Summary
The enormous progress made in recent years in the field of information and communication technology and also in sensor and computer technology has affected numerous fields of medicine and is capable of inducing even radical changes in diagnostic and therapeutic processes. This is particularly true for cardiology, where, for example, telemetric monitoring of cardiac and circulatory functions has been in use for many years. Nevertheless, broad application of newer telemedical processes has not yet been achieved to the extent one would expect from the encouraging results of numerous clinical studies in this field and the state of the art of the underlying technology. In the present paper, the Working Group on Rhythmology of the Austrian Cardiological Society aims to provoke a critical discussion of the digital change in cardiology and to make recommendations for the implementation of those telemedical processes that have been shown to exert positive effects on a wide variety of medical and economic parameters. The greatest benefit of telecardiological applications is certainly to be found in the long-term care of patients with chronic cardiovascular diseases. Accordingly, follow-up care of patients with cardiological rhythm implants, management of chronic heart failure and secondary prevention following an acute cardiac event during rehabilitation are currently the most important fields of application. Telemedicine is intended to enable high-quality and cost-efficient care for an increasing number of patients, whose care poses one of the greatest challenges to our healthcare system. Not least of all, telemedicine should make a decisive contribution to improving the quality of life of this segment of the population by favorably influencing mortality, morbidity and hospitalization as well as the patient’s contribution to treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The technical revolution that was initiated by the digitalization of almost all areas of life in recent years is now felt ubiquitously and immediately. Whether it be self-driving cars, the increasing use of artificial intelligence and large amounts of data (big data) to control and analyze everyday processes that are no longer manageable for the individual person or the advance of robot technology in medicine and the production of goods, all of these have kicked off the so-called fourth industrial revolution. This revolution affects the way we live, work and communicate with each other. The merger of digitalization and medicine has opened up completely new possibilities for diagnostics and treatment and is in the process of challenging or replacing many traditional and proven care concepts.
Despite the numerous advantages associated with this development, there are also a number of concerns, e.g. with respect to data security and protection, systems reliability, or with respect to consequences for people, especially on the psychological level. In addition, there are increasing fears that various involved organizations are not or will not be able to adequately keep up with the changes wrought by digitalization. It therefore stands to reason that the opportunities that digitalization is opening up in medicine should be made use of jointly with all other parties involved (patients, other health service providers, medical technology, etc.) in order to create a positive and sustainable future.
Despite the fact that mortality from cardiovascular diseases has been declining in recent decades, at least in the industrialized countries, the diagnosis and treatment still pose a major organizational and financial challenge for national healthcare systems. The number of newly diagnosed cardiovascular diseases is increasing year by year in Europe and also in Austria [1] and these diseases are still the most frequent cause of death. In 2015, an estimated 83.5 million people in the European Union suffered from a cardiovascular disease [2], and roughly the same number in the USA. As a result of the steadily rising life expectancy, the treatment duration for chronically ill patients is steadily growing, thus increasing the amount of care required in both inpatient and outpatient settings.
In 2009, the Austrian Cardiological Society (ÖKG) published a position paper on telemedicine (TM) in cardiology based on the latest scientific evidence, in which some telemedical processes for cardiology were given a positive review and their widespread use was recommended for Austria [3]. The American Heart Association (AHA; [4]) as well as the European Society of Cardiology (ESC; [5]) and the German Cardiac Society (DGK; [6,7,8,9]) have meanwhile dealt with the topic in policy papers. All these societies are agreed that in contrast to the rapidly growing evidence for the advantages of TM in cardiology, broad implementation of TM in regular operations is proceeding at a much slower pace or has yet to materialize. The barriers to the widespread use of TM in cardiology have already been identified [4,5,6,7,8,9] and include standardization, quality assurance, interoperability and financing.
Both the new knowledge gained in and the rapid technical developments in recent years now require a complete revision and update of the abovementioned position paper of the Austrian Cardiological Society from 2009, in order to make pertinent recommendations for the implementation of telemedical procedures in cardiology in Austria.
Definitions
Telemedicine (TM) refers to the provision of health services using information and communication technology (ICT) in cases where the patient and the healthcare practitioner or two healthcare practitioners are in different places when service is to be provided. This requires secure and stable transmission of medical data and information for the prevention, diagnosis, treatment and further care of patients in the form of text, sound, images or in any other form. This is done in constant compliance with data protection regulations.
The WHO defines TM in a much more complex way, highlighting not only the benefits for the patient but also the various advantages for the healthcare system [10]. It emphasizes that TM is still an open dynamically evolving science that constantly picks up new technical developments, thereby reacting to changing demands [11].
The artificial term eHealth, on the other hand, is not yet clearly defined although it is used more and more frequently [12]. Depending on which target group is addressed (physicians, patients, technicians, lawyers, health politicians or health economists, etc.), eHealth is used synonymously with other established terms, such as TM (or other tele‑X terms) or also new terms such as online health, cybermedicine and (Internet) consumer health informatics. Technically speaking eHealth means among other things that telemedicine applications rely on the Internet infrastructure or technology. The pervasiveness of the Internet means that direct patient-computer interaction is also becoming increasingly important as a supplement to the classical physician-patient consultation and is therefore often considered part of the eHealth field, as are networking efforts in the healthcare system (e.g. electronic patient records) or general IT-based infrastructure initiatives (such as the Austrian ELGA).
In addition, the term eHealth refers to the efforts of various actors in the healthcare system (insurance companies, health portals, virtual self-help groups) to make health information and services accessible to lay consumers and patients via the Internet. The same applies to the globally observed trend where patients search the Internet for information about medical topics and thus exert a greater influence on their own healthcare.
The term mHealth, an abbreviation for mobile health, stands for support for TM procedures and healthcare efforts by means of mobile devices, such as smartphones, tablets or personal digital assistants (PDA) [13] as well as by means of lifestyle and health applications that can be operated via sensors. With rising healthcare costs and more self-confident and better-informed patients, mHealth is increasing in importance; however, healthy consumers who use applications for prevention or wellness are also important users of mHealth.
mHealth comprises a number of technical application possibilities. These include the determination and transmission of vital parameters, such as blood glucose levels or body temperature and also communication or motivational applications to remind people to take medication. The use of application software (apps) plays a major role here because the sensors installed in smartphones can be used to record and process a large amount of health-related data [14].
In principle, the older term telematics refers to any technology that links the fields of telecommunications and information technology.
Telemonitoring, also known as remote monitoring (RM), is the continuous monitoring and transmission of data on body functions by means of sensors and telemetry, especially for chronically ill patients or patients at risk. This can be done either locally in a hospital or in the patient’s private setting. Possible monitoring parameters and their combinations are manifold and enable medical care to be tailored to the needs of the individual patient.
Telerehabilitation (TR) means, in analogy to the abovementioned terms that ICT is used in various treatment processes in rehabilitation (R). Formally, TR includes the use of telecommunications and RM, but more recent developments also use robotics, computer games and many other forms of virtual reality to enable the provision of R services at locations remote from the institution [15, 16]. Very different subareas of R are supported, such as assessment, definition of the R target, monitoring, training and physiotherapy, prevention, intervention, supervision, evaluation, training, and counseling. Service can be provided when the patient is either at home, in a general community center, in a care facility offering varying degrees of care, or in a school. TR is a form of medical treatment that can theoretically be administered throughout the rest of a patient’s life span or at least during the entire course of a particular treatment [16]. As the first telemedical form of treatment in Austria, TR was explicitly included in Austria’s General Social Security Act as a possible treatment option.
Telemedical aftercare and remote monitoring of cardiac implantable electronic devices
The follow-up care of patients with cardiac implantable electronic devices (CIED), such as pacemakers (PM), implantable defibrillators cardioverters (ICD), devices for cardiac resynchronization therapy (CRT) or implantable loop recorders (ILR) currently takes place almost exclusively intramurally in Austria and dedicated resources are increasingly being exhausted. In the case of purely antibradycardia CIED, it is recommended that after implantation the system be checked at least every 6 months or annually for the first 3 years, thereafter every 6 months and at even shorter intervals, if required, or when the battery is nearing the end of its life. The follow-up intervals for other implantable systems are usually 3 months from implantation or even less if necessary. Since the life-prolonging effect of CIED treatment is obvious, this also means a constant increase in the number of affected patients and, thus, the amount of follow-up care required [17].
Another problem is that in the interval between two follow-up appointments device or electrode malfunctions or a deterioration in the patient’s condition can occur, which are only detected at the next check-up unless acute inpatient treatment is required. On the other hand, completely correct device function is diagnosed during the vast majority of routine checks in the outpatient department, where the patient is in good clinical condition. Consequently, the implant does not need to be reprogrammed and the therapy does not need to be changed.
The use of TM in the ongoing care of patients with CIED has already been realized in two different processes. Telemedical follow-up is known as remote interrogation (RI) and enables telemetric monitoring of the implant outside a medical aftercare facility at specific scheduled times with transmission of data. The data transfer can be initialized automatically or by patients themselves. The second procedure is RM of the CIED, which includes a continuous (mostly daily) query and forwarding of large amounts of patient-related and device-related information, almost independent of the patient’s assistance. In both cases, the data are transmitted to a server and processed accordingly. The supervising healthcare practitioner can subsequently view the results via the Internet.
Aftercare via RI or RM includes not only the transmission of data on system integrity (e.g. battery status, impedances and stimulation thresholds) but also clinical data (heart rate, arrhythmia burden, patient activity, therapies, etc.) and the automatic transmission of predefined alerts. In the case of unremarkable information the system merely records but in the case of predefined deviations from normal values notification is additionally sent to the aftercare personnel. In the latter case, the closely meshed collection of follow-up data must of course be analyzed promptly and will have prespecified therapeutic consequences; however, only a few studies have really examined the effect of daily or weekly transmissions but instead often only those of semiannual transmissions, i.e. RI. This can also explain the difference in study results. In any case, this form of aftercare also leads to a significant reduction in effort and expense, because the conventional aftercare intervals can be extended, and thus also to a reduction in the auxiliary costs for each individual outpatient check-up, such as those for necessary patient transport [18].
The RI and RM of patients with CIED requires an additional extracorporeal transmission device that communicates telemetrically with the implant. This device retrieves the data from the CIED and transmits them via telecommunication.
Pacemakers
For more than 60 years permanent PMs have been improving and/or prolonging the life of patients with severe bradycardia. In Austria, about 60,000 patients have a PM, with about 8500 new devices being implanted every year. Accordingly, the number of necessary outpatient implant follow-ups is also increasing.
Nearly all devices implanted today are suitable for RI or RM; however, in contrast to CRT, the ESC has not yet issued a class I recommendation for RM or RI of PMs. In view of the constantly growing amount of data regarding this technology, such a recommendation is to be expected in an update of the respective guidelines planned for 2021 [19].
Data transmitted from a PM by RM or RI include battery status, lead integrity and function, data on signal amplitudes and stimulation thresholds, and patient-related or disease-related information.
The fact that RM is a safe alternative to outpatient follow-up care was already established in 2012 by the COMPAS study. In that study 538 PM patients were randomized to undergo RM or standard outpatient aftercare. During a mean follow-up of 18 months it was demonstrated that RM is safe and that it can significantly reduce the number of outpatient follow-ups. Even in that study it was noteworthy that RM was able to document more arrhythmias, and consequently PM programming as well as the corresponding medication was adapted more frequently. Overall, RM significantly reduced the number of unscheduled outpatient follow-ups, hospitalizations and strokes [20].
The PREFER study that was previously conducted in patients with single or dual chamber PM [21], produced similar findings. Even after 3 months RM detected clinically relevant events, especially arrhythmias, significantly more frequently than in the control group. In addition, atrial high-rate episodes (AHRE) associated with an increased rate of thromboembolic complications were detected in 30–50% of patients with CIED, with atrial fibrillation (AF) being the most frequent form of arrhythmia.
At present it is not yet clear at which arrhythmia burden anticoagulation should be initiated, given the correct indications. Even arrhythmia duration of 6 min could increase the risk of stroke; AF lasting 3.8 h is apparently associated with a ninefold increase in the risk of stroke in CRT patients [22]. With RM, arrhythmias can be diagnosed much earlier and appropriate therapy can be initiated, such as the decision to undergo antiarrhythmic therapy or ablation. Whether early anticoagulation can actually reduce thromboembolic events has been reported differently by different studies.
Most studies on the use of TM in CIED follow-up have involved mixed cohorts of patients with PM, ICD, CRT and CRT‑D. Telemedical monitoring of the devices and lead integrity was seen to be technically feasible and safe. In the TRUST study, RM detected CIED system malfunctions after 1 day on average, compared to 5 days in the control group, and a significant 45% reduction in outpatient follow-ups was achieved [18]. The less frequent outpatient follow-ups did not result in an increase in mortality or stroke rate in this group. The reduction in outpatient check-ups, which are usually conducted in a special outpatient clinic, not only increase the quality of life for patients but also helps reduce costs for the healthcare system.
The goal of TM is to customize the currently recommended aftercare intervals. For example, 6 months might already be too long for some patients, while other patients might not need to be checked that often. In order to adapt the follow-up intervals to the particular patient’s current situation using RI or RM, it must be ensured that all serious events are safely recorded, which is indeed guaranteed according to the current studies. Thanks to TM, outpatient follow-up intervals for PM patients can thus be safely reduced.
The importance of detecting asymptomatic atrial arrhythmias—especially AF—with a view to preventing stroke in patients with chronic heart failure (HF) will be discussed again in the section “Cardiac resynchronization therapy”.
The only leadless pacemaker (Micra™, Medtronic Inc., Minneapolis, MN, USA) currently on the market also permits telemedical follow-up. Since this pacemaker is a single-chamber device implanted in the right ventricle, it is just as unable to detect atrial arrhythmias as conventional single-chamber pacemakers with a lead implanted in the right ventricle (VVI or VVIR devices); however, a leadless device from the same family (Micra™ VDD) has already been intensely tested and will be available in the coming months. Recommendations for the follow-up of patients with an implanted PM utilizing telemedicine ar provided in Table 1.
Cardiac resynchronization therapy
Cardiac resynchronization therapy (CRT) is one of the established therapies for chronic HF and leads to a significant reduction in morbidity and mortality [23]. In accordance with current guidelines, the devices are monitored on an outpatient basis at intervals of 3–6 months; however, all currently available CRT systems are also suitable for telemedical follow-up. This feature is not yet sufficiently used even though it was designated a class I indication by the Heart Rhythm Society (HRS) in its latest consensus statement [24]. A recent study showed that only 47% of patients with a CRT implant receive telemedical aftercare, and this was only 8% after 1 year [25].
Telemedical monitoring by RM offers several advantages. Not only can the function of devices and leads be checked, but also the patient’s clinical status can be monitored using specific algorithms and the possible occurrence of rhythm disturbances can be monitored. This not only leads to a reduction in costs due to the elimination of outpatient check-ups but if applied consistently it can also reduce hospital stays and mortality [26]. In this connection the EFFECT study showed a significant decrease in the hospitalization rate (0.27 per year in the control group vs. 0.16 per year in the RM group; risk reduction 0.59; p = 0.0004) and in costs [27].
The results of the TRUST study with respect to the reduction in unnecessary outpatient CIED check-ups were also impressively confirmed for HF patients, namely by the MORE Care study, where a 38% reduction in such check-ups and a significant decrease in hospitalizations were observed in the RM group [28]. These effects were also seen in patients with advanced HF (NYHA class III/IV). At the same time, RM was able to detect device-associated problems, such as lead failure or premature battery depletion at an earlier stage.
Currently, ICD and CRT patients are followed up at 6‑month intervals in special outpatient departments but by using RI or RM, outpatient follow-up intervals were able to be adapted to the individual patient’s needs or reduced.
HF is often associated with atrial fibrillation, and both influence each other negatively. In patients with a CRT system, newly occurring atrial fibrillation that without RM goes undetected can lead to a clinical worsening of HF, an increase in the hospitalization rate and the number of unnecessary ICD shocks, a decrease in biventricular stimulation and an increase in stroke rate [22, 29]. These negative effects can potentially be minimized by early detection of atrial fibrillation with RM. Furthermore, RM can also identify the need for cardioversion or can show that the biventricular stimulation level is reduced because of the arrhythmia. The TRUST study showed that the time from arrhythmia to diagnosis and treatment dropped from 36 days to 1 day for ventricular fibrillation and from 28 days to 1 day for ventricular tachycardia [18]. In the CONNECT study, the reaction time also declined from 22 days to 4.6 days (p ≤ 0.01) [30]. With prompt evaluation of whether a therapy was effective and appropriate or inappropriate (e.g. T‑wave oversensing, magnetic interference, no ventricular arrhythmias), the CIED can be reprogrammed in time, if necessary. With RM the number of inappropriate and appropriate shocks can be reduced and the battery life of CRT‑D devices can be extended compared to conventional follow-up. In the ECOST study, not only was the number of inappropriate shocks reduced by 52% but also the resulting hospitalization rate due to inappropriate shocks was significantly reduced by 72% [31].
HF is a major, steadily increasing health problem and a major reason for hospitalization. The reason underlying the high mortality rate is HF progression. Therefore, early detection of the factors contributing to this progression is desirable. Thus, RM used to monitor HF can be particularly helpful in the management of these patients. To assess the compensation status in HF patients with CIED, various data from device-specific parameters can be obtained telemetrically.
In CRT systems, data on how well the left ventricular lead (stimulation level, stimulation threshold) is functioning also provide important information on the effectiveness of electrical therapy for HF. The detection of atrial and ventricular tachyarrhythmias, the percentage of biventricular stimulation and patient activity can influence therapy. Nearly 100% biventricular stimulation is essential for a patient’s response to CRT. The INTIME study showed a reduction in the worsening of HF symptoms from 27.2% in the control group to 18.9% in the RM group (p = 0.013) [32].
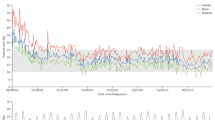
Furthermore, the heart rate itself, as well as heart rate variability, respiratory rate or thoracic impedance can be used as surrogate parameters for HF status. Thoracic impedance correlates closely with pulmonary arterial occlusion pressure and can thus point to impending cardiac decompensation; however, the high rate of false positive alarms caused by such algorithms appears to be problematic in the clinical routine and, moreover, randomized studies showed no survival benefit. The goal is therefore to combine several sensors and measurement parameters in order to overcome the limitations of a single sensor. A new improved algorithm that also includes a low activity level, a low biventricular stimulation rate and a high nocturnal heart rate, would seem to increase the diagnostic value significantly [33]. Newer algorithms, such as HeartLogicTM, attempt to achieve better detection of HF events by combining several physiological sensors (S1 and S3, respiratory rate, respiratory volume, patient activity, thoracic impedance). The MultiSENSE study showed a sensitivity of 70% [34], and a large randomized study is currently underway on this topic.
Data on the influence of RI or RM of CRT aggregates on mortality differ. While MORE-CRT [35] and REFORM [36] did not show a significant survival benefit, other studies have shown a clear reduction in mortality [18, 21, 28, 32]. The ALTITUDE study showed a 50% reduction in mortality after 1 and 5 years, with the lowest mortality risk seen when clinical factors such as weight and blood pressure were also analyzed [37]. In a prospective registry, the 1‑year mortality in the telemedically monitored group was significantly lower than in the control group (2.1% vs. 11.5%) and this effect was maintained at 3 years (4.9% vs. 22.3%) [38]. Prompt initiation of RM (median 4 weeks after implantation) is evidently associated with lower mortality than is starting at a later time [39].
In a recent meta-analysis of seven randomized studies (4932 ICD/CRT‑D patients with a follow-up of 12–24 months) Parthiban et al. showed that there was no difference in all-cause mortality between patients undergoing conventional or telemedical follow-up (odds ratio, OR = 0.83; 0.58–1.17). A comparison of the TM systems RI vs. RM, however, showed that RM systems, i.e. with daily transmission, led to a significant reduction in all-cause mortality (OR = 0.65) ([40]. Concerning to the follow-up of patients with implanted CRT devices respective recommendations are summarized in Table 2.
Implantable cardioverters defibrillators
The telemedical aftercare of implantable cardioverter defibrillators (ICD) differs only slightly from that of PM or CRT devices. With the ICD, in addition to the battery status and the stimulation components, classical lead function parameters (stimulation threshold, stimulation impedance, sensing) are also automatically monitored and the data transmitted. In the case of ICD systems with an atrial lead, not only ventricular but also atrial arrhythmias can be detected and stored, depending on the programming. The evaluation of detailed frequency histograms in follow-up care provides reliable information on the long-term course of the disease. In the case of ICDs, the following device-specific measurements are also evaluated:
-
shock impedance (integrity of the ICD shock coil)
-
intracardiac electrograms (IEGM) of ventricular arrhythmias treated with shock or antitachycardia pacing (ATP)
-
IEGM of untreated ventricular tachycardias stored in a monitor-only zone.
Telemedical follow-up is also possible for subcutaneously implanted ICD (S-ICD), although fewer parameters are available here. Technical or rhythmological abnormalities that prompt alerts in the case of S‑ICD are:
-
ERI reached (low battery voltage)
-
shock impedance outside the normal values
-
recording of an ECG recorded during a shock
-
atrial fibrillation episodes lasting more than 6 min in the AF monitor
If a telemedical report of delivered shocks or ATPs is received by the center, a manual check by the attending healthcare practitioner is recommended independent of the device, which can at least be carried out as a telephone visit with the patient. Using the IEGMs or ECGs, a decision must be made on whether therapy is adequate or inadequate and whether reprogramming or other therapy options (medication or ablation) need to be initiated.
For all ICD devices, technical abnormalities and thus the increased risk of inadequate shocks mean the patient urgently requires a check-up in the aftercare center, while for some arrhythmia-related alerts a therapy recommendation can also be made by telephone (e.g. increasing the dose of antiarrhythmic drugs).
For ICD patients under close TM care, personal outpatient checks can be performed at longer intervals. The latest HRS expert consensus recommends an annual check-up in this connection [24]. In light of the recent randomized RM-ALONE study, pure RM should even be strived for in telemedical centers providing intensive care for patients with S‑ICD or with ICDs without CRT function for 2 years after implantation [41]. In this case, patients will only be asked to come in to the center for a personal check-up if there are technical or arrhythmic abnormalities.
Loop recorder
Implantable loop recorders (ILR) are indicated for diagnostic purposes in various clinical situations [42]:
-
unexplained and infrequent syncope
-
palpitations
-
cryptogenic stroke
-
management of ventricular arrhythmias in arrhythmogenic cardiomyopathies or channelopathies
-
atrial fibrillation burden before and after ablation
Even after myocardial infarction, a high incidence of bradycardia and tachycardia was detected by means of ILR [43]. The first generation of ILR was used to work up primarily unexplained syncope [44]. Later, it was also used to detect atrial fibrillation in single-channel ECG analysis [45] as well as for telemedical follow-up. The latest generation of ILRs, which have meanwhile been miniaturized, offers automated RM [46] and improved analysis of atrial fibrillation [47]. The insertion of an ILR is therefore currently a class I indication for primarily unexplained syncope [48], as well as a class IIa indication for cryptogenic stroke [49].
Even in 2015 the HRS classified the telemedical follow-up of an ILR as an expert consensus class I indication (level C) [24]. A recent study supported this expert opinion [50]. In 154 patients (mean age 63 years) with ILRs for various indications followed during a 12-month period, a diagnosis was made in 99 patients (64%) and therapy (oral anticoagulation, pacemaker/ICD implantation, electrophysiological examination/ablation, antiarrhythmic therapy) prescribed in 60 patients (39%). In 26 of these 60 patients, this therapy decision was made with TM and without symptoms 2.4 days after detection in contrast to 3.8 months if the patient had appeared for the scheduled semi-annual check-up.
In contrast to other CIEDs, there are currently no randomized studies involving telemedical aftercare. For this reason, the data from the currently ongoing BIO/GUARD-MI study will be interesting. In this study, patients after myocardial infarction (acute or chronic) with an ejection fraction >35%, a CHADS-VASc score ≥4 (≥5 in women) and with no known atrial or ventricular arrhythmias will be enrolled and randomized for daily automatic telemedical follow-up or conventional check-up [51].
Thus, automatic daily telemedical follow-up is also beneficial and clinically useful for ILRs regardless of the indication, even if expert consensus currently designates this only as a class I indication.
From the available evidence, the following assessment can therefore be made for daily practice with all CIEDs:
RM and RI care is appropriate in the treatment and care of patients with CIED and does not exceed what is necessary and justified.
Heart failure
Chronic HF is an epidemiologically significant disease with a prevalence of 1–2% in the general population. Due to epidemiological changes resulting from the aging population and improved options in acute cardiological care, the prevalence of HF is expected to increase exponentially over the next decades [52]. At the same time, the complexity of the disease will increase, not least of all because of the frequency of concomitant diseases, especially in older patients. Despite important progress in treatment, morbidity and mortality remain very high. The high event rate and especially repeated hospital admissions for worsening HF are associated with enormously high costs and a clear reduction in quality of life.
HF therapy calls for interdisciplinary, integrated treatment throughout the course of the disease in the sense of a multidisciplinary management program and not episodic care. The transitions at the interfaces from intramural to extramural and to the healthcare practitioner in the extramural sector should be as seamless as possible. Care programs conducted by multidisciplinary teams can prevent acute events and thus considerably improve the reality of care. Multidisciplinary care not only includes optimal therapy for the disease, but also disease-specific training of patients to improve adherence and self-monitoring.
In the meantime, there is sufficient evidence for the feasibility and effectiveness of TM in the care of HF patients. Of the main fields of digital cardiology defined by the ESC in 2016 [53] at least three are directly applicable to HF:
-
1.
telemedical care concepts (including RM)
-
2.
mobile health applications (mHealth) including applications (apps)
-
3.
personalized health applications (pHealth) including portable or implanted sensors
These applications can support exchanges between the various healthcare practitioners (“doc2doc”) as well as direct communication between the patient and the treating physicians (“doc2patient”). The former enables an exchange between remote medical professionals, while the latter enables a direct connection between the healthcare practitioner and the patient in the home environment by means of information and communication media.
1. Telemedical care concepts (including RM)
The telemedically supported care of patients with chronic HF is embedded in a holistic outpatient care concept using RM, which comprises various pillars:
Sensor-based measurements of physiologic parameters are transferred from the patient’s home and analyzed by medical personnel. If predefined limits are not adhered to, escalating counter-steps can be initiated. Likewise, information on the patient’s current state of health and therapy compliance can be obtained. Training by the nursing staff takes place at the patient’s home. The attending physician can use the telemetrically obtained data to facilitate and speed up optimization of therapy in order to achieve the guideline-based HF treatment.
Various prerequisites are given for the technical implementation of RM:
The noninvasive (e.g. scales, blood pressure machine) or invasive (e.g. pacemaker and/or ICD systems, CardioMems™, Abbott Inc., Plymouth, MN, USA) measuring devices must be available in the patient’s home. A device for data transmission (e.g. a specially configured smartphone) is also needed. The IT infrastructure is located at the medical service provider. Encrypted data transmission between the healthcare practitioner and the patient and vice versa must be guaranteed to comply with data protection regulations (see Table 3).
Integration of TM in the care of the HF patient is possible in different settings:
RM via web-based data access by the supervising healthcare practitioner
The patient sends the digital datasets to a web-based electronic patient file. The healthcare practitioner analyzes the data and, depending on the relevance and urgency of the data not conforming to the predefined limits, reacts by contacting the patient directly and initiating any necessary therapy steps (e.g. increasing the dose of diuretic) or, if necessary, referral to a hospital. HerzMobil Tirol and HerzMobil Steiermark [54,55,56,57], which have already become part of the standard care system, are prototypical for this care structure. It is explicitly pointed out that the RM systems are not designed or approved for emergency care.
Telemedically supported care by a TM center (TMC) staffed by specialist physicians
The patient’s vital signs data are transmitted to a TMC that is manned by specialists around the clock every day of the week. The electronic patient file contains all important medical reports concerning the patient. If the patient’s condition worsens the TMC undertakes direct interventions, which are usually coordinated with the attending physician. During the night or on weekends, the medical staff of the TMC can react directly without contacting the attending physician. The effectiveness of this care system was demonstrated in the randomized, multicenter TIM-HF2 study. With 1538 HF patients enrolled, the primary endpoint (days lost due to unplanned cardiovascular hospitalization and death from any cause) in the 1‑year follow-up showed a significant advantage for patients in the RM group over the conventionally managed control group (HR = 0.80, p = 0.046). Similarly, the overall mortality rate of 7.9 per 100 person-years was significantly lower in the RM group than in the control group (11.3 per 100 person-years, hazard ratio, HR = 0.70; p = 0.028). These findings were achieved regardless of whether the patient lived in a structurally weak rural area or in a metropolitan region. RM is thus also suitable for compensating regional differences in care between town and country and for realizing an overall improvement in the quality of care [58].
RM through a medical call center
Data collected from the patients are transferred to a call center, where patient-specific threshold values are stored in the patient’s electronic file. In the event that threshold values are exceeded, the call center forwards the information to the treating healthcare practitioner, who decides on any necessary diagnostic or therapeutic consequences.
The effect of various RM interventions on individual clinical endpoints has been investigated repeatedly, but the results were very inconsistent. A meta-analysis from a Cochrane review concluded that RM reduced all-cause mortality by 20% and HF hospitalizations by 30% [59]. The Heart Failure Association of the ESC (HFA) recommends that home telemonitoring be considered to reduce hospital admissions for cardiovascular and HF reasons as well as cardiovascular deaths: this corresponds to a class IIb recommendation. The care concept should be used synergistically with existing structures and should not function entirely impersonally. In addition, a good cost-benefit ratio is also recommended [60].
TM must be used sensibly, which is why goals, responsibilities, time and action structures must be explicitly defined in each individual area.
2. Mobile health applications (mHealth) including applications (apps)
An example of mHealth in HF management is the website www.heartfailurematters.org of the HFA, which is available free of charge in several languages. The e‑VitaHF study investigated the effect of using this website versus a dedicated interactive platform (e-Vita) for disease management including RM and knowledge transfer versus conventional therapy in 450 patients after 1:1:1 randomization. After 3 months the intensely managed groups showed a greater ability to help themselves, as measured by the European heart failure self-care behavior scale (EHFScB), but this advantage was no longer detectable after 12 months [61].
3. Personalized health applications (pHealth)
The implantation of a wireless pressure sensor (CardioMemsTM) in the pulmonary artery allows continuous hemodynamic monitoring of pulmonary artery pressure. The prospective, randomized CHAMPION study conducted in in 550 NYHA III patients investigated the effect of using pulmonary artery pressure to steer therapy and demonstrated a significant reduction in HF-related hospitalizations [62]. The option to use RM for this new form of hemodynamic monitoring of HF patients was included in the ESC HF guidelines as a class IIb recommendation for recently hospitalized patients to reduce further hospitalizations and is one of the first pHealth applications for HF [23].
4. Future developments
In future, data collected by RM can be used not only for direct intervention in the event that clinical parameters are exceeded but also for the creation of therapeutic aids for healthcare practitioners by means of artificial intelligence (AI). Two models are given as examples:
-
1.
Create prediction models for early detection of disease progression. This is intended to provide healthcare practitioners with a means of detecting unfavorable developments in individual patients at an early stage and in order to take countermeasures in good time.
-
2.
Draw up an algorithm that assesses how well the current therapy adheres to guidelines and also presents it, for example, in the form of a traffic light system. This is intended to alert healthcare practitioners to therapy options that have not yet been exhausted and thus ensure continuous therapy optimization.
At HerzMobil Tirol these fields of application are currently the subject of intense research and their use in everyday clinical practice is already foreseeable [63]
Telerehabilitation
Although rehabilitation following an acute cardiac event, cardiac surgery or other intervention in the cardiovascular system (CR) has been shown to have a positive effect on morbidity and mortality [65, 66], the implementation of rehabilitation remains remarkably low worldwide. In Europe, fewer than 50% of all patients participate in cardiac rehabilitation (CR) following a cardiac event (ACS including myocardial infarction, aortocoronary bypass grafting, percutaneous coronary intervention, and others), and CR for primary prevention is practically nonexistent [67]. In Austria, the percentage of patients undergoing CR after myocardial infarction was as modest as 40% in 2013/2014 and clearly less than 10% after hospitalization for acute HF [68], even though the prevalence of HF is as high in Austria as elsewhere in Europe. Reasons for this, as given in the international literature, include too low referral rates, long distance to the next appropriate CR facility, and various other patient-related, occupational or social problems [69].
Furthermore, it is general knowledge that the personal improvements in lifestyle, risk factors, adherence to therapy, and regular physical fitness achieved during CR are not sustained after CR, but largely fade away within a year after CR completion [70]. Future additions or alternatives to existing CR should therefore not only help improve access to CR, but also be able to maintain or even expand the primary improvements in the relevant parameters mentioned above over a longer period of time [71].
Over the last decade, technologies for telediagnosis and teleintervention have experienced exponential growth, paving the way for the development of CTR. The services offered under this title are extremely diverse and include evaluation, assessment, monitoring, prevention, intervention, supervision, training, counseling and coaching. All these things have no formal structure and data exchange takes place in a variety of ways, such as by telephone, text message, e‑mail, or by means of multimodal systems such as videoconferencing (VC) or web-based platforms [72]. It should be noted, however, that according to the provisions of the Austrian Health Telematics Act 2012, data transmission via telephone, SMS and e‑mail is only secure when it can be guaranteed that sender and recipient are clearly identified and that data transmission goes through protected channels. For e‑mails, encrypted data transmission and a qualified signature are required.
The study groups largely investigated to date by means of CTR included patients with coronary heart disease (CHD) or HF. Several randomized controlled trials have demonstrated an additional positive effect of cardiac CTR when added to conventional CR [73, 74]. Various communication technologies are used: telecoaching to increase adherence to therapy when necessary, and fitness plans and suggestions for more physical activity are offered that are tailored to the patient and patient needs [71]. Frederix et al. impressively demonstrated that a 1-year CTR program conducted in addition to the standard CR reduces the number of follow-up hospital admissions and is cost-effective [75]; however, completely replacing conventional phase II CR with CTR does not appear to be advantageous at this time.
A particularly interesting field of application is TR in HF. Since the current ESC guidelines for the treatment of this disease include regular aerobic training to improve functional capacity and symptoms, as well as long-term care of the patient in a multidisciplinary disease management program (DMP) as a class I A therapy recommendation [23], it is obvious that CR in HF should also be included in a DMP in order to optimize neurohumoral therapy under controlled conditions, establish cardiovascular training of the patient and provide a customized long-term exercise and training program. Since this may require a longer period of time, CTR can be seen to be cost-effective and at least equally effective, if not superior.
In a recent study by Hwang et al., patients with stable HF were treated with VC over 12 weeks as part of a real-time telemonitored training program supplemented by appropriate VC training, and the results were compared with those for conventional ambulatory CR. Here, too, it was impressively demonstrated that with respect to clinical endpoints the same improvements can be achieved with CTR, but at a clearly lower cost. In addition, CTR was more attractive for patients and was associated with fewer adverse side-effects [76]. This study also essentially confirmed the results of similar earlier studies, although it should be noted that the aim of those projects was primarily to provide integrated medical care for HF patients [77, 78] and that RM, as an essential part of CTR, revealed the advantages of TM-supported treatment as a secondary aspect. In a study published in 2018, it was also shown that weekly televisits and daily RM of vital parameters provided alone after hospitalization are well-suited to reduce unplanned emergency admissions for decompensated HF and the length of hospital stays, as well as to improve patients’ quality of life. Furthermore, a trend to reduced costs per case was observed [79]. Within the framework of HerzMobil Tirol, the concept of cardiac telerehabilitation for patients with cardiac insufficiency is currently being evaluated in the form of a pilot project in cooperation with the Austrian Pension Insurance Institution and readied for routine use.
Another, relatively new CTR concept is provided by the so-called expanded rehabilitation/aftercare programs (ERAP), which can be seen as a transition from the short-term offers in the framework of traditional CR to support in the daily life of the patients [80]. The advantage of such programs is that if rehabilitation success is limited but rehabilitation potential is still given, instead of extending conventional CR with all its ensuing costs, treatment can be continued in the patient’s home with fitness therapy, education and counseling. A further positive aspect of this approach is that R targets already achieved can be further consolidated or maintained in the long term. A Swedish study also showed that such a patient-centered aftercare intervention over a total of 6 months also improves the rate of return to work [81].
Although for the time being such programs are offered only sporadically throughout Europe, persons who previously participated in rehabilitation and in particular who are now back at work could benefit from telemedical support within the framework of an ERAP, in that time-consuming travel to and from rehabilitation is no longer necessary and the patient no longer has to adhere to the office and therapy hours of the healthcare practitioner, all of which hinder the pursuit of a profession alongside CR. This concept is thus a promising addition to phase III CR, has already proven to be effective and cost-efficient on several occasions and increases the degree to which patients accept and use therapy as well as their therapy adherence ([73]; Recommendations based on the above mentioned findings are given in Table 4.
Legal aspects of cardiological telemedicine
The breathtaking progress of new technologies in electronic communication, including digitalization and AI, has long since taken a firm grip on medicine. Not surprisingly, this also gives rise to legal questions, some of which will be briefly discussed here.
Based on the principle of the immediacy of the practice of medicine contained in the Austrian Physicians Act, it has been argued for decades that this completely rules out distance or remote treatment for clinical disciplines. In actual fact, however, the Austrian Physicians Act does not contain any provision from which a generally valid face to face requirement can be derived. Rather, limits may instead result from the fact that the physician must comply with the state of the art of medicine to safeguard the well-being of the patient. If telemedicine safeguards the patient’s well-being in the same manner, no legal objection can be raised against its use. Contrarily, the situation would be different if telemedicine entailed greater risks for the patient, the causes of which could be manifold (e.g. system failure, transmission errors, the patient’s care is not guaranteed in the event of a sudden incident because the responsible specialist is not available, a full battery of diagnostics requires direct contact with the treating physician). It should also be pointed out how important it is for therapists to provide full information to patients, as many cases may have different advantages and disadvantages that play a decisive role in the patient’s decision to grant or withhold consent.
If patients are cared for by telemedical means in such a way that they are to treat themselves (e.g. regularly collect important data and subsequently transmit these electronically, e.g. to the attending physician or the clinic providing treatment), then the information provided to the patient by a therapist is also of particular importance in this respect. It is necessary to train the patient beforehand and to ensure that the patient, alone or with the support of nonmedical personnel, is able to follow instructions correctly and at the right time, as well as to transmit the data without technical problems.
It should also be pointed out that it is possible to optimize treatment by obtaining a second opinion (teleconsultation, remote diagnosis). Also to be mentioned are the opportunities for using telemedicine for cooperation between physicians and nursing staff, especially in extramural care.
In general, it goes almost without saying that in addition to the laws governing the medical profession, it is necessary to comply with all legal requirements in the field of data security (see in Austria the Health Telematics Act, GTelG 2012) as well as the Data Protection Act (including GDPR) and the Medicinal Products Act, for example also when using health-related apps.
Revolutionary developments such as the use of artificial intelligence mentioned above will in future give rise to the question to what extent physicians, without incurring any legal risks, can decide not to follow a recommendation that was generated by a computer from millions of data, but instead to act according to their personal professional experience. In any case, legal uncertainty should be avoided.
Technical framework for telemedical CIED aftercare in Austria
The telemedical care of patients with implanted cardiac devices requires unidirectional, regular and fault-tolerant data communication from the implanted device to the treating healthcare practitioner. Of central and critical importance is the interoperability between the CIEDs of different manufacturers and the IT systems of electronic medical records in the outpatient or inpatient care model.
International and national standardization initiatives and standards define framework conditions for interoperability on an organizational, legal, semantic and technical level [6, 82]. The HRS also recommends fully integrated electronic data transfer from the CIED manufacturer to the treating healthcare practitioner and the patients, because it can be expected to bring advantages for all parties involved [83, 84].
The basic principles, definitions and essential concepts of interoperability are described at the European level in the document “European Interoperability Framework—Implementation Strategy” [85]. Interoperability is defined as the ability of organizations to work together to achieve mutually beneficial goals by exchanging information and knowledge about business processes and data sharing through IT systems. In this way, principles and recommendations are established that serve to implement interoperability. Concrete specifications are available at the European level that are already being implemented for the cross-border exchange of patient summaries and e‑medication [86, 87].
Of the 12 principles of European interoperability listed, openness, transparency, data portability, user centricity, security, data protection and administrative simplification are of particular importance in the field of telemedicine [85]. The recommendations state that national frameworks and strategies must be aligned with the European recommendations and that extensions and special features can be taken into account in the national context, as needed. In addition, they require that data portability be ensured and that data can be transferred easily between systems and applications without unjustified restrictions, taking legal requirements into account.
At the national level in Austria, basic requirements for the IT architecture for telemonitoring of implanted cardiac devices are defined in the “Framework Directive for the IT Infrastructure for the Use of Telemonitoring” of the Ministry of Health [88]. This framework directive also explicitly describes implant aftercare. In connection with this framework, Fig. 3 shows a schematic diagram of IT architecture for telemonitoring of implanted cardiac devices. The data transfer is performed in a standardized way for measured data from telemonitoring as well as for data resulting from implantation of the devices (e.g. operation report, pacemaker ID) via non-directional (e.g. ELGA) or directional communication channels (e.g. DAME, MedicalNet) to the treating physicians and other healthcare practitioners.
IT architecture adapted for telemonitoring of implanted cardiac devices. Data transmission from the implant to the patient device (interface A) and further to the manufacturer’s IT infrastructure (interface B) is the responsibility of the medical device manufacturer. From the manufacturer’s IT infrastructure, the implant data are transferred via the standardized interface 3 to the technology platform (TP). From TP on to the healthcare professional identical existing interfaces (4, 5) for delivery and retrievement of medical reports to and from ELGA are used
The legally compulsory entries in the implant registry could also be made with automation technology immediately after implantation. This would reduce the effort required for reporting to the registry and clearly increase the data quality of the implant registry through daily updates with complete information.
In the healthcare sector, interoperability is being developed internationally by the non-profit organization Health Level Seven International (HL7) with certified ANSI standards and readied for national implementation. HL7 was founded in 1987 with the aim of developing basic structures (frameworks) and standards for the exchange, integration, retrieval and forwarding of electronic health data to enable the provision of healthcare in clinical practice and the evaluation of health systems. In Austria, HL7 has been represented since 2007 by the non-profit association HL7 Austria, whose purpose is to improve electronic data communication and interoperability in the healthcare sector by means of HL7’s international standards. HL7 Austria adapts the HL7 standards to the conditions of the Austrian healthcare system and defines national standards such as CDA implementation guidelines.
Interface A from the implanted device to the patient device and interface B from the patient device to the IT infrastructure of the device manufacturer in Fig. 3 are the responsibility of the manufacturer of these medical devices. Due to backward compatibility and the great effort required to develop new medical devices, it is neither necessary nor does it make sense technically to provide standardized communication protocols for this purpose. This will most likely not change in the medium term either; however, standardized IT interfaces are already strongly recommended for interface 3. The international standard ISO/IEEE 11073-10103, which defines the terminology for pacemakers, ICD and CRT systems and implantable monitors, is particularly noteworthy [89]. This terminology enables semantically structured data transfer from the manufacturer-specific ICT system to the electronic medical history.
For telemonitoring of data from CIED, the IT standards mentioned in the Telemonitoring Framework Directive are recommended [88]. Development in this area is very dynamic and it is strongly recommended that further development of the IT standards be performed jointly with the user organizations and the representatives of the manufacturers in Austria as well as with the international partner organizations, above all HL7, IEEE, PCHA, IHE, ESC, HRS, and the associations representing the device manufacturers in Austria (AustroMed) and in Europe (MedTech Europe) (Table 5). It is also recommended that this cooperation be sustainable for the longer term. For this purpose, sufficient resources and structures are to be provided in order to include all interested parties concerned (e.g. physicians and other healthcare practitioners, device manufacturers, standardization organizations, ELGA).
Economic aspects of telemonitoring—benefits for the healthcare system
Of course, any assessment of a new technology today must also include its economic benefit. Already in 2015, the European Health Economic Trial on Home Monitoring in ICD patients attempted to show the impact on costs and net financial impact in five European countries [90]. For this purpose, 312 VVI or DDD-ICD patients were randomly assigned to receive care with or without telemonitoring and a clear difference was shown in how both groups used resources. Patients with RM required significantly fewer outpatient check-ups (3.79 ± 1.67 vs. 5.53 ± 2.32; p < 0.001), numerically fewer hospital admissions (0.67 ± 1.18 vs. 0.85 ± 1.43; p < 0.23) and shorter hospital stays (6.31 ± 15.5 days vs. 8.26 ± 18.6 days; p < 0.27). From the perspective of the providers (physicians and hospitals), the expenditures for patient follow-up were similar, with the total cost per patient being numerically (not significantly) lower. The net financial impact did not differ between the two groups.
In 2016, the Health Economics Committee of the European Heart Rhythm Association published a meta-analysis of randomized controlled studies on telemonitoring of implantable cardiac electronic devices and their effect on use of the healthcare system [91]. This analysis of 11 studies showed that RM led to a significant reduction in patient contacts (RR = 0.6; 95% CI = 0.43–0.73, p < 0.001) at similar rates of hospitalization. The total costs for patient care were reduced by 10–55% with RM.
Another meta-analysis looked at the largest randomized controlled trials for RM of ICD patients: IN-TIME, ECOST and TRUST [92]. This meta-analysis of more than 2400 patients showed RM to bring an absolute mortality reduction of 1.9% (95% CI = 0.1–3.8%; p = 0.037) after 1 year, as well as a reduction in the combined endpoint mortality from any cause or hospitalization for HF of 5.6% (p = 0.007; RR = 0.64). An economic analysis has not yet been conducted, but especially the massive reduction in hospital admissions should indicate a clear advantage for RM.
Thus, also from an economic point of view the use of telemonitoring for implantable cardiac electronic devices can be seen to make sense. A prerequisite in Austria is certainly the suitability of telemedical services for billing purposes in order to be able to provide sufficient resources in this area.
Abbreviations
- AAI:
-
Single chamber atrial pacing
- AAIR:
-
Single chamber atrial rate response pacing
- ACS:
-
Acute coronary syndrome
- AF:
-
Atrial fibrillation
- AHA:
-
American Heart Association
- AHRE:
-
Atrial high-rate episode
- AI:
-
Artificial intelligence
- ATP:
-
Antitachycardia pacing
- CDA:
-
Clinical document architecture
- CHD:
-
Coronary heart disease
- CIED:
-
Cardiac implantable electronic device
- CR:
-
Cardiac rehabilitation
- CRT:
-
Cardiac resynchronization therapy
- CRT‑P:
-
Cardiac resynchronization therapy-pacing only
- CRT‑D:
-
Cardiac resynchronization therapy with defibrillator/cardioverter back-up
- CTR:
-
Cardiac telerehabilitation
- DDD:
-
Dual chamber sequential pacing
- DDDR:
-
Dual chamber sequential rate response pacing
- DGK:
-
German Society for Cardiology
- DMP:
-
Disease management program
- ELGA:
-
“Elektronische Gesundheitsakte” (Electronic health records)
- ERAP:
-
Expanded rehabilitation/aftercare program
- ERI:
-
Elective replacement indicator
- ESC:
-
European Society of Cardiology
- HFA:
-
Heart Failure Association of the ESC
- HL7:
-
Health Level Seven International
- HRS:
-
Heart Rhythm Society
- ICD:
-
Implantable defibrillator cardioverter
- ICT:
-
Information and communication technology
- IEGM:
-
Intracardiac electrogram
- ILR:
-
Implantable loop recorder
- IT:
-
Information technology
- NYHA:
-
New York Heart Association
- ÖKG:
-
Austrian Cardiological Society
- PDA:
-
Personal digital assistant
- PM:
-
Pacemaker
- R:
-
Rehabilitation
- RI:
-
Remote interrogation
- RM:
-
Remote monitoring
- RRT:
-
Recommended replacement time
- S‑ICD:
-
Subcutaneous implantable defibrillator cardioverter
- TM:
-
Telemedicine
- TMC:
-
Telemedical center
- TR:
-
Telerehabilitation
- VC:
-
Videoconferencing
- VVI:
-
Single chamber ventricular pacing
- VVIR:
-
Single chamber ventricular rate response pacing
- WHO:
-
World Health Organization
References
Wilkins E, Wilson L, Wickramasinghe K, et al. European cardiovascular disease statistics 2017. Brussels: European Heart Network; 2017.
Atlas Writing Group, Timmis A, Townsend N, Gale C, et al. European Society of Cardiology: Cardiovascular Disease Statistics 2017. Eur Heart J. 2018;39:508–79. https://doi.org/10.1093/eurheartj_ehx628.
Gruska M. Telemedizin in der Kardiologie. J Kardiol. 2009;16:66–70.
Schwamm LH, Chumbler N, Brown E, et al. Recommendations for the implementation of telehealth in cardiovascular and stroke care: a policy statement from the American Heart Association. Circulation. 2017;135:e24–e44. https://doi.org/10.1161/cir.0000000000000475.
Frederix I, Caiani EG, Dendale P, et al. ESC e‑Cardiology Working Group Position Paper: overcoming challenges in digital health implementation in cardiovascular medicine. Eur J Prev Cardiol. 2019;26:1166–77. https://doi.org/10.1177/2047487319832394.
Stockburger M, Helms TM, Perings CA, et al. Nutzenbewertung des strukturierten Telemonitorings mithilfe von aktiven Herzrhythmusimplantaten. Kardiologe. 2017;11:452–9. https://doi.org/10.1007/s12181-017-0203-8.
Helms TM, Müller A, Perings C, et al. Das Telemedizinische Zentrum als essenzieller Baustein konzeptioneller Ansätze zum Telemonitoring kardialer Patienten. Herzschrittmacherther Elektrophysiol. 2017;28:293–302. https://doi.org/10.1007/s00399-017-0527-x.
Helms TM, Stockburger M, Köhler F, et al. Grundlegende Strukturmerkmale eines kardiologischen Telemedizinzentrums für Patienten mit Herzinsuffizienz und implantierten Devices, Herzrhythmusstörungen und erhöhtem Risiko für den plötzlichen Herztod. Herzschrittmacherther Elektrophysiol. 2019;30:136–42. https://doi.org/10.1007/s00399-018-0606-7.
Helms TM, Stockburger M, Köhler F, et al. Positionspapier Telemonitoring. Herzschrittmacherther Elektrophysiol. 2019;30:287–97. https://doi.org/10.1007/s00399-019-0630-2.
WHO. A health telematics policy in support of WHO’s Health-For-All strategy for global health development: report of the WHO group consultation on health telematics. 11–16 December 1997; Geneva. Geneva: World Health Organization; 1998.
WHO. Global Observatory for eHealth. Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. Geneva: World Health Organization; 2010.
Pagliari C, Sloan D, Gregor P, et al. What is eHealth (4): a scoping exercise to map the field. J Med Internet Res. 2005;7(1):e9. https://doi.org/10.2196/jmir.7.1.e9.
Istepanian RSH, Pattichis SC, Laxmiinarayan S. Ubiquitous mHealth systems and the convergence towards 4G mobile technologies. In: Istepanian RSH, Pattichis SC, Laxmiinarayan S, editors. M‑health: emerging mobile health systems. London: Springer; 2006. pp. 3–14.
Europäische Kommission. 219 final: Grünbuch über Mobile-Health-Dienste. Brüssel: Europäische Kommission. COM; 2014.
Rodriguez AC, Roda C, Gonzalez P, et al. Contextualizing tasks in telerehabilitation systems for older people. In: International workshop on ambient assisted living. Cham: Springer; 2015. pp. 29–41.
Brennan DM, Tindall L, Theodoros D, et al. A blueprint for telerehabilitation guidelines-October 2010. Telemed J E Health. 2011;17:662–5. https://doi.org/10.1089/tmj.2011.0036.
Rybak K. Telemedizin in der Überwachung und Nachsorge von Herzschrittmachern und Systemen zur Kardialen Resynchronisationstherapie (CRT). In: Goss F, Middeke M, Mengden T, al, editors. Praktische Telemedizin in Kardiologie und Hypertensiologie. Stuttgart: Springer; 2009. pp. 58–77.
Varma N, Epstein AE, Irimpen A, et al. Efficacy and safety of automatic remote monitoring for implantable cardioverter-defibrillator follow-up: the Lumos‑T Safely Reduces Routine Office Device Follow-up (TRUST) trial. Circulation. 2010;122:325–32. https://doi.org/10.1161/circulationaha.110.937409.
Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace. 2013(15):1070–1011. https://doi.org/10.1093/europace/eut206.
Mabo P, Victor F, Bazin P, et al. A randomized trial of long-term remote monitoring of pacemaker recipients (the COMPAS trial). Eur Heart J. 2012;33:1105–11. https://doi.org/10.1093/eurheartj/ehr419.
Crossley GH, Chen J, Choucair W, et al. Clinical benefits of remote versus transtelephonic monitoring of implanted pacemakers. J Am Coll Cardiol. 2009;54:2012–9. https://doi.org/10.1016/j.jacc.2009.10.001.
Shanmugam N, Boerdlein A, Proff J, et al. Detection of atrial high-rate events by continuous home monitoring: clinical significance in the heart failure-cardiac resynchronization therapy population. Europace. 2012;14:230–7. https://doi.org/10.1093/europace/eur293.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975. https://doi.org/10.1002/ejhf.592.
Slotwiner D, Varma N, Akar JG, et al. HRS Expert Consensus Statement on remote interrogation and moni-toring for cardiovascular implantable electronic devices. Heart Rhythm. 2015;12:e69–e100. https://doi.org/10.1016/j.hrthm.2015.05.008.
Varma N, Piccini J, Snell J, et al. The relationship between level of adherence to automatic wireless remote monitoring and survival in pacemaker and defibrillator patients. J Am Coll Cardiol. 2015;65:2601–10. https://doi.org/10.1016/j.jacc.2015.04.033.
Capucci A, de Simone A, Luzi M, et al. Economic impact of remote monitoring after implantable defibrillators implantation in heart failure patients: an analysis from the EFFECT study. Europace. 2017;19:1493–9. https://doi.org/10.1093/europace/eux017.
Ladapo JA, Turakhia MP, Ryan MP, et al. Health Care Utilization and Expenditures Associated with remote monitoring in patients with implantable cardiac devices. Am J Card. 2016;117:1455–62. https://doi.org/10.1016/j.amjcard.2016.02.015.
Boriani G, Da Costa A, Quesada A, et al. Effects of remote monitoring on clinical outcomes and use of healthcare resources in heart failure patients with biventricular defibrillators: results of the MORE-CARE multicentre randomized controlled trial. Eur J Heart Fail. 2017;19:416–25. https://doi.org/10.1002/ejhf.626.
Santini M, Gasparini M, Landolina M, et al. Device-detected atrial tachyarrhythmias predict adverse outcome in real-world patients with implantable biventricular defibrillators. J Am Coll Cardiol. 2011;57:167–72. https://doi.org/10.1016/j.jacc.2010.08.624.
Crossley GH, Boyle A, Vitense H, et al. The CONNECT (Clinical Evaluation of Remote Notification to Reduce Time to Clinical Decision) trial: the value of wireless remote monitoring with automatic clinician alerts. J Am Coll Cardiol. 2011;57:1181–9. https://doi.org/10.1016/j.jacc.2010.12.012.
Guédon-Moreau L, Lacroix D, Sadoul N, et al. A randomized study of remote follow-up of implantable cardioverter defibrillators: safety and efficacy report of the ECOST trial. Eur Heart J. 2013;34:605–14. https://doi.org/10.1093/eurheartj/ehs425.
Hindricks G, Taborsky M, Glikson M, et al. Implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME): a randomised controlled trial. Lancet. 2014;384:583–90.
Vamos M, Nyolczas N, Bari Z, et al. Refined heart failure detection algorithm for improved clinical reliability of Optivol alerts in CRT‑D recipients. Card J. 2018;25:236–44. https://doi.org/10.5603/cj.a2017.0077.
Boehmer JP, Hariharan R, Devecchi FG, et al. A multisensor algorithm predicts heart failure events in patients with implanted devices: results from the multiSENSE study. JACC Heart Fail. 2017;5:216–25. https://doi.org/10.1016/j.jchf.2016.12.011.
Leclercq C, Burri H, Curnis A, et al. Cardiac resynchronization therapy non-responder to responder conversion rate in the more response to cardiac resynchronization therapy with MultiPoint Pacing (MORE-CRT MPP) study: results from Phase I. Eur Heart J. 2019;40:2979–87. https://doi.org/10.1093/eurheartj/ehz109.
Hindricks G, Elsner C, Piorkowski C, et al. Quarterly vs. yearly clinical follow-up of remotely monitored recipients of prophylactic implantable cardioverter-defibrillators: results of the REFORM trial. Eur Heart J. 2014;35:98–105. https://doi.org/10.1093/eurheartj/eht207.
Saxon LA, Hayes DL, Gilliam FR, et al. Long-term outcome after ICD and CRT implantation and influence of remote device follow-up: the ALTITUDE survival study. Circulation. 2010;122:2359–67. https://doi.org/10.1161/circulationaha.110.960633.
Akar JG, Bao H, Jones PW, et al. Use of remote monitoring is associated with lower risk of adverse outcomes among patients with implanted cardiac defibrillators. Circ Arrhythm Electrophysiol. 2015;8:1173–80. https://doi.org/10.1161/circep.114.003030.
Mittal S, Piccini J, Snell J, et al. Improved surivival in patients enrolled promptly into remote monitoring following cardiac electronic device implantation. J Interv Card Electrophysiol. 2016;46:129–36. https://doi.org/10.1007/s10840-016-0112-y.
Parthiban N, Esterman A, Mahajan R, et al. Remote monitoring of implantable cardioverter-defibrillators: a systematic review and meta-analysis of clinical outcomes. J Am Coll Cardiol. 2015;65:2591–600. https://doi.org/10.1016/j.jacc.2015.04.029.
García-Fernández FJ, Osca-Asensi J, Romero R, et al. Safety and efficiency of a common and simplified protocol for pacemaker and defibrillator surveillance based on remote monitoring only: a long-term randomized trial (RM-ALONE). Eur Heart J. 2019;40:1837–46. https://doi.org/10.1093/eurheartj/ehz067.
Brignole M, Vardas P, Hoffman E, et al. Indications for the use of diagnostic implantable and external ECG loop recorders. Europace. 2009;11:671–87. https://doi.org/10.1093/europace/eup097.
Bloch Thomsen PE, Jons C, Raatikainen MJ, et al. Long-term recording of cardiac arrhythmias with an implantable cardiac monitor in patients with reduced ejection fraction after acute myocardial infarction: the Cardiac Arrhythmias and Risk Stratification After Acute Myocardial Infarction (CARISMA) study. Circulation. 2010;122:1258–64. https://doi.org/10.1161/circulationaha.109.902148.
Krahn AD, Klein GJ, Yee R, et al. Final results from a pilot study with an implantable loop recorder to determine the etiology of syncope in patients with negative noninvasive and invasive testing. Am J Cardiol. 1998;82:117–9.
Hindricks G, Pokushalov E, Urban L, et al. Performance of a new leadless implantable cardiac monitor in detecting and quantifying atrial fibrillation: results of the XPECT trial. Circ Arrhythm Electrophysiol. 2010;3:141–7. https://doi.org/10.1161/circep.109.877852.
Pürerfellner H, Sanders P, Pokushalov E, et al. Miniaturized reveal LINQ insertable cardiac monitoring system: first-in-human experience. Heart Rhythm. 2015;12:1113–9. https://doi.org/10.1016/j.hrthm.2015.02.030.
Sanders P, Pürerfellner H, Pokushalov E, et al. Performance of a new atrial fibrillation detection algorithm in a miniaturized insertable cardiac monitor: results from the Reveal LINQ Usability Study. Heart Rhythm. 2016;13:1425–30. https://doi.org/10.1016/j.hrthm.2016.03.005.
Brignole M, Moya A, de Lange FJ, et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J. 2018;39:1883–948. https://doi.org/10.1093/eurheartj/ehy037.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019;140:e125–e51.
Maines M, Zorzi A, Tomasi G, al at. Clinical impact, safety, and accuracy of the remotely monitored implantable loop recorder Medtronic Reveal LINQTM. Europace. 2018;20:1050–7. https://doi.org/10.1093/europace/eux187.
Søgaard P, Behrens S, Konyi A, et al. Transmission and loss of ECG snapshots: Remote monitoring in implantable cardiac monitors. J Electrocardiol. 2019;56:24–8. https://doi.org/10.1016/j.jelectrocard.2019.06.005.
Eurlings CGMJ, Boyne JJ, de Boer RA, et al. Telemedicine in heart failure-more than nice to have? Neth Heart J. 2019;27:5–15. https://doi.org/10.1007/s12471-018-1202-5.
Cowie MR, Bax J, Bruining N, et al. e‑Health: a position statement of the European Society of Cardiology. Eur Heart J. 2016;37:63–6. https://doi.org/10.1093/eurheartj/ehv416.
Von der Heidt A, Ammenwerth E, Bauer K, et al. HerzMobil Tirol network: rationale for and design of a collaborative heart failure disease management program in Austria. Wien Klin Wochenschr. 2014;126:734–41. https://doi.org/10.1007/s00508-014-0665-7.
Modre-Osprian R, Poelzl G, Von Der Heidt A, et al. Closed-loop healthcare monitoring in a collaborative heart failure network. Stud Health Technol Inform. 2014;198:17–24. https://doi.org/10.3233/978-1-61499-397-1-17.
Ammenwerth E, Fetz B, Gstrein S, et al. Herzmobil, an integrated and collaborative telemonitoring-based disease management program for patients with heart failure: a feasibility study paving the way to routine care. JMIR Cardio. 2018;2:e11. https://doi.org/10.2196/cardio.9936.
Poelzl G, Fetz B, Altenberger J, et al. Heart failure disease management programs in Austria 2019—a systematic survey of the Heart Failure Working Group and the Working Group for Cardiological Assistance and Care Personnel of the Austrian Society of Cardiology. Wien Klin Wochenschr. 2020; https://doi.org/10.1007/s00508-020-01615-y.
Koehler F, Koehler K, Deckwart O, et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392:1047–57. https://doi.org/10.1016/s0140-6736(18)31880-4.
Nigls SC, Clark RA, Dierckx R, et al. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst Rev. 2015; https://doi.org/10.1002/14651858.cd007228.pub3.
Seferovic PM, Ponikowski P, Anker SD, et al. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21:1169–86. https://doi.org/10.1002/ejhf.1531.
Wagenaar KP, Broekhuizen BDL, Jaarsma T, et al. Effectiveness of the European Society of Cardiology/Heart Failure Association website ‘heartfailurematters.org’ and an e‑health adjusted care pathway in patients with stable heart failure: results of the ‘e-Vita HF’ randomized controlled trial. Eur J Heart Fail. 2019;21:238–46. https://doi.org/10.1002/ejhf.1354.
Abraham WT, Stevenson LW, Bourge RC, et al. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: complete followup results from the CHAMPION randomised clinical trial. Lancet. 2016;387:453–61. https://doi.org/10.1016/s0140-6736(11)60101-3.
Eggerth A, Modre-Osprian R, Hayn D, et al. Comparison of body weight trend algorithms for prediction of heart failure related events in home care setting. Stud Health Technol Inform. 2017;236:219–26. https://doi.org/10.3233/978-1-61499-759-7-219.
Moertl D, Altenberger J, Bauer N, et al. Disease management programs in chronic heart failure: position statement of the Heart Failure Working Group and the Working Group of the Cardiological Assistance and Care Personnel of the Austrian Society of Cardiology. Wien Klin Wochenschr. 2017;129:869–78. https://doi.org/10.1007/s00508-017-1265-0.
Oldridge N, Pakosh M, Grace SL. A systematic review of recent cardiac rehabilitation meta-analyses in patients with coronary heart disease or heart failure. Future Cardiol. 2019;15:227–49. https://doi.org/10.2217/fca-2018-0085.
Pack QR, Goel K, Lahr BD, et al. Participation in cardiac rehabilitation and survival after coronary artery bypass graft surgery: a community-based study. Circulation. 2013;128:590–7. https://doi.org/10.1161/circulationaha.112.001365.
Kotseva K, Wood D, De Bacquer D, et al. EUROASPIRE IV: a European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol. 2016;23:636–48. https://doi.org/10.1177/2047487315569401.
Gyimesi M, Fülöp G, Ivansits S, et al. Rehabilitationsplan. Wien: Gesundheit Österreich; 2016.
Mampuya WM. Cardiac rehabilitation past, present and future: an overview. Cardiovasc Diagn Ther. 2012;2:38–49. https://doi.org/10.3978/j.issn.2223-3652.2012.01.02.
Janssen V, De Gucht V, van Exel H, et al. Beyond resolutions? A randomized controlled trial of a self-regulation lifestyle programme for post-cardiac rehabilitation patients. Eur J Prev Cardiol. 2013;20:431–41. https://doi.org/10.1177/2047487312441728.
Brouwers RW, Kraal JJ, Traa SC, et al. Effects of cardiac telerehabilitation in patients with coronary artery disease using a personalised patient-centred web application: protocol for the SmartCare-CAD randomised controlled trial. BMC Cardiovasc Disord. 2017;17:46–57. https://doi.org/10.1186/s12872-017-0477-6.
Galea MD. Telemedicine in rehabilitation. Phys Med Rehabil Clin N Am. 2019;30:473–83. https://doi.org/10.1016/j.pmr.2018.12.002.
Frederix I, Solmi F, Piepoli MF, et al. Cardiac telerehabilitation: a novel cost-efficient care delivery strategy that can induce long-term health benefits. Eur J Prev Cardiol. 2017;24:1708–17. https://doi.org/10.1177/2047487317732274.
Thorup CB, Grønkjær M, Spindler H, et al. Pedometer use and self-determined motivation for walking in a cardiac telerehabilitation program: a qualitative study. BMC Sports Sci Med Rehabil. 2016;8:24. https://doi.org/10.1186/s13102-016-0048-7.
Frederix I, Vandijck D, Hens N, et al. Economic and social impact of increased cardiac rehabilitation uptake and cardiac telerehabilitation in Belgium—a cost-benefit analysis. Acta Cardiol. 2017;73:222–9. https://doi.org/10.1080/00015385.2017.1361892.
Hwang R, Bruning J, Morris NR, et al. Home-based telerehabilitation is not inferior to a centre-based program in patients with chronic heart failure: a randomised trial. J Physiother. 2017;63:101–7. https://doi.org/10.1016/j.jphys.2017.02.017.
Piotrowicz E, Baranowski R, Bilinska M, et al. A new model of home-based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence. Eur J Heart Fail. 2010;12:164–71. https://doi.org/10.1093/eurjhf_hfp181.
Piotrowicz E, Zieliski T, Bodalski R, et al. Home-based telemonitored Nordic walking training is well accepted, safe, effective and has high adherence among heart failure patients, including those with cardiovascular implantable electronic devices: a randomised controlled study. Eur J Prev Cardiol. 2015;22:1368–77. https://doi.org/10.1177/2047487314551537.
Nouryan C, Morahan S, Pecinka K, et al. Home telemonitoring of community dwelling heart failure patients after home care discharge. Telemed J E Health. 2019;25:447–54. https://doi.org/10.1089/tmj.2018.0099.
Momsen AH, Hald K, Nielsen CV, et al. Effectiveness of expanded cardiac rehabilitation in patients diagnosed with coronary heart disease: a systematic review protocol. JBI Database System Rev Implement Rep. 2017;15:212–9. https://doi.org/10.11124/jbisrir-2016-003265.
Fors A, Swedberg K, Ulin K, et al. Effects of personcentred care after an event of acute coronary syndrome: two-year follow-up of a randomised controlled trial. Int J Cardiol. 2017;249:42–7. https://doi.org/10.1016/j.ijcard.2017.08.069.
Müller A, Rybak K, Klingenheben T, et al. Empfehlungen zum Telemonitoring bei Patienten mit implantierten Herzschrittmachern, Defibrillatoren und kardialen Resynchronisationssystemen. Kardiologe. 2017;7:181–93. https://doi.org/10.1007/s12181-013-0496-1.
Slotwiner DJ, Abraham RL, Al-Khatib SM, et al. HRS White Paper on interoperability of data from cardiac implantable electronic devices (CIEDs). Heart Rhythm. 2019;16:e107–e27. https://doi.org/10.1016/j.hrthm.2019.05.002.
Slotwiner DJ, Tarakji KG, Al-Khatib SM. Transparent sharing of digital health data: a call to action. Heart Rhythm. 2019;16:e95–e106. https://doi.org/10.1016/j.hrthm.2019.04.042.
EU Commission. European interoperability framework—implementation strategy, annex 2. COM; 2017. 134 final, Brussels, 23.3.2017.
EU Commission. Recommendation on a European Electronic Health Record exchange format. Brussels, 2019. (C(2019)800).
EU Commission. Commission Decision 2015/1302 of 28 July 2015 on the identification of ‘Integrating the Healthcare Enterprise’ profiles for referencing in public procurement. Brussels, 2015.
Sauermann S. Rahmenrichtlinie für die IT-Infrastruktur bei der Anwendung von Telemonitoring. Wien: BMGAS; 2018.
IEEE/ISO/CEN 11073. Health informatics—Point-of-care medical device communication.
Heidbuchel H, Hindricks G, Broadhurst P, et al. EuroEco (European Health Economic Trial on Home Monitoring in ICD Patients): a provider perspective in five European countries on costs and net financial impact of follow-up with or without remote monitoring. Eur Heart J. 2015;36:158–69. https://doi.org/10.1093/eurheartj_ehu339.
Klersy C, Boriani G, De Silvestri A, et al. Effect of telemonitoring of cardiac implantable electronic devices on healthcare utilization: a meta-analysis of randomized controlled trials in patients with heart failure. Eur J Heart Fail. 2016;18:195–204. https://doi.org/10.1002/ejhf.470.
Hindricks G, Varma N, Kacet S, et al. Daily remote monitoring of implantable cardioverter-defibrillators: insights from the pooled patient-level data from three randomized controlled trials (IN-TIME, ECOST, TRUST). Eur Heart J. 2017;38:1749–55. https://doi.org/10.1093/eurheartj/ehx015.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
M. Gruska has received research grants and/or honoraria from the following companies: Biotronik. L. Fiedler has received research grants and/or honoraria from the following companies: Abbott, Biotronik, Boston Scientific. M. Gwechenberger has received research grants and/or honoraria from the following companies: Abbott, Biotronik, Boston Scientific, Medtronic. P. Lercher has received research grants and/or honoraria from the following companies: Biotronik, Medtronic. M. Martinek has received research grants and/or honoraria from the following companies: Abbott, Biotronik, Boston Scientific, Medtronic. M. Nürnberg has received research grants and/or honoraria from the following companies: Abbott, Biotronik, Boston Scientific, Medtronic. C. Schukro has received research grants and/or honoraria from the following companies: Biotronik, Boston Scientific, Medtronic. D. Scherr has received research grants and/or honoraria from the following companies: Biotronik, Medtronic, Zoll. C. Steinwender has received research grants and/or honoraria from the following companies: Abbott, Biotronik, Boston Scientific, Medtronic. M. Stühlinger has received research grants and/or honoraria from the following companies: Biotronik, Medtronic. A. Teubl has received research grants and/or honoraria from the following companies: Abbott, Biotronik, Microport. G. Aigner, J. Altenberger, D. Burkart-Küttner, G. Pölzl, G. Porenta and S. Sauermann declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The present recommendations were approved by the Austrian Cardiological Society in a resolution adopted by the Board of Directors on 2 March 2020.
All authors contributed equally to this position paper on behalf of the Working Group Rhythmology of the Austrian Cardiological Society.
Rights and permissions
About this article
Cite this article
Gruska, M., Aigner, G., Altenberger, J. et al. Recommendations on the utilization of telemedicine in cardiology. Wien Klin Wochenschr 132, 782–800 (2020). https://doi.org/10.1007/s00508-020-01762-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-020-01762-2