Abstract
Introduction
Endoscopic dilation is the preferred management strategy for caustic esophageal strictures (CES). However, the differences in outcome for different dilators are not clear. We compared the outcome of CES using bougie and balloon dilators.
Methods
Between January 2000 and December 2016, the following data of all the patients with CES were collected: demographic parameters, substance ingestion, number of strictures, number of dilations required to achieve ≥ 14 mm dilation, post-dilation recurrence, and total dilations. Patients were divided into two groups for the type of dilator, i.e., bougie or balloon. The two groups were compared for baseline parameter, technical success, short- and long-term clinical success, refractory strictures, recurrence rates, and major complications.
Results
Of the 189 patients (mean age 32.17 ± 12.12 years) studied, 119 (62.9%) were males. 122 (64.5%) patients underwent bougie dilation and 67 (35.5%) received balloon dilation. Technical success (90.1% vs. 68.7%, p < 0.001), short-term clinical success (65.6% vs. 46.3%, p value 0.01), and long-term clinical success (86.9% vs. 64.2%, p < 0.01) were higher for bougie dilators compared to balloon dilators. Twenty-four (12.7%) patients developed adverse events which were similar for two groups. On multivariate analysis, use of bougie dilators (aOR 4.868, 95% CI 1.027–23.079), short-term clinical success (aOR 5.785, 95% CI 1.203–27.825), and refractory strictures (aOR 0.151, 95% CI 0.033–0.690) were independent predictors of long-term clinical success.
Conclusion
Use of bougie dilators is associated with better clinical success in patients with CES compared to balloon dilators with similar rates of adverse events.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Caustic ingestion is a major public health problem throughout the world, especially in the developing countries [1,2,3]. While the incidence of caustic ingestion in the western world is declining, data from the developing countries are still scarce [3]. Initial management includes resuscitation and nutritional support. Early esophagogastroduodenoscopy (EGD), within 24 to 48 h of ingestion, has been an important measure to assess the extent and severity of mucosal injury [4, 5]. Endoscopic grading of injury helps in triaging the patients for early discharge as well as predicting the development of long-term complication of cicatrisation [4].
Various strategies are suggested to prevent stricture formation including systemic corticosteroids, proton pump inhibitors, nasoduodenal tube placement, endoluminal stenting, or early bougie dilation [6,7,8,9]. However, none of these are unequivocal in preventing stricture formation. Symptomatic esophageal stricture develops in 70–100% of the patients with high-grade injury, i.e., Zargar grade 2b and 3 [4]. Stricture formation is a late sequela of caustic injury and develops after 2 to 3 weeks of ingestion [10]. Strictures once formed are either subjected to endoscopic dilation or undergo surgical resection or bypass. Endoscopic dilation is the initial preferred strategy for such strictures. The clinical success of endoscopic dilation varies from 46 to 100% [11,12,13,14]. These differences in successful outcome are partially accounted for by the different timing of starting of dilation, use of different dilators (bougie or balloon), different intervals between successive dilations, use of adjunctive local therapies, and different definitions of end-points.
Use of specific dilators for stricture dilation depends on the complexity of stricture as well as operators’ preference. Early studies had used bougie dilators while most endoscopists in recent times prefer through-the-scope balloon dilators for stricture dilation. However, no comparative data are available for the efficacy of these dilators in caustic esophageal strictures (CES). Therefore, the present study was aimed at analyzing our data for patients with CES to compare the efficacy and safety of bougie and balloon dilators.
Methods
This study was a retrospective analysis of prospectively collected data of patients with CES between January 2000 and December 2016. The study was approved by the institute’s ethics committee. The study population included all the patients with esophageal strictures who fulfilled the following criteria: (a) esophageal stricture documented on endoscopy and esophagography, (b) esophageal stricture secondary to caustic injury, with or without gastric involvement, and (c) strictures dilated with either bougie or through-the-scope (TTS) balloon dilators, but not both. Excluded were patients with strictures ≥ 6 cm in length, patients with concomitant cicatrized stomach with inadequate gastric capacity precluding endoscopic assessment and dilation, incomplete clinical details, history of prior endoscopic dilation or surgical intervention for CES, or directly referred to surgery for CES management.
Data collection
Clinical data were collected including demographic profile, type of caustic substance ingested, intention of ingestion, as well as time elapsed before presentation. Number of esophageal strictures and presence of gastric strictures were also recorded. Esophageal strictures were either dilated with Savary Gilliard (SG) bougie dilators (Cook Medical Inc., Winston Salem, NC, USA) or through-the-scope balloon (Controlled Radial Expansion, CRE, Boston Scientific Corp, Marlborough, MA USA) dilators. We used esophageal fixed wire-guided TTS CRE balloons (Boston Scientific Corp, Marlborough, MA USA) for stricture dilation. Length of the balloon was 8 cm and diameter was variable from 6 to 15 mm. When fluoroscopy was required for strictures which were not easily negotiable with a balloon, wire-guided TTS CRE balloons (balloon length 5.5 cm and diameter 6–15 mm) from the same manufacturer were used. Data collected for dilation included starting and ending diameter of first dilation, number of dilations required to achieve ≥ 14 mm dilation, post-dilation recurrence, and total number of dilations.
All the included patients were categorized into two groups based on the type of dilator used. Group 1 consisted of patients who were dilated with SG bougie dilators and Group 2 included those who underwent dilation using TTS balloon dilators. The two groups were compared for baseline parameters including age, gender, months elapsed after ingestion, and number of CES.
Outcomes
Outcome parameters compared were technical success, short- and long-term clinical success, mean number of dilations required to achieve technical (diameter ≥ 14 m) success, total number of dilations, proportion of refractory strictures, recurrence rates after short-term clinical success and major complicate rates.
Dilation technique
Dilations were performed using SG bougie or TTS balloon dilators by one of the two expert endoscopists (RK and SKS). All the dilations were performed after an informed consent under conscious sedation using intravenous midazolam (0.025–0.1 mg/kg, Fulsed, Ranbaxy, Mumbai, India) and tramadol (50–100 mg, Contramal, Abbott India Limited, Mumbai, India). Prior to starting dilation, a detailed contrast study using barium sulfate (100% weight/volume) was done to look for the length, severity, and complexity of the strictures. Prior to 2005, all the CES were dilated with bougie dilators. After the availability of new generation TTS balloon dilators, the use of bougie or balloon dilator was decided by the complexity of strictures, residual gastric capacity to allow bougie dilators, and the operator’s preference. Balloon dilators were preferred when distal anatomy beyond the stricture was not clear, stomach capacity was significantly reduced, or multiple esophageal strictures with variable luminal diameters were present. Bougie dilators were preferred when the stricture was single but angulated, when patients had multiple strictures with comparable luminal diameter and adequate stomach capacity to accommodate the tapered end of bougie dilator.
For bougie dilation, a steel guidewire with spring tip was placed across the esophageal stricture under endoscopic guidance. Over the guidewire, the chosen bougie was passed at least 5–10 cm beyond the stricture, excluding the tapered end. For balloon dilation, the TTS balloon was passed across the stricture under endoscopic vision. Balloon was positioned in a way that stricture lay between the ends of the balloon. Balloon was inflated using water with the Alliance inflation device (Boston Scientific Corp, Marlborough, MA, USA). Balloon was kept inflated at each diameter for 1 min. Pressures for dilation were as per the manufacturer’s instructions. Fluoroscopy was used for difficult strictures, when the spring tip guidewire or the balloon dilator would not pass freely across the stricture. In multiple and tortuous strictures, wire-guided balloons were preferred. The size of the initial dilator used was determined by the diameter of stricture on a contrast radiograph. In patients with associated symptomatic gastric cicatrization, gastric dilation was started once esophageal stricture was dilated till 12 mm and endoscope was negotiable into the stomach. Gastric strictures were dilated with TTS wire-guided balloon dilators, irrespective of the type of dilator used for esophageal strictures. Esophageal dilations were performed at 2–3 weekly intervals with an aim to achieve dilation of ≥ 14 mm.
Adjunctive treatment included the use of triamcinolone or mitomycin as described earlier at the stricture site [15], or self-expanding plastic stents (SEPS) or self-expanding metallic stent (SEMS) placement for refractory esophageal strictures. The timing and type of adjunctive treatment for the refractory stricture was as per the endoscopist’s preference.
After each session of stricture dilation, patients were observed for 4–6 h for any warning symptoms or signs (severe persistent chest pain, dyspnea, hemodynamic instability,.and subcutaneous emphysema over neck/chest). If a patient had any warning symptoms or signs during the observation period or when the endoscopist had clinical suspicion of perforation during dilation, a contrast-enhanced computed tomography (CT) with oral contrast was performed. When the dilation was uneventful and no warning symptoms or signs were observed, patients were discharged after 6 h with instruction to report to emergency when required.
Definitions
Technical success was defined as the ability to achieve a diameter of ≥ 14 mm [16,17,18,19]. Clinical success was identified as short- and long-term clinical success. Short-term clinical success was defined as the absence of dysphagia at 1 month after achieving a diameter of ≥ 14 mm. Long-term clinical success was defined as the ability to maintain normal weight with ability to swallow solid without requiring further dilation for 12 months after the last dilation. A refractory stricture was defined as failure to achieve successful dilation up to a 14-mm diameter after five sessions performed every 2–3 weeks [20]. Recurrence was defined as occurrence of symptoms with endoscopic evidence of stricture after initial short-term clinical success.
Adverse events were defined as per the American Society of Gastrointestinal Endoscopy (ASGE) definitions [21]. Adverse events were identified as (a) perforation—full thickness breach in esophageal wall continuity after dilation of the stricture, (2) bleeding—post-dilation bleeding in the form of hematemesis and/or melena with a hemoglobin drop of ≥ 2 g/dL, and (3) others adverse events. Other adverse events included any form of complication requiring hospitalization or prolongation of admission by > 24 h or ICU admission. Adverse events were also categorized as early or late. Early adverse events were defined as adverse events which developed before achieving a diameter of ≥ 14 mm while late adverse events developed on re-dilations after achieving a diameter of ≥ 14 mm.
Statistical analysis
All the collected data were entered in the Microsoft Excel 2019 spreadsheet and SPSS version 28.0.1.1 (IBM, Armonk, New York, USA) was used to analyze the data. Continuous variables were presented as mean (standard deviation, SD) or median (interquartile range, IQR) and proportions were expressed as percentages. The means among the two groups were compared using independent sample t test for normally distributed variables and Mann–Whitney U test for non-normally distributed data. For categorical variables, χ2 test/Fisher exact F test with correction were used. Univariate analysis was done to find significant variables for long-term clinical success. Using significant variables on univariate analysis, multivariate analysis was done to identify predictors of long-term clinical success. The results were presented as unadjusted and adjusted Odds ratios (ORs) with 95% confidence intervals (CIs). A two-sided p value less than 0.05 was considered statistically significant.
Results
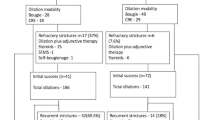
Between January 2000 and December 2016, among 391 patients with CES, 189 patients were included in the present study (Fig. 1). Excluded patients had dilation with both the type of dilators (n = 86), incomplete data or lost to follow-up (n = 64), those who underwent surgery for > 6 cm long stricture (n = 47) and history of previous dilation elsewhere (n = 5). The median duration of presentation after caustic ingestion was 3 months (IQR 2–6.3 months). The caustic substance ingested was an acid in 140 (74.1%) patients and an alkali in 26 (13.8%). 23 (13.2%) patients ingested other substances or the nature of caustic was not known. Single esophageal strictures were identified in 137 (72.9%) patients while 52 (26.6%) patients had multiple strictures. Table 1 gives the characteristics of the included patients.
Overall, 155 (82%) patients achieved technical success and 149 (78.8%) achieved long-term clinical success with endoscopic dilation in the present cohort (Figs. 2, 3). 40 (21.2%) patients underwent surgery after failed endoscopic dilation or complications. Indications of surgery were failure to achieve long-term clinical success after endoscopic dilations (n = 26) and post-dilation complications (n = 14).
Patients were divided into two groups based on the type of dilator used for stricture dilation. 122 (64.5%) patients underwent stricture dilation using bougie dilators while 67 (35.5%) underwent TTS balloon dilation. The mean age and gender distribution were comparable among the two groups (Table 2). Patients who underwent balloon dilation had a higher number of multiple esophageal strictures compared to bougie dilators (41.8% vs. 19%, p < 0.01).
Technical and clinical success
Technical success was higher among the patients dilated with bougie dilators than balloon dilators (90.1% vs. 68.7%, p < 0.001). Short-term clinical success was also significantly more with bougie dilators (65.6% vs. 46.3%, p = 0.01). Recurrence of dysphagia after initial short-term clinical success was more with balloon dilators than bougie dilators, however, statistically non-significant (67.7% vs. 56.3%, p = 0.269).
After initial dilation, long-term clinical success was achieved only in 45 (23.8%) patients, which was higher with bougie dilators than balloon dilators (28.7% vs. 14.9%, p = 0.034). 25 patients underwent surgery after failed initial dilation or dilation-related adverse events. The remaining 119 patients underwent re-dilation, 79 in the bougie dilator group and 40 in the balloon dilator group. After subsequent sessions of re-dilation (with or without use of adjunctive therapy), 104 patients of 119 showed long-term clinical improvement in dysphagia. After re-dilation, additional long-term clinical success was similar for both the types of dilators, bougie (71/79, 89.87%) vs. balloon (33/40 82.5%), p = 0.25. Overall, long-term clinical success was more with bougie dilators compared to balloon dilators (86.9% vs. 64.2%, p < 0.01).
Predictors of long-term successful outcome
All the available parameters were assessed for predicting long-term success of endoscopic dilation in CES. Among 189 patients, 149 patients had successful long-term outcome, while 40 patients underwent surgery. On univariate analysis, long-term clinical success group had higher number of single strictures, more technical success and short-term clinical success, higher use of bougie dilators and adjunctive therapy, and a lesser number of refractory strictures compared to failed group (Supplementary Table 1).
Multivariate analysis was done using significant parameters on univariate analysis, to assess the predictors of successful long-term outcome. Use of bougie dilators (OR 5.251, 95% CI 1.155–23.872, aOR 4.868, 95% CI 1.027–23.079) and short-term clinical success (OR 5.517, 95% CI 1.332–22.840, aOR 5.785, 95% CI 1.203–27.825) were independent positive predictors of successful long-term outcome while refractory stricture (OR 0.149, 95% CI 0.034–0.646, aOR 0.151, 95% CI 0.033–0.690) was an independent negative predictor of successful long-term outcome (Table 3).
Adverse events
Twenty-four (12.7%) patients developed adverse events during the endoscopic dilation therapy. Overall, early and late adverse event rates were comparable with both the types of dilators (Table 4). In the present cohort, 21 (11.1%) patients developed esophageal perforation of which nine were managed conservatively and 12 underwent surgery. Among the nine patients of perforation managed conservatively, two underwent clip closure, one required self-expanding metallic stent, while the other six were managed with nil per orally and intravenous antibiotics. All patients managed conservatively were started on esophageal re-dilation after 3–4 weeks.
Other adverse events were massive bleeding in two patients and vasovagal cardiac arrest in one patient. Bleeding developed in both the patients after bougie dilation (with a 14 mm bougie) while cardiac arrest developed in a patient with balloon dilation with a 12 mm balloon. One patient with bleeding was managed conservatively while another required surgery. Patient with vasovagal cardiac arrest was revived and underwent surgery for CES without further sessions of dilation.
Overall, 14 patients underwent surgery for dilation related complications. Of these, one patient developed anastomotic leak post surgery and died secondary to sepsis.
Discussion
In this comparative study, endoscopic stricture dilation of CES showed higher technical success (90.1% vs. 68.7%), short-term (65.6% vs. 46.3%) and long-term clinical success (86.9% vs. 64.2%) with bougie dilators compared to balloon dilators. Recurrence of dysphagia after initial short-term clinical success (67.7% vs. 56.3%) and adverse events were not different for either of the dilators. Multivariate analysis suggested that use of bougie dilators (aOR 4.868, 95% CI 1.027–23.079), achievement of short-term clinical success after initial dilation (aOR 5.785, 95% CI 1.203–27.825), and the presence of refractory stricture (aOR: 0.151, 95% CI 0.033–0.690) were independent predictors of long-term clinical success.
Since caustic strictures are often long, tight, and eccentric with significant wall fibrosis, it makes them more resistant to dilation compared to other strictures. Contrary to the recommended five sessions to achieve a diameter of ≥ 14 mm, these strictures often require more sessions of dilation [12, 22]. Our data support this observation and showed that 35.4% of the esophageal strictures in our cohort were refractory. We found better short- and long-term clinical success with bougie dilators, though their use had more refractory strictures compared to balloon dilators (43.5% vs. 20%, p = 0.005). This may seem contradictory. The number of dilatations to achieve ≥ 14 mmm was also higher and the number of total dilations too, when compared to balloon dilators. Refractory strictures by definition would need more dilations. We feel the reason for a seemingly conflicting result of greater success but more requirement of dilation lies in the fact that bougie dilation allows the endoscopist to ‘feel’ the resistance and limit the diameter of dilation. This does not happen with balloons where, in fact, you tend to dilate to a preconceived diameter. Perhaps that is the reason balloon dilation was associated with a greater incidence of perforation, though not significant. In light of these observations, the use of the term ‘refractory strictures’ seems superfluous since the end point should be success in terms of freedom from dysphagia.
Both bougie and balloon dilators are effective in ameliorating dysphagia in esophageal strictures. A metaanalysis on comparative studies on bougies versus balloons showed that both were equally effective and safe in treating benign esophageal strictures [23]. However, it included only 12 cases of CES. Observational studies on bougie dilation in CES have shown a technical success of 41–100% and clinical success of 25–100% [9, 16, 24,25,26]. With the advancement of TTS balloons in the last two decades, esophageal strictures are increasingly being dilated with balloon dilators. Studies have reported a technical success of 90–100% and clinical success of 46–100% with balloon dilators [11, 13, 27,28,29]. The use of different definitions of technical and clinical success leads to variable success rates. These variable results explain the need for standardized definitions for technical and clinical outcome. We found higher clinical success (short and long term) with bougie dilators. In the presence of complex and eccentric strictures, balloon dilation could cause differential dilation of stricture segments while bougies provide a uniform dilation. Also, in very tight and fibrotic strictures, balloons may not achieve the intended diameter due to compressibility of the balloon. These hypotheses may explain the higher efficacy of bougie dilators compared to balloon dilators, however, the exact cause for poor clinical success with balloon needs further evaluation. Future studies should assess the adequacy of diameter achieved after each dilation for different dilators.
On multivariate logistic regression, we identified the use of bougie dilators, short-term clinic success, and refractory stricture as independent predictors of long-term clinical success. The presence of multiple strictures and time elapsed before presentation had no effect on long-term clinical success. Multiple studies have shown poor clinical outcome for long segment strictures (> 6 cm), cricopharyngeal strictures, multiple strictures and delayed initiation of dilation [14, 24, 30, 31]. In the present study, patients with long segment (> 6 cm) strictures were excluded. We found better outcome with bougie dilators compared to balloon dilators for CES. None of the available studies have compared these dilators for CES. Other parameters found to predict long-term clinical success were short-term clinical success after initial dilation and the presence of refractory strictures. The presence of refractory strictures is a useful and independent parameter to predict poor long-term success. However, refractoriness in CES is an operator-dependent measure and most endoscopists do not use the Kochman’s definition for refractory benign esophageal stricture. Standardized definitions to identify refractory strictures in CES need further studies. Also, the clinical benefit of step-up adjunctive therapies in these refractory strictures is a matter of research.
Stricture dilation is categorized as a high-risk therapeutic procedure [21, 32]. The associated adverse events after dilation include perforation, bleeding, cardiopulmonary adverse events, and other endoscopy or anesthesia-related adverse events [21]. Development of such adverse events are often the cause of treatment failure. In the present study, 12.7% patients developed adverse events and 62.5% of these events occurred during sessions of dilation, i.e., before a stricture diameter of at least 14 mm was achieved. Perforation is the most common adverse event reported after stricture dilation with incidence reported between 0–35% [26, 31,32,33,34]. Perforation developed in 11.1% patients in the present cohort followed by other adverse events, e.g., bleeding (1%) and vasovagal cardiac arrest (0.5%). The adverse events identified in the present study were slightly higher than reported in the recent studies [26, 28]. Factors like ulceration and nutritional status which affect healing and air sufflation, which increases microleaks, affect the adverse event rates. Such confounding factors could not be studied due to unavailability of data and need to be explored in future studies. The death rates after perforation are variable, ranging from 0 to 18% [14, 35]. With early identification of perforation, the mortality has reduced significantly [14, 34]. In the present study, one patient died after esophageal perforation due to persistent sepsis after surgery.
Strengths of our study are that it includes the largest number of esophageal strictures due to caustic ingestion, and long-term longitudinal follow-up at a single center. We used standard definitions for technical and clinical success and refractory strictures. There are, however, a number of limitations in the present study. First, being a retrospective study, data on certain parameters, which could have confounding effects, were either not available or not equally distributed. Also, a significant proportion of patients from the cohort had incomplete data or were lost to follow-up and only patients with complete follow-up were included. This selective nature of study could introduce selection bias. Future randomized studies with long-term follow-up will be required to confirm the results of this study. Second, the length of strictures was assessed non-uniformly by the available data including esophagogram, computed tomography, or on endoscopy. The data on luminal diameter were incomplete and its effect on clinical outcome could not be assessed. Third, balloon dilations were done without fluoroscopy and obliteration of the waist could not be ensured in all cases. Lastly, as a referral center, most patients presented at late stage with delayed initiation of dilation, and underlying malnutrition could have affected the treatment outcome.
In conclusion, the study shows that use of bougie dilators is associated with better clinical success compared to balloon dilators in CES, with similar rates of adverse events.
References
Li Y, Langworthy J, Xu L, Cai H, Yang Y, Lu Y, Wallach SL, Friedenberg FK (2020) Nationwide estimate of emergency department visits in the United States related to caustic ingestion. Dis Esophagus 33(6):doaa012
Pannu AK, Bhalla A, Vamshi V, Upadhyay MK, Sharma N, Kumar S (2022) Changing spectrum of acute poisoning in North India: a hospital-based descriptive study. Turk J Emerg Med 22(4):192–199
Gummin DD, Mowry JB, Spyker DA, Brooks DE, Osterthaler KM, Banner W (2018) 2017 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th annual report. Clin Toxicol 56(12):1213–1415
Zargar SA, Kochhar R, Mehta S, Mehta SK (1991) The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc 37(2):165–169
Temiz A, Oguzkurt P, Ezer SS, Ince E, Hicsonmez A (2012) Predictability of outcome of caustic ingestion by esophagogastroduodenoscopy in children. World J Gastroenterol 18(10):1098–1103
Katibe R, Abdelgadir I, McGrogan P, Akobeng AK (2018) Corticosteroids for preventing caustic esophageal strictures: systematic review and meta-analysis. J Pediatr Gastroenterol Nutr 66(6):898–902
Mahawongkajit P, Tomtitchong P, Boochangkool N, Mingmalairak C, Awsakulsutthi S, Havanond C (2021) A prospective randomized controlled trial of omeprazole for preventing esophageal stricture in grade 2b and 3a corrosive esophageal injuries. Surg Endosc 35(6):2759–2764
Wang RW, Zhou JH, Jiang YG, Fan SZ, Gong TQ, Zhao YP, Tan QY, Lin YD (2006) Prevention of stricture with intraluminal stenting through laparotomy after corrosive esophageal burns. Eur J Cardiothorac Surg 30(2):207–211
Tiryaki T, Livanelioğlu Z, Atayurt H (2005) Early bougienage for relief of stricture formation following caustic esophageal burns. Pediatr Surg Int 21(2):78–80
Bruzzi M, Chirica M, Resche-Rigon M, Corte H, Voron T, Sarfati E, Zagdanski AM, Cattan P (2019) Emergency computed tomography predicts caustic esophageal stricture formation. Ann Surg 270(1):109–114
Kim JH, Song HY, Kim HC, Shin JH, Kim KR, Park SW, Jung HY, Lee GH, Park SI (2008) Corrosive esophageal strictures: long-term effectiveness of balloon dilation in 117 patients. J Vasc Interv Radiol 19(5):736–741
Broor SL, Raju GS, Bose PP, Lahoti D, Ramesh GN, Kumar A, Sood GK (1993) Long term results of endoscopic dilatation for corrosive oesophageal strictures. Gut 34(11):1498–1501
Gupta P, Gulati A, Reddy YR, Samanta J, Kochhar R (2019) Does esophageal wall thickness on computed tomography predict response to endoscopic dilatation in patients with corrosive esophageal strictures? J Gastroenterol Hepatol Open 3(5):405–408
Uygun I, Arslan MS, Aydogdu B, Okur MH, Otcu S (2013) Fluoroscopic balloon dilatation for caustic esophageal stricture in children: an 8-year experience. J Pediatr Surg 48(11):2230–2234
Kochhar R, Ray JD, Sriram PV, Kumar S, Singh K (1999) Intralesional steroids augment the effects of endoscopic dilation in corrosive esophageal strictures. Gastrointest Endosc 49(4 Pt 1):509–513
Ilkin Naharci M, Tuzun A, Erdil A, Ates Y, Bagci S, Yamanel L, Dagalp K (2006) Effectiveness of bougie dilation for the management of corrosive esophageal strictures. Acta Gastroenterol Belg 69(4):372–376
Singhal S, Kar P (2007) Management of acid- and alkali-induced esophageal strictures in 79 adults by endoscopic dilation: 8-years’ experience in New Delhi. Dysphagia 22(2):130–134
Joshi P, Yadav R, Dangi A, Kumar P, Kumar S, Gupta V, Gupta V, Chandra A (2020) Corrosive esophageal strictures: from dilatation to replacement: a retrospective cohort study. Dysphagia 35(4):558–567
Saeed ZA, Winchester CB, Ferro PS, Michaletz PA, Schwartz JT, Graham DY (1995) Prospective randomized comparison of polyvinyl bougies and through-the-scope balloons for dilation of peptic strictures of the esophagus. Gastrointest Endosc 41(3):189–195
Kochman ML, McClave SA, Boyce HW (2005) The refractory and the recurrent esophageal stricture: a definition. Gastrointest Endosc 62(3):474–475
ASGE Standards of Practice Committee, Ben-Menachem T, Decker GA, Early DS, Evans J, Fanelli RD, Fisher DA, Fisher L, Fukami N, Hwang JH, Ikenberry SO, Jain R, Jue TL, Khan KM, Krinsky ML, Malpas PM, Maple JT, Sharaf RN, Dominitz JA, Cash BD (2012) Adverse events of upper GI endoscopy. Gastrointest Endosc. 76(4):707–718
Vermeulen BD, de Zwart M, Sijben J, Soons E, van der Weerd L, Arese D, von den Hoff DW, Craviotto V, Tan ACITL, Groenen MJM, Bogte A, Repici A, Spaander MCW, Siersema PD (2020) Risk factors and clinical outcomes of endoscopic dilation in benign esophageal strictures: a long-term follow-up study. Gastrointest Endosc. 91(5):1058–1066
Josino IR, Madruga-Neto AC, Ribeiro IB, Guedes HG, Brunaldi VO, de Moura DTH, Bernardo WM, de Moura EGH (2018) Endoscopic dilation with bougies versus balloon dilation in esophageal benign strictures: systematic review and meta-analysis. Gastroenterol Res Pract 2018:5874870
Tharavej C, Pungpapong SU, Chanswangphuvana P (2018) Outcome of dilatation and predictors of failed dilatation in patients with acid-induced corrosive esophageal strictures. Surg Endosc 32(2):900–907
Poley JW, Steyerberg EW, Kuipers EJ, Dees J, Hartmans R, Tilanus HW, Siersema PD (2004) Ingestion of acid and alkaline agents: outcome and prognostic value of early upper endoscopy. Gastrointest Endosc 60(3):372–377
Povilavičius J, Samalavičius NE, Verkauskas G, Trainavičius K, Povilavičienė M (2019) Conservative treatment of caustic oesophageal injuries in children: 15 years of experience in a tertiary care paediatric centre. Gastroenterol Rev 14(4):286–291
Doo EY, Shin JH, Kim JH, Song HY (2009) Oesophageal strictures caused by the ingestion of corrosive agents: effectiveness of balloon dilatation in children. Clin Radiol 64(3):265–271
Taşkinlar H, Bahadir GB, Yiğit D, Erdoğan C, Avlan D, Nayci A (2017) Effectiveness of endoscopic balloon dilatation in grade 2a and 2b esophageal burns in children. Minim Invasive Ther Allied Technol 26(5):300–306
Temiz A, Oguzkurt P, Ezer SS, Ince E, Hicsonmez A (2010) Long-term management of corrosive esophageal stricture with balloon dilation in children. Surg Endosc 24(9):2287–2292
Hammoudi N, Giaoui A, Lambert J, Dhooge M, Corte H, Tran-Minh ML, Cattan P, Gornet JM (2022) Predictive factors for the success of endoscopic dilation of esophageal caustic stricture: the experience of a French tertiary reference center. Surg Endosc 36(8):5660–5668
Gün F, Abbasoğlu L, Celik A, Salman ET (2007) Early and late term management in caustic ingestion in children: a 16-year experience. Acta Chir Belg 107(1):49–52
Karnak I, Tanyel FC, Büyükpamukçu N, Hiçsönmez A (1998) Esophageal perforations encountered during the dilation of caustic esophageal strictures. J Cardiovasc Surg 39(3):373–377
Rao KS, Ananthakrishnan N, Banerjee A (1988) Corrosive oesophagitis: an analysis of 50 cases. Aust N Z J Surg 58(9):723–726
Fan Y, Song HY, Kim JH, Park JH, Ponnuswamy I, Jung HY, Kim YH (2011) Fluoroscopically guided balloon dilation of benign esophageal strictures: incidence of esophageal rupture and its management in 589 patients. Am J Roentgenol 197(6):1481–1486
Gündoğdu HZ, Tanyel FC, Büyükpamukçu N, Hiçsönmez A (1992) Conservative treatment of caustic esophageal strictures in children. J Pediatr Surg 27(6):767–770
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
AKS and AJ wrote the initial manuscript; YRR, SA, and PG collected the data; AKS performed the analysis; SKS and RK did all the endoscopic procedures; RK critically revised the manuscript. All authors reviewed and approved the final version.
Corresponding author
Ethics declarations
Disclosures
Dr. Anupam Kumar Singh, Dr. Yalaka Rami Reddy, Dr. Anuraag Jena, Dr. Sreekanth Appasani, Dr. Pankaj Gupta, Prof. Saroj Kant Sinha, and Prof Rakesh Kochhar have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, A.K., Reddy, Y.R., Jena, A. et al. Endoscopic dilation with bougies versus balloons in caustic esophageal strictures: 17-year experience from a tertiary care center. Surg Endosc 37, 8236–8244 (2023). https://doi.org/10.1007/s00464-023-10384-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10384-4