Abstract
Background
The identification of metastatic lymph nodes is one of the most important prognostic factors in gastrointestinal (GI) cancers. Near-infrared fluorescence (NIRF) imaging has been successfully used in GI tumors to detect the lymphatic pathway and the sentinel lymph node (SLN), facilitating fluorescence image-guided surgery (FIGS) with the purpose to achieve a correct nodal staging. The aim of this study was to analyze the current results of NIRF SLN navigation and lymphography through data collected in the EURO-FIGS registry.
Methods
Prospectively collected data regarding patients and ICG-guided lymphadenectomies were analyzed. Additional analyses were performed to identify predictors of metastatic SLN and determinants of fluorescence positivity and nodal metastases outside the boundaries of standard lymphadenectomies.
Results
Overall, 188 patients were included by 18 surgeons from 10 different centers. Colorectal cancer was the most reported pathology (77.7%), followed by gastric (19.1%) and esophageal tumors (3.2%). ICG was injected with higher doses (p < 0.001) via extraparietal side (63.3%), and with higher volumes (p < 0.001) via endoluminal side (36.7%). Overall, NIRF SLN navigation was positive in 75.5% of all cases and 95.5% of positive SLNs were retrieved, with a metastatic rate of 14.7%. NIRF identification of lymph nodes outside standard lymphatic stations occurred in 52.1% of all cases, 43.8% of which were positive for metastatic involvement. Positive NIRF SLN identification was an independent predictor of metastasis outside standard lymphatic stations (OR = 4.392, p = 0.029), while BMI independently predicted metastasis in retrieved SLNs (OR = 1.187, p = 0.013). Lower doses of ICG were protective against NIRF identification outside standard of care lymphadenectomy (OR = 0.596, p = 0.006), while higher volumes of ICG were predictive of metastatic involvement outside standard of care lymphadenectomy (OR = 1.597, p = 0.001).
Conclusions
SLN mapping helps identifying potentially metastatic lymph nodes outside the boundaries of standard lymphadenectomies. The EURO-FIGS registry is a valuable tool to share and analyze European surgeons’ practices.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In gastrointestinal (GI) cancers, the presence or absence of metastatic lymph nodes (LN) is one of the most important prognostic factors and potentially drives the indication for adjuvant treatment (chemo/radiotherapy) [1, 2].
Consequently, the appraisal of regional LN involvement is crucial to achieve a correct nodal staging in oncological GI resections.
In recent years, several analyses investigated the prognostic impact of different approaches, such as sentinel lymph nodes (SLNs) assessment, the location of LN metastases, and lymphatic mapping navigation systems, with mixed results.
SLNs are defined as the first lymph nodes in the lymphatic pathway draining a primary solid malignancy [3]. SLN navigation is an oncologically validated approach for early-stage gastric cancer in Eastern countries [4], and although it remains controversial in the management of colorectal cancer, it may improve the staging of patients by performing ultrastaging methods on SLNs to identify occult micro-metastases missed when using conventional histopathological examination [5,6,7]. The SLN identification can be achieved with a peritumoral injection of a dye (generally a blue dye) combined or not with gamma-ray emitting radiotracers. However, blue dyes cannot be easily visualized through adipose tissue, and the localization of radiotracers accumulated in the nodes with the γ-probe exposes patients and caregivers to ionizing radiations, requiring the involvement of a nuclear medicine facility and inducing high management costs [5, 8, 9].
Additionally, nodal navigation could help to identify LNs outside the boundaries of regulated lymphadenectomy, subsequently allowing for a tailored extended lymphadenectomy. Near-infrared fluorescence (NIRF) with indocyanine green (ICG) has emerged as an effective technique to identify LNs intra-operatively and consequently has been successfully applied in patients with various tumor types, including GI cancers. Although several reviews demonstrated the high sensitivity of NIRF for lymphatic pathways and SNL detection [10,11,12], its routine use is still not supported by universally accepted and shared guidelines. Moreover, surgeons usually adopt different techniques based on personal experience and preference.
An international registry, collecting huge amounts of data from various centres, could be an important tool to analyze and standardise those data thus substantially contributing to create guidelines.
The aim of the present study group was to create a tool to collect high-volume data and share the experiences of surgeons regarding NIRF in order to facilitate collaborations between European surgical centers and promote scientific comparisons. For this reason, based on the collaboration between the Research Institute against Digestive Cancer (IRCAD, Strasbourg), the Institute of Image Guided Surgery (IHU, Strasbourg) and the Technology Committee of the European Association for Endoscopic Surgery (EAES), a European registry on fluorescence image-guided surgery (EURO-FIGS), funded by the Association for Cancer Research (ARC, France) and held in the IHU-IRCAD facilities, was launched.
Currently, the registry is collecting data on the following topics: (I) near-infrared cholangiography (preliminary results published in 2019 [13]), (II) bowel anastomosis perfusion evaluation (preliminary results published in 2020 [14]), (III) fluorescence-based lymphography, analyzed in this study.
The primary aim of this study was to describe the EURO-FIGS Registry on NIRF applied to SLN navigation, illustrate the current status of NIRF lymphography in GI oncological resections, and assess the standard practice across centers on FIGS.
Materials and methods
The registry
The EURO-FIGS registry (https://www.euro-figs.eu) is a secured online platform that primarily aims to prospectively collect centralized data on fluorescence guidance applications in various surgical settings. This database, which is accessible to members only, includes anonymized cases performed using FIGS. The EURO-FIGS registry, was approved by the University of Strasbourg and by the French authority protecting privacy, which reports to the French Data Protection Authority (CNIL: Commission Nationale de l’Informatique et des Libertés or “National Commission for Data Protection and Liberties”), under the reference number 2007309v0. Participants in the network of the principal investigator (MD) were invited to register their cases. Written informed consent was obtained from all included patients and retrieved by the submitting Institutions. The consent form was drafted in English, Italian, and French but possibly translated into different national languages.
Study design and data collection
This is a multicenter, registry-based, observational study. Given the descriptive and non-interventional design of the EURO-FIGS registry, surgeons were encouraged to describe their experience and the institutional practice with FIGS. Moreover, as the EURO-FIGS registry aims to allow comparisons across practitioners, institutions, and countries, no standard recommendations or technical restrictions were fixed.
Demographics, operative details including NIRF procedures, ICG-related adverse events, and pathological features were retrieved through a combination of multiple-choice and open-ended questions (Appendix A) and prospectively collected.
Preoperative characteristics included age, sex, BMI (kg/m2), and country of origin of included centers. Intraoperative data consisted of the type of surgery (colorectal, gastric, and esophageal) and fluorescence imaging types of equipment. NIRF technique for SLN detection (even possible frozen section) and LN mapping was assessed and performed using a peritumoral ICG bolus injection. Injection site, ICG dosing (mg/ml), and the IGG injected volume (ml) were retrieved.
SLN was defined as the first lymph node in the lymphatic pathway receiving drainage from the primary solid malignancy [3]. The following variables have been considered and analyzed: SLN identification, retrieval, and involvement.
As positive nodes can be located beyond the borders of standard nodal dissections, fluorescent nodes identified outside the boundaries of a standard of care lymphadenectomy, their retrieval, and histology were evaluated.
Specialized pathologists analyzed all the specimens at each participant Institution. Data regarding preoperative imaging study or clinical stage were not collected in the registry.
Technology application
NIRF was performed after peritumoral injection of ICG, via flexible endoscopy for endoluminal submucosal administration, or via laparoscopy for extraparietal application. Dosing, site of ICG injection, distance between the camera and the target organ, fluorescence imaging equipment and all other procedural steps depended on surgeons’ preferences.
Statistical analysis
Continuous variables were expressed as mean with standard deviation (±SD) and were compared using the Student’s t test or the Mann-Whitney U test, as appropriate. Categorical variables were reported as absolute numbers and percentages (%) and compared using the Chi-square or Fisher's exact test, as appropriate. Backward stepwise logistic regression analyses were performed to identify possible predictors of metastatic lymph node identification through NIRF. The variables were assessed for multicollinearity and were removed from the model when necessary. Only statistically significant variables (p<0.05) at univariate analysis were included in the full multivariable model. Logistic regression analysis was not applied for the esophageal cancer group due to the small size of the population. Two-tailed p values were considered statistically significant when less than 0.05. All analyses were performed using SPSS software (IBM SPSS Statistics for Windows, Version 25.0 Armonk, NY: IBM Corp).
Results
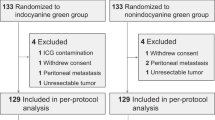
Overall, 18 surgeons from 10 centers (Contributing Centers are listed in Appendix B) were involved in the study. The distribution per country was as follows: Italy (n = 138), Spain (n = 45) and Romania (n = 5). A total of 188 patients (103 men / 85 women) with available data on NIRF for LN detection were recorded in the WEB-based EURO-FIGS registry from July 2017 to March 2021 and included in the analysis. The most common surgical resection was for colorectal cancer (77.7%), followed by gastric cancer (19.1%), and esophageal cancer (3.2%). Baseline and operative characteristics of the entire population are listed in Table 1.
NIR cameras
The following NIR cameras were used: D-Light-P (Karl Storz, Germany, n=73), SPY (Stryker, USA, n=47), PINPOINT (Novadaq, Canada, n=28), Firefly (Intuitive Surgical, USA, n=23), VISERA ELITE (Olympus, Japan, n=10), and Artemis Spectrum® (Quest Medical Imaging BV, Netherlands, n=6).
ICG injection methods, dose and volume
ICG was injected through the extraparietal side (EPS) during laparoscopic procedures in most cases (63.3%). In 69 patients (36.7%), however, ICG was injected through the endoluminal side (ELS) using endoscopy. Of note, in 9 colorectal cancer cases, ICG was injected submucosally in the peritumoral tissue after the specimen extraction (ex vivo).
ICG dose and volume
The dose and the volume of ICG varied significantly within the entire population (Fig. 1). Overall, ICG doses varied between 0.083 mg/mL and 5 mg/mL, with a median of 1.12 mg/mL. The mean dose of ICG was significantly higher in ELS procedures compared to EPS procedures (p<.001). By contrast, the mean volume of the fluorophore was significantly higher via EPS injection compared to the ELS one (p<.001) (Fig. 2). After stratification for the surgical indication, ICG volume and dose significantly differed in colorectal surgery (all p<0.001), but were similar between EPS and ELS injection in both gastric and esophageal procedures. (Table 2).
NIRF SLN detection
Overall, NIRF SLN detection was achieved in 142 cases (75.5%) regardless of the type of the technique used, while it was not performed by surgeons in the remaining patients. Among the included cases, 52 were obtained via ELS (36.6%) and 90 (63.4%) via EPS injection approach. SLNs were retrieved in 136 (95.8%) patients and further classified as metastatic in 20/136 cases (14.7%). Frozen sections were performed in 13 cases (9.6%). None of SLNs retrieved after ex vivo injection in colorectal cases resulted metastatic. SLN detection rate with NIRF, SLN retrieval, and the number of positive SLN stratified according to the surgical procedure are reported in Table 3.
NIRF identification of lymph nodes beyond the planned lymphadenectomy (according to oncological standards)
As showed in Table 3, NIRF detected a lymphatic drainage located beyond the borders of standard nodal dissections in more than a half of patients, and 98% of the detected LNs were retrieved. Among these, 43.8% showed a metastatic involvement and the rate of frozen section was 8.3%. Fluorescence visualization of such nodal stations did not differ between EPS and ELS ICG injection in the overall population and also once stratified by surgical procedures. CRC population had higher rate of metastatic involvement after retrieval of fluorescent lymph nodes outside the boundaries of a standard of care lymphadenectomy (45.8%) when compared to GC (35%), while EsC showed nodal involvement in 2/4 retrieved cases.
Predictors of NIRF identification of metastatic SLNs
Patients with higher BMI had higher probability to present metastatic SLNs, as shown by univariate (OR=1.158, p=.008) and multivariate analysis (OR=1.187, p=.013) (Supplementary Table 1).
Predictors of NIRF positivity outside the boundaries of a standard of care lymphadenectomy
The identification of metastatic SLNs increased the risk of NIRF identification of lymph nodes outside the boundaries of a standard of care lymphadenectomy only in the CRC population, as shown by univariate (OR=5.500, 95% CI=1.152–26.266, p=.033) and multivariate (OR=6.876, 95% CI=1.366–34.619, p=.019) regression analysis (Supplementary table 2).
Predictors of nodal metastases outside the boundaries of a standard of care lymphadenectomy
Endoscopic submucosal injection of ICG for CRC was the best method to detect metastatic extraregional LNs, at both univariate (OR=11.667, 95% CI=3.044–44.717, p<.001) and multivariate (OR=11.730, 95% CI=2.065–66.618, p=.005) regression model (Supplementary Table 3)
ICG-related adverse events
There were no adverse events. An intraperitoneal spillage of ICG occurred in 4 cases, making NIRF unapplicable.
Discussion
The appraisal of the nodal involvement is a crucial step in the treatment of gastrointestinal tumors, hence determining the potential need for (neo)adjuvant chemoradiotherapy. Right and precise nodal mapping and lymphadenectomy are mandatory, and are one of the main goals of oncologic surgeons. However, in spite of regulated and standardized lymphadenectomies, a certain rate of "node negative disease (NND)" patients continue to experience local recurrence [11, 15, 16].
Several techniques were reported to improve right nodal staging and subsequently reduce the local recurrence rate, varying from ultrastaging techniques of NND SLN(s) to extended lymphadenectomy outside the boundaries of a standard of care lymphadenectomy. However, there is no current consensus on the best protocol for nodal mapping (and staging) or lymphography [7, 11, 17, 18].
NIRF nodal mapping has been shown to allow for the detection of sentinel and locoregional lymph nodes in gastrointestinal malignancies. However, results were not compelling as methods were not standardized, particularly in terms of dosing and timing of ICG administration [6, 11, 19,20,21,22,23,24].
In this study, we presented the results of the EURO-FIGS registry on SLN mapping and lymphography in GI tumors with the aim to share European experiences to rapidly collect high-volume data.
Regarding the overall population, differences were noted regarding the injection method, with a higher rate of extraparietal side vs endoluminal side injection. However, the biggest differences were observed in ICG dose and volume. The mean dose was higher in ELS procedures, while mean volume was higher in EPS procedures. These preliminary findings suggest that a lower concentration of die could be enough for lymph nodal navigation after EPS injection of the die. These data are in line with those reported in the literature [6] and confirmed in our study’s colorectal cancer population. In spite of this huge data variability, the injection method, as well as ICG dose and volume, do not seem to influence the identification of SLN via NIRF except for gastric cancer population (but only in the univariate analysis) (Supplementary table 1).
NIRF SLN navigation was positive in the overall population in 75.5% of cases. In colorectal, gastric, and esophageal cancer population, the detection rate was 72.6%, 86.1%, and 83.3%, respectively, while the lymph node metastatic rate was 14.7%. These rates are slightly lower than others reported in the literature [6, 11, 25], but still similar, thereby confirming the efficacy of this method, although with the well-known limitations of the SLN identification for malignancies [26].
The 9 cases of “ex vivo” SLN research, were added at the dawn of NIRF and the registry itself (July 2017). Ex vivo SLN fluorescence-based detection in CRC hesitated in a metastatic lymph nodes and was concordant with the final locoregional nodes status. However, the real potential of this technique stands in the opportunity to find SLN (even in an extracorporeal setting) to be further analyzed by ultrastaging techniques to find micro-metastases [7].
The factors analyzed as potential predictors of SLN NIRF identification showed that only the presence of metastasis outside the boundaries of a standard of care lymphadenectomy could be considered as a predictor. Although the presence of metastasis in the identified SLN was extremely (or even obviously) related to SLN NIRF identification (OR 12.547^8), it was not statistically significant and not further investigated.
By analyzing the factors which could affect the presence of metastatic LNs in the overall population, only BMI and the presence of metastasis outside the boundaries showed this relationship. Regarding the colorectal cancer population, the univariate analysis maintained only the NIRF identification of LNs outside the boundaries. When considering the NIRF identification of LNs outside the boundaries of a standard of care lymphadenectomy, it resulted positive in about half (52.1%) of cases. This rate was slightly higher than with standard lymphadenectomy, as also reported by Kwon et al. [27]. In particular, with the use of NIRF or not, the NIRF group showed a significantly greater number of LNs retrieved (mostly outside the boundaries).
Regarding the factors which could predict NIRF positivity outside the boundaries, the univariate and multivariate analyses allowed to identify the mean dose of the fluorophore as a predictor in the overall population. The multivariate analysis also maintained the female gender and mostly the presence of metastatic SLN as independent predictors. These data were confirmed in the colorectal cancer population only and could well suggest the lymphadenectomy to be extended outside the boundaries of colorectal standard of care lymphadenectomy when the NIRF identification is positive.
These findings are difficult to construe and data are lacking in the literature. This correlation could be explained by the propensity of surgeons to perform a preoperative endoluminal injection in more advanced stage tumors, hence explaining such noteworthy data. Obviously, this could be a valuable starting point for future studies.
Many authors reported that significantly more LNs were harvested in the ICG group than the non-ICG group, even and especially outside the boundaries of a standard of care lymphadenectomy [11, 27, 28].
Villegas-Tovar performed a diagnostic test accuracy meta-analysis, confirming high (91%) detection rates when using ICG for LNs mapping in colorectal surgery, also reporting that the overall performance of ICG for the detection of metastatic nodes is poor [25].
The use of international registries, thanks to the big data collected instead of single centers studies, is evermore spreading in the surgical scientific researches.
Notwithstanding the interesting findings and results, this study and the EURO-FIGS registry have several limitations. First, the registry is still confined to the PI network and strongly limited by specific regulations in some European countries, subsequently hindering the proper understanding of the use of FIGS in Europe. Second, although the registry provided for three digestive tract procedures, the majority of cases involved colorectal procedures, according to the epidemiological series in Western countries. The small number of collected esophageal cancers (only four cases) was not representative at all and did not allow them to be included in the specific statistical analysis. Third, in its current form, the registry does not include data on preoperative imaging study, postoperative course and oncological features and follow-up, resulting in the inability to determine the effect of extended ICG-guided lymphadenectomy on postoperative outcomes and prolonged disease-free survival, the preclusion to find correlations between preoperative radiological work-up, and not include data on timing before and during ICG injection. Moreover, right colonic resections were not included in the registry, and differences between left colonic or rectal resections, total or subtotal gastrectomy, and type of esophagectomy were not reported. These data will be implemented in the future versions of the registry.
The NIRF is a validated tool in the hands of surgeons, in order to better stage (via ultrastaging techniques) patients and not to leave potential metastatic LNs outside the boundaries. However, it needs new validated fluorophores which could be targeted to specific tumoral markers. In the next years, the routine use of innovative techniques and software to improve the detection of metastatic LNs could widely spread. Augmented reality imaging associated with powered algorithms and also video software fluorescence analysis could well enhance the visualization of oncological resection planes and vascular structures and act as an in situ tumor identifier with greater details [29, 30].
These results could let the surgeons perform more tailored surgical interventions, with the aim to reduce the rate of postoperative complications, and particularly the rate of local recurrence. These results could lead to direct worthwhile clinical applications and potentially provide the basis for a shared international consensus and European guidelines.
Conclusions
The EURO-FIGS fluorescence-based lymphography analysis pinpoints a huge disparity in terms of ICG dose, and injection methods across European centers. Notwithstanding this discrepancy, it has been confirmed to be a safe and valuable tool to perform real-time, non-ionizing, SLN mapping and to identify (potentially metastatic) LNs outside the boundaries of regulated lymphadenectomies.
In addition, the registry could be a helpful tool to share experience and promote European consensus guidelines.
References
Benson AB, Venook AP, Al-Hawary MM et al (2018) Nccn guidelines insights: colon cancer, version 2.2018. J Natl Compr Canc Netw 16(4):359–369. https://doi.org/10.6004/jnccn.2018.0021
Ajani JA, D’Amico TA, Almhanna K et al (2016) Gastric cancer, version 3.2016, nccn clinical practice guidelines in oncology. J Natl Compr Canc Netw 14(10):1286–1312. https://doi.org/10.6004/jnccn.2016.0137
Wiese D, Sirop S, Yestrepsky B et al (2010) Ultrastaging of sentinel lymph nodes (slns) vs. Non-slns in colorectal cancer–do we need both? Am J Surg. https://doi.org/10.1016/j.amjsurg.2009.08.032
Mitsumori N, Nimura H, Takahashi N et al (2014) Sentinel lymph node navigation surgery for early stage gastric cancer. World J Gastroenterol 20(19):5685–5693. https://doi.org/10.3748/wjg.v20.i19.5685
van der Pas MH, Meijer S, Hoekstra OS et al (2011) Sentinel-lymph-node procedure in colon and rectal cancer: a systematic review and meta-analysis. Lancet Oncol 12(6):540–550. https://doi.org/10.1016/S1470-2045(11)70075-4
Picchetto A, Seeliger B, La Rocca S et al (2019) fluorescence-guided detection of lymph node metastases of gastrointestinal tumors. Chirurg 90(11):891–898. https://doi.org/10.1007/s00104-019-01039-z
Picchetto A, Diana M, Swanström LL et al (2020) Upstaging nodal status in colorectal cancer using ex vivo fluorescence sentinel lymph node mapping: preliminary results. Minim Invasive Ther Allied Technol. https://doi.org/10.1080/13645706.2020.1798464
Vahrmeijer AL, Hutteman M, van der Vorst JR, van de Velde CJ, Frangioni JV (2013) Image-guided cancer surgery using near-infrared fluorescence. Nat Rev Clin Oncol 10(9):507–518. https://doi.org/10.1038/nrclinonc.2013.123
Schaafsma BE, Verbeek FP, van der Vorst JR et al (2013) Ex vivo sentinel node mapping in colon cancer combining blue dye staining and fluorescence imaging. J Surg Res 183(1):253–257. https://doi.org/10.1016/j.jss.2013.01.003
Jeremiasse B, van den Bosch CH, Wijnen MWHA, Terwisscha van Scheltinga CEJ, Fiocco MF, van der Steeg AFW (2020) Systematic review and meta-analysis concerning near-infrared imaging with fluorescent agents to identify the sentinel lymph node in oncology patients. Eur J Surg Oncol 46(11):2011–2022. https://doi.org/10.1016/j.ejso.2020.07.012
Huang Y, Pan M, Chen B (2021) A systematic review and meta-analysis of sentinel lymph node biopsy in gastric cancer, an optimization of imaging protocol for tracer mapping. World J Surg 45(4):1126–1134. https://doi.org/10.1007/s00268-020-05900-9
Puccetti F, Cinelli L, Genova L et al (2022) Applicative limitations of indocyanine green fluorescence assistance to laparoscopic lymph node dissection in total gastrectomy for cancer. Ann Surg Oncol 29(9):5875–5882. https://doi.org/10.1245/s10434-022-11940-3
Agnus V, Pesce A, Boni L et al (2019) Fluorescence-based cholangiography: preliminary results from the ihu-ircad-eaes euro-figs registry. Surg Endosc. https://doi.org/10.1007/s00464-019-07157-3
Spota A, Al-Taher M, Felli E et al (2021) Fluorescence-based bowel anastomosis perfusion evaluation: results from the ihu-ircad-eaes euro-figs registry. Surg Endosc. https://doi.org/10.1007/s00464-020-08234-8
Ong MLH, Schofield JB (2016) Assessment of lymph node involvement in colorectal cancer. World J Gastrointest Surg 8(3):179–192. https://doi.org/10.4240/wjgs.v8.i3.179
Smith DD, Schwarz RR, Schwarz RE (2005) Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large us-population database. J Clin Oncol 23(28):7114–7124. https://doi.org/10.1200/JCO.2005.14.621
Takahashi N, Nimura H, Fujita T et al (2017) Laparoscopic sentinel node navigation surgery for early gastric cancer: a prospective multicenter trial. Langenbecks Arch Surg 402(1):27–32. https://doi.org/10.1007/s00423-016-1540-y
Romanzi A, Mancini R, Ioni L, Picconi T, Pernazza G (2021) Icg-nir-guided lymph node dissection during robotic subtotal gastrectomy for gastric cancer. A single-centre experience. Int J Med Robot. https://doi.org/10.1002/rcs.2213
Hirche C, Mohr Z, Kneif S et al (2012) Ultrastaging of colon cancer by sentinel node biopsy using fluorescence navigation with indocyanine green. Int J Colorectal Dis 27(3):319–324. https://doi.org/10.1007/s00384-011-1306-5
Cahill RA, Anderson M, Wang LM, Lindsey I, Cunningham C, Mortensen NJ (2012) Near-infrared (nir) laparoscopy for intraoperative lymphatic road-mapping and sentinel node identification during definitive surgical resection of early-stage colorectal neoplasia. Surg Endosc 26(1):197–204. https://doi.org/10.1007/s00464-011-1854-3
Tummers QR, Boogerd LS, de Steur WO et al (2016) Near-infrared fluorescence sentinel lymph node detection in gastric cancer: a pilot study. World J Gastroenterol 22(13):3644–3651. https://doi.org/10.3748/wjg.v22.i13.3644
Liberale G, Vankerckhove S, Galdon MG et al (2016) Sentinel lymph node detection by blue dye versus indocyanine green fluorescence imaging in colon cancer. Anticancer Res 36(9):4853–4858. https://doi.org/10.21873/anticanres.11048
Currie AC (2019) Intraoperative sentinel node mapping in the colon: potential and pitfalls. Eur Surg Res 60(1–2):45–52. https://doi.org/10.1159/000494833
Baiocchi GL, Molfino S, Molteni B et al (2020) Fluorescence-guided lymphadenectomy in gastric cancer: a prospective western series. Updates Surg 72(3):761–772. https://doi.org/10.1007/s13304-020-00836-0
Villegas-Tovar E, Jimenez-Lillo J, Jimenez-Valerio V et al (2020) Performance of indocyanine green for sentinel lymph node mapping and lymph node metastasis in colorectal cancer: a diagnostic test accuracy meta-analysis. Surg Endosc 34(3):1035–1047. https://doi.org/10.1007/s00464-019-07274-z
Jeremiasse B, van den Bosch CH, Wijnen MWHA et al (2020) Systematic review and meta-analysis concerning near-infrared imaging with fluorescent agents to identify the sentinel lymph node in oncology patients. Eur J Surg Oncol 46(11):2011–2022. https://doi.org/10.1016/j.ejso.2020.07.012
Kwon IG, Son T, Kim HI, Hyung WJ (2019) Fluorescent lymphography-guided lymphadenectomy during robotic radical gastrectomy for gastric cancer. JAMA Surg 154(2):150–158. https://doi.org/10.1001/jamasurg.2018.4267
Liu M, Xing J, Xu K et al (2020) Application of near-infrared fluorescence imaging with indocyanine green in totally laparoscopic distal gastrectomy. J Gastric Cancer 20(3):290–299. https://doi.org/10.5230/jgc.2020.20.e25
Forgione A, Barberio M, Agnus V et al (2021) Precision image-guided colonic surgery: proof of concept for enhanced preoperative and intraoperative vascular imaging. Surg Endosc 35(2):962–970. https://doi.org/10.1007/s00464-020-08000-w
Dalli J, Loughman E, Hardy N et al (2021) Digital dynamic discrimination of primary colorectal cancer using systemic indocyanine green with near-infrared endoscopy. Sci Rep 11(1):11349. https://doi.org/10.1038/s41598-021-90089-7
Acknowledgements
The authors would like to thank: Guy Temporal and Christopher Burel, professionals in medical English proofreading, for their valuable assistance.
Funding
The EURO-FIGS registry is funded by a grant from the ARC Foundation for Cancer Research (9, rue Guy Môquet, 94803 Villejuif Cedex, France, https://www.fondation-arc.org), within the framework of the ELIOS (Endoscopic Luminescent Imaging for precision Oncologic Surgery) project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Michele Diana is the PI and the recipient of the ELIOS grant from the ARC Foundation and a member of the Advisory Board of Diagnostic Green. Salvador Morales-Conde reports grants and other relationships with Medtronic, BD Bard, Ethicon, Olympus, Karl Storz, Stryker, Dipro, Baxter, and B. Braun, outside the submitted work. Gian Luca Baiocchi is consultant of Stryker. Jacques Marescaux is the President of the IRCAD, which is partly funded by Karl Storz and Medtronic. Andrea Picchetto, Lorenzo Cinelli, Elisa Bannone, Lorenzo Casali, Giuseppe Spinoglio, Christian Franzini, Caterina Santi, Giancarlo D’Ambrosio, Catalin Copaescu, Alessio Rollo, Andrea Balla, Pasquale Lepiane, Alessandro M. Paganini, Paolo Detullio, Silvia Quaresima, Antonio Pesce, Tartamella Luciano, Giorgio Bianchi have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix A: List of items registered
-
Patient’s gender
-
Patient’s age
-
Patient’s BMI
-
Diagnosis (Esophageal cancer; Gastric cancer; ColoRectal cancer)
-
Surgical Procedure (Esophageal surgery, Gastric surgery, Colorectal surgery)
-
Camera type
-
Injection site
-
Dose of fluorophore (mg/mL)
-
How many mM injected?
-
ICG dose (mg/mL)
-
Adverse events of ICG administration?
-
Sentinel node(S) identification?
-
Sentinel node(S) retrieval?
-
Was the pathology positive for metastatic sentinel lymph node?
-
Did you visualize any fluorescent node(s) outside the boundaries of a standard of care lymphadenectomy?
-
Did you retrieve them?
-
Was the pathology positive for metastases in the other extra lymph nodes visualized?
-
Do you have any other comment(s)?
Appendix B: Contributing centers
University Hospital Virgen del Rocio | 35 |
AOU Policlinico Umberto I, Sapienza University of Rome | 17 |
Department of Clinical and Experimental Sciences, Brescia University—Italy | 36 |
Department of Medical and Surgical Sciences and Advanced Technologies “G.F. Ingrassia”—University of Catania | 1 |
Hospital Álvaro Cunqueiro | 7 |
Hospital Vithas Nuestra Señora de Fátima | 2 |
IEO (European Institute of Oncology), Milan, Italy | 22 |
Metabolic and Bariatric Surgery Center—Ponderas Acdemic Hospital | 4 |
Ospedale di Fidenza, AUSL Parma, Italy | 63 |
Ponderas Academic Hospital | 1 |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Picchetto, A., Cinelli, L., Bannone, E. et al. Fluorescence-based sentinel lymph node mapping and lymphography evaluation: results from the IHU-IRCAD-EAES EURO-FIGS registry. Surg Endosc 37, 5472–5481 (2023). https://doi.org/10.1007/s00464-023-10043-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10043-8