Abstract
Background
Indocyanine green has been widely employed as a secure and easy technique for sentinel lymph node mapping in different types of cancer. Nonetheless, the usage of Indocyanine green has not been fully implemented due to the heterogeneous results found in published studies. Thus, the objective of this meta-analysis is to evaluate the overall performance of Indocyanine green for sentinel lymph node mapping and node metastasis in patients undergoing colorectal cancer surgery.
Methods
An extensive systematic search was performed to identify relevant studies in English and Spanish with no time limit restrictions. For the meta-analysis, a hierarchical summary receiver operating characteristic curve (HSROCs) was constructed, and quantitative data synthesis was performed using random effects models. Specificity, sensitivity, positive, and negative likelihood ratios were obtained from the corresponding HSROC. Between-study heterogeneity was visually evaluated using Galbraith plot, and publication bias was quantified using Deeks’ method.
Results
A total of 11 studies were included for analysis. The pooled detection rate for sentinel lymph node mapping was 91% (80–98%). Covariates significantly influencing the pooled detection rate were having colon cancer (estimate: 1.3001; 1.114 to 1.486; p < 0.001) and the usage of a laparoscopic approach (estimate: 1.3495; 1.1029 to 1.5961; p < 0.001). The performance of Indocyanine green for the detection of metastatic lymph nodes yielded an area under the roc curve of 66.5%, sensitivity of 64.3% (51–76%), and specificity of 65% (36–85%).
Conclusions
Indocyanine green for the detection of sentinel lymph node mapping demonstrates better accuracy when used in colonic cancer and by a laparoscopic approach. Nevertheless, its overall performance for the detection of lymph node metastasis is poor.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In colorectal cancer, the removal of the tumor along with the lymph nodes related to the lesion is the current standard treatment. Thus, an adequate assessment of the sentinel lymph nodes during surgery is important due to the contribution it makes to the staging of the disease and its prognostic value [1,2,3,4].
Experience gained from other types of cancer, such as breast cancer, demonstrates the importance of the search for the sentinel lymph node in colorectal cancer. If the sentinel lymph node is located and proven to be positive, a complete lymph node dissection would be indicated [5,6,7,8,9,10,11,12]. This underlines the importance of a highly sensitive method that would allow us to map those sentinel lymph nodes adequately, helping us to detect the implicated metastatic lymph nodes. It has been suggested that a more extensive nodal dissection could help to improve the survival time of patients undergoing colorectal cancer surgery [13, 14]. Therefore, the purpose of node mapping does not fall only on the detection of the sentinel lymph node, but also in identifying the vast majority of lymph nodes with suspected metastases in order to perform a limited lymphatic dissection.
For several years, Indocyanine green has been widely employed as a secure and easy technique for node mapping in patients with multiple types of cancer [3, 5, 6, 11]. Still, due to the heterogeneity found in published studies, the usage of Indocyanine green has not been fully implemented for all procedures [9, 15]. The objective of this meta-analysis is to evaluate the overall performance of Indocyanine green for sentinel lymph node mapping and mapping of node metastasis in patients undergoing colorectal cancer surgery.
Methods
Eligibility criteria, information sources, search strategy
An extensive systematic search was performed using databases PubMed, ISI Web of Science, and SCOPUS to identify relevant studies published in English and Spanish, with no time limit restrictions, utilizing combinations of relevant MeSH term, keywords, and word variants for “Indocyanine green,” “indocyanine,” “colorectal neoplasms,” “colorectal,” “cancer,” “colonic,” “colonic cancer”. Other sources were manually searched for potentially relevant published studies. The first search was run on December 5th, 2017. Afterward, an update was extended until January 2019. No institutional research board approval nor informed consents are needed for systematic reviews and meta-analysis in our institution.
This review was done adhering to the recommendation on “Synthesizing Evidence from Diagnostic Accuracy Test (SEDATE) guidelines” [16] and PRISMA [17] guidelines for systematic reviews and meta-analysis. The study protocol was agreed between the authors, and one of them (A.L) being external to the group acted as a reviewer of it. Also, before running the analysis, the protocol was registered at the prospective international registry of systematic reviews (PROSPERO: CDR42018084841).
All abstracts identified were assessed by two independent evaluators (E.V. and J.J.), both blinded to authorship, authors’ institutions, and study results. Studies meeting inclusion criteria were full-text reviewed. The external author (A.L.) independently resolved any disagreement between evaluators. In cases of relevant studies with missing information, corresponding authors were reached by email. Annex 1 in the supplementary material details the search strategy and query syntaxes.
The primary endpoint of this review was to assess the performance of Indocyanine green for sentinel lymph node mapping, defined as the staining of the sentinel node that was confirmed by direct observation during the surgical procedure. The secondary endpoint was to evaluate the performance of Indocyanine green for the detection of lymph node metastasis.
Study selection
Criteria for inclusion in this systematic review were observational studies and case series of patients with colorectal cancer undergoing open or laparoscopic surgery using Indocyanine green injection as the primary technique for sentinel lymph node mapping. Exclusion criteria were studies with less than five patients, no adequately described surgical procedure, studies evaluating other types of cancer differently than colorectal cancer, reviews, and studies with not enough information to obtain the 2 × 2 tables.
Data extraction
The following data were extracted on a datasheet: author, year of publication, country where the study was conducted, study design, original inclusion criteria, exclusion criteria, total number of patients included in the study, mean age at surgery, number of lymph nodes detected by indocyanine green, In vivo or ex vivo assessment of the nodes, number of metastatic lymph nodes identified at histological analysis, type of near-infrared light and camera used for node mapping, latency time from Indocyanine green injection to the observation of the sentinel lymph node, and the surgical technique performed.
Quality assessment
Two reviewers (D.G.G. and F.P.R) independently assessed the quality of the selected studies. Quality assessment was carried out using the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool. This tool evaluates the quality of the included studies concerning biases affecting their applicability in four principal branches: patient selection, index test, reference standard, and flow and timing [18]. Results from these questions were graphed and assessed using Review Manager.
Statistical analysis
For the primary outcome, a single proportion meta-analysis with Arcsine transformation for small studies was performed using random effects modeling (weighting by the inverse of the variance). Between-study heterogeneity was assessed using tau2, χ2 (Cochrane Q), and I2 statistics. Results were presented using forest plots. For the secondary outcome, each article extracted information that was used to produce a 2 × 2 table for calculation of sensitivity and specificity [18, 19]. Obtained results were pooled in a meta-analysis using hierarchical summary receiver–operating characteristics (hSROC) curve. The model was fitted using a generalized linear mixed model approach that corresponds to the empirical Bayes fitting for the HSROC model [20,21,22]. Results were presented using pooled sensitivity, specificity, positive and negative likelihood ratios, and hSROC curves. Between-study heterogeneity was visually assessed using the Galbraith plot (Diagnostic log odds ratio against the inverse of the sensitivity) to visually identify outliers [23]. A formal investigation of heterogeneity was performed using various meta-regressions to evaluate the contribution of several covariates on the pooled detection rate and sensitivity. The possibility of publication bias was assessed using Deeks’ funnel plot asymmetry test [25, 26], where p < 0.05 was considered as significant asymmetry [24, 25]. All statistical analysis was conducted using the Meta-Analysis of Diagnostic Accuracy (mada) package [R project] [18, 19], MIDAS [26], and METANDI [27] from STATA v.15.0 (Texas College Station).
Results
Study selection
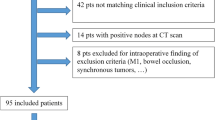
A total of 282 studies were identified by database searching, with three additional studies included manually (Fig. 1). Of them, 25 studies were eligible for full-text review. After review, 11 studies were retained for analysis [28,29,30,31,32,33,34,35,36,37,38], while 14 papers were excluded due to the following reasons: One of them because the technique used for surgery was not clear [39], three of them were about types of cancer other than colorectal cancer [40,41,42], two had less than five cases [43, 44] and two more were reviews [15, 45], and six of them because there was not enough information to obtain the 2 × 2 tables needed for analysis [3, 46,47,48,49,50]. The attributes of the included articles are portrayed in Table 1. Annex 1 details the full search strategy.
Risk of bias of the included studies
Among the 11 included studies [28,29,30,31,32,33,34,35,36,37,38], author’s judgement for risk of bias depicted high risk of bias in six studies according to patient selection [29, 32,33,34,35,36], while two more had high risk of bias according to the index test [33, 38] and one more in the reference standard [38]. Only four studies showed an unclear risk of bias according to the reference standard [28, 32, 33, 35]. Supplementary Figs. 1 and 2 tabulates the risk of bias of the studies included in the meta-analysis according to the QUADAS-2 tool for diagnostic test accuracy reviews [51].
Synthesis of results
Eleven studies [28,29,30,31,32,33,34,35,36,37,38] were selected for this systematic review and meta-analysis adding up to 281 patients that underwent surgery because of colorectal cancer. Participant’s age at surgery was 66.5 (SD 4.3) years. The mean number of retrieved lymph nodes per patient was 11, ranging from 2 to 23, while the number of metastatic lymph nodes detected by HE staining during histological examination was 4.6 (SD 4.2). The mean latency period from Indocyanine green injection to the node mapping was 39.4 min, ranging from 6 to 152 min. From the 281 patients that were included, 36% (102/281) underwent open colorectal cancer surgery (laparotomy), 39% had laparoscopic surgery, and 25% of the patients had no specification on which technique was used for surgery.
Indocyanine green for sentinel lymph node mapping
Detection rates were obtained from the 11 eligible studies [28,29,30,31,32,33,34,35,36,37,38]. The weighted detection rate by random effects model using Indocyanine green staining for sentinel lymph node mapping was 91% (95% CI 80–98%). Figure 2 shows the forest plot for the individual and overall detection rates. There was a high between-study heterogeneity (I2 = 87%; T2 = 0.06; p < 0.01). Bias quantification by Egger method showed significant publication bias among studies (− 3.77; − 6.04 to 1.51; p = 0.003). Nonetheless, the sensitivity analysis showed that studies rated as high quality by the QUADAS-2 scale had 0% heterogeneity and 94% detection rate (87–98%) (Fig. 3).
Meta-regressions for sentinel lymph node mapping
A meta-regression was performed to assess the influence of different variables to the pooled detection rate. The only significant variable influencing the pooled detection rate was the type of cancer, patients with colon cancer had significantly higher detection rates (estimate: 1.3001; 95% CI 1.114–1.486; p < 0.001) and those with rectal cancer had the lowest detection of sentinel lymph nodes at surgery (estimate: − 0.3793; 95% CI − 0.7534 to 0.0052; p < 0.046). Also, a significant positive influence was found when surgery was performed using a laparoscopic approach rather than by laparotomy (estimate: 1.3495; 95% CI 1.1029–1.5961; p < 0.001). Table 2 shows the calculated estimates for all variables.
Performance of Indocyanine green for the detection of metastatic lymph nodes
A total of 11 studies [28,29,30,31,32,33,34,35,36,37,38] had information on the total number of metastatic nodes stained by indocyanine green. The constructed hSROC curve (Fig. 4) showed an area under the curve of 66.5% with pooled sensitivity of 64.3% (95% CI 51–76%) and specificity of 65% (95% CI 36–85%). The mean positive and negative likelihood ratios were 2.0 (95% CI 1.1–3.6), and 0.59 (95% CI 0.40–0.86), respectively, resulting in a Diagnostic Odds Ratio of 3.81 (95% CI 1.3–8.2). Visual assessment of heterogeneity by Galbraith’s plot depicted a low heterogeneity among studies, while Deeks’ test found no significant publication bias (p = 0.11; Supplemental Fig. 3). Individual estimates of diagnostic performance for each study are shown in Fig. 5.
Meta-regression for the detection of lymph node metastasis
To establish the influence of all possible determinants influencing the overall sensitivity for lymph node metastasis, several meta-regressions were performed. The only two variables that influenced the pooled sensitivity were the type of cancer, where colon cancer was found to have significantly higher sensitivity compared to colorectal and rectal cancer (estimate: 0.655; 95% CI 0.548–0.762; p < 0.001), and the surgical approach, where the use of laparoscopy yielded higher sensitivity when compared to open surgery (estimate: 0.677; 95% CI 0.543–0.812; p < 0.001). Table 2 shows all calculated estimates.
Discussion
Main findings
There are three main findings in our analysis: Firstly, there is a 91% (95% CI 80–98%) detection rate when using Indocyanine green for the lymph node mapping. Although this yields a significant heterogeneity among studies, the sensitivity analysis showed that this would be reduced to 0% for high quality studies as evaluated by the QUADAS-2 scale, resulting in higher overall detection of lymph nodes (94% detection rate; 95% CI 87–98%). Secondly, the meta-regression analysis showed that the main cofactors influencing the detection of lymph nodes and the performance of Indocyanine green for lymph node metastasis were the type of cancer being assessed, where colon cancer yielded higher detection rates and higher sensitivity, and also, the usage of a laparoscopic approach, with higher detection rates and sensitivity compared to open surgery. And finally, an AUC of 66.5%, a pooled sensitivity of 64.3% (95% CI 51–76%), and specificity of 65% (95% CI 36–85%) showed that the overall performance of Indocyanine green for the detection of metastatic nodes is poor.
Comparison with existing literature
A previous meta-analysis conducted by Xiong et al. in 2014, found Indocyanine green to be a promising and safe technique for lymph node mapping and the detection of metastatic lymph nodes. Xiong found an overall detection rate of 96% and high sensitivity (86%) and specificity (100%) for the detection of metastatic nodes. Nonetheless, the study conducted by Xiong was performed on different types of cancer, from breast cancer to colorectal cancer. In this analysis, we aimed to assess the detection rate and the performance of Indocyanine green only for colorectal cancer to avoid bias and to accurately assess the estimates for this disease.
In 2017, Currie et al. conducted a low-biased study on 30 patients with colon cancer [30]. In this study, the authors performed the procedure using a laparoscopic approach with the usage of Indocyanine green for the mapping of the lymph nodes. From the 30 patients enrolled, successful lymph node mapping was achieved in 27 of them, yielding a detection rate of 90%. From the 27 patients with successful lymph node mapping by indocyanine green, only nine patients had positive nodes containing malignancy resulting in a 33% sensitivity and 90% specificity. These results are comparable to the ones in this study, yielding a similar detection rate (90% vs. 91%) but not similar sensitivity (33% vs. 64%).
Another recent study by Weixler et al. enrolling 220 stage I–III colon cancer patients [38] using a similar methodology found Indocyanine green to have a 98% detection rate for lymph node mapping, and a pooled sensitivity of 64% and specificity of 93% for the detection of micro-metastasis.
Clinical implications
The primary purpose of colorectal cancer surgery is to perform the excision of the tumor, followed by the removal of the lymph nodes related to it. Thus, a method with proper detection of these tumor-related nodes would be the ideal candidate for use in surgery. In this context, the results from this study suggest that the use of indocyanine green for sentinel lymph node mapping would yield good results, especially considering those higher quality studies (94%), supporting indocyanine green as a suitable method for node mapping as the primary focus of the test. This differs from the detection of node metastases, which are related not only to the sentinel lymph node itself but also to the extent of the tumor and clinical-histological classification. As for our clinical practice in Hospital Clinic of Barcelona, we have used this method for research purposes, and according to the results of this meta-analysis, we still need to gather higher quality information before incorporating this approach in our daily clinical practice.
Strengths and limitations
Our study has several strengths. Firstly, our systematic review was carried out by two independent investigators, who were blinded to authorship, hospital’s name, and results, limiting the bias in selecting publications for the final analysis. Secondly, since there were no time restrictions for our search, a large number of papers were evaluated to ensure the best results for the systematic review and final analysis. We were able to analyze a total of 281 patients undergoing surgery for colorectal cancer. Finally, our statistical analysis allowed us to perform several tests to formally assess the high heterogeneity found between studies, including meta-regressions, and sensitivity analysis to show different results according to the influence of several cofactors.
Limitations of this study are the significant heterogeneity found between studies, which was later reduced in the case of high quality studies using the sensitivity analysis. And in the same scenario, the low number of high quality studies found in the literature could limit the interpretation of results; thus, no recommendations can be made at this stage until more information is gathered in higher quality studies.
Conclusion
Indocyanine green is a useful method for lymph node mapping when used in colorectal cancer surgery; this significantly improves in colon cancer and through a laparoscopic approach. Nonetheless, there is still a need for higher quality evidence evaluating the performance of indocyanine green in colorectal cancer; thus, no recommendations can be made from the existing literature regarding its performance and security.
References
Saha S, Sehgal R, Patel M, Doan K, Dan A, Bilchik A, Beutler T, Wiese D, Bassily N, Yee C (2006) A multicenter trial of sentinel lymph node mapping in colorectal cancer: prognostic implications for nodal staging and recurrence. Am J Surg 191:305–310
Saha S, Bilchik A, Wiese D, Espinosa M, Badin J, Ganatra BK, Desai D, Kaushal S, Singh T, Arora M (2001) Ultrastaging of colorectal cancer by sentinel lymph node mapping technique—a multicenter trial. Ann Surg Oncol 8:94S–98S
van der Pas MH, Meijer S, Hoekstra OS, Riphagen II, de Vet HC, Knol DL, van Grieken NC, Meijerink WJ (2011) Sentinel-lymph-node procedure in colon and rectal cancer: a systematic review and meta-analysis. Lancet Oncol 12:540–550
Baxter NN, Virnig DJ, Rothenberger DA, Morris AM, Jessurun J, Virnig BA (2005) Lymph node evaluation in colorectal cancer patients: a population-based study. J Natl Cancer Inst 97:219–225
Stoffels I, von der Stuck H, Boy C, Poppel T, Korber N, Weindorf M, Dissemond J, Schadendorf D, Klode J (2012) Indocyanine green fluorescence-guided sentinel lymph node biopsy in dermato-oncology. J Dtsch Dermatol Ges 10:51–57
Namikawa K, Yamazaki N (2011) Sentinel lymph node biopsy guided by indocyanine green fluorescence for cutaneous melanoma. Eur J Dermatol 21:184–190
Murawa D, Hirche C, Dresel S, Hunerbein M (2009) Sentinel lymph node biopsy in breast cancer guided by indocyanine green fluorescence. Br J Surg 96:1289–1294
Jung SY, Kim SK, Kim SW, Kwon Y, Lee ES, Kang HS, Ko KL, Shin KH, Lee KS, Park IH, Ro J, Jeong HJ, Joo J, Kang SH, Lee S (2014) Comparison of sentinel lymph node biopsy guided by the multimodal method of indocyanine green fluorescence, radioisotope, and blue dye versus the radioisotope method in breast cancer: a randomized controlled trial. Ann Surg Oncol 21:1254–1259
He K, Chi C, Kou D, Huang W, Wu J, Wang Y, He L, Ye J, Mao Y, Zhang GJ, Wang J, Tian J (2016) Comparison between the indocyanine green fluorescence and blue dye methods for sentinel lymph node biopsy using novel fluorescence image-guided resection equipment in different types of hospitals. Transl Res 178:74–80
Chiu CC (2010) Sentinel lymph node biopsy in breast cancer guided by indocyanine green fluorescence (Br J Surg 2009; 96: 1289–1294). Br J Surg 97:455; Author Reply 455–456
Hirche C, Murawa D, Mohr Z, Kneif S, Hunerbein M (2010) ICG fluorescence-guided sentinel node biopsy for axillary nodal staging in breast cancer. Breast Cancer Res Treat 121:373–378
Nimura H, Narimiya N, Mitsumori N, Yamazaki Y, Yanaga K, Urashima M (2004) Infrared ray electronic endoscopy combined with indocyanine green injection for detection of sentinel nodes of patients with gastric cancer. Br J Surg 91:575–579
Chen SL, Bilchik AJ (2006) More extensive nodal dissection improves survival for stages I to III of colon cancer: a population-based study. Ann Surg 244:602–610
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 21:2912–2919
Xiong L, Gazyakan E, Yang W, Engel H, Hunerbein M, Kneser U, Hirche C (2014) Indocyanine green fluorescence-guided sentinel node biopsy: a meta-analysis on detection rate and diagnostic performance. Eur J Surg Oncol 40:843–849
Sotiriadis A, Papatheodorou SI, Martins WP (2016) Synthesizing Evidence from Diagnostic Accuracy TEsts: the SEDATE guideline. Ultrasound Obstet Gynecol 47:386–395
Fleming PS, Seehra J, Polychronopoulou A, Fedorowicz Z, Pandis N (2013) A PRISMA assessment of the reporting quality of systematic reviews in orthodontics. Angle Orthod 83:158–163
Harbord RM, Deeks JJ, Egger M, Whiting P, Sterne JA (2007) A unification of models for meta-analysis of diagnostic accuracy studies. Biostatistics 8:239–251
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58:982–990
Rutter CM, Gatsonis CA (2001) A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med 20:2865–2884
Macaskill P (2004) Empirical Bayes estimates generated in a hierarchical summary ROC analysis agreed closely with those of a full Bayesian analysis. J Clin Epidemiol 57:925–932
Chu H, Cole SR (2006) Bivariate meta-analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. J Clin Epidemiol 59:1331–1332; Author Reply 1332–1333
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
van Enst WA, Ochodo E, Scholten RJ, Hooft L, Leeflang MM (2014) Investigation of publication bias in meta-analyses of diagnostic test accuracy: a meta-epidemiological study. BMC Med Res Methodol 14:70
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58:882–893
Dwamena BA (2007) Midas: a program for meta-analytical integration of diagnostic accuracy studies in Stata. http://repec.org/wcsug2007/Dwamena-wsug2007.pdf
Harbord RM (2008) Metandi: Stata module for meta-analysis of diagnostic accuracy. Statistical Software Components from Boston College Department of Economics Boston College
Andersen HS, Bennedsen ALB, Burgdorf SK, Eriksen JR, Eiholm S, Toxvaerd A, Riis LB, Rosenberg J, Gogenur I (2017) In vivo and ex vivo sentinel node mapping does not identify the same lymph nodes in colon cancer. Int J Colorectal Dis 32:983–990
Cahill RA, Anderson M, Wang LM, Lindsey I, Cunningham C, Mortensen NJ (2012) Near-infrared (NIR) laparoscopy for intraoperative lymphatic road-mapping and sentinel node identification during definitive surgical resection of early-stage colorectal neoplasia. Surg Endosc 26:197–204
Currie AC, Brigic A, Thomas-Gibson S, Suzuki N, Moorghen M, Jenkins JT, Faiz OD, Kennedy RH (2017) A pilot study to assess near infrared laparoscopy with indocyanine green (ICG) for intraoperative sentinel lymph node mapping in early colon cancer. Eur J Surg Oncol 43:2044–2051
Hirche C, Mohr Z, Kneif S, Doniga S, Murawa D, Strik M, Hunerbein M (2012) Ultrastaging of colon cancer by sentinel node biopsy using fluorescence navigation with indocyanine green. Int J Colorectal Dis 27:319–324
Kusano M, Tajima Y, Yamazaki K, Kato M, Watanabe M, Miwa M (2008) Sentinel node mapping guided by indocyanine green fluorescence imaging: a new method for sentinel node navigation surgery in gastrointestinal cancer. Dig Surg 25:103–108
Liberale G, Galdon MG, Moreau M, Vankerckhove S, El Nakadi I, Larsimont D, Donckier V, Bourgeois P (2016) Ex vivo detection of tumoral lymph nodes of colorectal origin with fluorescence imaging after intraoperative intravenous injection of indocyanine green. J Surg Oncol 114:348–353
Liberale G, Vankerckhove S, Galdon MG, Larsimont D, Ahmed B, Bouazza F, Moreau M, El Nakadi I, Donckier V, Bourgeois P, R&D Group for the Clinical Application of Fluorescence Imaging at the Jules Bordet Institute (2016) Sentinel lymph node detection by blue dye versus indocyanine green fluorescence imaging in colon cancer. Anticancer Res 36:4853–4858
Noura S, Ohue M, Seki Y, Tanaka K, Motoori M, Kishi K, Miyashiro I, Ohigashi H, Yano M, Ishikawa O, Miyamoto Y (2010) Feasibility of a lateral region sentinel node biopsy of lower rectal cancer guided by indocyanine green using a near-infrared camera system. Ann Surg Oncol 17:144–151
Noura S, Ohue M, Seki Y, Yamamoto T, Idota A, Fujii J, Yamasaki T, Nakajima H, Murata K, Kameyama M, Yamada T, Miyashiro I, Ohigashi H, Yano M, Ishikawa O, Imaoka S (2008) Evaluation of the lateral sentinel node by indocyanine green for rectal cancer based on micrometastasis determined by reverse transcriptase-polymerase chain reaction. Oncol Rep 20:745–750
Watanabe J, Ota M, Suwa Y, Ishibe A, Masui H, Nagahori K (2016) Real-time indocyanine green fluorescence imaging-guided complete mesocolic excision in laparoscopic flexural colon cancer surgery. Dis Colon Rectum 59:701–705
Weixler B, Rickenbacher A, Raptis DA, Viehl CT, Guller U, Rueff J, Zettl A, Zuber M (2017) Sentinel lymph node mapping with isosulfan blue or indocyanine green in colon cancer shows comparable results and identifies patients with decreased survival: a Prospective Single-Center Trial. World J Surg 41:2378–2386
Arezzo A, Arolfo S, Mistrangelo M, Mussa B, Cassoni P, Morino M (2014) Transrectal sentinel lymph node biopsy for early rectal cancer during transanal endoscopic microsurgery. Minim Invasive Ther Allied Technol 23:17–20
Lan YT, Huang KH, Chen PH, Liu CA, Lo SS, Wu CW, Shyr YM, Fang WL (2017) A pilot study of lymph node mapping with indocyanine green in robotic gastrectomy for gastric cancer. SAGE Open Med 5:2050312117727444
Hirche C, Dresel S, Krempien R, Hunerbein M (2010) Sentinel node biopsy by indocyanine green retention fluorescence detection for inguinal lymph node staging of anal cancer: preliminary experience. Ann Surg Oncol 17:2357–2362
Boni L, David G, Mangano A, Dionigi G, Rausei S, Spampatti S, Cassinotti E, Fingerhut A (2015) Clinical applications of indocyanine green (ICG) enhanced fluorescence in laparoscopic surgery. Surg Endosc 29:2046–2055
Liberale G, Vankerckhove S, Galdon MG, Donckier V, Larsimont D, Bourgeois P (2015) Fluorescence imaging after intraoperative intravenous injection of indocyanine green for detection of lymph node metastases in colorectal cancer. Eur J Surg Oncol 41:1256–1260
Tamura K, Hotta T, Yokoyama S, Matsuda K, Iwamoto H, Yamaue H (2017) Using indocyanine green fluorescent imaging to successfully resect metachronous regional lymph node recurrence of rectosigmoid cancer. Asian J Endosc Surg 11(1):47–49
Keller DS, Ishizawa T, Cohen R, Chand M (2017) Indocyanine green fluorescence imaging in colorectal surgery: overview, applications, and future directions. Lancet Gastroenterol Hepatol 2:757–766
Yeung TM, Wang LM, Colling R, Kraus R, Cahill R, Hompes R, Mortensen NJ (2018) Intraoperative identification and analysis of lymph nodes at laparoscopic colorectal cancer surgery using fluorescence imaging combined with rapid OSNA pathological assessment. Surg Endosc 32:1073–1076
Nishigori N, Koyama F, Nakagawa T, Nakamura S, Ueda T, Inoue T, Kawasaki K, Obara S, Nakamoto T, Fujii H, Nakajima Y (2016) Visualization of lymph/blood flow in laparoscopic colorectal cancer surgery by ICG Fluorescence Imaging (Lap-IGFI). Ann Surg Oncol 23(Suppl 2):S266–S274
Nagata K, Endo S, Hidaka E, Tanaka J, Kudo SE, Shiokawa A (2006) Laparoscopic sentinel node mapping for colorectal cancer using infrared ray laparoscopy. Anticancer Res 26:2307–2311
Miyoshi N, Ohue M, Noura S, Yano M, Sasaki Y, Kishi K, Yamada T, Miyashiro I, Ohigashi H, Iishi H, Ishikawa O, Imaoka S (2009) Surgical usefulness of indocyanine green as an alternative to India ink for endoscopic marking. Surg Endosc 23:347–351
Handgraaf HJ, Boogerd LS, Verbeek FP, Tummers QR, Hardwick JC, Baeten CI, Frangioni JV, van de Velde CJ, Vahrmeijer AL (2016) Intraoperative fluorescence imaging to localize tumors and sentinel lymph nodes in rectal cancer. Minim Invasive Ther Allied Technol 25:48–53
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, QUADAS-2 Group (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Acknowledgements
We are grateful to Dr. Jose Rafael Villafan-Bernal for his help in carefully revising the manuscript.
Funding
No funding was needed for this study.
Author information
Authors and Affiliations
Contributions
All authors participated in the study. VTE, JLJ, and JVV performed the literature search and the acquisition of data. DGG and FPR performed the quality analysis for the selected studies. MPR and DLFB performed the data analysis. MPB, OPA, and LAM participated in the interpretation of data and revised the article. All authors approved the final version of the article.
Corresponding author
Ethics declarations
Conflict of interest
Antonio M. Lacy, PhD. reports grants from Medtronic, grants from Olympus Medical, personal fees from Applied Medical, personal fees from Conmed, outside the submitted work, but reports no conflicts of interests. Eduardo Villegas-Tovar, Julio Jimenez-Lillo, Valeria Jimenez-Valerio, Alejandro Diaz-Giron-Gidi, Regina Faes-Petersen, Ana Otero-Piñeiro, Beatriz Martin-Perez, Borja De Lacy, and Raigam J. Martinez-Portilla have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Villegas-Tovar, E., Jimenez-Lillo, J., Jimenez-Valerio, V. et al. Performance of Indocyanine green for sentinel lymph node mapping and lymph node metastasis in colorectal cancer: a diagnostic test accuracy meta-analysis. Surg Endosc 34, 1035–1047 (2020). https://doi.org/10.1007/s00464-019-07274-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07274-z