Abstract
Introduction
In patients with benign and refractory esophageal strictures (BES), repeating initial dilations in short intervals could be recommended, but little data are available to validate this strategy. Our aim was to evaluate long-term results of a scheduled program of repeated and sustained esophageal dilations in patients with refractory strictures.
Methods
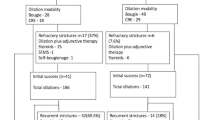
Patients with BES requiring five or more dilations were retrospectively included and divided in two groups for analysis: a SCHEDULED group (SDG) where patients were systematically rescheduled for the 5 first dilations; ON-DEMAND group (ODG) where patients were dilated only in case of recurrence of the dysphagia. Comparison between SDG and ODG was done with a 1:1 matching analysis and etiology of stricture. Clinical success was defined as the absence of dysphagia for more than a year.
Results
39 patients with refractory BES were included with post-operative stenosis in 51.2% and post-caustic injury 28.2%; 10 were in SDG and 29 in ODG. In overall analysis (39 patients), the follow-up was 64.4 ± 32 months, success rate was 79.5% and duration of treatment was 27.3 ± 20 months, and mean number of dilations was 11.7 per patient. The need for dilations decreased significantly after 18 months of treatment with an average of 0.56 dilations per semester. Self-expandable metallic stent insertion was associated with an increased rate of complications (5.9% vs 59.1% p = 0.001). In matched analysis (10 ODG vs 10 SDG patients), the duration of treatment was lower in SDG (18.8 vs 41.4 months, p = 0,032) with a higher probability of remission (survival analysis, Log-rank: p = 0,019) and the success rate did not differ between ODG and SDG patients (80% vs 90%; NS).
Conclusion
Overall, long-term esophageal dilations resulted in a 79.5% success rate and the need for further dilatations decreased significantly in both groups after 18-month follow-up. A scheduled dilation program was associated with a higher probability of final success and lower treatment duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Benign esophageal strictures (BES) can be of multiple origins and have a negative impact on patient quality of life and nutritional status. Nowadays, stricture etiology varies depending on the centers and geographical areas. The different categories of etiology are distributed between anastomotic strictures in 27%–50% of cases, peptic strictures in 20%–26% of cases, caustic in 8.5%–60% of cases, post-radiation therapy in 2%–12% of cases, and other rarer etiologies [1, 2].
The standard treatment for BES is endoscopic dilation, using either Savary-Gilliard bougies or hydraulic dilation balloons, both with similar effectiveness and safety profiles [3,4,5]. However, while the majority of patients will no longer have dysphagia after < five dilations, approximately 10% will still be symptomatic [6], tending to be “refractory” and requiring further treatment sessions [7]. In 2005, a definition of refractory stricture was put forward as the inability to maintain a luminal diameter of ≥ 14 mm after five sequential dilatation sessions [8]. Several associated treatment methods have been studied in suchlike refractory strictures. Local steroid injection has shown good results for peptic strictures [9, 10], but its efficacy seems limited for strictures of caustic or anastomotic origin [11, 12]. Radial incision is reserved for short strictures of < 1.5 cm in length [13, 14]. However, a randomized controlled trial has failed to show a significant improvement in the incised group [15]. Similarly, covered self-expandable metal stents (SEMS) seemed effective in approximately 40% of patients, but they were associated with high recurrence rates and stent-related adverse events [16, 17].
Surgery can also be a therapeutic solution in cases of BES that do not respond to endoscopic treatment. Excision of the stenosis can be performed with replacement by a gastric, colonic, or jejunal tube. Replacement by a gastric tube is preferred when feasible given it has lower morbidity rates. However, it is not uncommon for this option to be impossible given its lesion involvement (caustic injury, esogastric anastomosis) [18].
Although guidelines recommend to perform frequent dilations to quickly calibrate the esophageal diameter [19], there are little data in the literature to support this therapeutic strategy, with no study having evaluated the relationship between dilation intervals and patient outcomes.
Thus, the aim of this study was to retrospectively assess the efficacy of a prolonged endoscopic dilatation program in problematic and refractory BES. We aimed to identify the effects of a scheduled dilatation program, among other factors, on efficacy, duration, and complication rate.
Patients and methods
Patients
This was a retrospective single-center study conducted at the North Hospital (Hôpital Nord), Marseille, France. All patients treated in our endoscopy unit for repeat esophageal dilatations for refractory stricture between 01/10/2003 and 01/01/2019 were eligible for study inclusion.
The inclusion criteria were patients over 18 years of age, suffering from dysphagia due to a BES not allowing passage of a therapeutic gastroscope (11 mm), and who had already undergone five or more dilation sessions. Patients were excluded in the event of a neoplastic etiology, long strictures (> 3 cm), or esophageal motor disorders (characterized by 100% failed esophageal peristalsis).
The data used were anonymized and collected from the Assistance Publique-Hôpitaux de Marseille (Marseille Public Hospitals) computer file (Axigate SAS, Paris, France) which is disclosed to the Commission Nationale de l’Informatique et des Libertés (CNIL, French National Commission for Data Protection). The baseline data concerning patients, strictures, and treatment modalities were collected after local IRB approval and declaration of the database (PADS 20-391).
Endoscopic procedures
All endoscopic dilation procedures were performed under general anesthesia. The first dilation was always performed under fluoroscopic control after opacification to characterize the stricture and place a guide wire. Procedures were scheduled for the majority of cases in ambulatory settings, unless short hospitalization after the endoscopy was required due to patient clinical conditions or residence location.
The choice whether the balloon or bougie procedure was performed and the first dilation diameter were dependent on the operator’s preference. Each patient underwent the same technique throughout treatment.
Balloon dilation procedures were performed with through-the-scope (TTS) controlled radial expansion (CRE) (Boston Scientific Corporation, Natick, USA) or Hercules (Cook Endoscopy, Salem, USA) dilation balloons. During each session, the expansion diameter was not increased by more than 3 mm. Dilations using Savary-Gilliard bougies were carried out under fluoroscopic guidance with insertion of a Savary guidewire. Three bougies of successively increasing diameters (according to "the rule of three") were placed from the moment when the operator felt resistance to the passage of the bougies through the stricture.
After the procedure, patients were systematically administered oral proton pump inhibitors.
Dilation strategies
Since 2012, two physicians in our unit have changed their therapeutic protocol and have decided to apply scheduled dilations in patients with strictures at risk of becoming refractory (caustic, post-surgical, narrow strictures < 3–4 mm). Other physicians continued to perform dilations on demand during the study period.
For the study analysis, patients were divided in two groups based on the operators’ strategy: (i) a scheduled dilatation group (SDG). This included patients who underwent five dilations during the four initial months, with the remaining dilations during the following year. (ii) An ON-DEMAND group (ODG), including patients dilated only in the event of dysphagia recurrence.
Basically, the scheduled dilatation program was as follows: three first dilations were performed with a two-week interval, and then the two following dilations were performed with a four–six-week interval, a total maximum period of four months. After the fifth initial dilation performed within a four-month period, the patient was offered dilation with a three-month interval for at least one year. Upon dysphagia recurrence too early during the interval, the patient was offered a return to a one-month interval. The use of SEMS was down to the physician’s discretion in agreement with the patient. It was considered for patients when repeat dilations were required at very short intervals as a temporary respite solution; dilations were continued thereafter. Esophageal SEMS used were always fully covered with a classic shape, from Taewong, with a 22 mm internal diameter and a length varying from 8 to 12 cm. The choice of SEMS type was decided by the physician.
Study objectives and outcomes
The main objective was to assess the clinical success rate and the time taken to reach clinical success.
The secondary objectives were to evaluate the number of dilation sessions required, the complication rate, and the effects of SEMS placement.
Definitions
Patients were considered as a “Clinical success” if they were able to eat soft solids without dysphagia recurrence during at least one year after the last dilation.
Patients were considered as a “Failure” if they had dysphagia with soft diet, if they underwent esophageal surgery, if any enteral or parenteral feeding was needed, or if dilation was performed less than one year ago since the last dilation.
Adverse events
We classified adverse events according to three types of complications: (i) complications related to procedures requiring a new endoscopy, (ii) perforations directly related to dilation, and (iii) complications related to esophageal SEMS (migration, stricture budding in the upper pole, fistula in the upper pole).
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics version 20.0 (Inc., IL., USA). Continuous variables are presented as mean ± standard deviation or as median with the first and third quartiles. Categorical variables are presented as numbers and percentages. The relationship between categorical variables was assessed using the Pearson’s Chi-squared test or the Fisher’s exact test if the theoretical numbers were below five. The relationship between a qualitative and a quantitative variable was evaluated using the Mann–Whitney or Wilcoxon tests. The correlation between the quantitative variables was analyzed by the Pearson correlation test. A correlation threshold R > 0.5 was required to define a strong correlation between two quantitative variables. Survival curves were plotted using the Kaplan–Meier approach using the log-rank test. A p-value of p < 0.05 defined statistical significance for all analyses. For the comparison between the ODG and SGD groups, the patients in the SGD group were matched in 1:1 ratio with patients with the same stricture etiology in the ODG group.
Results
Study population
Between October 2003 and January 2019, 806 esophageal dilatations were performed on 228 patients for non-malignant esophageal strictures. Out of these 228 patients, 39 (17 females) with refractory stenosis were included for study analysis (> 5 dilations). 13 patients were included in a SDG program. Among them, 3 were not included because they were not refractory and presented an improvement of dysphagia with a good calibration at the 3rd or 4th endoscopy. The etiologies of the stenoses and patient characteristics are presented in Table 1. Overall, there were 29 ODG patients and 10 SDG patients.
Modality of endoscopic treatment (Table 2)
A total of 455 dilations were performed on the 39 patients. The device used was a hydraulic balloon (CRE, Boston Scientific, USA) for 380 dilations (83.6%) and Savary-Gilliard bougies for 75 (16.4%) dilations.
The median number of dilations per patient was 11 [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]. There were 10.3 ± 4.2 dilations in the ODG group vs 15.3 ± 6.2 dilations in SDG group (Table 3) (p = 0.049).
The mean follow-up period was 64.4 ± 32 months.
Results of the endoscopic treatment
Success rate (Table 2)
At the end of follow-up, 79.5% (31/39) of patients were considered as achieving clinical success, 5.1% (2/39) were still undergoing endoscopic treatment (last dilation < 1 year), and 15.4% (6/39) were considered as a failure. The final success rate did not significantly differ between ODG and SDG patients (80% vs 90%; NS) (Table 3).
Factors influencing the success rate
Univariate analysis did not identify any factors as being associated with a higher success rate. There was no significant association between the etiology, the length, and the localization of strictures with the success rate (p = 0,539, p = 0.512, p = 0.474, respectively).
Duration of treatment and dilation intervals
The mean treatment duration was 27.3 ± 20 months. The inter-dilation intervals significantly increased over time in our population (R = − 0.683, p < 0,001). In the first trimester, patients underwent an average of 3.2 ± 1.5 dilations per trimester. Then, starting from the fifth trimester of treatment, the interval between dilations decreased to less than one dilation per trimester. After 18 months, patients underwent an average of 0.38 dilations per trimester and 0.56 dilations per semester (Fig. 1).
The treatment duration was lower in the SDG group; 41.4 ± 27.9 months in the ODG group vs 18.8 ± 12.7 months in the SDG group (p = 0.032) (Table 3). Kaplan–Meier survival analysis showed that SDG patients had faster remission (log-rank test; p = 0,047) compared to ODG patients (Fig. 2).
Complications
Fourteen patients (35.9%) had complications during endoscopic treatment. Two patients underwent esophageal perforation following hydraulic dilation (0.04% of all dilations). These perforations were successfully treated by SEMS insertion in the same procedure. One patient had an episode of upper GI bleeding 48 h after dilation and one patient had a large mucosal dilaceration without perforation, preventively treated with SEMS.
Nine of these 14 complications were related to SEMS with the need for a re-intervention: three fistulas (two trachea-esophageal fistulas), three impactions causing dysphagia, two migrations, and one hemorrhagic stripping during stent removal. The placement of a SEMS was significantly associated with the occurrence of complications. The overall complications rate was 5.9% in patients without SEMS (1/17 patients) vs 59.1% in patients with SEMS (13/22 patients) (p = 0.001). A re-intervention was more frequent in patients with SEMS: 50% with SEMS (11/22 patients) vs 5.9% without SEMS (1/17) (p = 0.003).
Outcome of patients considered as a failure (Fig. 3)
Eight patients were considered a failure. Two were still undergoing dilations at the end of the follow-up and therefore lacked the one-year follow-up without dysphagia required to be considered a success. One patient died during management because of a tracheo-esophageal fistula due to an esophageal SEMS. Five patients underwent surgery: one with esogastric anastomosis and four with retrosternal esophagocoloplasty with esocolic anastomosis. Among the patients operated on, one died as a result of the operation (colonic interposition) and the four other patients presented an improvement in dysphagia.
Discussion
The success of endoscopic dilations in the literature varies according to the definitions of success used. For strict naïve dilation, the success rate is between 80 and 98% [20, 21]. Our patient series here showed a success rate of 79.5% for all causes in a specific population of more severe and refractory strictures. This success rate is considerably higher than results in the literature, showing a success rate of 88% in naïve patients with the same definition of success [20].
Our series of 39 patients with refractory strictures highlights the potential effect of proposing an early and aggressive dilatation program from the outset of management of patients with risk factors for long-acting strictures. Our analysis showed the probability of a faster recovery in time for patients having received a scheduled management compared to patients dilated “on demand”. Due to our relatively small patient group, our study series failed to reach statistical significance for several other outcomes: there was a non-significant trend towards higher success rate (90% vs. 75.9%, p = 0.568) in patients who received scheduled dilations, with only one failure in this group of 10 patients.
Besides the UK guidelines [19], there are minimal data supporting an early and aggressive management of BES. Only a single study has shown less recurrence and a shorter treatment duration for patients who underwent more initial phase dilations [22]. Thus, our findings reinforce the 2017 UK guidelines [19]. These recommend dilation every 15 days until a diameter of 15 mm is achieved in order to favor faster resolution. The role of surgery is not well defined in the UK guidelines due to limited data availability. However, it is suggested that surgery could be offered to patients who do not respond or who are intolerant to other measures (weak recommendation).
The surgical management of refractory stricture remains largely documented in caustic injuries when the procedure performed can be a retrosternal colonic interposition with esocolic anastomosis, or esogastric anastomosis depending on stomach vitality. In these such cases, there does not seem to be a difference in prognosis between resection and stricture bypass, with an improvement rate in dysphagia of approximately 80% [18].
Regarding the natural history and evolution of esophageal stricture, an analogy can be made with anastomotic strictures in liver transplant patients; calibration time is long and an aggressive management is recommended with an increased number of plastic stents for a prolonged period [23]. In this way, a stricture can combine with an excessive healing process given that hypertrophic or keloid scars can occur. Hypertrophic scars are characterized by excessive fibrogenesis leading to hypertrophy of the initial wound for a long period of more than 18 months [24]. Unlike keloid scars, hypertrophic scars tend to improve steadily after a very long period (> 18 months) [25]. A high proportion of BES in our patient series followed a somewhat similar behavior to hypertrophic scars, with better outcomes after 18 months of management (Fig. 1). The main treatment for hypertrophic skin scars is pressure therapy because mechanical forces have been shown to induce scar remodeling with histological improvement and reorganization of the extracellular matrix [26]. There are limited data on the in vitro effect of endoscopic dilations. However, considering the better therapeutic results in patients with short dilation intervals, we could hypothesize that dilation acts in the same way as pressure therapy and results in a potential decrease in the pro-fibrotic mechanisms described above.
Therefore, persisting with stricture dilation appears to be the main strategy to propose to patients with refractory BES because (i) the success rate is good, (ii) success can be achieved very late in management, and (iii) alternatives to endoscopic treatment have higher morbidity rates (decreased quality of life with enteral nutrition, and risk of mortality of 4–6% and 18.7%–36% of dysphagia recurrence with esophageal reconstruction surgery) [18, 27].
However, surgical management of refractory stricture could remain an option in a number of cases. We recognize that this should be considered according to the risk–benefit assessment and in agreement with the patient. This is particularly in the case of complications related to the stenosis or endoscopic management (aspiration, fistula, etc.) or when patients are intolerant to repeat endoscopic dilations.
In contrast to the UK guidelines [19], we excluded SEMS insertion from our therapeutic algorithm. This is because it showed not only a higher rate of adverse events, but it is also a temporary solution with a dysphagia recurrence rate of approximately 69% after SEMS removal [28].
We are conscious that this study series has several limitations since it is a single-center and retrospective study. However, BES is a rare and heterogeneous condition and we initially wanted to restrict the study to our center to limit the number of different procedure practices (each patient was treated by the same physician with the same technique in our center). Additionally, we carried out a matched analysis in order to limit the biases induced by the different stricture etiologies within our population. The results of this study must be interpreted with caution due to the very small number of patients and the heterogeneity in the etiologies of the strictures. We consider that we cannot draw any formal conclusions from these data. However, we recognize that it was important to describe our results as they form the basis of reflection for the development of subsequent prospective studies that are required to confirm the potential benefits of a scheduled program of esophageal dilatations.
In conclusion, this study demonstrated that the management of BES with endoscopic dilation is safe and effective in 80% of cases. It additionally highlighted the potential impact of an early aggressive scheduled dilatation program in cases of strictures with high risk of recurrence (anastomotic, caustic, or tight and narrowing). Our analysis demonstrated that an early and aggressive scheduled dilatation program was indeed associated with a shorter duration of treatment.
From a practical point of view, it is important to inform the patients that the treatment is long (> one year). On the other hand, their quality of life will be increasingly less affected over time given the need for dilation decreases drastically after 18 months, resulting in the requirement of less than one dilation per semester.
References
Pereira-Lima JC, Ramires RP, Zamin I et al (1999) Endoscopic dilation of benign esophageal strictures: report on 1043 procedures. Am J Gastroenterol 94:1497–1501
Kochhar R, Makharia GK (2002) Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointest Endosc 56:829–834
Cox JG, Winter RK, Maslin SC et al (1988) Balloon or bougie for dilatation of benign oesophageal stricture? An interim report of a randomised controlled trial. Gut 29:1741–1747
Yamamoto H, Hughes RW, Schroeder KW et al (1992) Treatment of benign esophageal stricture by Eder-Puestow or balloon dilators: a comparison between randomized and prospective nonrandomized trials. Mayo Clin Proc 67:228–236
Saeed ZA, Winchester CB, Ferro PS et al (1995) Prospective randomized comparison of polyvinyl bougies and through-the-scope balloons for dilation of peptic strictures of the esophagus. Gastrointest Endosc 41:189–195
van Boeckel PGA, Siersema PD (2015) Refractory esophageal strictures: what to do when dilation fails. Curr Treat Options Gastroenterol 13:47–58
Repici A, Small AJ, Mendelson A et al (2016) Natural history and management of refractory benign esophageal strictures. Gastrointest Endosc 84:222–228
Kochman ML, McClave SA, Boyce HW (2005) The refractory and the recurrent esophageal stricture: a definition. Gastrointest Endosc 62:474–475
Ramage JI, Rumalla A, Baron TH et al (2005) A prospective, randomized, double-blind, placebo-controlled trial of endoscopic steroid injection therapy for recalcitrant esophageal peptic strictures. Am J Gastroenterol 100:2419–2425
Altintas E, Kacar S, Tunc B et al (2004) Intralesional steroid injection in benign esophageal strictures resistant to bougie dilation. J Gastroenterol Hepatol 19:1388–1391
Hirdes MMC, van Hooft JE, Koornstra JJ et al (2013) Endoscopic corticosteroid injections do not reduce dysphagia after endoscopic dilation therapy in patients with benign esophagogastric anastomotic strictures. Clin Gastroenterol Hepatol 11(795–801):e1
Camargo MA, Lopes LR, de Grangeia T et al (2003) Use of corticosteroids after esophageal dilations on patients with corrosive stenosis: prospective, randomized and double-blind study. Rev Assoc Med Bras 49:286–292
Hordijk ML, Siersema PD, Tilanus HW et al (2006) Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc 63:157–163
Yano T, Yoda Y, Satake H et al (2013) Radial incision and cutting method for refractory stricture after nonsurgical treatment of esophageal cancer. Endoscopy 45:316–319
Hordijk ML, van Hooft JE, Hansen BE et al (2009) A randomized comparison of electrocautery incision with Savary bougienage for relief of anastomotic gastroesophageal strictures. Gastrointest Endosc 70:849–855
Eloubeidi MA, Talreja JP, Lopes TL et al (2011) Success and complications associated with placement of fully covered removable self-expandable metal stents for benign esophageal diseases (with videos). Gastrointest Endosc 73:673–681
Fuccio L, Hassan C, Frazzoni L et al (2015) Clinical outcomes following stent placement in refractory benign esophageal stricture: a systematic review and meta-analysis. Endoscopy 48:141–148
Javed A, Pal S, Dash NR et al (2011) Outcome Following Surgical Management of Corrosive Strictures of the Esophagus. Ann Surg 254:62–66
Sami SS, Haboubi HN, Ang Y et al (2018) UK guidelines on oesophageal dilatation in clinical practice. Gut 67:1000–1023
Chiu Y-C, Hsu C-C, Chiu K-W et al (2004) Factors Influencing Clinical Applications of Endoscopic Balloon Dilation for Benign Esophageal Strictures. Endoscopy 36:595–600
Park JY, Song H-Y, Kim JH et al (2012) Benign Anastomotic Strictures After Esophagectomy: Long-Term Effectiveness of Balloon Dilation and Factors Affecting Recurrence in 155 Patients. Am J Roentgenol 198:1208–1213
Saeed ZA, Ramirez FC, Hepps KS et al (1997) An objective end point for dilation improves outcome of peptic esophageal strictures: a prospective randomized trial. Gastrointest Endosc 45:354–359
Tringali A, Barbaro F, Pizzicannella M et al (2016) Endoscopic management with multiple plastic stents of anastomotic biliary stricture following liver transplantation: long-term results. Endoscopy 48:546–551
Wolfram D, Tzankov A, Pülzl P et al (2009) Hypertrophic scars and keloids–a review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg 35:171–181
Mahdavian Delavary B, van der Veer WM, Ferreira JA et al (2012) Formation of hypertrophic scars: evolution and susceptibility. J Plast Surg Hand Surg 46:95–101
Costa AM, Peyrol S, Pôrto LC et al (1999) Mechanical forces induce scar remodeling Study in non-pressure-treated versus pressure-treated hypertrophic scars. Am J Pathol 155:1671–1679
Chirica M, Veyrie N, Munoz-Bongrand N et al (2010) Late Morbidity After Colon Interposition for Corrosive Esophageal Injury. Ann Surg 252:271–280
Kim JH, Song H-Y, Choi EK et al (2009) Temporary metallic stent placement in the treatment of refractory benign esophageal strictures: results and factors associated with outcome in 55 patients. Eur Radiol 19:384–390
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Marc Barthet, Véronique Vitton, Jean-Michel Gonzalez, MD. Véronique Vitton, and Antoine Debourdeau declare that they have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Debourdeau, A., Barthet, M., Benezech, A. et al. Assessment of long-term results of repeated dilations and impact of a scheduled program of dilations for refractory esophageal strictures: a retrospective case–control study. Surg Endosc 36, 1098–1105 (2022). https://doi.org/10.1007/s00464-021-08376-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08376-3