Abstract
Background
Predictors of the efficacy of endoscopic dilation for caustic esophageal stricture have been poorly studied.
Methods
All patients undergoing an endoscopic dilation for an esophageal caustic stricture between 1990 and 2015 in a French national reference center were included. Success of dilation was defined by self-food autonomy without the need for reconstructive esophageal surgery.
Results
During the study period, 894 patients were admitted after caustic ingestion. Among them, 101 patients developed esophageal stricture and 92 patients were eligible for analysis (missing data in 8 cases, 1 patient died before endoscopic dilation). In this cohort (median age 42 years, women 53%, strong alkali 74%, suicide attempt 77%, hydrostatic balloon use 93%), the overall success rate of dilation was 57% with a median number of 3 dilation sessions (274 sessions, range 1–17). Factors predicting the success of the procedure were: non-inflammatory stricture or non-inflammatory intercalated mucosa between stricture (88% vs 47%, p = 0.001), a single stricture versus 2 or more strictures (69% vs 47% vs 33%, respectively, p = 0.04), a stricture of less than 5 cm (70% vs 27%, p < 0.001) and the existence of mild/ moderately tight or very tight stricture (70% vs 21% of success, p < 0.001). Perforation rate was 6.5% (18/274) requiring emergency surgery in 2 cases.
Conclusion
Several characteristics of caustic esophageal strictures are significantly associated with the success rate of endoscopic dilation. Our data may be useful for customizing treatment strategies in patients with a caustic stricture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and aims
Corrosive ingestion is a rare but potentially devastating event [1]. In adults, ingestions are mainly secondary to a suicide attempt and are potentially life-threatening [2]. This situation requires a multidisciplinary approach with the need for care in an expert center for the most severely affected patients [3, 4]. In the absence of emergency digestive resection, the most common sequelae are stricture formation. If it occurs, endoscopic treatment is the first-line treatment option that is generally performed with a session of stepwise bougie or balloon dilation. This procedure is safe and effective for short and long-term relief of esophageal symptoms in patients with caustic stricture [5]. However, caustic esophageal stricture (CES) seems more difficult to treat than other benign strictures with a higher tendency to become refractory to dilation [6, 7]. A recent study has shown that CES was associated with the need for more dilation sessions than other benign strictures [8]. However, data on the efficacy of endoscopic dilation of caustic stricture are scarce. As a result, there is great inter-individual variability in endoscopic practices that can lead to inappropriate endoscopic procedures or potentially avoidable surgery due to a lack of knowledge of the endoscopic lesions predicting the success of the procedure. Most studies have evaluated the success rate of the procedure by concomitantly analyzing all causes of benign stricture; caustic ingestion being the least common [8, 9]. Recently, computed tomography (CT)-scan has emerged as a better tool to evaluate esophageal corrosive injuries in the acute phase of ingestion, leading to an enlargement of conservative management than when the decision was based on endoscopic findings [10,11,12]. CT scan has contributed to better selection of patients with transmural necrosis requiring emergency surgery but leads to an increasing number of digestive strictures. These strictures are usually diagnosed within four months of ingestion, with a median delay of the occurrence of 47 days [12, 13]. Dysphagia consecutive to CES has a major impact on the nutritional status and the quality of life of the patients and a secondary surgical reconstruction may be necessary in case of dilation failure with substantial morbi-mortality rates [14]. The increasing number of caustic esophageal strictures in the era of CT-scan algorithm.
To date, no study has specifically investigated predictors of success of endoscopic dilation for caustic oesophageal stricture. In this study, we report the long-term results of dilation with a focus on predictive factors of the success of this procedure in a French expert center.
Patients and methods
Cohort selection
Patients undergoing at least one esophageal dilation for caustic stricture at our center between January 1990 and October 2015 were identified either from a hospital database known as PMSI (Programme de Médicalisation des Systèmes d’Information) or from the analysis of prospectively collected records of endoscopy reports. All patients provided informed written consent for the endoscopic procedure. The study protocol has been declared to the CNIL (Commission Nationale de l’Informatique et des Libertés; number 2218472). All data were anonymously collected and, according to the Loi Jardé (French law amended by Order no. 2016-800 and its implementing decree no. 2016-1537 of 16/11/2016 relating to research involving the human person), no patient consent was needed, as the treatment implemented in this study was one of the therapeutic options in this setting.
Endoscopic dilation procedure
We used adult gastroscopes only. From 1990 to 2008, both bougie and hydrostatic balloons were used, the type of procedure is left to the discretion of the endoscopist. From 2009, only balloons were used using a through-the-scope balloon (CRE, Controlled Radial Expansion, Boston Scientific Cork Ltd, Cork, Ireland), with 15–18 or 18–20 mm diameter, which was passed through the stricture under visual control only or after placement of a guidewire under either fluoroscopic or endoscopic guidance. The balloon was inflated for no more than 60 s per procedure. Subsequent dilation sessions were only scheduled in case of reappearance of dysphagia. Several dilations could be performed on the same stricture or in the case of multiple concomitant stenoses during the same session or a need for calibration of a residual stricture.
Data collection
At the first hospital admission for caustic ingestion, data on age, sex, reason for ingestion, characteristics of caustic, endoscopic findings according to the Zargar classification [15], CT-scan findings according to Chirica et al. [4], and early medico-surgical patient management were recorded.
At the first endoscopic dilation session, the following characteristics were recorded: time from ingestion to dilation, type of dilation used, number of strictures, inflammatory or fibrotic aspect of the stricture, and adjacent esophagus, diameter, and length of the stricture. The diagnosis of stricture was retained if the lesion was impassable by the adult endoscope. The endoscopist classified the stricture caliber as mild tight, moderately tight, and very tight. A stricture was considered to be long if its length was more than 5 cm.
At each endoscopic dilation session, the following data were noted: time since the last dilation session and aspect of endoscopic lesions as described above.
Endpoints
The overall success of endoscopic dilation was defined by the effectiveness of the overall strategy after one or more sessions allowing to avoid esophageal reconstructive surgery and to achieve nutritional autonomy. This nutritional status was defined by a stable weight with a varied diet and no need for home artificial nutrition at the last follow-up visit after a successful dilation program. In patients responding to these criteria, all the esophageal strictures were passable with the endoscope after the last dilation session of the overall procedure. In some patients, a new dilation session was performed after the date defining overall success in case of mild dysphagia but considered uncomfortable by the patient. It was not included in the analysis if it was isolated and occurred more than one year after the last session of the effective dilation.
Overall failure was defined as the inability to successfully dilate the esophageal stricture with the need for surgery during follow-up. As the study included patients with a long period of follow-up, we did not use uniform criteria to define refractory stricture. Technical failure or an inability to maintain a normal luminal diameter after several sequential dilations were usually considered refractory. Our primary objective was to assess the overall success rate of endoscopic dilation. The secondary objectives were to evaluate the complication rate and to determine predictive factors of the success of the procedure.
Statistical analysis
Quantitative variables are expressed using median and inter-quartile range (IQR), and qualitative variables using count and percentages. Comparison between success and failure groups was performed using Fisher’s exact test for qualitative variables and Wilcoxon’s test for quantitative variables.
Cumulative incidence of surgery was assessed in a competing risk framework, with overall success as the competing endpoint.
Statistical analyses were performed using R version 4.0.3, all tests were two-tailed and a p-value of less than 0.05 was considered statistically significant.
Results
Population
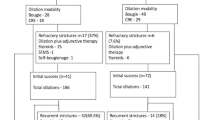
During the study period, 894 patients were hospitalized in Saint-Louis Hospital following caustic ingestion. Among them, 218 patients (24.5%) underwent emergency digestive resection and 129 patients (19.2% of the cohort with initial conservative treatment) developed esophageal stricture. In these patients, 101 had at least one endoscopic esophageal dilation. Eight patients treated by dilation were excluded for the following reasons: missing data (n = 6) and dilation sessions not carried out entirely in our center (n = 2). One patient died of cardiac arrest on induction of anesthesia at the first dilation session and was therefore excluded from the analysis. The study population includes therefore 92 patients. The characteristics of the whole population and the study population is presented in Fig. 1 and Table 1, respectively.
Strictures characteristics
The median time from ingestion to the diagnosis of stricture was 32 days (range: 6–263). The reasons for the endoscopy were as follows: dysphagia with documented stricture on barium swallow (n = 78) and systematic endoscopy for calibration of a residual stricture in 15% of the cases (n = 14). At the first dilation session, patients had a single stricture in 53% of the cases (n = 49), two strictures in 37% of the cases (n = 34), and more than two strictures in 10% of the cases (n = 9). These strictures were located for 11% in the upper third, 29% in the middle third, and 16% in the lower third of the esophagus. Forty patients (44%) had several strictures located in different esophageal segments. Ten patients (11%) had an associated gastric stricture.
A total of 146 esophageal strictures were recorded. The length of each stricture was for 10% an isolated ring, for 70% a short stricture ≤ 5 cm and 20% a long stricture of more than 5 cm. The maximum stricture caliber for each patient was mild tight in 18% of the cases, moderately tight in 54% of the cases, and very tight in 28% of the cases. When available (n = 68; 73%), the endoscopic aspect of the edges of at least one of the strictures or the adjacent mucosa was inflammatory in 43 cases (64%).
Overall results of the first dilation session
The median time from caustic ingestion to the first endoscopic dilation session was 83 days (range: 22–291). Hydrostatic dilation was used in 93% of the cases and bougies in 7% of the cases. This first session permitted the dilation of all stricture in 74% of patients (n = 68), allowing exploration of the gastric cavity and was therefore considered as successful. Among these, perforation occurred in 6% of the cases (n = 6). The failure rate of this first procedure was 26% (n = 24). The reasons for failure were: technical failure because the stricture was too long (n = 7) or too tight (n = 2), interruption of the procedure for fear of perforation (n = 10), and occurrence of a perforation (n = 5).
Overall success of the dilation strategy
After a median follow-up of 18.4 months (range 1.3–261.4), endoscopic dilation was successful in 57% of the patients (n = 53) after a median number of 3 endoscopic dilation sessions per patient (range 1–17); (Fig. 2). The cumulative incidence of success was 22.8% at 6 months, 45% at 12 months, 48.6% at 18 months, and 51.1% at 24 months. The median time between the first and last dilation sessions was 86 days. Overall dilation failure occurred in 43% of the patients (n = 39) after a median number of 2 dilation sessions (range 1–7). The reasons for failure were as follows: technical failure in 63% of the cases (n = 24), endoscopic perforation in 25% of the cases (n = 9) and a multidisciplinary decision to stop subsequent endoscopic procedures, stricture considered to be refractory due to too many dilation sessions in 13% of the cases (n = 5; number of sessions ≥ 5) and unknown in 2% of the cases (n = 1); (Table 2). The cumulative incidence of esophageal reconstructive surgery was 5.4%, 22%, and 29.2% respectively at 6, 12, and 24 months (Fig. 3).
Predictive factors for endoscopic dilation overall success
Several endoscopic features at the first endoscopic dilation session were associated with the success of the procedure. Among the tested parameters, the factors predicting the success of the procedure were: non-inflammatory stricture or non-inflammatory intercalated mucosa between stricture (88% of success vs 47%, p = 0.001), a single stricture versus two or more than two stricture (69% vs 47% vs 33% of success, respectively, p = 0.04), a stricture of less than 5 cm (70% vs 27% of success, p < 0.001) and the existence of mild/moderately tight or very tight stricture (70% vs 21% of success, p < 0.001). Conversely, the reason for ingestion, the type of products ingested, the dilation modality, and the site of esophageal stricture was not associated with the probability of overall success (Table 3).
Dilation complications
Among the 274 endoscopic dilation sessions, 18 perforations (6.5%) occurred. These 18 perforations occurred in 16 patients and corresponded to 17 esophageal and 1 diastatic gastric perforations. Seven of these 18 perforations were considered serious (39%). Two patients had undergone emergency surgery and five patients required intensive care medical management. Endoscopic treatment of perforation was not performed in any of them. No death occurred following perforation. The remaining eleven patients were treated medically, with resting of the gastrointestinal tract and antibiotics, allowing a rapid improvement in all cases. After esophageal perforation, a new attempt of dilation had been made in 3 cases, despite the rule to stop dilations after perforation, with one final success. One death was observed during follow-up related to metastatic gastric cancer in a patient successfully treated by dilation.
Discussion
This is the largest study evaluating the efficacy of endoscopic dilation for CES in adults. Our data suggest that this approach is successful for more than half of the patients after a mean number of 3 endoscopic dilation sessions. This rate is lower than in some series of the literature. However, the success criteria were unclear and/or heterogeneous. In an old Indian study using fiberoptic endoscopes, the success rate after a median of 8 bougie dilation sessions of 52 patients with CES was 93.6% but only 36 patients had a follow-up of more than six months and the overall success rate was defined solely by the improvement of a dysphagia score [16]. Two studies including 13 and 18 patients with caustic stricture reported a success rate of 92% and 83.3% but the treatment was also considered effective only on dysphagia scores. [17, 18]. Recently, a study of 891 endoscopic dilations of esophageal stricture mainly with bougies, 21 is of caustic origin, reported in this subgroup an overall success rate of 62% close to the result in our population [8]. This heterogeneity in success rate does not seem to be related to the technique used. Indeed, a meta-analysis of 461 patients comparing the use of bougies to the use of balloons in benign esophageal stricture did not show any difference regarding symptomatic relief, recurrence rate, and severe adverse events [19]. We report for the first-time predictors of success of endoscopic dilation of CES in adults. Caustic strictures are known to be more difficult to dilate than other benign strictures of the esophagus [7]. Factors predictive of the success of endoscopic dilation of benign esophageal stricture have already been reported in the literature [20]. However, to our knowledge, no study in adults specifically focusing on caustic stricture has been done on the subject. The increasing use of CT-scan in the acute phase of ingestion increases the rate of surgical sparing, which will lead to more frequent used dilatation for CES. A better understanding of factors predicting the success of this endoscopic procedure is, therefore, an emerging need in patients whose secondary management has become more complex. We confirm that complex strictures whether long, multiple, or associated with a severely stenosed lumen are associated with failure of endoscopic procedure. One new finding is the association between the inflammatory character of both stricture and intercalated mucosa between stricture and the risk of failure. These data suggest that in the case of inflammatory lesions, the strategy should be different. It may be discussed to postpone a dilation session or to discuss another modality of endoscopic management. To date, only one pediatric study involving 100 children has specifically investigated factors predictive of success in endoscopic dilation for caustic stricture [21]. This showed that long stricture, the existence of gastroesophageal reflux, and concomitant pharyngeal damage were predictive of dilation failure whereas a dysphagia-free period of 8 weeks or more within the first year of dilations was considered as a predictor of success. Our perforation rate seems higher than previously reported after esophageal endoscopic dilation [22]. However, an excess rate of perforation has been previously reported in the case of CES [16]. Mortality after endoscopic esophageal perforation appears high with a rate of 4.8% in a recent study [23]. However, the rates reported in the literature take into account all the causes of perforation, dilation being only one of the mechanisms. Our mortality rate is nil which is in line with a study reporting no deaths after instrumental endoscopic post-dilation perforation for benign stricture [24]. As caustic ingestions are associated with peri-esophageal fibrosis, we do not perform endoscopic treatment in case of perforations because of the very limited risk of mediastinitis. Different alternatives to endoscopic dilation such as steroids injection, stenting, or incisional therapy have been tested in cases of refractory esophageal stricture but no technique has been validated by a randomized study [25]. In particular biodegradable stents seem to be ineffective in cases of caustic stricture [26]. A double-blind, randomized, placebo-controlled trial including forty children with caustic esophageal strictures has shown that Mitomycin C application after dilation was significantly associated with a reduced number of dilation sessions to alleviate dysphagia but this result needs to be confirmed in adults [27]. In the future, early intervention with intravenous corticosteroid therapy in patients at high risk of stricture according to CT-scan in the acute phase of ingestion seems promising. The French CORTICAU trial is currently underway [28] with the main objective of reducing the incidence of stricture in the intervention group. Another approach in the case of refractory stricture onset is tissue engineering used to create substitutes adapted to short segment esophageal replacement and therefore replace conventional surgical reconstruction [29].
An excess risk of squamous cell carcinoma of 1000 compared to the general population has been reported in case of conservative treatment after caustic esophageal burns [30]. However, the impact of other risk factors, particularly alcohol-smoking intoxication or gastroesophageal reflux disease is unknown. It seems that repeated stricture dilation could play a major role in cancerization. This is an argument not to continue dilation sessions indefinitely in case of stricture recurrence. Therefore, endoscopic surveillance with either chromoendoscopy or narrowband image enhanced endoscopy has been proposed after a successful dilation program, although difficult in a population with a majority of psychiatric problems [31].
Our work has some important limitations as this is a monocentric and retrospective analysis study with a long inclusion period which may lead to a bias in the interpretation of our data. No standardized protocol for scheduling the dilation sessions was planned and the medical-surgical attitude may have varied over time in case of refractory stricture. We finally acknowledge that symptoms were not systematically quantified especially concerning dysphagia with the Eckardt score [32]. However, we included in the definition of the overall success rate, the absence of residual esophageal stricture and the achievement of nutritional autonomy without home artificial nutrition which is a major concern in patient’s quality of life and health. This study has some major strengths as well. We report on the real-life experience of a national tertiary center specializing for many years in the treatment of caustic burns in adults. In contrast to the majority of studies on endoscopic dilation of benign esophageal strictures, our work only deals with caustic stricture with procedures performed by expert endoscopists. We also described for the first time the factors predictive of successful dilation in this specific population with a long follow-up.
Conclusion
Our study confirms that endoscopic dilation is a safe and effective procedure for CES and defines predictive criteria for success. Validation of new techniques in case of failure of endoscopic dilation is urgently needed.
References
Hugh TB, Kelly MD (1999) Corrosive ingestion and the surgeon. J Am Coll Surg 189:508–522
Chang JM, Liu NJ, Pai BC et al (2011) The role of age in predicting the outcome of caustic ingestion in adults: a retrospective analysis. BMC Gastroenterol 11:72
Contini S, Scarpignato C (2013) Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol 19:3918–3930
Chirica M, Kelly MD, Sarfati E, Cattan P (2017) Caustic ingestion. Lancet 389:2041–2052
Broor SL, Raju GS, Bose PP et al (1993) Long term results of endoscopic dilation for corrosive oesophageal strictures. Gut 34(11):1498–1501
Piotet E, Escher A, Monnier P (2008) Esophageal and pharyngeal strictures: report on 1862 endoscopic dilations using the Savary-Gilliard technique. Eur Arch Oto-Rhino-Laryngol 265:357–364
Rodrigues-Pinto E, Pereira P, Ribeiro A et al (2016) Risk factors associated with refractoriness to esophageal dilation for benign dysphagia. Eur J Gastroenterol Hepatol 28:684–688
Vermeulen B, de Zwart M, Sijben J et al (2020) Risk factors and clinical outcomes of endoscopic dilation in benign esophageal strictures: a long-term follow-up study. Gastrointest Endosc 91(5):1058–1066
Pereira-Lima JC, Ramires RP, Zamin I Jr et al (1999) Endoscopic dilation of benign esophageal strictures: report on 1043 procedures. Am J Gastroenterol 94(6):1497–1501
Chirica M, Resche-Rigon M, Pariente B et al (2015) Computed tomography evaluation of high-grade esophageal necrosis after corrosive ingestion to avoid unnecessary esophagectomy. Surg Endosc 29:1452–1461
Chirica MR, Zagdanski AM, Bruzzi M et al (2016) Computed tomography evaluation of esophagogastric necrosis after caustic ingestion. Ann Surg 264:107–113
Bruzzi M, Chirica M, Resche-Rigon M et al (2019) Emergency computed tomography predicts caustic esophageal stricture formation. Ann Surg 270(1):109–114
Tseng YL, Wu MH, Lin MY et al (2004) Massive upper gastrointestinal bleeding after acid-corrosive injury. World J Surg 28:50–54
Chirica M, Veyrie N, Munoz-Bongrand N et al (2010) Late morbidity after colon interposition for corrosive esophageal injury: risk factors, management, and outcome. A 20-years experience. Ann Surg 252:271–280
Zargar SA, Kochhar R, Mehta S et al (1991) The role of fibe-roptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc 37:165–169
Broor SL, Raju GS, Bose PP et al (1993) Long term results of endoscopic dilation for corrosive oesophageal strictures. Gut 34:1498–1501
Chiu YC, Liang CM, Tam W et al (2013) The effects of endoscopic-guided balloon dilations in esophageal and gastric strictures caused by corrosive injuries. BMC Gastroenterol 13:99
Zhang C, Zhou X, Yu L et al (2013) Endoscopic therapy in the treatment of caustic esophageal stricture: a retrospective case series study. Dig Endosc 25(5):490
Josino IR, Madruga-Neto AC, Ribeiro IB et al (2018) Endoscopic dilation with bougies versus balloon dilation in esophageal benign strictures: systematic review and meta-analysis. Gastroenterol Res Pract. https://doi.org/10.1155/2018/5874870
Poincloux L, Rouquette O, Abergel A (2017) Endoscopic treatment of benign esophageal strictures: a literature review. Expert Rev Gastroenterol Hepatol 11(1):53–64
El-Asmar KM, Allam AM (2020) Predictors of successful endoscopic management of caustic esophageal strictures in children: when to stop the dilations? J Pediatr Surg S0022–3468(20):30595–30599
Chirica M, Champault A, Dray X et al (2010) Esophageal perforations. J Visc Sirg 147(3):e117–e128
Hauge T, Kleven OC, Johnson E et al (2019) Outcome after iatrogenic esophageal perforation. Scand J Gastroenterol 54(2):140–144
Wesdorp IC, Bartelsman JF, Huibregtse K et al (1984) Treatment of instrumental oesophageal perforation. Gut 25(4):398–404
Everett SM (2019) Endoscopic management of refractory benign oesophageal strictures. Ther Adv Gastrointest Endosc 12:2631774519862134
Kochhar R, Samanta J, Basha J et al (2017) Biodegradable stents for caustic esophageal strictures: do they work? Dysphagia 32(4):575–582
El-Asmar KM, Hassan MA, Abdelkader HM et al (2013) Topical mitomycin C application is effective in management of localized caustic esophageal stricture: a double-blinded, randomized, placebo-controlled trial. J Pediatr Surg 48(7):1621–1627
Corte H, Assistance Publique Hôpitaux de Paris, Corticosteroid Treatment in the Acute Phase of Caustic Ingestion Management (CORTICAU). NCT03760354
Poghosyan T, Catry J, Luong-Nguyen M et al (2016) Esophageal tissue engineering: current status and perspectives. J Visc Surg 153(1):21–29
Zhang X, Wang M, Han H et al (2012) Corrosive induced carcinoma of esophagus after 58 years. Ann Thorac Surg 94:2103–2105
Pennachi C, Hourneaux de Moura DT, Amorim R et al (2017) Lugol’s iodine chromoendoscopy versus narrow band image enhanced endoscopy for the detection of esophageal cancer in patients with stricture secondary to caustic/corrosive agent ingestion. Arq Gastroenterol 54(3):250–254
Eckardt VF, Aignherr C, Bernhard G (1992) Predictors of out-come in patients with achalasia treated by pneumatic dilation. Gastroenterology 103:1732–1738
Author information
Authors and Affiliations
Contributions
NH: writing. AG, MD: data collection. MLTM, PC, HC: copy editing of the manuscript. LJ: statistical work. JMG: manuscript coordination, writing, and data collection.
Corresponding author
Ethics declarations
Disclosures
Dr Jean-Marc Gornet has served as a speaker for Amgen, Janssen Cilag, Sanofi,Takeda and Tillots Pharma. Dr My-Linh Tran-Minh received honoraria from Abbvie and Dr Nassim Hammoudi from Janssen. Drs. Audrey Giaoui, Jérôme Lambert, Marion Dhooge, Hélène Corte and Pierre Cattan have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hammoudi, N., Giaoui, A., Lambert, J. et al. Predictive factors for the success of endoscopic dilation of esophageal caustic stricture: the experience of a French tertiary reference center. Surg Endosc 36, 5660–5668 (2022). https://doi.org/10.1007/s00464-021-08781-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08781-8