Abstract
Outcome of endoscopic dilatation in acid-induced corrosive esophageal stricture is less known. This study aims to determine the outcome of dilatation and predictors of failed dilatation in patients with acid-induced corrosive esophageal stricture. Patients diagnosed of corrosive esophageal strictures were included. Endoscopic dilatation with graded Savary-Gilliard dilator was performed as the first line treatment. Outcome of dilatation was considered favorable when patients were able to swallow solid without intervention at least six months after successful dilatation. Failure of dilatation was defined as one of the following; complete luminal stenosis, inability to perform safe dilatation, perforation, and inability to maintain adequate luminal patency. Surgery or repeated dilatation was indicated in failed dilatations. There were 55 patients with corrosive esophageal strictures. Of 55 patients, 41 (75%) had failed dilatation (38 having esophageal replacement procedure, two continue repeated dilatation and one unfit for surgery). Of 323 sessions of dilatations, eight out of 55 patients (14.5%) had perforations. There was no dilatation-related mortality. Patients with concomitant pharyngeal stricture (p = 0.0001), long (≥ 10 cm) stricture length (p < 0.0001), number of dilatation >6 sessions per year (p = 0.01) and refractory stricture (inability to pass a larger than 11 mm dilator within three sessions) (p = 0.01) were more likely to have failed dilatation. Thirty-two of 38 patients with surgery had good swallow outcome with one operative mortality (2.6%). At the median follow-up of 61 months, overall favorable outcome was 84% after surgery and 25% for dilatation (p < 0.0001). Majority of patients with acid-induced corrosive esophageal stricture were refractory to dilatation. Esophageal dilatations were ultimately failed in three-fourth of the patients. Concomitant cricopharyngeal stricture, long stricture length, requiring frequent dilatation, and refractory to >11 mm dilatation were factors associated with failed dilatation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal strictures are a major complication following corrosive ingestion. The majority of previous reports included mainly patients who unintentionally ingested alkaline substances [1,2,3]. Acid ingestion is relatively uncommon and is usually associated with suicidal attempts [1, 4]. The injury severity depends on many factors, including the level of acidity of the agent (pH <2 or pH >15), contact time, amount, and purpose of ingestion [1, 2, 5,6,7,8,9]. The purpose of ingestion may represent the most important factor to predict the injury severity. Intentional ingestion is usually associated with severe injury and stricture [1, 4]. In Thailand, acidic substances are present in various toilet cleaning agents and are easily accessible over the counter across the country. The active ingredient in the cleaners is mainly hydrochloric acid at concentration ranging from 7 to 20%.
Endoscopic dilatation is recommended as a primary treatment for caustic esophageal strictures [10,11,12]. However, its therapeutic efficacy has been less known. Variable treatment outcome have been reported in previous studies [4, 11, 13,14,15]. The majority of esophageal strictures caused by accidental ingestion usually do not require surgical treatment and are successfully treated by esophageal dilatation [2, 5, 14]. Conversely, strictures resulting from intentional ingestion of large quantities of highly corrosive substances are typically refractory to dilatation [4]. Several adjunctive options, including esophageal stenting [16], intralesional steroid injection [17], and the local application of mitomycin-c [18, 19], have been proposed to enhance therapeutic effect of dilatation in refractory strictures. However, their treatment outcomes are inconclusive. Both long-term repeated dilatation [12, 14] and surgical intervention [20] are advocated for these patients. The use of continue repeated dilatation could be ineffective in some patients. Surgical treatment is currently a mainstay therapy in patients with failed dilatation. A favorable swallowing outcome has been reported in approximately 80% of patients, and the operative mortality is less than 5% [21,22,23].
The aims of this study were to evaluate the efficacy of endoscopic bougie dilatation in adult patients with acid-induced corrosive esophageal strictures and to identify factors associated with failed endoscopic esophageal dilatation.
Patients and methods
We reviewed the medical records of patients diagnosed with corrosive esophageal strictures from August 2001 to July 2015 at King Chulalongkorn Memorial Hospital. Only patients with a history of ingesting acidic substances were included. The majority of patients were initially treated at outside hospitals and were referred to our center after the strictures developed. The patients who had emergency esophagogastric resection, anastomotic stricture, prior history of esophageal stent placement, or intralesional steroid injection were excluded. The clinical information and treatment outcomes of all patients, including demographics, nutritional status, dysphagia grading, and endoscopic, esophagogram, and surgical findings, were collected and analyzed. The majority of patients with an initial diagnosis of endoscopic grade 2 or more had an esophagogram at 3–4 weeks after ingestion, except for the cases with a high risk of aspiration. The endoscopic dilatation was attempted initially for all esophageal strictures, and surgical interventions were offered to patients with failed dilatations. The risks and benefits of surgical treatment and continue repeated dilatation were discussed with the patients who had refractory or recurrent strictures.
Definitions
A favorable outcome of endoscopic dilatation or surgery was defined as having the ability to swallow solid or semisolid food and maintain nutritional status without requiring endoscopic or surgical intervention or supplemental feeding via enterostomy for at least six months after adequate dilatation or surgery.
An unfavorable outcome or failure of dilatations was defined using the following criteria: (1) inability to properly place a guidewire for safe dilatationFootnote 1, (2) complete luminal strictureFootnote 2, (3) iatrogenic esophagogastric perforation or dilatation-related mortality, or (4) refractory or recurrent stricture.
A refractory stricture was defined as the inability to successfully dilate to a 14-mm diameter at 2-week intervals over five sessions [24].
A recurrent stricture was defined as the inability to maintain luminal patency for more than 4 weeks after a successful 14-mm dilatation [24].
An unfavorable outcome of surgery was defined using the following criteria: (1) patients were unable to swallow solid or semisolid food within 6 months after surgery, (2) frequent severe aspiration >1 time/month, (3) death, (4) requiring feeding enterostomy supplementation, or (5) requiring endoscopic intervention >1 time/6 months or re-operation.
Outcome evaluation
All patients had a minimum follow-up of 6 months after dilatation or surgery. At the median duration of 61 months, all patients were interviewed and evaluated regarding swallowing function, dysphagia grading, nutritional status, history of aspiration, and general physical examination. The outcomes of endoscopic dilatation and surgery were evaluated. Additionally, the factors associated with an unfavorable outcome of dilatation were determined.
Endoscopic esophageal dilatation
Endoscopic esophageal dilatation is the standard primary treatment in patients with caustic esophageal strictures in our surgical unit, and surgery is reserved for patients with failed dilatation. The first dilatation occurred 4–8 weeks after ingestion. The risks and benefits of esophageal dilatation were presented to patients prior to initiating treatment. In our dilatation program, all patients with esophageal strictures are scheduled for dilatation at 2-week intervals until adequate diameter. Dilatation is considered adequate when 14 mm diameter over five sessions is reached or 12.8 mm in some patients who are able to swallow solid/semisolid without symptom of dysphagia. Patients with adequate dilatation are followed up for recurrence of dysphagia symptom every 1 month for the first 6 months, then every 3–6 months. Patients with recurrent dysphagia following adequate dilatation (recurrence) and patients with inadequate dilatation over five sessions (refractory) who refused or had yet decided to undergo surgery were scheduled for periodic continue repeated dilatation at 2 to 12-week intervals, depending on their dysphagia symptom and dilatation findings. Information regarding risks and benefits of continue repeated dilatation and esophageal replacement surgery are also provided to these groups of patients.
All sessions were performed under general anesthesia using graded Savary-Gilliard dilators passed over a guidewire using fluoroscopic monitoring. All patients were in the supine position, and an upper endoscopy was performed to evaluate the stricture characteristics. A spring-tip guidewire was passed through the stricture orifice down to the stomach and was monitored by endoscopy and fluoroscopy. The proper positioning of the guidewire for safe dilatation required a loop of the distal end of a guidewire to form within the stomach (Fig. 1). Then, gradual stepwise dilatation from a 5-mm to a 7-, 9-, 11-, 12.8-, 14-, and 15-mm diameter was performed. The “rule of three” was applied in each session. The patients without complications were discharged on the next day after dilatation. Long-term proton pump inhibitor medications were routinely prescribed to all patients after dilatation. The patients with perforations were considered to have failed dilatation and had emergency surgery or conservative treatment, depending on their clinical findings and conditions.
Statistical analysis
The Mann–Whitney U test was used to compare qualitative variables, and the Chi square test was used for categorical comparisons. The data are expressed as medians with ranges in parenthesis and the means ± SD. We considered results with p-values less than 0.05 as statistically significant.
Results
There were 65 patients diagnosed with corrosive esophageal stricture from August 2001 to July 2015 at King Chulalongkorn Memorial Hospital. We excluded 10 of the 65 patients due to the following reasons: 5 patients with upper GI discontinuity from previous emergency esophagogastrectomy, three patients with alkali ingestion, and two patients who were lost to follow-up. Thus, 55 patients (22 males, 33 females) were enrolled in the study, and the median follow-up time was 61 months (range 14–168 months). The patient demographic data and stricture characteristics are summarized in Table 1. The median patient age was 31 years (range 15–68 years). Toilet cleaning agents with 7–20% hydrochloric acid (HCl) as an active ingredient were ingested in 96% (53/55) of the patients. The other two patients swallowed sulfuric and formic acid. Ingestion with suicidal intent was reported in 95% (52/55) of cases. All patients were treated initially at the outside hospitals and were referred to our surgical unit when strictures developed. The median time from the ingestion to the first session of esophageal dilatation was 8 weeks (range 3–1020 weeks). One patient presented with a benign esophageal stricture 20 years after caustic ingestion. The median esophageal stricture length was 12 cm (range 2–20 cm). The data indicated that 60% of patients had a stricture length ≥ 10 cm and that 11% of cases had strictures <5 cm. Concomitant gastric scarring, cricopharyngeal stricture, and laryngeal deformity were identified in 85% (33/39), 49% (27/55), and 13% (7/55) of patients, respectively.
Endoscopic bougie dilatation was initially attempted in all 55 patients. A total of 323 sessions of dilatation was performed. There were esophagogastric (6 esophageal, 2 gastric) perforations reported in eight patients (14.5%). Seven of the 8 perforations occurred during the first or second session with the diameter of 11–12.8 mm. Of eight patients with perforations, seven patients underwent successful emergency surgery and one of them was successfully managed by non-operative treatment. All eight patients subsequently had esophageal replacement procedure approximately 6 months later. There was no dilatation-related mortality. The treatment outcomes and findings of esophageal dilatation are shown in Table 2. A favorable outcome was evident in 25% (14/55) of the 55 patients treated with dilatations. Of the 14 patients with favorable outcomes, nine had a stricture length ≥5 cm. There was an unfavorable outcome in 41 patients, including eight patients with perforations, five patients with complete luminal strictures, five patients in whom safe dilatation could not be performed, and 23 patients who were recurrence/refractory to dilatation. Of 23 patients with recurrence/refractory to dilatation, two of them received long-term periodic repeated dilatation. These patients were able to swallow solid or semisolid food and were well-nourished at a median follow-up of 15 months. The median number of dilatation sessions was significantly lower in patients with favorable outcomes than that in patients with unfavorable outcomes after excluding eight patients with perforations [two sessions (range 1–30) vs. six sessions (range 1–60), p = 0.04)]. Compared to patients with unfavorable outcomes, the patients with favorable outcomes had significantly shorter stricture lengths [(5 cm (range 2–12) vs. 13 cm (range 12–20), p < 0.0001]. We observed that all patients who were refractory to >11-mm dilatation within three sessions were ultimately refractory to 14-mm dilatation over five sessions as well.
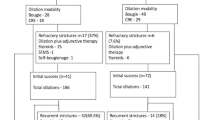
Of 41 patients with unfavorable outcome of esophageal dilatation, 38 underwent esophageal replacement procedures (Fig. 2). Of these 38 patients, 21 patients were recurrence/refractory to dilatation, four patients had complete luminal strictures, eight patients had perforations, and inability to properly place a guidewire in five patients. Four patients who had complete luminal stenoses were lost to follow-up after adequate dilatation. All of these patients had complete cricopharyngeal obliteration and returned to our unit with severe malnutrition. We were unable to place the guidewire properly for safe dilatation in five patients after a median of two dilatation sessions. The tip of the guidewire was unable to pass through the esophagogastric junction into the stomach in three patients due to multiple stricture sites with angulation. The distal end of the guidewire was unable to form a loop in the stomach in two patients because of severe gastric cicatrization. The swallowing outcomes were evaluated using the same criteria as the dilatation at a median follow-up of 52 months after surgery. A favorable outcome after surgery was achieved in 84% (32/38) (Fig. 3) of patients, and the surgical mortality rate was 2.6% (1/38).
Characteristics of failed dilatation, their treatments, and swallow function of 41 patients with unfavorable outcome of endoscopic bougie dilatation. Of these 41 patients, 38 underwent esophageal replacement procedure approximately 6 months after ingestion, two patients had periodic repeated dilatation and 1 patient was unfit for surgery having life-long enteral feeding. Of 38 patients undergoing colon interposition, 32 (84%) had good swallow function with one (2.6%) operative mortality
We identified factors associated with unfavorable outcomes of bougie dilatation in patients with acid-induced corrosive esophageal strictures. These factors included the following: (1) stricture length ≥10 cm, (2) number of dilatation session >6/year, (3) a stricture that was unable to be dilated >11 mm in diameter over 3 sessions, and (4) concomitant cricopharyngeal stricture (Table 3).
Discussion
The caustic ingestions with suicide attempts typically results in severe stricture of the esophagus. In this study, we reported the treatment outcome of dilatations in a homogeneous group of patients who had acid-induced corrosive esophageal strictures due to suicide-related ingestions. In Thailand, strong corrosive agents can be easily accessed in the form of toilet cleaning agents available over the counter. The majority of these agents contain hydrochloric acid (HCl) as an active ingredient, and the concentrations range from approximately 7–20%. The severity of caustic esophageal injury depends on many factors, including the purpose of ingestion, active ingredient of substances, concentration of the caustic agent, amount of substance consumed, and contact time [2]. The purpose of ingestion may be the most important factor for predicting the severity of organ injury. Patients ingesting chemicals with suicidal intent typically consumed a large amount of strong acid or alkali substances [5]. Conversely, accidental ingestion is typically associated with a small amount of chemical. A study from the United States over a 28-year period reported 95 patients with caustic ingestion. The majority of these patients had accidental ingestion. Approximately 60% of the patients had a mild degree (grade 1) or no esophageal injury (grade 0), and only 15% had grade 3 injury [3]. In contrast, a report from Taiwan including 273 caustic ingestion patients with a suicidal intent rate of 70% showed a severe (grade 3) esophageal injury rate of 45% [6]. Consequently, the incidence of late esophageal stricture was higher in the group of patients with a more severe injury grading. The incidence of esophageal stricture ranged from 40-57% following grade 2b and 69–80% after grade 3 injury [5, 25].
Endoscopic esophageal dilatation has been recommended as a standard primary treatment of corrosive esophageal stricture. The treatment efficacy is comparable between the balloon and bougie techniques [14]. The outcomes of dilatation in corrosive strictures are poorer than those in dilatation of other benign strictures and included more sessions of dilatations and higher rates of recurrence and perforation [26]. Moreover, corrosive esophageal strictures resulting from suicidal-related ingestion were more likely to be refractory to dilatation. The outcomes of dilatations in previous studies of corrosive esophageal strictures are summarized in Table 4. The reports of long-term clinical success are variable and range from 40 to 90% [4, 11, 13,14,15]. A study from India that primarily included patients with accidental ingestion and stricture length <2 cm reported a success rate for dilatation of >80% [11]. Conversely, Poley et al. reported a clinical success rate of only 43% with dilatation treatment in a cohort with a suicidal intent rate of 85% [4]. In our series with 95% suicidal-related ingestion, there was a favorable outcome of dilatation in only 25% of the patients. The differences in clinical success between these studies may result from the difference in stricture severity. The studies that included a higher proportion of patients with suicidal intent were more likely to reveal more refractory strictures and have a lower percentage of clinical success after esophageal dilatation.
Kochman et al. recently defined refractory benign esophageal stricture (RBSE) and recurrent stricture as an inability to successfully dilate to a 14-mm diameter over five sessions at 2-week intervals and the inability to maintain luminal patency for more than 4 weeks after successful 14-mm dilatation, respectively [24]. Investigators agree that caustic strictures are more likely to be refractory to dilatation than other etiologies. The management of caustic esophageal strictures that is refractory to dilatation remains controversial. The current acceptable therapeutic options include repeated dilatation with or without adjunctive treatment and surgery. Repici et al. investigated the natural history and long-term outcome of endoscopic dilatation with and without esophageal stenting in 70 patients. The study population included seven cases with caustic strictures diagnosed as refractory or recurrent benign esophageal strictures according to Kochman’s definition. The authors found that long-term clinical resolution (at least 6 months) was achieved in 31.4% (22/70) of cases [19/48 (40%) for dilatation alone and 3/24 (12.5%) for dilatation with stenting] [27]. The findings confirm that endoscopic dilatations with or without adjunctive esophageal stent placement in patients with refractory esophageal strictures are less effective. Similar outcomes were demonstrated in our study, and only two out of 25 (8%) patients with refractory or recurrent strictures had favorable outcomes after repeated dilatation. These two patients with recurrent stricture after adequate dilatation who refused surgery underwent long-term periodic repeated dilatation at 12-week intervals (four sessions/year). They were satisfactory with the treatment and had good swallow function and nutritional status without the need of enteral feeding. There are several adjunctive therapeutic options available to avoid surgical intervention, including biodegradable esophageal stents, intralesional steroid injection, endoscopic stricture incision, and application of mitomycin-c. However, data on these supplemental options in caustic strictures are limited [16,17,18,19]. Thus, additional large prospective trials are needed to confirm their efficacy.
Predictors of failed dilatation in corrosive esophageal stricture are less known. Lahoti et al. investigated the predictors of response to endoscopic dilatation of corrosive esophageal strictures in one study. They found that that patients with a maximal esophageal wall thickness of ≥9 mm measured by CT scan required a significantly higher number of sessions for successful dilatation than the cases with a wall thickness <9 mm (7.57 ± 1.8 vs. 1.42 ± 0.27 sessions, p < 0.05) [28]. We identified 4 factors associated with failed dilatation, namely, stricture length ≥ 10 cm, concomitant cricopharyngeal stricture, requirement of frequent dilatation (>6 sessions of dilatation per year), and strictures refractory to dilatation of more than 11-mm in diameter over 3 sessions. Of the 55 patients in our study, 11 (20%) patients have no risk factors, 12 patients have one, 17 patients have two, 11 patients have three, and 4 patients have four factors. The patients who are negative for all of these factors have a 100% success rate from dilatation treatment. Of 12 patients with one risk factor, 8 (75%) patients have unfavorable outcome. All 32 patients (100%) presenting with more than 1 factor have failed dilatation. This implies that patients without any risk factors are good candidates for dilatation. Conversely, patients with multiple risk factors would ultimately fail dilatation treatment. However, these predictors are based on our retrospective observation. Validation is needed in prospective study before clinical application is initiated.
Esophageal perforation continues to be a major complication of esophageal dilatation. The perforation can be associated with high morbidity and mortality [29]. The perforation rate for benign esophageal strictures is 0.18-0.4% [30, 31]. The incidence was higher (0–32%) in caustic strictures [4, 11, 13,14,15] (Table 4). A study by Broor et al. reported the perforation rate as 8 out of 52 patients (15%) using rigid dilators and noted that the risk of perforation was increased in patients with caustic injuries and in cases with long, eccentric, and tight strictures [11]. In our study, the incidence of perforation was 14.5% (8/55 patients). All 8 perforations had stricture length more than 10 cm. Seven out of 8 perforations occurred during the first or second session with 11–12.8-mm dilators. The higher perforation rate may partially result from the higher severity and more refractory strictures in corrosive-induced than in other etiologies. Special attention must be paid for all the technical details during the dilatation in patients with corrosive esophageal stricture.
Surgical treatment remains a standard of care for caustic refractory strictures. Clinical success has been reported at 76–84%, with 27–62% morbidity and 3–4.2% mortality [21,22,23]. Our study also revealed similar findings. Favorable outcomes were observed in 84% of cases, and there was a 2.6% (1/38) operative mortality rate. The rate of favorable outcomes was significantly higher among patients undergoing surgical treatment than that among patients with repeated dilatation. There is currently no uniform indication for surgery. Several investigators advocate surgery in patients with a stricture length >3 cm, and some authors consider a failure of dilatation as a surgical indication. We found that complete luminal stricture, inability to perform safe dilatation, iatrogenic perforation, and refractory stricture were indicators for failed dilatation and definitely represent indications for surgery.
There were some limitations in this study due to the nature of retrospective case series. The assessment of esophageal stricture length was performed non-uniformly depending on the available examination data for each patient, including esophagogram, endoscopy, and surgical findings or esophagectomized specimens. The decision regarding tightness, size of dilator, and failure of dilatation was made liberally by an operating endoscopist. As a referral center, patients were selected who had high stricture severity, delayed dilatation treatment, and severe malnutrition, which may have affected the treatment outcome.
In conclusion, endoscopic dilatation is still a mainstay primary treatment in corrosive esophageal stricture. However, the majority of acid-induced corrosive esophageal strictures are refractory to dilatation. Endoscopic bougie dilatations are ultimately failed in about three forth of the patients. Concomitant cricopharyngeal stricture, long stricture length (>10 cm), requiring frequent dilatation (>6 sessions/year), and refractory to >11 mm dilatation were factors associated with failed dilatation.
Notes
The inability to properly place a guidewire for safe dilatation was defined when a loop of the distal end of the guidewire was unable to be formed within the stomach before dilatation was initiated.
Complete luminal stricture was defined when there was an inability to identify a luminal orifice to negotiate a guidewire.
References
Arevalo-Silva C, Eliashar R, Wohlgelernter J, Elidan J, Gross M (2006) Ingestion of caustic substance: a 15-year experience. Laryngoscope 116:1422–1426
Celik B, Nadir A, Sahin E, Kaptanoglu M (2009) Is esophagoscopy necessary for corrosive ingestion in adults? Dis Esophagus 22:638–641
Tohda G, Sugawa C, Gayer C, Chino A, McGuire TW, Lucas CE (2008) Clinical evaluation and management of caustic injury I the upper gastrointestinal tract in 95 adult patients in an urban medical center. Surg Endosc 22:1119–1125
Poley J-W, Steyerberg EW, Kuipers EJ, Dees J, Hartmans R, Tilanus HW, Siersema PD (2004) Ingestion of acid and alkaline agents: outcome and prognostic value of early upper endoscopy. Gastrointest Endosc 60:372–377
Cabral C, Chirica M, Chaisemartin Cd, Gornet JM, Munoz-Bongrand N, Halimi B, Cattan P, Sarfati E (2012) Caustic injuries of the upper digestive tract: a population observational study. Surg Endosc 26:214–221
Cheng HT, Cheng CL, Lin CH, Tang JH, Chu YY, Liu NJ, Chen PC (2008) Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol 8:31
Keh SM, Onyekwelu N, McManus K, McGuigan J (2006) Corrosive injury to upper gastrointestinal tract: still a major surgical dilemma. World J Gastroenterol 12:5223–5228
Gumaste VV, Dave PB (1992) Ingestion of corrosive substances by adults. Am J Gastroenterol 87:1–5
Berthet B, Castellani P, Brioche MI, Assadourian R, Gautheir A (1996) Early operation for severe corrosive injury of the upper gastrointestinal tract. Eur J Surg 162:951–955
Bothereau H, Munoz-Bongrand N, Lambert B, Montemagno S, Cattan P, Sarfati E (2007) Esophageal reconstruction after caustic injury: is there still a place for right coloplasty? Am J Surg 193:660–664
Broor SL, Raju GS, Bose PP, Lahoti D, Ramesh GN, Kumar A, Sood GK (1993) Long term results of endoscopic dilatation for corrosive esophageal stricture. Gut 34:1498–1501
Zhang C, Zhou X, Yu L, Ding J, Shi R (2013) Endoscopic therapy in the treatment of caustic esophageal stricture: a retrospective case series study. Dis Endosc 25:490–495
Ilkin Naharci M, Tuzun A, Erdil A, Ates Y, Bagci S, Yamanel L, Dagalp K (2006) Effectiveness of bougie dilation for the management of corrosive esophageal strictures. Acta Gastroenterol Belg 69:372–376
Singhal S, Kar P (2007) Management of acid- and alkali-induced esophageal strictures in 79 adults by endoscopic dilatation: 8-years’ experience in New Delhi. Dysphagia 22:130–134
Song HY, Han YM, Kim HN, Kim CS, Choi KC (1992) Corrosive esophageal stricture: safety and effectiveness of balloon dilatation. Radiology 184:373–378
Karakan T, Utku OG, Dorukoz O, Colak SB, Erdal H, Karatay E, Tahtaci M, Cengiz M (2013) Biodegradable stents for caustic esophageal strictures: a new therapeutic approach. Dis Esophagus 26:319–322
Kochhar R, Ray JD, Sriram PVJ, Kumar S, Singh K (1999) Intralesional steroids augment the effects of endoscopic dilatation in corrosive esophageal strictures. Gastrointest Endosc 49:509–513
El-Asmar KM, Hassan MA, Abdelkader HM (2013) Hamza AF (2013) Topical mitomycin-c application is effective in management of localized caustic esophageal stricture: a double-blinded, randomized, placebo-controlled trial. J Pedriatr Surg 48:1621–1627
Nagaich N, Nijhawan S, Katiyar P, Sharma R, Rathore M (2014) Mitomycin-c: ‘a ray of hope in refractory corrosive esophageal strictures. Dis Esophagus 27:203–205
Harlak A, Yigit T, Coskun K, Ozer T, Mentes O, Gulec B, Kozak O (2013) Surgical treatment of caustic esophageal strictures in adults. Int J Surg 11:164–168
Wu MH, Tseng YL, Lin MY, Lai WW (2001) Esophageal reconstruction for hypopharyngoesophageal strictures after corrosive injury. Eur J Cardiothorac Surg 19:400–405
Knezevic JD, Radovanovic NS, Simic AP, Kotarac MM, Skrobic OM, Konstantinovic VD, Pesko PM (2007) Colon interposition in the treatment of esophageal caustic strictures: 40 years of experience. Dis Esophagus 20:530–534
Chirica M, Resche-Regon M, Bongrand NM, Zohar S, Halimi B, Gornet JM, Sarfati E, Cattan P (2012) Surgery for caustic injuries of the upper gastrointestinal tract. Ann Surg 256:994–1001
Kochman ML, McClave SA, Boyce HW (2005) The refractory and the recurrent esophageal stricture: a definition. Gastrointest Endosc 62:474–475
Zargar SA, Kochhar R, Nagi B, Mehta S, Mehta SK (1989) Ingestion of corrosive acids. Spectrum of injury to upper gastrointestinal tract and natural history. Gastroenterology 97:702–707
Rodrigues-Pinto E, Pereira P, Ribeiro A, Lopes S, Moutinho-Ribeiro P, Silva M, Peixoto A, Gaspar R, Macedo G (2016) Risk factors associated with refractoriness to esophageal dilatation for benign dysphagia. Eur J Gastroenterol Hepatol 28:684–688
Repici A, Small AJ, Mendelson A, Javoni M, Correale L, Hassan C, Ridola L, Anderloni A, Ferrara EC, Kochman ML (2016) Natural history and management of refractory benign esophageal strictures. Gastrointest Endosc 84:222–228
Lahoti D, Broor SL, Basu PP, Gupta A, Sharma R, Pant CS (1995) Corrosive esophageal strictures: predictors of response to endoscopic dilation. Gastrointest Endosc 41:196–200
Karnak I, Tanyel FC, Buyukpamukcu N, Hicsonmez A (1998) Esophageal perforations encountered during the dilatation of caustic esophageal strictures. J Cardiovasc Surg 39:373–377
Piotet E, Escher A, Monnier P (2008) Esophageal and pharyngeal strictures: report on 1862 endoscopic dilatations using the Savary-Gilliard technique. Eur Arch Otorhinolaryngol 265:357–364
Silvis SE, Nebel O, Rogers G, Sugawa C, Mandelstam P (1976) Endoscopic complications. Results of the 1974 American Society of Gastrointestinal Endoscopy surgery. JAMA 235:928–930
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Tharavej, Pungpapong, Chansawangphuvana have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Tharavej, C., Pungpapong, Su. & Chanswangphuvana, P. Outcome of dilatation and predictors of failed dilatation in patients with acid-induced corrosive esophageal strictures. Surg Endosc 32, 900–907 (2018). https://doi.org/10.1007/s00464-017-5764-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5764-x