Abstract
Telecardiology is one of the fastest-growing fields in telemedicine. In primary care, teleconsultations, telediagnosis, and tele-education, applied in an integrated manner, possibly associated with tools such as computer decision support systems, may improve the quality of care for cardiovascular diseases, especially hypertension, atrial fibrillation, heart failure, and acute myocardial infarction (AMI). In specialized care, there is extensive literature on the use of telemonitoring among patients with heart failure (HF), with evidence of reduced number of hospitalizations and all-cause mortality, as well promotion of patient empowerment. Several studies have demonstrated that hypertension telemonitoring strategies have a beneficial short- and medium-term impact on blood pressure control. Telecardiology has also different applications in emergency services, including electrocardiogram transmission, which can be associated with synchronous teleconsultation, to assist the early diagnosis and management of patients with acute coronary syndrome (ACS), with evidence of reduced AMI short- and long-term mortality. Decision support systems could also to aid in the diagnosis, management, and prediction of cardiac complications in patients with ACS, prehospital bedside ultrasound image transmission, and image transmission and support in the diagnosis and management of patients with stroke. Telehealth interventions aimed at enabling remote rehabilitation programs can overcome barriers to access while preserving clinical supervision and individualized exercise prescription. Remote monitoring using implantable devices has mixed results in clinical outcomes. Cost and quality in a telecardiology service are strictly related to the monitoring and management of the process.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Telemedicine
- Telecardiology
- Teleconsultation
- Tele-regulation
- Telediagnosis
- Tele-education
- Telehealth
- Noncommunicable diseases
- Primary care
- Specialized care
Telecardiology
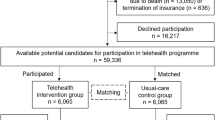
In this chapter, we aimed to make an overview of recent applications of telecardiology in primary and specialized care, as well as to give examples of our practice in telecardiology. Our group is part of a Brazilian public telehealth network, the Telehealth Network of Minas Gerais, a partnership among seven public universities, with broad experience in cardiology. Since 2005, more than 4.9 million tele-electrocardiograms have already been analyzed, as well as 3693 Holter, 655 ambulatory blood pressure monitoring, and 133,284 teleconsultations. We have been working on different clinical decision support systems and short message service (SMS) programs.
Telecardiology in Primary Care
In primary care, teleconsultations, tele-diagnosis, and tele-education, applied in an integrated manner, possibly associated with tools such as decision support systems (DSS), may improve the quality of care for cardiovascular diseases, especially hypertension, atrial fibrillation, heart failure, and acute myocardial infarction. In remote municipalities with few inhabitants, primary care is often the only level of local healthcare and may receive patients with acute cardiovascular disease in an outpatient setting, especially in large countries with less integrated systems with difficult patients’ removal to a more complex healthcare unit. Thus, telecardiology in primary care may improve the quality of care not only for chronic diseases, but also may support the emergency care for acute coronary diseases and arrhythmias.
Tele-regulation may support primary care to qualify access to specialized care. The applications of telecardiology in primary care will be briefly reviewed.
Health Promotion and Prevention
In cardiology, health promotion actions for primary and secondary prevention of cardiovascular diseases have an outstanding impact in morbimortality, and may be associated with significant cost reduction in healthcare expenses due to the decrease in specialized consultations, hospitalizations, and emergency hospital admissions [1]. Telemedicine may be useful in controlling risk factors for coronary artery disease, such as improving blood pressure (BP) control [2,3,4,5], reducing glycohemoglobin in diabetic patients [6,7,8], and improving lipid profile [9, 10]. Furthermore, it may help to reduce weight, body mass index (BMI), and waist circumference in obese or overweight patients [5, 11,12,13] as well as increasing the success of smoking cessation programs [14].
Several modalities of telemedicine can assist in this regard, such as mobile phone text or audio messaging systems, which have shown positive results in medication adherence, change in eating habits, and physical activity in patients with hypertension, diabetes, obesity, or patients who had an acute myocardial infarction (AMI) [13, 15]. Twenty-four-hour monitoring services are becoming more frequent through the development of pieces of equipment which are linked to telemedicine systems, such as a stethoscope, balance, digital thermometer, BP monitors, remote monitoring of vital signs, and implantable electronic devices [16, 17]. Even simple watches have been transformed into monitoring systems with technology to report heart rate, presence of arrhythmias, stress level (analyzing humidity and skin temperature), optical BP monitoring, and physical activity [18, 19]. There are several applications which are now available for the guidance of healthcare professionals, patients, or even for self-care [16].
Decision Support Systems
Decision Support Systems (DSS) add knowledge and information of specific patients for physicians, other healthcare professionals, or patients themselves to improve the quality of the treatment and patient outcomes (www.healthit.gov/topic/safety/clinical decision support). The Community Preventive Services Task Force recommends using these systems in the prevention of cardiovascular diseases. Such recommendation is based on low-to-moderate quality of evidence, which show an increase in cardiovascular risk factors screening; antiplatelet therapy prescription for primary prevention; and also, healthy diet, physical activity, and smoking cessation counseling [20]. It may have wide application in primary healthcare, but results are still inconsistent when considering its clinical impact, with few isolated studies demonstrating an increase in smoking abstinence, adherence to drug treatment, and physical activity engagement, and a slight reduction in BMI (mean reduction = −0.10) [21].
Regarding emergency room (ER) admissions, hospitalizations, and cardiovascular events, studies have shown no consistent impact so far, but further studies are required. In one study, which assessed an educational strategy for health professionals associated with DSS alerts compared to an isolated educational strategy, lower mortality rates were observed in the intervention group [22].
Teleconsultation
Teleconsultation can be defined as a second opinion system that allows information exchange between distant healthcare professionals and local healthcare professionals to discuss a clinical case when a specialist is not locally available (Fig. 24.1) [23]. They can be synchronous/real-time (with simultaneous interaction; by video, web conference, telephone, or toll-free telephone number) or asynchronous/store-and-forward, in a time-independent basis (Fig. 24.1).
Teleconsultations may have great applications in primary care to support healthcare professionals in remote and resource-constrained areas, including timely access to correct medical information, quality improvement of the diagnosis and treatment process, increased physician trust, and significant improvement in the total quality of healthcare [24]. As a tool with potential to increase primary care resolution, it may be incorporated into the workflow of primary care units as a part of the regulatory process of the municipality. Thus, it represents an efficient way to reduce waiting times for a face-to-face appointment with a cardiologist.
There are still few studies on the impact of teleconsultations on hard outcomes, such as mortality. A systematic review by Liddy et al. [25] cited a randomized study comparing patients who had had teleconsultation to those who had been offered a traditional referral. The authors assessed the impact on death, myocardial infarction, catheterization or emergency angioplasty, and ER visits. The teleconsultation group was more likely to have an appointment with the cardiologist and fewer ER admissions.
Continued education and professional qualification are other benefits of the teleconsultations, as well as a reduced sense of isolation, for the professionals who work in remote areas.
Overall, patients and medical professionals appear to be satisfied with teleconsultation services [26,27,28]. However, the quality of the service should be assessed periodically using predetermined criteria to ensure sustained positive effects (Fig. 24.2) [29]. Our group recently published a paper describing a methodology to analyze the quality of teleconsultations [24].
The methodology started with a literature review to analyze methodologies that had already been used to evaluate the quality of asynchronous teleconsultations in the following databases: Medline, Lilacs, and Scielo. In Medline, the following descriptors were used: telemedicine, remote consultation, medical audit; and terms: teleconsultation, audit, quality. In Lilacs and Scielo corresponding terms were used. Due to the lack of studies analyzing teleconsultation in the literature, it was necessary to develop our methodology. With this purpose, specialists from our group were consulted and an initial version was developed, tested, and improved over time, resulting in the criteria showed in Table 24.1.
We established five domains which represented important items to be assessed:
-
1.
Quality: Technical and scientific knowledge based on the best online available evidence, point-of-care information summaries, and guidelines from the Brazilian Ministry of Health.
-
2.
Objective: Focus and details which are required for an answer to be complete.
-
3.
Ethics: If the teleconsultant has an ethical behavior.
-
4.
Courtesy: If the teleconsultant is polite when answering a query.
-
5.
Grammar: Adequacy of grammar and vocabulary basic rules).
Each category received a score from 1 to 3 from the lowest to the highest grade.
This methodology has been used for feedback of the teleconsultation team and continued improvement of our service (Fig. 24.2). It can be easily replicated in other services worldwide to guarantee high quality of periodic auditing and may have positive impact to the quality of services provided by large-scale telemedicine services.
Tele-Regulation
The demand for specialist referrals is growing worldwide, surpassing what most services can offer in terms of specialists’ consultation, and thus waiting lists are becoming increasingly longer [30]. Telehealth interventions, especially when involving tele-regulation, have shown a great impact in reducing waiting times, qualifying demands to avoid unnecessary referrals [31,32,33]. By using guiding protocols, tele-regulation enables to classify the demand for specialized care according to a risk classification, and the final decision regarding referrals’ priority is a joint decision between both the attending and the tele-regulator physician [30,31,32,33].
Telediagnosis
Tele-electrocardiography is a very popular modality in telecardiology, as it is a simple exam and requires low-cost technology for transmitting files easily, even with slow Internet connections (Fig. 24.3). It can be easily incorporated into the primary care routine, due to its great utility and technology suitability for places with basic infrastructure in poor and remote areas [34, 35]. Twenty-four-hour Holter monitoring and ambulatory blood pressure monitoring (ABPM) are other exams which have been analyzed by telecardiology services.
Recently, Artificial Intelligence (AI) has helped large electrocardiogram databases to facilitate the execution of the exam reports, as well as to increase their accuracy. Decision support systems qualify care, with the potential to improve the management of patients with cardiovascular diseases, such as hypertension, atrial fibrillation, and heart failure.
Tele-echocardiography has also shown to be a promising strategy to enable access to initial cardiology investigation, early diagnosis, prioritization of referrals, and organization of waiting lines in healthcare systems. Initial evidence for its use comes from population-based screening studies, such as in rural India, where more than 1000 echocardiograms were performed in about 11 hours and sent to the cloud computing with good agreement between preliminary field diagnosis and expert reports (k = 0.85) and an alarming 16% rate of significant abnormalities (including 32.9% of heart valve abnormalities) [36]. Evidence also suggests that even in high-income regions such as the United Kingdom, population-based echocardiographic screening in primary care by non-specialists proved to be an attractive strategy, with clinically significant (moderate-to-severe) valve disease observed in 6.4% of asymptomatic population aged ≥65 years, with prevalence associated with socioeconomic factors [37]. The strategy may be especially useful in low-income countries, where presumably there is a high burden of undiagnosed cardiovascular disease and limitations in the provision of specialized care, including conventional echocardiography. The tele-echocardiography strategy was initially tested in Brazil in a rheumatic heart disease screening program (study PROVAR: Rheumatic Valve Disease Screening Program), which established a research protocol acquisition routine at the research level simplified with portable and ultraportable devices by paramedics (nurses and technologists), uploaded to dedicated cloud computing system for expert storage and remote interpretation [38, 39]. In addition to remote diagnostics, telemedicine was also used for training health professionals on basic principles of echocardiography through interactive online modules. The effectiveness of online training has been demonstrated even by the accuracy of these professionals for the basic diagnosis of rheumatic heart disease [38]. In this project, there was a high prevalence of subclinical rheumatic heart disease (4.2%), a significant finding considering the impact of the disease on public health [40].
Telediagnosis exams should be submitted to periodic audits, to guarantee the quality of the services (Fig. 24.2).
Tele-Education
Remote educational activities in cardiology for healthcare professionals may help improving the quality of care. Patient-focused educational activities should also be encouraged for their empowerment.
Specialized Care
Heart Failure
There is extensive literature on the use of telemedicine strategies to monitor patients with heart failure (HF), aiming to reduce hospitalizations, which are associated with increased morbidity, mortality, and costs. Additionally, there is evidence it may increase the patients’ empowerment. Interventions range from using traditional technologies, such as structured telephone support, telemonitoring using innovative technologies with implantable or wearable devices, DSS, and machine learning to predict complications [41,42,43]. Although evidence is variable, overall there is a positive impact. However, the application of these strategies in clinical practice is still very limited by regulatory, logistical, and financial restraints [44].
Telemonitoring can be either invasive or noninvasive. Sensors are tools which are increasingly embedded in smartphones and other mobile devices, and are capable of detecting, recording, and responding to specific data, for instance, patients’ vital signs. Sensor’s logging can generate large data sets that can be transmitted in real time to healthcare professionals [45]. As many multi-professional intervention programs often have geographical, economic, and bureaucratic barriers, telemonitoring may be a solution to promote better care for patients with HF [41].
Evidence about structured telephone support and noninvasive telemonitoring in HF patients was summarized in a Cochrane systematic review, which included 41 studies. Structured telephone support has shown to reduce all-cause mortality (RR 0.87, 95% CI 0.77–0.98; n = 9222) and HF-related hospitalizations (RR 0.85, 95% CI 0.77–0.93; n = 7030), both with moderate quality of evidence. As for telemonitoring, it also reduced all-cause mortality (RR 0.80, 95% CI 0.68–0.94; n = 3740) and HF-related hospitalizations (RR 0.71, 95% CI 0.60–0.83; n = 2148), both with moderate quality of evidence [45].
In another meta-analysis [46], which assessed 26 studies, 2506 patients were followed by telemonitoring, including the transmission of vital signs, a time-dependent effect was observed. Short-term follow-up (up to 180 days) demonstrated better results in hard outcomes, including mortality, which were not achieved with a follow-up for a period longer than 1 year. On the other hand, telemonitoring has not shown to reduce hospitalization, regardless of the follow-up time. An increase in ER visits was observed in the telemonitoring group, thus, it raises the question of how an intervention that does not reduce hospitalization can impact on mortality. Perhaps early detection of decompensating sign encourages patients to seek medical attention, which can be promptly treated with diuretics and vasodilators without the need for intensive therapy.
The evidence regarding length of hospital stay is even more controversial as among seven structured telephone support and nine telemonitoring studies, only one study of each intervention observed a significant reduction in length of hospital stay. However, a much more noteworthy number of studies, 9 of 11 structured telephone support and 5 of 11 telemonitoring, reported significant improvements in quality of life and welfare. Three of nine structured telephone support studies and one of six cost-monitoring telemonitoring studies noted a reduction in cost, and two telemonitoring studies reported cost increases due to the cost of the intervention and increased medical management. Seven of the nine studies that assessed knowledge about HF and self-care behaviors observed significant improvements. Although acceptability among participants was observed between 76% and 97%, a decrease in participants’ adherence over time can be challenging. In this review, adherence rates varied between 55.1% and 65.8% for structured telephone support and 75% and 98.5% for telemonitoring [45].
The benefit of telemonitoring in HF was recently confirmed by the publication of “The Interventional Telemedical Management in Heart Failure II (TIM-HF2)” study. This was a prospective, randomized, and multicenter clinical trial in which 1571 HF patients with New York Heart Association (NYHA) functional classification II or III or those who had been hospitalized for heart failure within 12 months prior to randomization and with ejection fraction (LVEF) of 45% or less were randomly assigned to remote management or just usual care lasting up to 393 days [47]. Patients assigned to remote patient care lost an average of 17.8 days per year due to unplanned cardiovascular hospital admissions compared to 24.2 days per year for patients assigned to usual care. All-cause mortality had a hazard ratio (HR) 0.70, 95% (CI 0.50–0.96; p = 0.0280) in favor of telemonitoring, but cardiovascular mortality was not significantly different between the two groups (HR 0.671, 95% CI 0.45–1.01; p = 0.0560) [47].
New devices which monitor intracardiac pressures have the most compelling evidence for the use of telemonitoring and are related to the use of more advanced technologies. CardioMEMS is a device implanted percutaneously in the pulmonary artery that transmits central pressure values to a platform. When pulmonary artery pressure levels reach values above a certain threshold, the physician receives an alert and a trend statement indicating pulmonary congestion or low cardiac output. Other devices for right ventricular implantation are already in experimental use. The “CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients (CHAMPION)” study [48] evaluated HF patients with NYHA function capacity III in 64 United States centers, who were randomized to use an electronic central unit that receives hemodynamic data from CardioMEMS or for control group treatment. In the monitored group, doctors used daily data from pulmonary artery pressure measurements to guide treatment. At the mean follow-up of 15 months, there was a 37% reduction in the rate of HF-related hospitalizations compared to the control group [49].
Hypertension
Telemonitoring strategies can also be applied to control BP. They are frequently confused with the self-monitoring BP approach. Studies which evaluated antihypertensive medication titration using self-monitoring present contradictory results; moreover, the precise role of telemonitoring on self-monitoring is unclear.
Several studies have demonstrated that hypertension telemonitoring strategies with clinical pharmacist involvement have a beneficial short- and medium-term impact on BP control. Margolis et al. [50] evaluated the effect of this intervention after a 54-month follow-up in a randomized cluster study of 16 primary care centers, which involved 450 patients (228 in telemonitoring and 222 in usual care). The intensive telemonitoring intervention has shown sustained effects on BP control for up to 24 months (12 months after the end of the intervention), losing longer-term efficacy [50].
The INTERACT study was a randomized controlled trial in which 303 patients using oral antihypertensive and/or hypolipidemic medication were allocated to receive or not SMS text messages. The group receiving text messages improved adherence to the prescribed medication at 6 months compared to the patients who did not receive any messages. Overall, there was a 16% improvement in medication adherence [50, 51].
In the TASMINH4 study, 1182 patients were randomly allocated (1:1:1) for antihypertensive titration by the attending physician who used clinical readings (usual care group), performing monitoring alone (self-monitoring group), or using telemonitoring self-monitoring (telemonitoring group). It has been observed that the use of BP self-monitoring to support antihypertensive therapy in the treatment of individuals with poorly controlled hypertension in primary care results in lower systolic BP without increasing the workload of the healthcare team. After 1 year, patients whose medication was adjusted using self-monitoring, with or without telemonitoring, had significantly lower systolic blood pressure than those who received office-adjusted BP treatment. Blood pressure in the telemonitoring group for medication titration has a faster decrease (at 6 months than the control group), an effect that is likely to reduce cardiovascular events even further and may improve management [52, 53].
A Cochrane systematic review [54] aimed to establish the effectiveness of mobile phone interventions to improve medication adherence for primary prevention of cardiovascular disease in adults. Participants were recruited from primary care units or outpatient clinics in high-income countries (Canada, Spain) and middle- and high-income countries (South Africa, China), but interventions received varied widely. One trial evaluated an intervention focused on adherence to blood pressure medication, provided exclusively through the SMS, whereas a different intervention involved blood pressure monitoring combined with feedback provided via smartphone. The authors judged the body of evidence for the efficacy of mobile phone–based interventions as poor quality with regards to objective outcomes (blood pressure and cholesterol). Considering two studies which evaluated medication adherence along with lifestyle modifications, one reported a slight improvement in lowering low-density lipoprotein cholesterol (LDL-c), while the other found no benefit whatsoever. A study (1372 participants) of a text-based intervention for adherence showed little effect in systolic blood pressure reduction for the intervention group which received informational-only text messages, and uncertain evidence of benefit about the second intervention model which provided additional interactivity with participants. One study examined the effect of blood pressure monitoring combined with a mobile phone text-messaging system and reported moderate benefits on systolic and diastolic blood pressure. There was conflicting evidence from two trials aimed at adherence to medication along with lifestyle advice using multicomponent interventions. While the former found great benefits on blood pressure levels, the latter showed no such effect. The authors concluded that there is poor quality evidence regarding the effects of mobile phone interventions to increase adherence to prescription drugs for primary prevention. In conclusion, there is currently uncertainty about the effectiveness of such interventions based on this review.
Emergency Services
Telemedicine has different applications in emergency services , including electrocardiogram transmission, which can be associated with synchronous teleconsultation, to assist the early diagnosis and management of acute coronary syndrome (ACS) cases (Fig. 24.4) [55].
Schematic representation of telemedicine for emergency acute care. Treatment strategies using telemedicine are shown for Acute Coronary Syndrome (ACS). EKG: surface electrocardiogram. Situation A: The patient goes to the nearest RAU for own means, or calls the prehospital care service and is taken to the RAU for a basic ambulance without electrocardiograph. Situation B: The patient calls the prehospital care service and an ambulance without a doctor, but with an electrocardiograph provides the care. Situation C: The patient calls the prehospital care service and an ambulance with a doctor and an electrocardiograph provides the care
Decision support systems could also to aid in the diagnosis, management, and prediction of cardiac complications in patients with ACS [56], prehospital bedside ultrasound image transmission, [57] and image transmission and support in the diagnosis and management of patients with stroke [58]. The use of DSS could increase adherence to ACS patient management guidelines recommendations, but evidence on its impact on clinical outcomes is still lacking [58].
Telecardiology on Myocardial Infarction Systems of Care
Myocardial infarction systems of care aim to integrate prehospital, hospital, and hemodynamic services where patients with acute myocardial infarction (AMI) are managed in a given region to optimize their management. This system is proposed to better delineate these patients’ care, involving early diagnosis, prehospital care, initial treatment, thrombolytic use, referral to a specialized hospital and post-event follow-up. It aims for high quality, effective, and safe care for patients with AMI, optimizing resources and reducing disparities in access to care [56, 59].
Telemedicine services play a crucial role in AMI systems of care as they facilitate communication from the physician in a low-complexity emergency unit or hospital and prehospital healthcare professional with cardiologists at a hub or hemodynamic center hospital that will receive the patient. Cardiologists may assist in the following:
-
1.
Analyzing and interpreting the electrocardiogram in order to obtain an accurate and early diagnosis of ST-segment elevation myocardial infarction [54, 60]
-
2.
Guidance on the best management, helping to decide if there is indication of thrombolytic use and other medications by using synchronous teleconsultations [55, 60]
-
3.
Monitoring the patient’s clinical condition through telemonitoring, with synchronous data transmission [60]
In patients submitted to primary PCI, prehospital electrocardiogram, and transmission to PCI center can decrease treatment time, by direct admission of the patient in the catheterization laboratory, bypassing the ER [55].
A typical telemedicine system of care consists of a specialized center (hub) and multiple remote care units distributed within a geographic region (spoke centers), connected bidirectionally with the help of a communication channel (Fig. 24.4). The specialized center can be a cardiology referral hospital, an ambulance regulation service, or a telemedicine center. Some AMI systems of care are comprised of more than one specialized center, each with certain remote units with regional coverage [61].
In recent years, the use of telemedicine tools in AMI has soared worldwide. A recent meta-analysis included studies in Europe (11), North America (8), South America (5), Asia (9), and Australia (2) with 16,960 patients. There was a moderate quality of evidence that the use of telemedicine strategies plus usual care reduces in-hospital mortality by 37% (relative risk [RR] 0.63 [95% CI 0.55–0.72]), with a number needed to treat (NNT) of 29 (confidence interval [CI] 95% 23–40), when compared to usual care without telemedicine. This analysis also showed poor quality of evidence that this intervention reduces door-to-balloon time (mean difference 28 (95% CI −35, −20) minutes), 30-day mortality (RR 0.62 [95% CI 0.43–0.85]) as well as long-term mortality (RR 0.61 [95% CI 0.40–0.92]) [55].
Management of Oral Anticoagulant Users
Self-management strategies have been associated with a significantly lower risk of ischemic stroke compared with treatment with direct oral anticoagulants, while no significant differences were observed for major bleeding or mortality. However, decreased vigilance is a potential problem in detecting patients who are unable to take care of their treatment. A structured education program is required for all stakeholders (patients, their caregivers, and healthcare professionals), as well as an increased quality control system [62,63,64].
Cardiac Rehabilitation
Guidelines recommend cardiac rehabilitation for patients after myocardial infarction, percutaneous coronary intervention (PCI), or coronary artery bypass graft (CABG) surgery. However, it is still underused, with only 14–31% of participants among all eligible patients. Difficulties in patient access to attend face-to-face sessions and high costs are important barriers [65]. In this sense, telehealth interventions using information and communication technologies to enable remote rehabilitation programs can overcome barriers to access while preserving clinical supervision and individualized exercise prescription [66].
In a systematic review that included 11 studies, the type of intervention proposed was highly variable and included the use of mobile or desktop applications, biosensors, and interventions using fixed-line phone calls. The interventions involved prescription and/or performance monitoring and adherence. All interventions included feedback, education, psychosocial support, and/or change behavior via fixed-line phone calls, mobile messaging, email, website, online tutorials, or online chat [67].
It was observed that the level of physical activity was higher in the intervention group compared to usual care. As for face-to-face rehabilitation, telehealth interventions were more effective for physical activity improvement, exercise adherence, in lowering diastolic blood pressure and LDL-c levels, with low to moderate quality of evidence. The telehealth rehabilitation was similar to face-to-face rehabilitation with regards to aerobic exercise levels and other modifiable cardiovascular risk factors [67].
The Telehab III study was a prospective multicenter randomized controlled clinical trial with cardiac rehabilitation patients. There were 140 patients randomly allocated to a 24-week tele-rehabilitation together with usual rehabilitation group and a usual rehabilitation group only. The additional intervention which involved tele-rehabilitation contributed even further to improvements in physical activity and quality of life and may induce persistent health benefits [68].
In a Chinese clinical trial, 98 NYHA classes I to III HF patients were randomized to either a home exercise training program via teleconsultation for 8 weeks or usual outpatient follow-up. Significant statistically improvements were observed in the experimental group regarding quality of life and 6-minute test compared to the control group. The results corroborate that physical training programs via teleconsultation is an effective alternative method for cardiac rehabilitation [69].
The REMOTE-CR is a non-inferiority randomized controlled trial which tested costs and effects of a real-time teleconsultation cardiac rehabilitation in 162 HF patients and demonstrated that it is a cost-effective alternative to increase the scope of rehabilitation [70].
Home cardiac rehabilitation may be an alternative to increase patient engagement in the program by offering greater flexibility and options for activities. Therefore, it is a reasonable choice which can suit the patient’s values and preferences, and can be implemented in their daily routine [71]. The association of tele-rehabilitation with conventional rehabilitation was more effective and efficient when compared to the conventional rehabilitation program only, promoting a reduction in readmissions rate due to cardiovascular causes and increasing quality of life [68, 72].
Remote Monitoring Using Implantable Devices
Pacemaker telemonitoring showed no significant improvement in the quality of life and number of cardiovascular events; however, events were detected and treated earlier, thus reducing hospitalization and hospital visits (routine and emergency). Moreover, it was cheaper than the in-hospital follow-up [73].
Another form of implantable monitoring can be performed using implantable cardiac defibrillators (ICDs) or resynchronization devices. Some of these devices may have multiparameter monitoring software such as thoracic impedance and right ventricular filling pressure measurements captured by the electrode on the right ventricle. A groundbreaking 2008 study suggested that the use of such devices had clinical benefit in 92 NYHA class III patients [74]. Later, the IN-TIME study tested a similar strategy using multiparameter monitoring devices (ICDs and resynchronization devices). In this study, the parameters studied were events such as ventricular and atrial tachyarrhythmia, a low percentage of biventricular pacing, increased frequency of ventricular premature beats, decreased patient activity, and intracardiac electrogram abnormalities. If these parameters had any abnormalities, the system triggered phone calls to a specific contact. The group allocated for remote monitoring showed a significant reduction in combined clinical outcome and total mortality [75].
Other similar studies also demonstrated a reduction in combined clinical outcomes, often related to a decreased need for face-to-face visits [76]. Results from an unselected population cohort study also indicate benefits of using information obtained from remote monitoring with ICD/cardiac resynchronization therapy (CRT) on mortality [77]. However, a meta-analysis with 11 randomized trials evaluating 5703 patients showed no consistent results on clinical outcomes. In this meta-analysis, telemonitoring devices were associated with a reduction in the total number of visits (planned, unplanned, and ER) (RR 0.56; 95% CI 0.43–0.73, P < 0.001); however, hospitalization rates from cardiac causes (RR 0.96; 95% CI 0.82–1.12, P = 0.60) and the composite endpoints of ER, unplanned hospital visits, or hospitalizations (RR 0.99; 95% CI 0.68–1.43, P = 0.96) was similar between the groups. Total and cardiac mortality were also similar between groups [78].
Telecardiology Monitoring and Management
Cost and quality in a telecardiology service are strictly related to the monitoring and management of the process. To have adequate control of cost and quality it is necessary to establish the management framework based on Key Performance Indicators (KPI). Monitoring KPI variations, corrective actions are taken to reach the established goals.
There are two types of KPIs: those related to the final goals or objectives of the whole process (high-level KPIs) and those related to the subprocesses or activities necessary to achieve those goals (low-level KPIs). Initially, high-level indicators and respective goals must be defined based on the objective to be reached. In a second step, those KPIs are deployed according to the subprocesses to have control of every step along the main process. The deployment level has to compromise monitoring cost and amount of information: A very deep deployment results in detailed information but has a high monitoring cost.
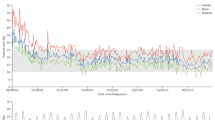
To demonstrate the use of KPIs in telecardiology, it will be considered as an example a Tele-Electrocardiogram Service: ECG signal is collected in remote sites and sent to a diagnostic center to be analyzed by a cardiologist. Then a diagnostic report is sent back to requesting doctor. The main objective of such service is to produce a precise diagnostic report rapidly at low cost. The subprocesses involved to reach such objectives are ECG data collection and transfer, medical analysis, and report delivery. Based on these premises it is possible to establish the high-level KPIs and to deploy them in subprocess KPIs.
High-Level KPIs for a Tele-ECG Service
Based on the main objective of the tele-ECG service to produce a precise diagnostic report rapidly at low cost, it is possible to establish the following KPIs:
-
1.
Production: The number of diagnostic reports made in a specific time interval, usually by month, and the accumulated number of reports. These KPI allows evaluation of the acceptance of the service and to scale future needs of labor and infrastructure.
-
2.
Response time: Defined as the time interval between the ECG data, it is introduced in the system and the diagnostic report is available to the requesting doctor. To reduce this KPI it is necessary to control each time step between these two events.
-
3.
Report precision: This KPI depends on how precision evaluation is measured. In a specific quality control system, different cardiologists reevaluate a predetermined number of reports. The percentage of discordances can be used as KPI precision measurement.
-
4.
Unitary report cost: Corresponds to the total expenditure in a specific time interval, usually in a month, divided by the total number of reports produced in the same time interval. A precise control of this KPI requires its deployment in each type of cost and activity. This KPI is usually compared to the savings concerning the face-to-face exam cost.
Deployment of High-Level KPIs for a Tele-ECG Service (Low-Level KPIs)
Once the high-level KPIs and their goals are established, it is necessary to obtain more detailed information regarding the subprocesses leading to main goals. The deployment of those high-level KPIs has to consider the following factors affecting the KPI:
-
1.
Production: Depends on the number of remote sites implemented and the number of exams per site. The deployment of this KPI results in the following KPIs, for example:
-
a.
Percentage of service coverage defined as the number of implemented sites divided by the number of viable sites in a geographic area to be implemented
-
b.
The number of exams per site
-
c.
Percentage of service utilization defined as the number of sites using the service divided by the number of implemented sites
-
a.
-
2.
Response Time: The response time depends on the following subprocess time KPIs:
-
a.
Sending time defined as time interval between EGC data sent by remote site and acceptance by the system (it measures the quality of Internet infrastructure)
-
b.
Waiting time for report defined as the time interval between ECG data acceptance by the system and ECG data file opening by the cardiologist
-
c.
Report time corresponding to the time between data file opening and report availability
-
d.
Visualization time by the requesting doctor after report availability
-
a.
-
3.
Report precision: The quality of the report mainly depends on the cardiologist and the report time. Consequently, the KPI percent of discordances can be deployed:
-
a.
Percent of discordances by cardiologist
-
b.
Percent of discordances by report time (usually those below a specific report time)
-
a.
-
4.
Unitary report cost: Cost has different sources such as labor, equipment maintenance, utilities, depreciation, etc. The unitary report cost KPI can be deployed as:
-
a.
Unitary labor cost
-
b.
Unitary maintenance cost and etc.
-
a.
These different categories permit to implement a cost follow-up to find the reason of cost increase or reduction in order to implement corrective actions to reduce cost or to implement good practices in case of cost reduction.
Splitting fixed and variable cost KPIs
-
c.
Unitary fixed cost
-
d.
Unitary variable cost
allow to evaluate cost fluctuations due to exam demand variation.
Some of these KPIs, in a specific situation, demand a deeper deployment. For instance, a long waiting time for report can be caused by mismatch between demand and report production. In this case, deploying this KPI in an hourly demand KPI and comparing it to the hourly report production KPI, permit to adjust doctor’s availability to exam demand.
In summary, KPIs are an important tool for management of any process and for a Tele ECG Service it would not be different, as it has been demonstrated by actual application of this method by the authors. Monthly, sometimes weekly or daily, follow-up of the KPIs results a strict control of the service, allowing correction of eventual deviations from established goals. Similarly, the method can be applied to other telecardiology applications.
References
Bashshur RL, Howell JD, Krupinski EA, Harms KM, Bashshur N, Doarn CR. The empirical foundations of telemedicine interventions in primary care. Telemed e-Health. 2016;22(5):342–75.
McKinstry B, Hanley J, Wild S, Pagliari C, Paterson M, Lewis S, et al. Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial. BMJ. 2013;346:f3030.
McManus RJ, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376(9736):163–72.
Nilsson M, Rasmark U, Nordgren H, Hallberg P, Skönevik J, Westman G, et al. The physician at a distance: the use of videoconferencing in the treatment of patients with hypertension. J Telemed Telecare. 2009;15(8):397–403.
Park M-J, Kim H-S, Kim K-S. Cellular phone and internet-based individual intervention on blood pressure and obesity in obese patients with hypertension. Int J Med Inform. 2009;78(10):704–10.
Charpentier G, Benhamou P-Y, Dardari D, Clergeot A, Franc S, Schaepelynck-Belicar P, et al. The Diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves HbA1c in poorly controlled type 1 diabetic patients: a 6-month, randomized, open-label, parallel-group, multicenter trial (TeleDiab 1 Study). Diabetes Care. 2011;34(3):533–9.
Marcolino MS, Maia JX, Alkmim MBM, Boersma E, Ribeiro AL. Telemedicine application in the care of diabetes patients: systematic review and meta-analysis. PLoS One. 2013;8(11):e79246.
Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care. 2009;32(2):234–9.
Goulis D, Giaglis G, Boren S, Lekka I, Bontis E, Balas EA, et al. Effectiveness of home-centered care through telemedicine applications for overweight and obese patients: a randomized controlled trial. Int J Obes. 2004;28(11):1391.
Rodriguez-Idigoras MI, Sepulveda-Munoz J, Sanchez-Garrido-Escudero R, Martinez-Gonzalez JL, Escolar-Castelló JL, Paniagua-Gomez IM, et al. Telemedicine influence on the follow-up of type 2 diabetes patients. Diabetes Technol Ther. 2009;11(7):431–7.
Appel LJ, Clark JM, Yeh H-C, Wang N-Y, Coughlin JW, Daumit G, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365(21):1959–68.
Muñiz J, Gómez-Doblas JJ, Santiago-Pérez MI, Lekuona-Goya I, Murga-Eizagaetxebarría N, Cruz-Fernández JM, et al. The effect of post-discharge educational intervention on patients in achieving objectives in modifiable risk factors six months after discharge following an episode of acute coronary syndrome,(CAM-2 Project): a randomized controlled trial. Health Qual Life Outcomes. 2010;8(1):137.
Gusmão LL, Ribeiro AL, Souza-Silva MVR, Gomes PR, Beleigoli AM, Cardoso CS, et al. Implementation of a text message intervention to promote behavioural change and weight loss among overweight and obese Brazilian primary care patients. J Telemed Telecare. 2018;25(8):476–83.
Marcolino MS, Oliveira JAQ, D’Agostino M, Ribeiro AL, Alkmim MBM, Novillo-Ortiz D. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018;6(1):e23.
Chow CK, Redfern J, Hillis GS, Thakkar J, Santo K, Hackett ML, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314(12):1255–63.
Thangada ND, Garg N, Pandey A, Kumar N. The emerging role of mobile-health applications in the management of hypertension. Curr Cardiol Rep. 2018;20(9):78.
McConnell MV, Turakhia MP, Harrington RA, King AC, Ashley EA. Mobile health advances in physical activity, fitness, and atrial fibrillation: moving hearts. J Am Coll Cardiol. 2018;71(23):2691–701.
Kumari P, Mathew L, Syal P. Increasing trend of wearables and multimodal interface for human activity monitoring: a review. Biosens Bioelectron. 2017;90:298–307.
Riffenburg KM, Spartano NL. Physical activity and weight maintenance: the utility of wearable devices and mobile health technology in research and clinical settings. Curr Opin Endocrinol Diabetes Obes. 2018;25(5):310–4.
Hopkins D. Community preventive services task F. clinical decision support systems recommended to prevent cardiovascular disease. Am J Prev Med. 2015;49(5):796–9.
Njie GJ, Proia KK, Thota AB, Finnie RK, Hopkins DP, Banks SM, et al. Clinical decision support systems and prevention: a community guide cardiovascular disease systematic review. Am J Prev Med. 2015;49(5):784–95.
Roumie CL, Elasy TA, Greevy R, Griffin MR, Liu X, Stone WJ, et al. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med. 2006;145(3):165–75.
Nerlich M, Balas EA, Schall T, Stieglitz S-P, Filzmaier R, Asbach P, et al. Teleconsultation practice guidelines: report from G8 global health applications subproject 4. Telemed J E Health. 2002;8(4):411–8.
Marcolino MS, Alkmim MB, Pessoa CG, Maia JX, Cardoso CS. Development and implementation of a methodology for quality assessment of asynchronous teleconsultations. Telemed e-Health. 2019;26(5):651–8.
Liddy C, Moroz I, Mihan A, Nawar N, Keely E. A systematic review of asynchronous, provider-to-provider, electronic consultation services to improve access to specialty care available worldwide. Telemed J e-Health. 2019;25(3):184–98.
Thijssing L, Tensen E, Jaspers MW, editors. Patient’s perspective on quality of teleconsultation services. MIE; 2016.
Petcu R, Kimble C, Ologeanu-Taddei R, Bourdon I, Giraudeau N. Assessing patient’s perception of oral teleconsultation. Int J Technol Assess Health Care. 2017;33(2):147–54.
Soriano Marcolino M, Minelli Figueira R, Pereira Afonso dos Santos J, Silva Cardoso C, Luiz Ribeiro A, Alkmim MB. The experience of a sustainable large-scale Brazilian telehealth network. Telemed e-Health. 2016;22(11):899–908.
Benjamin A. Audit: how to do it in practice. BMJ. 2008;336(7655):1241–5.
Olayiwola JN, Anderson D, Jepeal N, Aseltine R, Pickett C, Yan J, et al. Electronic consultations to improve the primary care-specialty care interface for cardiology in the medically underserved: a cluster-randomized controlled trial. Ann Family Med. 2016;14(2):133–40.
Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed Telecare. 2016;22(8):504–12.
Maeyama MA, Calvo MCM. A Integração do Telessaúde nas Centrais de Regulação: a Teleconsultoria como Mediadora entre a Atenção Básica e a Atenção Especializada. Revista Brasileira de Educação Médica. 2018;42(2):63–72.
Pfeil JN. Avaliação da regulação de consultas médicas especializadas baseada em Protocolo+ Teleconsultoria. 2018.
Ribeiro ALP, Alkmim MB, Cardoso CS, Carvalho GGR, Caiaffa WT, Andrade MV, et al. Implementation of a telecardiology system in the state of Minas Gerais: the Minas Telecardio Project. Arq Bras Cardiol. 2010;95(1):70–8.
Sparenberg A, Russomano T, de Azevedo D, editors. Transmission of digital electrocardiogram (ECG) via modem connection in Southern Brazil. The 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2004: IEEE.
Singh S, Bansal M, Maheshwari P, Adams D, Sengupta SP, Price R, et al. American society of echocardiography: remote echocardiography with web-based assessments for referrals at a distance (ASE-REWARD) study. J Am Soc Echocardiogr. 2013;26(3):221–33.
d’Arcy JL, Coffey S, Loudon MA, Kennedy A, Pearson-Stuttard J, Birks J, et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study. Eur Heart J. 2016;37(47):3515–22.
Lopes EL, Beaton AZ, Nascimento BR, Tompsett A, Dos Santos JP, Perlman L, et al. Telehealth solutions to enable global collaboration in rheumatic heart disease screening. J Telemed Telecare. 2018;24(2):101–9.
Nascimento BR, Sable C, Nunes MCP, Diamantino AC, Oliveira KK, Oliveira CM, et al. Comparison between different strategies of rheumatic heart disease echocardiographic screening in Brazil: data from the PROVAR (Rheumatic Valve Disease Screening Program) study. J Am Heart Assoc. 2018;7(4):e008039.
Nascimento BR, Beaton AZ, Nunes MCP, Diamantino AC, Carmo GA, Oliveira KK, et al. Echocardiographic prevalence of rheumatic heart disease in Brazilian schoolchildren: data from the PROVAR study. Int J Cardiol. 2016;219:439–45.
Gensini GF, Alderighi C, Rasoini R, Mazzanti M, Casolo G. Value of telemonitoring and telemedicine in heart failure management. Card Fail Rev. 2017;3(2):116.
Bashi N, Karunanithi M, Fatehi F, Ding H, Walters D. Remote monitoring of patients with heart failure: an overview of systematic reviews. J Med Internet Res. 2017;19(1):e18.
Yun JE, Park J-E, Park H-Y, Lee H-Y, Park D-A. Comparative effectiveness of telemonitoring versus usual care for heart failure: a systematic review and meta-analysis. J Card Fail. 2018;24(1):19–28.
Fraiche AM, Eapen ZJ, McClellan MB. Moving beyond the walls of the clinic: opportunities and challenges to the future of telehealth in heart failure. JACC: Heart Failure. 2017;5(4):297–304.
Inglis SC, Clark RA, Dierckx R, Prieto-Merino D, Cleland JG. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst Rev. 2015;103(4) https://doi.org/10.1136/heartjnl-2015-309191.
Pekmezaris RTL, Williams M, Patel V, Makaryus A, Zeltser R, et al. Home telemonitoring in heart failure: a systematic review and metaanalysis. Health Affairs (Millwood). 2018;37(12):1983–9.
Koehler F, Koehler K, Deckwart O, Prescher S, Wegscheider K, Kirwan BA, et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392(10152):1047–57.
Abraham WT, Adamson PB, Bourge RC, Aaron MF, Costanzo MR, Stevenson LW, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet. 2011;377(9766):658–66.
Abraham WT, Stevenson LW, Bourge RC, Lindenfeld JA, Bauman JG, Adamson PB. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: complete follow-up results from the CHAMPION randomised trial. Lancet. 2016;387(10017):453–61.
Margolis KL, Asche SE, Dehmer SP, Bergdall AR, Green BB, Sperl-Hillen JM, et al. Long-term outcomes of the effects of home blood pressure telemonitoring and pharmacist management on blood pressure among adults with uncontrolled hypertension: follow-up of a cluster randomized clinical trial. JAMA Netw Open. 2018;1(5):e181617.
Wald DS, Bestwick JP, Raiman L, Brendell R, Wald NJ. Randomised trial of text messaging on adherence to cardiovascular preventive treatment (INTERACT trial). PLoS One. 2014;9(12):e114268.
McManus RJ, Mant J, Franssen M, Nickless A, Schwartz C, Hodgkinson J, et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. 2018;391(10124):949–59.
Monahan M, Jowett S, Nickless A, Franssen M, Grant S, Greenfield S, et al. Cost-effectiveness of telemonitoring and self-monitoring of blood pressure for antihypertensive titration in primary care (TASMINH4). Hypertension. 2019;73(6):1231–9.
Palmer MJ, Barnard S, Perel P, Free C. Mobile phone-based interventions for improving adherence to medication prescribed for the primary prevention of cardiovascular disease in adults. Cochrane Database Syst Rev. 2018;6:CD012675.
Marcolino MS, Maia LM, Oliveira JAQ, Melo LDR, Pereira BLD, Andrade-Junior DF, et al. Impact of telemedicine interventions on mortality in patients with acute myocardial infarction: a systematic review and meta-analysis. Heart. 2019;105(19):1479–86.
Oliveira Junior MT, Canesin MF, Marcolino MS, Ribeiro AL, Carvalho AC, Reddy S, et al. Telemedicine guideline in Patient Care with Acute Coronary Syndrome and Other heart Diseases. Arq Bras Cardiol. 2015;104(5 Suppl 1):1–26.
DeBusk RF, Miller NH, Raby L. Technical feasibility of an online decision support system for acute coronary syndromes. Circ Cardiovasc Qual Outcomes. 2010;3(6):694–700.
Nelson BP, Chason K. Use of ultrasound by emergency medical services: a review. Int J Emerg Med. 2008;1(4):253–9.
Wechsler LR, Demaerschalk BM, Schwamm LH, Adeoye OM, Audebert HJ, Fanale CV, et al. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48(1):e3–e25.
Nascimento BR, Brant LCC, Marino BCA, Passaglia LG, Ribeiro ALP. Implementing myocardial infarction systems of care in low/middle-income countries. Heart. 2019;105(1):20–6.
Filgueiras Filho NM, Feitosa Filho GS, Solla DJF, Argolo FC, Guimaraes PO, Paiva Filho IM, et al. Implementation of a regional network for ST-segment-elevation myocardial infarction (STEMI) care and 30-day mortality in a low- to middle-Income City in Brazil: findings from Salvador’s STEMI Registry (RESISST). J Am Heart Assoc. 2018;7(14):e008624.
Brasen CL, Madsen JS, Parkner T, Brandslund I. Home management of warfarin treatment through a real-time supervised telemedicine solution: a randomized controlled trial. Telemed J e-Health. 2019;25(2):109–15.
Pozzi M, Mitchell J, Henaine AM, Hanna N, Safi O, Henaine R. International normalized ratio self-testing and self-management: improving patient outcomes. Vasc Health Risk Manag. 2016;12:387–92.
Heneghan CJ, Garcia-Alamino JM, Spencer EA, Ward AM, Perera R, Bankhead C, et al. Self-monitoring and self-management of oral anticoagulation. Cochrane Database Syst Rev. 2016;7:CD003839.
Saia M, Mantoan D, Fonzo M, Bertoncello C, Soattin M, Sperotto M, et al. Impact of the regional network for AMI in the management of STEMI on care processes, outcomes and health inequities in the Veneto region, Italy. Int J Environ Res Public Health. 2018;15(9):1980.
Beatty AL, Fukuoka Y, Whooley MA. Using mobile technology for cardiac rehabilitation: a review and framework for development and evaluation. J Am Heart Assoc. 2013;2(6):e000568.
Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;102(15):1183–92.
Frederix I, Hansen D, Coninx K, Vandervoort P, Vandijck D, Hens N, et al. Medium-term effectiveness of a comprehensive internet-based and patient-specific Telerehabilitation program with text messaging support for cardiac patients: randomized controlled trial. J Med Internet Res. 2015;17(7):e185.
Peng X, Su Y, Hu Z, Sun X, Li X, Dolansky MA, et al. Home-based telehealth exercise training program in Chinese patients with heart failure: a randomized controlled trial. Medicine. 2018;97(35):e12069.
Maddison R, Rawstorn JC, Stewart RAH, Benatar J, Whittaker R, Rolleston A, et al. Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart. 2019;105(2):122–9.
Taylor RS, Dalal H, Jolly K, Moxham T, Zawada A. Home-based versus Centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2010;(1):CD007130.
Frederix I, Hansen D, Coninx K, Vandervoort P, Vandijck D, Hens N, et al. Effect of comprehensive cardiac telerehabilitation on one-year cardiovascular rehospitalization rate, medical costs and quality of life: a cost-effectiveness analysis. Eur J Prev Cardiol. 2016;23(7):674–82.
Lopez-Villegas A, Catalan-Matamoros D, Martin-Saborido C, Villegas-Tripiana I, Robles-Musso E. A systematic review of economic evaluations of pacemaker Telemonitoring systems. Rev Esp Cardiol. 2016;69(2):125–33.
Bourge RC, Abraham WT, Adamson PB, Aaron MF, Aranda JM Jr, Magalski A, et al. Randomized controlled trial of an implantable continuous hemodynamic monitor in patients with advanced heart failure: the COMPASS-HF study. J Am Coll Cardiol. 2008;51(11):1073–9.
Hindricks G, Taborsky M, Glikson M, Heinrich U, Schumacher B, Katz A, et al. Implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME): a randomised controlled trial. Lancet. 2014;384(9943):583–90.
De Simone A, Leoni L, Luzi M, Amellone C, Stabile G, La Rocca V, et al. Remote monitoring improves outcome after ICD implantation: the clinical efficacy in the management of heart failure (EFFECT) study. Europace. 2015;17(8):1267–75.
Kurek A, Tajstra M, Gadula-Gacek E, Buchta P, Skrzypek M, Pyka L, et al. Impact of remote monitoring on long-term prognosis in heart failure patients in a real-world cohort: results from all-comers COMMIT-HF trial. J Cardiovasc Electrophysiol. 2017;28(4):425–31.
Klersy C, Boriani G, De Silvestri A, Mairesse GH, Braunschweig F, Scotti V, et al. Effect of telemonitoring of cardiac implantable electronic devices on healthcare utilization: a meta-analysis of randomized controlled trials in patients with heart failure. Eur J Heart Fail. 2016;18(2):195–204.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Marcolino, M.S. et al. (2021). Telecardiology. In: Latifi, R., Doarn, C.R., Merrell, R.C. (eds) Telemedicine, Telehealth and Telepresence. Springer, Cham. https://doi.org/10.1007/978-3-030-56917-4_24
Download citation
DOI: https://doi.org/10.1007/978-3-030-56917-4_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-56916-7
Online ISBN: 978-3-030-56917-4
eBook Packages: MedicineMedicine (R0)