Abstract
Background
Colorectal liver metastases (CRLM) occur in roughly half of patients with colorectal cancer. Minimally invasive surgery (MIS) has become an increasingly acceptable and utilized technique for resection in these patients, but there is a lack of specific guidelines on the use of MIS hepatectomy in this setting. A multidisciplinary expert panel was convened to develop evidence-based recommendations regarding the decision between MIS and open techniques for the resection of CRLM.
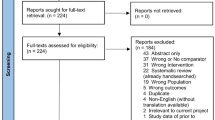
Methods
Systematic review was conducted for two key questions (KQ) regarding the use of MIS versus open surgery for the resection of isolated liver metastases from colon and rectal cancer. Evidence-based recommendations were formulated using the GRADE methodology by subject experts. Additionally, the panel developed recommendations for future research.
Results
The panel addressed two KQs, which pertained to staged or simultaneous resection of resectable colon or rectal metastases. The panel made conditional recommendations for the use of MIS hepatectomy for both staged and simultaneous resection when deemed safe, feasible, and oncologically effective by the surgeon based on the individual patient characteristics. These recommendations were based on low and very low certainty of evidence.
Conclusions
These evidence-based recommendations should provide guidance regarding surgical decision-making in the treatment of CRLM and highlight the importance of individual considerations of each case. Pursuing the identified research needs may help further refine the evidence and improve future versions of guidelines for the use of MIS techniques in the treatment of CRLM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Aim of these guidelines and specific objectives
The purpose of these guidelines is to provide evidence-based recommendations from a surgeon and patient perspective regarding the surgical treatment of resectable CRLM. The guideline recommendations address the equipoise between MIS vs open techniques in the situation of simultaneous or staged resection of the primary tumor and hepatic metastases. Key target audience includes patients, surgeons, oncologists, and other health care providers in a clinical setting. In addition, policy-makers and insurance providers involved with healthcare services involving the treatment of CRLM, or evaluating benefits, harms, and costs associated with the procedures performed to treat the condition may also take these guidelines into consideration in their discussions and planning.
Given that a patient–surgeon perspective was taken, and not a population perspective, considerations such as resources required, certainty of evidence of required resources, cost-effectiveness and equity were not evaluated.
Description of the health problems
In the United States alone, roughly 150,000 patients are newly diagnosed with CRC each year, and roughly half of these patients will develop liver metastases during their life [1]. Over the past decade there have been significant improvements in the treatment of colorectal liver metastases with improving systemic therapy including novel targeted therapies. In addition to improved medical options, liver resection has become increasingly safe during this time, with improvements in operative technique as well as perioperative care. These factors have combined to increase consideration for surgical resection of CRLM, leading to increases in hepatectomy for this diagnosis. Meanwhile, MIS techniques across surgery have come to the mainstream. While MIS hepatectomy is not yet the standard of care, it has become increasingly common over the last decade. A review of the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) data from 2014 to 2015 demonstrated that roughly 12% of 6918 hepatectomies were performed using MIS techniques [2]. More recent analysis of the same database showed that roughly 19% of hepatectomies for CRLM in the United States in 2019 were completed with MIS technique [3]. Other regions have reported higher prevalence of MIS techniques: a 10-year registry study from 22 Italian centers that included all liver resections from 2008 to 2018 reported that 31.6% of hepatectomies were performed laparoscopically and the year-to-year rate of laparoscopic liver resection (LLR) increased over time, from an initial proportion of < 10%, to approximately two-thirds of liver resections in 2018, eclipsing 50% of liver resections in 2016 [4].
With the increase in popularity of MIS hepatectomy, there have been a myriad of reports demonstrating safety and feasibility of this technique, as well as the equivalent oncologic outcomes [5,6,7,8,9]. There are now two randomized controlled trials comparing MIS and open hepatectomy in this setting [10,11,12]. Despite the increase in popularity of MIS hepatectomy for the treatment of CRLM, there are no consensus guidelines regarding the use of this technique for resection of CRLM.
The decision as to which operative technique to utilize can be difficult, with a number of technical considerations that may affect the decision. These include patient-related factors (e.g., previous surgical history, condition of the patient’s liver, location of metastases within the liver, chemotherapy-induced liver damage, etc.), and factors related to the surgeon and system within which they operate (e.g., surgeon and institution experience, and available equipment). With the clear understanding that safety is paramount, these guidelines provide recommendations for the choice of technique when resection of CRLM is considered and the above factors allow for MIS hepatectomy as an appropriate, and safe, option.
The statements included in this guideline are the product of a systematic review of published literature on the topic, and the recommendations are explicitly linked to the supporting evidence. The strengths and weaknesses of the available evidence are highlighted, and expert opinion sought where the evidence is lacking.
Methods
A systematic review of the evidence informed the guideline recommendations [13]. The guideline panel developed and graded the recommendations employing the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach and using the GRADE guideline development tool [14,15,16]. Reporting of the guideline adheres to the Essential Reporting Items for Practice Guidelines in Healthcare (RIGHT) checklist [17]. A detailed description of the process and methodology used by the SAGES Guidelines Committee and in the development of this manuscript has been published separately [18].
Guideline panel organization
Experts in liver surgery were invited to participate in the Guideline Panel. All panel members were experienced in both open and MIS hepatectomy and submitted disclosures on potential conflicts of interest. The panel was primarily composed of surgeons from the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and the Americas Hepato-Pancreato-Biliary Association (AHPBA). A methodologist with guideline development expertise (M.A.) and a SAGES Guidelines Committee Fellow (A.C.) facilitated guideline panel meetings as non-voting members of the panel. The Chair of the panel (DRJ) declared no conflicts of interest (COI) and assessed the conflicts of the panelists as to be not relevant and not likely to influence the direction of strength of the recommendations. A full list of all contributors to the guideline development is provided in Appendix A.
The expert panelists developed evidence-based guideline recommendations. The panel used the GRADE methodology to assess the systematic review evidence and judge the certainty of evidence to inform the strength of recommendations [14]. After an introductory online conference reviewing the process and expectations, the panel convened during Fall 2019 for a series of virtual meetings to formulate and prioritize guideline questions. The guideline panelists then finalized key questions and corresponding PICOs (patient—intervention—comparator—outcome) in consultation with the methodologist and Committee Chair (A.P.). A systematic review of the evidence addressing the guideline questions has been published as a standalone publication [13]. After completion of the literature review, panel members were provided with the included articles and results of the systematic review pertinent to the KQs in advance of the meetings. During panel meetings, the group reviewed the GRADE Evidence Tables and completed the Evidence-to-Decision (EtD) frameworks, ultimately generating specific recommendations.
Guideline funding & declaration and management of competing interests
SAGES provided funding for the librarian, developing and running literature searches, and for guideline and systematic review methodologists (M.A. & A.A.S), and for half the salary of the Guidelines Committee Fellow (A.C.). No grants or other support came from industry, nor any input into the conception or development of this guideline. A SAGES standard COI form was collected from all guideline contributors by the guideline lead (D.R.J.). A full list of declarations is listed at the end of the manuscript.
Selection of questions and outcomes of interest
The equipoise between the choice of techniques for resecting CRLM is the focus of this guideline. Of note, the selection of this question assumes a patient population appropriate for either open or MIS resection. There are numerous reasons that a patient may not be eligible for MIS resection (prohibitive surgical history, anatomic considerations, etc.), but patient selection for MIS resection is beyond the scope of the current questions. Patients deemed ineligible for MIS approach by the treating physicians were not included in the literature body examined here; thus, the following guidelines would not apply in such cases. Originally the panel had decided on four KQs, hoping to evaluate the use of MIS hepatectomy in colon and rectal liver metastases separately. After completing the systematic review, however, the available studies did not reflect this division in their included patient populations. As such the experts agreed to condense the KQs into two with a combined population of CRC.
Given their longstanding experience with patients, panel members voted for outcomes that they considered most patient-surgeon dyads would consider important or critical for decision-making. The final set of question-specific outcomes were selected by simple majority. This is discussed in more detail in the separately published systematic review [13]. The relative importance of the included outcomes was decided by the panel members and reflect what they believe to be most important to patients.
Evidence synthesis and evaluation of certainty of evidence
Systematic review methodology employed for evidence synthesis is detailed elsewhere [13]. We used the GradePro guideline development software [19]. to generate GRADE evidence tables from systematic review findings and to document guideline panel deliberations in the GRADE evidence to decisions framework (EtD). Methods outlined in the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach handbook [20] were used to judge the certainty of evidence as high, moderate, low or very low. GRADE domains informing judgments of certainty include the overall risk of bias across data contributing studies, inconsistency between study findings, indirectness or limitations in generalizability of evidence, imprecision in estimates of effects due to lack of statistical power, and risk of publication bias. We used the best available evidence to inform guideline recommendations, as such, when available, evidence from RCTs was prioritized over observational studies.
Development of recommendations
Absolute and relative estimates of effects (and corresponding certainty judgements) for outcomes that were rated critical or important for decision-making were presented in the GRADE EtD as desirable or undesirable effects of MIS Hepatectomy when compared with open hepatectomy and presented to the guideline panel.
The panel then judged the magnitude of desirable and undesirable effects, the overall certainty of evidence, variability in patient values and preferences that may be assigned to outcomes, and balance of these effects. To assign relative values and preferences to outcomes and assess associated variability, panel members used their collective patient-centric experience as a proxy for direct patient involvement.
The panelists also considered the GRADE acceptability and feasibility criteria as they formulated the language of the guideline recommendations through an electronic anonymized voting procedure. Recommendations that were supported by at least 80% panel consensus were finalized. Any considerations in addition to the presented empiric evidence that the panel brought to bear in formulating the recommendations were also documented in the EtDs. The EtD tables are presented in Appendix B&C and summarized in the following recommendations.
Guideline document review
This guideline was reviewed and edited by all panel members. The revised draft was then distributed to the SAGES Guidelines Committee for comments and approval in accordance with SAGES Guidelines Committee policies. After incorporating these edits, the guideline was then submitted to the SAGES and AHPBA Executive Committee and Board of Directors for approval. The guideline was published online on its website (https://www.sages.org) for a period of public comment for additional quality assurance.
Recommendations
Key question 1
Should MIS versus open hepatectomy be used for resection of resectable colorectal liver metastases when performed separately from resection of primary cancer?
Recommendation
The panel suggests that patients with CRLM undergo an MIS rather than open hepatectomy for resectable colorectal liver metastases being resected separately from resection of the primary cancer when feasible.
(Conditional recommendation; low certainty of evidence).
Summary of the evidence
A total of three RCTs [11, 12, 21, 22] met inclusion criteria, however one trial, the OSLO-COMET Trial, published their oncological outcomes in a later article. For the OSLO-COMET trial, perioperative outcomes were taken from the original published results, whereas oncological outcomes were extracted from the later follow-up study with the corresponding follow-up (i.e. 1 yr, 3 yr, and 5 yr outcomes). These studies were used to inform the panel’s decision on this question. Additionally, 20 observational studies were found to meet inclusion criteria. The findings of these studies supported the RCT results and have been included in the systematic review, [13] however, they were not directly considered in the guideline recommendations. The main limitation to the available RCTs was low event rate for most outcomes, particularly survival outcomes, as well as unclear risk of bias due to larger tumors in the open hepatectomy patients.
Benefits
The panel judged that there are moderate benefits to MIS hepatectomy compared to open hepatectomy across critical outcomes.
-
1.
Perioperative complications defined as Clavien–Dindo Grade > 3 (3 RCTs with a total of 506 participants) absolute difference of 58 fewer patients per 1000 (95% CI 95 fewer to 0 fewer)
-
2.
Hospital Length of Stay (3 RCTs with a total of 506 participants) absolute difference of 6.61 fewer days (95%. CI 10.19 fewer to 3.03 fewer)
-
3.
Disease Free Survival (DFS) at 1 year (2 RCTs with a total of 233 participants) absolute difference of 19 more patients per 1000 (95% CI 190 fewer to 316 more)
-
4.
Overall Mortality 5 yr (3 RCTs with a total of 316 participants) absolute difference of 10 fewer patients per 1000 (95% CI 120 fewer to 130 more)
Harms
There was no evidence of harm from MIS hepatectomy of resectable colorectal liver metastases for any important or critical outcomes in any studies meeting inclusion criteria. Thus, the panel judged the potential harms of MIS hepatectomy to be trivial.
Certainty of evidence
The certainty of the above evidence was evaluated as low based on the reported outcomes for decision making. These outcomes were primarily limited by imprecision (Appendix B).
Decision criteria
For this judgement, the panel considered the value for decision-making that informed patients would place on the main outcomes based on their experience and the available evidence. Perioperative complications, DFS at 1 year, hospital length of stay, and 5-year overall mortality were determined to be outcomes of critical importance for decision-making. With regards to DFS, the consensus of the panel was that earlier DFS was most reflective of differences in operative technique, whereas DFS measured at later time points was related more to a patient’s biology than the operative technique used. Therefore, the panel elected to concentrate on this outcome as measured at 1 year from surgery.
With regards to mortality, on the other hand, the consensus was that perioperative mortality was too low to distinguish between these techniques at an early time point, and subtle oncologic differences in technique would not be reflected in early mortality, but instead would require years to manifest as a difference in mortality. Additionally, the panel was encouraged to think of outcomes from the patients’ perspective and the consensus was that 5-year survival would be the main objective of any patient with metastatic CRC. Therefore, after much deliberation, the panel focused on mortality at 5 years.
Other outcomes discussed by the panel in reference to KQ1 included estimated blood loss (EBL) and perioperative transfusion. The panel felt that these outcomes were only important in that they might affect DFS and mortality. Moreover, the panel felt that the patient would be most interested in DFS and mortality rather than differences in EBL and blood transfusion. Given that meaningful data existed for the critical outcomes of DFS and mortality, the panel did not feel the need to utilize the surrogate outcomes of EBL and transfusions as part of the final recommendation for KQ1.
Conclusions
The overall desirable effects from MIS approach were judged to be moderate, with trivial undesirable effects. The panel was in agreement that there is a clear benefit from MIS resection of CRLM with regards to hospital length of stay and perioperative complications, but there was no clear benefit with regards to DFS, one year, or 5-year mortality. As a result, the recommendation for MIS was only conditional. In the situation of limited, resectable liver metastases, with appropriate patient factors, and a surgeon with appropriate experience, minimally invasive approach offers the benefit of decreased complications and shorter length of stay, but there is no clear benefit with respect to oncologic or survival outcomes. The panel had discussion around whether the oncologic data had any reliability given the quality of the data and the limited data that was available. There was also discussion around the implicit bias in many trials published by surgeons with significant expertise in MIS techniques. Overall, the consensus was that MIS techniques did offer benefit if the patient factors and surgeon experience was favorable for this approach.
Key question 2
Should MIS or open hepatectomy be used for resection of synchronous, resectable colorectal liver metastases when performed simultaneously with resection of primary cancer?
Recommendation
The panel suggests that patients with CRLM may undergo an MIS hepatectomy rather than open hepatectomy for resectable colorectal liver metastases being resected simultaneously with the primary cancer when feasible.
(Conditional recommendation; very low certainty of evidence).
The panel judged that there are small desirable effects to MIS hepatectomy across critical and important outcomes and was unable to make conclusions about undesirable effects due to substantial imprecision. For this key question, there was substantial uncertainty throughout the data, with very low certainty of evidence, leading to a conditional recommendation for MIS hepatectomy.
Summary of the evidence
There were no randomized trials addressing this question, and a total of twelve observation studies that met inclusion criteria [6,7,8, 23,24,25,26,27,28,29,30]. These studies were used to inform the panel’s decision on this question. The main limitations to the available studies were low event rates for most outcomes and substantial risk of bias stemming from the retrospective and non-randomized nature of these studies. In addition, there was some heterogeneity between studies for certain outcomes.
Benefits
The panel judged that there were small desirable effects with MIS hepatectomy compared to open hepatectomy across critical outcomes.
-
1.
Hospital Length of Stay (11 observational studies with a total of 827 participants) absolute difference of 3 fewer days (95%. CI 3.82 fewer to 2.17 fewer)
-
2.
Estimated Blood Loss (10 observational studies with a total of 609 participants) absolute difference of 177.35 cc lower (95%. CI 273.17 cc lower to 81.53 cc lower)
Several of the outcomes of interest were judged to be noninformative by the panel. Due to the wide confidence intervals, the anticipated absolute effects ranged from large benefits to large harms. These outcomes included perioperative complications (Clavien–Dindo ≥ 3), R0 resection, perioperative transfusion, and 5-year mortality. Although these are included in the EtD for reference, the panel felt these outcomes were likely underpowered to detect a difference between MIS and open hepatectomy, thus they were not used in decision-making of this recommendation.
Harms
The panel determined the potential harms are unknown for MIS hepatectomy performed simultaneously with the resection of the primary tumor. The point estimate of DFS at one year showed some potential benefit of open hepatectomy, however, the estimated effects ranged from large benefit to large harm (anticipated absolute effect 14 fewer patients per 1000; 95% CI 313 fewer to 530 more).
Certainty of evidence or effects
The certainty of the above evidence was evaluated as very low based on the reported outcomes for decision-making. The certainty was limited by the observational nature of the available studies, imprecision, and some inconsistency between studies (Appendix C).
Decision criteria
For this judgement, the panel considered the value for decision-making that informed patients would place on the main outcomes based on their experience and the available evidence. Perioperative complications, hospital length of stay, R0 resection, DFS, and mortality were all deemed to be critical outcomes. Estimated blood loss and perioperative transfusion were deemed to be important outcomes. EBL and transfusion were not used for decision making in KQ1 as there was stronger evidence of what the committee considered more important outcomes that were available. We show the data on EBL and transfusion in the evidence to decision table for the question 1, however.
As with KQ1, the panel concentrated on DFS at 1 year and mortality at 5 years based on considerations discussed above, as well as importance from the patients’ perspective. The discussion amongst the panel around KQ2 centered around the uncertainty of the available evidence. There was broad agreement that the MIS approach decreases hospital length of stay, but the remainder of the outcomes remained controversial. In particular, the evidence around any DFS or mortality outcomes was unconvincing, with no clear harm or benefit identified. Additionally, while there was agreement at estimated blood loss is likely lower with MIS approach, this outcome was not considered as critical as others (as discussed above). In the end, the panel judged that there is likely small benefit to the MIS approach, particularly around length of stay and blood loss, and there was no clear evidence of harm or benefit in oncologic outcomes given substantial imprecision of the data.
Conclusions
The panel judged that the benefits of MIS approach to simultaneous resection of CRLM and primary disease were small, and that the evidence for any harms was unclear. The panel was in agreement that MIS approach leads to a shorter hospital length of stay, and likely to lower blood loss. The effect of MIS approach on the remainder of the outcomes, however, was unclear. Overall, there was very low certainty of evidence for this key question, and mixed outcomes on DFS and mortality. As a result, the panel decided on a conditional recommendation for MIS approach to simultaneous resection of resectable CRLM and primary tumor. In the situation of limited, resectable liver metastases, with appropriate patient factors, and a surgeon with appropriate experience, a minimally invasive approach may offer a small benefit, specifically with regards to shorter length of stay, but there is no clear benefit with respect to oncologic or survival outcomes.
Additional considerations for KQ1 and KQ2
Additional considerations expressed by the panel included a possible decreased hernia rate and earlier return to adjuvant chemotherapy with an MIS approach, although this was not directly explored by the systematic review.
While the panel reached a recommendation for the use of MIS hepatectomy for resectable colorectal liver metastases being resected both simultaneously and separately from resection of the primary cancer, these were conditional recommendations. There was consensus that this should be done only when the specific circumstances of the case, and the surgeon’s training and experience allow this to be done safely and with good oncologic outcomes.
The three RCTs that were considered for KQ1 were all performed at relatively high-volume centers and operations were performed by well-trained surgeons past their learning curve. In addition, these trials included mostly patients with only one or two lesions, and very few major hepatectomies. Similarly, the ten observational studies considered for KQ2 included patients from high volume centers operated on by surgeons with extensive experience.
Additionally, many of these non-randomized trials may have biased towards less complex resections in the MIS cohort. This must all be considered in the implementation of these recommendations, which do not necessarily apply to complex liver resections, particularly when surgeons and institutions do not have the training and expertise to safely perform these operations. In general, the recommendation for MIS hepatectomy should be applied only in situations where the surgeons and the facility have the training and experience to perform the resection safely with an appropriate oncologic outcome.
Recommendations for future research—KQ1 and KQ2
Based on expert opinion, the panel made multiple suggestions for future research priorities. Studies are needed to better understand which patients are most likely to benefit from MIS approach are needed, such as specifically comparing MIS and open approaches in specific populations, such as elderly and obese patients, as well as specific tumor locations. Similarly, future studies examining the impact of mutational burden on decision between MIS and open hepatectomy are needed.
With regards to RCTs, the panel recommended trials studying the effects of MIS vs open combined resection of CRLM, and RCTs better powered to address long term oncologic outcomes. In addition, the panel recommended research differentiating simultaneous MIS resection of CRLM combined with colon resection vs rectal resection, differences in rates and consequences of incisional hernia after open vs MIS hepatectomy, differences in quality of life, short and long-term after open vs MIS hepatectomy, and return to intended oncologic therapy after open vs MIS hepatectomy.
Discussion
Purpose of this guideline
Despite multiple previous manuscripts published around the choice of MIS or open hepatectomy for resection of CRLM, no formal guidelines have been developed. This guideline aims to make evidence-based recommendations based on outcomes critical to clinical decision-making and individualized recommendations based on a balance of clinical effects. This guideline emphasizes the values key stakeholders place on different outcomes and how this can affect individual recommendations. A secondary aim was to develop research recommendations based on where the panel felt there was a paucity of evidence during systematic review of the literature. This should help guide future research endeavors to where they are most needed.
Implementation and revision of these guidelines
Implementation
The panel believes that it is feasible to successfully implement these recommendations into local practice and that the recommendations will be accepted by stakeholders, with the following caveats. As stated above, these recommendations are based on literature that includes hepatectomies done by surgeons with extensive training and experience in MIS hepatectomy and may not apply to all surgeons. Implementation of these recommendations will require similarly specialized training where applicable. Similarly, much of this data includes mostly simple hepatectomies, such as wedge resections, segmentectomies and left lateral or left hepatectomies. Whilst a complex discussion of the degree of complexity of hepatic resection is beyond the scope of this document, there are many resources regarding this topic available [31, 32]. The panel believed that safety should come first and therefore a graduated approach to MIS hepatectomy would be encouraged to increase surgeon experience with patient safety being the first priority. Thus, implementation of these guidelines should involve more straight-forward hepatectomies first, with more complex operations attempted only after considerable experience, for both the surgeon and institution.
Updating these guidelines
After publication of these guidelines, the SAGES Living Guidelines Task Force will plan to perform repeat literature searches on a frequent interval to search for any new evidence. When substantive literature is identified, the guideline will undergo formal update.
Limitations of these guidelines
One of the main limitations of these guidelines is related to the low certainty of the evidence, particularly around simultaneous resection of CRLM and primary tumor. In addition, there was limited long term data with poor participant retention addressing oncologic outcomes. Additionally, the panel was comprised of academic surgeons who have specialized training in both MIS techniques and hepatobiliary surgery. With this in mind, the panel was very clear that MIS hepatectomy should be entertained based on both patient and surgeon factors, with safety always being the most important consideration. Although every effort was made to limit the bias of the participating individuals, their opinions and experience may be represented in their voting. Lastly, patient advocates were not used in the rating of the importance of outcomes, but instead determined by the surgeon panel members based on their collective experience. However, a strength of this guideline is the careful consideration for patient values and preferences in view of individual critical outcomes.
References
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC et al (2020) Colorectal cancer statistics, 2020. CA: Cancer J Clin. https://doi.org/10.3322/caac.21601
Stiles ZE, Behrman SW, Glazer ES, Deneve JL, Dong L, Wan JY et al (2017) Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB (Oxford) 19(11):957–965
Carpenter EAA, Valdera F et al (2022) Modern trends in minimally invasive versus open hepatectomy for colorectal liver metastasis: an analysis of ACS-NSQIP. Surg Endosc. https://doi.org/10.1007/s00464-022-09749-y
Famularo S, Donadon M, Cipriani F, Ardito F, Carissimi F, Perri P et al (2020) Hepatocellular carcinoma surgical and oncological trends in a national multicentric population: the HERCOLES experience. Updates Surg. https://doi.org/10.1007/s13304-020-00733-6
Pan L, Tong C, Fu S, Fang J, Gu Q, Wang S et al (2020) Laparoscopic procedure is associated with lower morbidity for simultaneous resection of colorectal cancer and liver metastases: an updated meta-analysis. World J Surg Oncol 18(1):251
Takasu C, Shimada M, Sato H, Miyatani T, Imura S, Morine Y et al (2014) Benefits of simultaneous laparoscopic resection of primary colorectal cancer and liver metastases. Asian J Endosc Surg 7(1):31–37
Ivanecz A, Krebs B, Stozer A, Jagric T, Plahuta I, Potrc S (2018) Simultaneous pure laparoscopic resection of primary colorectal cancer and synchronous liver metastases: a single institution experience with propensity score matching analysis. Radiol Oncol 52(1):42–53
Kawakatsu S, Ishizawa T, Fujimoto Y, Oba A, Mise Y, Inoue Y et al (2021) Impact on operative outcomes of laparoscopic simultaneous resection of colorectal cancer and synchronous liver metastases. Asian J Endosc Surg 14(1):34–43
Okuno M, Goumard C, Mizuno T, Omichi K, Tzeng CD, Chun YS et al (2018) Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc 32(4):1776–1786
Fretland AA, Aghayan DL, Edwin B (2019) Long-term survival after laparoscopic versus open resection of colorectal liver metastases. J Clin Oncol. https://doi.org/10.1200/JCO.2019.37.18_suppl.LBA3516
Fretland AA, Dagenborg VJ, Bjornelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW et al (2018) Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 267(2):199–207
Robles-Campos R, Lopez-Lopez V, Brusadin R, Lopez-Conesa A, Gil-Vazquez PJ, Navarro-Barrios A et al (2019) Open versus minimally invasive liver surgery for colorectal liver metastases (LapOpHuva): a prospective randomized controlled trial. Surg Endosc 33(12):3926–3936
Ozair A, Collings A, Adams A et al (2022) Minimally invasive versus open hepatectomy for the resection of colorectal liver metastases: a systemic review and meta-analysis. Surg Endosc 36(11):7915–7937
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M et al (2016) GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: clinical practice guidelines. BMJ. https://doi.org/10.1136/bmj.i2089
Alonso-Coello P, Schunemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M et al (2016) GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: introduction. BMJ. https://doi.org/10.1136/bmj.i2016
Andrews JC, Schunemann HJ, Oxman AD, Pottie K, Meerpohl JJ, Coello PA et al (2013) GRADE guidelines: 15. Going from evidence to recommendation-determinants of a recommendation’s direction and strength. J Clin Epidemiol 66(7):726–735
Chen Y, Yang K, Marusic A, Qaseem A, Meerpohl JJ, Flottorp S et al (2017) A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med 166(2):128–132
Rogers AT, Dirks R, Burt HA, Haggerty S, Kohn GP, Slater BJ et al (2021) Society of American Gastrointestinal and endoscopic surgeons (SAGES) guidelines development: standard operating procedure. Surg Endosc 35(6):2417–2427
GRADEpro GDT: GRADEpro guideline development tool.: McMaster University (developed by Evidence Prime, Inc.); Available from: www.gradepro.org.
Schunemann HJ, Brozek J, Guyatt G, Oxman AD. (2013) GRADE handbook for grading quality of evidence and strength of recommendations: The GRADE Working Group; 2013 [updated Updated October 2013]. Available from: https://guidelinedevelopment.org/handbook.
Kasai M, Van Damme N, Berardi G, Geboes K, Laurent S, Troisi RI (2018) The inflammatory response to stress and angiogenesis in liver resection for colorectal liver metastases: a randomized controlled trial comparing open versus laparoscopic approach. Acta Chir Belg 118(3):172–180
Aghayan DL, Kazaryan AM, Dagenborg VJ, Rosok BI, Fagerland MW, Waaler Bjornelv GM et al (2021) Long-term oncologic outcomes after laparoscopic versus open resection for colorectal liver metastases : a randomized trial. Ann Intern Med 174(2):175–182
Huh JW, Koh YS, Kim HR, Cho CK, Kim YJ (2011) Comparison of laparoscopic and open colorectal resections for patients undergoing simultaneous R0 resection for liver metastases. Surg Endosc 25(1):193–198
Jung KU, Kim HC, Cho YB, Kwon CH, Yun SH, Heo JS et al (2014) Outcomes of simultaneous laparoscopic colorectal and hepatic resection for patients with colorectal cancers: a comparative study. J Laparoendosc Adv Surg Tech A 24(4):229–235
Shin JK, Kim HC, Lee WY, Yun SH, Cho YB, Huh JW et al (2020) Comparative study of laparoscopic versus open technique for simultaneous resection of colorectal cancer and liver metastases with propensity score analysis. Surg Endosc 34(11):4772–4780
Hu MG, Ou-yang CG, Zhao GD, Xu DB, Liu R (2012) Outcomes of open versus laparoscopic procedure for synchronous radical resection of liver metastatic colorectal cancer: a comparative study. Surg Laparosc Endosc Percutan Tech 22(4):364–369
Chen KY, Xiang GA, Wang HN, Xiao FL (2011) Simultaneous laparoscopic excision for rectal carcinoma and synchronous hepatic metastasis. Chin Med J (Engl) 124(19):2990–2992
Goumard C, Nancy You Y, Okuno M, Kutlu O, Chen HC, Simoneau E et al (2018) Minimally invasive management of the entire treatment sequence in patients with stage IV colorectal cancer: a propensity-score weighting analysis. HPB (Oxford) 20(12):1150–1156
Xu X, Guo Y, Chen G, Li C, Wang H, Dong G (2018) Laparoscopic resections of colorectal cancer and synchronous liver metastases: a case controlled study. Minim Invasive Ther Allied Technol 27(4):209–216
Ratti F, Catena M, Di Palo S, Staudacher C, Aldrighetti L (2016) Impact of totally laparoscopic combined management of colorectal cancer with synchronous hepatic metastases on severity of complications: a propensity-score-based analysis. Surg Endosc 30(11):4934–4945
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2018) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267(1):13–17
Tanaka S, Kawaguchi Y, Kubo S, Kanazawa A, Takeda Y, Hirokawa F et al (2019) Validation of index-based IWATE criteria as an improved difficulty scoring system for laparoscopic liver resection. Surgery 165(4):731–740
Acknowledgements
We would like to thank Sarah Colon, the SAGES senior program coordinator, Holly Burt, the SAGES librarian, and the SAGES guideline committee members for their help with the creation of this guideline.
Disclaimer
Clinical practice guidelines are intended to indicate the best available approach to medical conditions as established by a systematic review of available data and expert opinion. The approach suggested may not necessarily be the only acceptable approach given the complexity of the healthcare environment. These guidelines are intended to be flexible, as the surgeon must always choose the approach best suited to the patient and to the variables at the moment of decision. These guidelines are applicable to all physicians who are appropriately credentialed regardless of specialty and address the clinical situation in question. These guidelines are developed under the auspices of SAGES and AHPBA, the guidelines committee, and approved by the Board of Governors of both societies. The recommendations of each guideline undergo multidisciplinary review and are considered valid at the time of production based on the data available. New developments in medical research and practice pertinent to each guideline are reviewed, and guidelines are periodically updated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Vreeland receives financial support for travel expenses and registration fees for meetings from the Metis Foundation and consulting fees from Bantam Pharmaceuticals for clinical trial design. Dr. Collings was employed by SAGES as the guideline’s fellow. Dr. Adams receives financial support for travel expenses and registration fees for annual meetings for SAGES and AHPBA from the Metis Foundation. Dr. Dirks has privately purchased stock in Johnson & Johnson. Dr. Ansari is a consultant guideline methodologist and remunerated by SAGES for contribution to this work. Dr. Cleary receives consulting fees from Ethicon, Erbe, and Olympus. Dr. Buell receives speaker and consulting fees from Ethicon and Covidien. Dr. Slater receives consulting fees from Bolder Surgical and Cook Medical. Dr. Pryor receives speaker fees from Gore, Ethicon, and Stryker. Dr. Jeyarajah is a consultant for Ethicon, Angiodynamics, and Sirtex. Drs. Ozair, Kushner, Sucandy, Morrell, Cloyd, Ceppa, Abou-Setta, Alseidi, Awad, Ayloo, Orthopoulos, Richardson, Sbayi, Wakabayashi, and Mr. Whiteside have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vreeland, T.J., Collings, A.T., Ozair, A. et al. SAGES/AHPBA guidelines for the use of minimally invasive surgery for the surgical treatment of colorectal liver metastases (CRLM). Surg Endosc 37, 2508–2516 (2023). https://doi.org/10.1007/s00464-023-09895-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09895-x