active control for several key secondary efficacy variables (Table 2). Rolapitant 180 mg had significantly greater rates of no emesis in the overall (67.0 and 46.7 %, p = 0.006), acute (91.0 vs 67.8 %, p < 0.001), and delayed phases (68.2 and 48.9 %, p = 0.008) compared with the active control group (Fig. 2). Significantly greater rates of no emesis were also observed in the rolapitant 90 mg group compared with active control, in the overall (61.5 and 46.7 %, p = 0.042) and the delayed phases (67.0 and 48.9 %, p = 0.012), but not in the acute phase (76.9 and 67.8 %, p = 0.162). Rates of no emesis for the rolapitant 9 and 22.5 mg groups did not achieve statistical significance compared with active control.
The rolapitant 180 mg group had significantly greater rates of no significant nausea in the overall (63.2 and 42.2 %, p = 0.005), acute (86.5 and 73.3 %, p = 0.029), and delayed (64.4 and 47.8 %, p = 0.026) phases compared with active control (Fig. 2). Response rates for no nausea in the overall, acute, and delayed phases did not achieve statistical significance for any rolapitant group compared with active control.
Fewer patients in the rolapitant 180 mg group required rescue medication (14 %) compared with active control (25 %). Time to first emesis or to rescue medication use was significantly longer during cycle 1 for patients treated with rolapitant 180 mg compared with active control (p = 0.011; Fig. 3). The K-M curve for the rolapitant 180 mg group demonstrated clear separation from the active control group as early as 6 h. For both treatment groups, the K-M curves reached a plateau at approximately 80 hours after the initiation of chemotherapy and remained separated thereafter, indicating a sustained benefit in the delayed phase.
Response rates for total control (no emesis, no rescue medication, and a maximum nausea VAS score of <5 mm) in the overall, acute, and delayed phases did not achieve statistical significance for any rolapitant group, but the 180-mg dose group demonstrated numerically higher rates in the overall (30.3 and 23.3 %), acute (51.7 and 48.9 %), and delayed (32.6 and 24.4 %) phases compared with active control. A significantly greater rate of complete protection (no emesis, no rescue medication, and a maximum nausea VAS score of <25 mm) was observed for rolapitant 180 mg in the acute phase (80.9 and 63.3 %, p = 0.009), but not in the delayed (52.9 and 42.2 %, p = 0.151) or overall (52.9 and 38.9 %, p = 0.058) phase compared with active control. Rates of complete protection for the other rolapitant groups did not achieve statistical significance in any phase.
Rolapitant 90- and 180-mg doses significantly (p < 0.05) improved the QoL of patients compared with active control, as determined by total nausea and vomiting scores of the FLIE questionnaire. The proportion of patients reporting no impact on daily life (FLIE score >108) was 65.1 and 62.6 % for rolapitant 180- and 90-mg doses compared with 44.4 % for active control (p = 0.005 and p = 0.012, respectively).
Safety
An overall summary of the most common treatment-related AEs by treatment in cycle 1 is shown in Table 3. Treatment-related AEs were generally mild and included constipation, headache, fatigue, and dizziness. Overall, serious AEs (SAEs) occurred in 52 (11 %) of 454 randomized patients during cycle 1. The incidence of SAEs was similar in all treatment groups and ranged from 9 to 14 %. SAEs were most likely related to chemotherapy or disease progression and included febrile neutropenia (3 %), neutropenia (1 %), vomiting (1 %), dehydration (1 %), nausea (1 %), pneumonia (1 %), and renal failure (1 %). All SAEs were considered unrelated to study drug, except for one SAE each of dizziness (9-mg dose group), elevated blood creatinine (90-mg dose group), and convulsions (90-mg dose group). Only the SAE of convulsion resulted in study discontinuation. This patient had prior history of convulsions associated with hyponatremia, and in this study, the convulsion AE also occurred concurrently with hyponatremia.
During cycle 1, 12 deaths occurred across treatment groups with no discernible dose trend: rolapitant 9 mg (n = 1), 22.5 mg (n = 4), 90 mg (n = 1), and 180 mg groups (n = 5) and active control (n = 1). None of the deaths were considered related to study drug and were most likely due to disease progression or chemotherapy. No appreciable safety concerns or dose-related effects were ascertained in clinical laboratory tests and measurements of vital signs and ECGs.
Discussion
This pivotal global study evaluated the efficacy, safety, and tolerability of the NK-1 receptor antagonist, rolapitant, for prevention of CINV. These results provide strong initial support to the superiority of rolapitant 180 mg over active control for the primary and secondary end points in patients with CINV in cycle 1. After correcting for multiple comparisons, results with rolapitant 180 mg are statistically robust, demonstrating significant improvements in CR compared with active control during cycle 1. In addition, improvements were observed, with no emesis and no significant nausea compared with active control during cycle 1. All other rolapitant dose groups generally achieved numerically greater response compared with active control for the CR, no emesis, and no significant nausea efficacy end points. Even though there are no studies directly comparing NK-1 receptor antagonists, the overall CR rate with rolapitant 180 mg (62.5 %) appears consistent with CR rates observed with other NK-1 receptor antagonists in patients with HEC treated for CINV [22–25] and greater than those observed with the 5-HT3 receptor antagonist palonosetron used without an NK-1 receptor antagonist [26].
Rolapitant was safe and well tolerated for all doses tested in this study. The incidence of AEs did not differ between rolapitant and active control. The AE profile of rolapitant is consistent with that of other NK-1 receptor antagonists and 5-HT3 receptor antagonists [13, 22, 26, 27].
Rolapitant has a distinct pharmacokinetic profile with a half-life of 180 vs. 9–12 h for aprepitant. Thus, a single dose of rolapitant can potentially provide long-lasting protection beyond the acute phase of CINV and obviate repeated administration during periods when patients may have nausea and/or vomiting [28]. Other NK-1 receptor antagonists are available for administration as a single dose for CINV treatment. Fosaprepitant (an intravenous formulation of aprepitant) has demonstrated efficacy as a single dose for CINV treatment in patients receiving HEC [25, 29]. However, rates of injection site reactions as high as 15 % have recently been reported with fosaprepitant [30, 31]. The oral fixed-dose combination of the NK-1 receptor antagonist netupitant and the 5-HT3 receptor antagonist palonosetron (NEPA) has demonstrated efficacy as a single oral dose for treating CINV in patients receiving HEC [22, 27, 32].
Managing drug-drug interactions in cancer patients with complex therapeutic needs has been an important consideration in the development of CINV therapies [28]. Rolapitant differs from existing NK-1 receptor antagonists, as it is neither an inhibitor nor inducer of CYP P450 3A4 (CYP3A4) and, thus, is unlikely to produce clinically important drug-drug interactions [28, 33, 34]. The NK-1 receptor antagonist aprepitant, the prodrug fosaprepitant, and the netupitant combination with palonosetron inhibit or induce CYP3A4 [17, 18]. These drug-drug interactions can necessitate dose adjustments of concomitantly administered drugs to avoid potential adverse events [10].
This study design mimicked clinical practice, as patients could receive any combination of chemotherapeutic agents as long as cisplatin, a highly emetogenic agent, was included. In addition, other therapies (such as CYP3A4-metabolized drugs) were allowed; thus, the results of this study are generalizable to the broader oncology population.
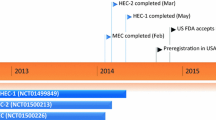
This study demonstrates the safety, tolerability, and efficacy of a rolapitant 180-mg dose administered in combination with a 5-HT3 receptor antagonist and dexamethasone. Rolapitant achieved significantly greater complete response rates than the 5-HT3 receptor antagonist and dexamethasone alone for CINV prevention. Rolapitant was safe and well tolerated at all doses evaluated in the study when administered 2 h prior to chemotherapy in patients receiving HEC. Based on these results, the 180-mg dose of rolapitant was selected for further clinical evaluation in phase 3 clinical trials, results of which are now available [35, 36].
References
Aapro M, Molassiotis A, Dicato M, Peláez I, Rodríguez-Lescure Á, Pastorelli D, Ma L, Burke T, Gu A, Gascon P, Roila F, PEER investigators (2012) The effect of guideline-consistent antiemetic therapy on chemotherapy-induced nausea and vomiting (CINV): the Pan European Emesis Registry (PEER). Ann Oncol 23:1986–1992
Basch E, Prestrud AA, Hesketh PJ, Kris MG, Feyer PC, Somerfield MR, Chesney M, Clark-Snow RA, Flaherty AM, Freundlich B, Morrow G, Rao KV, Schwartz RN, Lyman GH, American Society of Clinical Oncology (2011) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 29:4189–4198
Schwartzberg LS, Grunberg SM, Kris MG (2011) Recent advances and updated guidelines in the management of chemotherapy-induced nausea and vomiting. Clin Adv Hematol Oncol 9(11 Suppl 27):1–14
Grunberg SM, Deuson RR, Mavros P, Geling O, Hansen M, Cruciani G, Daniele B, De Pouvourville G, Rubenstein EB, Daugaard G (2004) Incidence of chemotherapy-induced nausea and emesis after modern antiemetics. Cancer 100:2261–2268
Warr JK (2014) Prognostic factors for chemotherapy induced nausea and vomiting. Eur J Pharmacol 722:192–196
Molassiotis A, Aapro M, Dicato M, Gascon P, Novoa SA, Isambert N, Burke TA, Gu A, Roila F (2014) Evaluation of risk factors predicting chemotherapy-related nausea and vomiting: results from a European prospective observational study. J Pain Symptom Manage 47:839–848
Neymark N, Crott R (2005) Impact of emesis on clinical and economic outcomes of cancer therapy with highly emetogenic chemotherapy regimens: a retrospective analysis of three clinical trials. Support Care Cancer 13:812–818
Van Laar ES, Desai JM, Jatoi A (2015) Professional educational needs for chemotherapy-induced nausea and vomiting (CINV): multinational survey results from 2,388 health care providers. Support Care Cancer 23:151–157
Rojas C, Raje M, Tsukamoto T, Slusher BS (2014) Molecular mechanisms of 5-HT (3) and NK (1) receptor antagonists in prevention of emesis. Eur J Pharmacol 722:26–37
Feyer P, Jordan K (2011) Update and new trends in antiemetic therapy: the continuing need for novel therapies. Ann Oncol 22:30–38
NCCN (2011) NCCN clinical practice guidelines in oncology: antiemesis version 1.2012. Fort Washington, PA
Roila F, Herrstedt J, Aapro M, Gralla RJ, Einhorn LH, Ballatori E, Bria E, Clark-Snow RA, Espersen BT, Feyer P, Grunberg SM, Hesketh PJ, Jordan K, Kris MG, Maranzano E, Molassiotis A, Morrow G, Olver I, Rapoport BL, Rittenberg C, Saito M, Tonato M, Warr D, ESMO/MASCC Guidelines Working Group (2010) Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol 21:232–243
Warr DG, Hesketh PJ, Gralla RJ, Muss HB, Herrstedt J, Eisenberg PD, Raftopoulos H, Grunberg SM, Gabriel M, Rodgers A, Bohidar N, Klinger G, Hustad CM, Horgan KJ, Skobieranda F (2005) Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breast cancer after moderately emetogenic chemotherapy. J Clin Oncol 23:2822–2830
Rojas C, Slusher BS (2012) Pharmacological mechanism of 5-HT3 and tachykinin NK-1 receptor antagonism to prevent chemotherapy-induced nausea and vomiting. Eur J Pharmacol 684:1–7
Morrow GR, Navari RM, Rugo HS (2014) Clinical roundtable monograph: new data in emerging treatment options for chemotherapy-induced nausea and vomiting. Clin Adv Hematol Oncol 12(3 Suppl 9):1–142
Navari RM (2013) Management of chemotherapy-induced nausea and vomiting: focus on newer agents and new uses for older agents. Drugs 73:249–262
Akynzeo Product Information (2014) Eisai Inc., Woodcliff Lakes, New Jersey
Emend Package Insert (2012) Merck & Co. Inc., Whitehouse Station, New Jersey
Poma A, Christensen J, Pentikis H, Arora S, Hedley HL (2013) Rolapitant and its major metabolite do not affect the pharmacokinetics of midazolam, a sensitive cytochrome P450 3A4 substrate. Poster 3441 presented at the MASCC International Symposium, Berlin, Germany, June 27–29
Poma A, Christensen J, Davis J, Kansra V, Martell RE, Hedley ML (2014) Phase 1 positron emission tomography (PET) study of the receptor occupancy of rolapitant, a novel NK-1 receptor antagonist. J Clin Oncol 32(suppl):e20690
Lindley CM, Hirsch JD, O’Neill CV, Transau MC, Gilbert CS, Osterhaus JT (1992) Quality of life consequences of chemotherapy-induced emesis. Qual Life Res 1:331–340
Gralla RJ, Bosnjak SM, Hontsa A, Balser C, Rizzi G, Rossi G, Borroni ME, Jordan K (2014) A phase III study evaluating the safety and efficacy of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting over repeated cycles of chemotherapy. Ann Oncol 25:1333–1339
Hesketh PJ, Grunberg SM, Herrstedt J, de Wit R, Gralla RJ, Carides AD, Taylor A, Evans JK, Horgan KJ (2006) Combined data from two phase III trials of the NK1 antagonist aprepitant plus a 5HT 3 antagonist and a corticosteroid for prevention of chemotherapy-induced nausea and vomiting: effect of gender on treatment response. Support Care Cancer 14:354–360
Hesketh PJ, Grunberg SM, Gralla RJ, Warr DG, Roila F, de Wit R, Chawla SP, Carides AD, Ianus J, Elmer ME, Evans JK, Beck K, Reines S, Horgan KJ, Aprepitant Protocol 052 Study Group (2003) The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin—the Aprepitant Protocol 052 Study Group. J Clin Oncol 21:4112–4119
Saito H, Yoshizawa H, Yoshimori K, Katakami N, Katsumata N, Kawahara M, Eguchi K (2013) Efficacy and safety of single-dose fosaprepitant in the prevention of chemotherapy-induced nausea and vomiting in patients receiving high-dose cisplatin: a multicentre, randomised, double-blind, placebo-controlled phase 3 trial. Ann Oncol 24:1067–1073
Aapro MS, Grunberg SM, Manikhas GM, Olivares G, Suarez T, Tjulandin SA, Bertoli LF, Yunus F, Morrica B, Lordick F, Macciocchi A (2006) A phase III, double-blind, randomized trial of palonosetron compared with ondansetron in preventing chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy. Ann Oncol 17:1441–1449
Aapro M, Rugo H, Rossi G, Rizzi G, Borroni ME, Bondarenko I, Sarosiek T, Oprean C, Cardona-Huerta S, Lorusso V, Karthaus M, Schwartzberg L, Grunberg S (2014) A randomized phase III study evaluating the efficacy and safety of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy. Ann Oncol 25:1328–1333
Aapro MS, Walko CM (2010) Aprepitant: drug-drug interactions in perspective. Ann Oncol 21:2316–2323
Celio L, Ricchini F, De Braud F (2013) Safety, efficacy, and patient acceptability of single-dose fosaprepitant regimen for the prevention of chemotherapy-induced nausea and vomiting. Patient Prefer Adherence 7:391–400
Hegerova LT, Leal AD, Grendahl DC, Seisler DK, Sorgatz KM, Anderson KJ, Hilger CR, Loprinzi CL (2015) An analysis of fosaprepitant-induced venous toxicity in patients receiving highly emetogenic chemotherapy. Support Care Cancer 23:55–59
Lundberg JD, Crawford BS, Phillips G, Berger MJ, Wesolowski R (2014) Incidence of infusion-site reactions associated with peripheral intravenous administration of fosaprepitant. Support Care Cancer 22:1461–1466
Hesketh PJ, Rossi G, Rizzi G, Palmas M, Alyasova A, Bondarenko I, Lisyanskaya A, Gralla RJ (2014) Efficacy and safety of NEPA, an oral combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy: a randomized dose-ranging pivotal study. Ann Oncol 25:1340–1346
Colon-Gonzalez F, Kraft WK (2010) Pharmacokinetic evaluation of fosaprepitant dimeglumine. Expert Opin Drug Metab Toxicol 6:1277–1286
Lanzarotti C, Rossi G (2013) Effect of netupitant, a highly selective NK 1 receptor antagonist, on the pharmacokinetics of midazolam, erythromycin, and dexamethasone. Support Care Cancer 21:2783–2791
Rapoport BL, Chasen M, Poma A, Hedley ML, Martell RE, Navan RM (2014) Phase 3 trial results for rolapitant, a novel NK-1 receptor antagonist, for the prevention of chemotherapy-induced nausea and vomiting (CINV) in patients receiving cisplatin-based, highly emetogenic chemotherapy (MEC). Poster presented at the American Society of Clinical Oncology Annual Meeting, Chicago, Illinois, May 30-June 1
Schnadig ID, Modiano MR, Poma A, Hedley ML, Martell RE, Schwartzberg LS (2014) Rolapitant, a novel NK-1 receptor antagonist, for the prevention of chemotherapy-induced nausea and vomiting (CINV) in subjects receiving moderately emetogenic chemotherapy (MEC). Poster presented at the American Society of Clinical Oncology Annual Meeting, Chicago, Illinois, May 30-June 1
Acknowledgments
Schering-Plough Corporation conducted the study, and TESARO, Inc. is reporting the results. The authors would like to acknowledge the editorial assistance of Richard S. Perry, PharmD, in the preparation of this manuscript, which was supported by TESARO Inc., Waltham, MA, and the help provided by Hajira B. Koeller, PhD, from TESARO Inc. in analyzing the data.
Authors’ contributions
All authors critically reviewed drafts of the manuscript, and all approved submission of the manuscript for publication. DC and LF were involved in the conduct of the study. BR, DC, LF, SA, and AP were involved in interpretation of the study results. SA performed the statistical analysis. YW was involved in the interpretation and writing of the manuscript.
Conflict of interest
Dr. Rapoport had full access to all of the primary data from this study and agrees to allow the journal to review the data, if requested. Dr. Rapoport received funding to conduct this research from Schering-Plough Corporation and currently serves as a consultant/advisor for TESARO, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rapoport, B., Chua, D., Poma, A. et al. Study of rolapitant, a novel, long-acting, NK-1 receptor antagonist, for the prevention of chemotherapy-induced nausea and vomiting (CINV) due to highly emetogenic chemotherapy (HEC). Support Care Cancer 23, 3281–3288 (2015). https://doi.org/10.1007/s00520-015-2738-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2738-1