Abstract
Background
Surgical resection of colorectal liver metastasis (CRLM) provides the best opportunity for prolonged survival. Eligibility for metastasectomy has expanded with technical advancements including parenchymal-sparing hepatectomy (PSH). Meanwhile, enthusiasm for minimally invasive surgery (MIS) has increased, though this approach may be preferentially utilized for technically straightforward cases. The purpose of this study is to characterize modern trends in open versus MIS approaches to partial hepatectomy and anatomic hepatectomy for CRLM within a nationwide cohort.
Methods
The American College of Surgeons’ National Surgical Quality Improvement Program (ACS-NSQIP) was used to investigate trends in MIS versus open hepatectomy for CRLM from 2015 to 2019. We examined baseline clinicopathologic and disease-related characteristics and compared trends in treatments over the study period.
Results
A total of 7457 patients undergoing hepatectomy for CRLM were identified (1367 MIS, 6090 open). Patients had similar clinicopathologic features between the two groups. Patients undergoing MIS resection less frequently received neoadjuvant therapy (51.1% vs 64.0%, p < 0.001) or concurrent intraoperative ablation (15.0% vs 21.3%, p < 0.001). Patients with tumors < 2 cm (34.9% vs 26.8%, p < 0.001) or only one to two tumors (82.8% vs 65.0%, p < 0.001) more commonly underwent MIS. MIS and open partial hepatectomies both significantly increased over the study period, but open partial hepatectomy increased at a greater rate than MIS (p < 0.001). Rates of anatomic resections have remained the same, with a greater proportion performed using an open approach (34.9% vs 16.4%, p < 0.001). Rates of operations consisting of > 1 concurrent partial hepatectomy are stable, but significantly more likely to be performed open (p < 0.001).
Conclusions
Hepatectomy for CRLM has increased from a rise in partial hepatectomy, potentially translating to increased use of PSH. Current trends suggest MIS approaches appear to be increasing, but selectively implemented for patients with less technically demanding disease characteristics. Educational efforts should be directed towards increased dissemination of parenchymal-sparing MIS techniques for more complex resections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Colorectal cancer is the fourth most common cancer in the USA [1]. The liver is the most common site of metastasis, occurring in approximately 50% of affected individuals [2,3,4]. While the majority of patients with colorectal liver metastasis (CRLM) have unresectable disease, advancements in perioperative management and improved surgical strategies, such as parenchymal sparing hepatectomy (PSH), have extended the eligibility for patients to undergo metastatectomy [2, 3, 5]. Five-year survival rates have recently been reported to be as high as 60%, compared to an accepted number of less than 30% in the 1980s, with approximately 20% achieving cure [2, 3, 6]. With modern management, to include PSH, salvageability is maintained in the case of recurrence. Up to 25% of patients may therefore undergo re-resection and achieve long-term survival [2, 7].
Minimally invasive surgery (MIS) is playing an increasing role in the management of CRLM. Retrospective data supports less blood loss and reduced length of stay (LOS) with an MIS approach, as well as non-inferior oncologic outcomes and mortality compared to open resection [8, 9]. In a recent single-institution randomized controlled trial, Fretland et al. demonstrated fewer postoperative complications, greater cost-effectiveness, and equivalent rate of negative resection margins in the laparoscopic compared to open arm [10]. Despite the apparent rise of both MIS and PSH techniques, which have undoubtedly revolutionized the care of patients with CRLM, existing literature characterizing trends in operative approach over the last decade is lacking. An analysis of the American College of Surgeons’ National Quality Improvement Program (ACS-NSQIP) registry investigated patterns in concurrent partial lobectomy and ablation for 2014 cases, but did not incorporate characteristics such as tumor size or number into the study and included resections for both benign and malignant pathologies, limiting the ability to draw conclusions regarding trends in CRLM treatment specifically [11]. Another study of patients within the Veterans Affairs health system analyzed trends in management of CRLM from 1998 to 2012, but did not stratify patients by operative approach (i.e., liver resection only, ablation, or a combination) [4]. With the evolving management of CRLM in an expanding pool of patients eligible for resection, a more recent and detailed examination of operative approach patterns in the context of tumor-specific disease characteristics is warranted.
In this study, we sought to characterize modern trends in an open versus MIS approach to partial hepatectomy and anatomic hepatectomy for CRLM within a nationwide cohort. We hypothesized that while the use of MIS and partial hepatectomy would increase over time, an open approach with possible anatomic resection would predominate for patients with technically demanding disease characteristics.
Materials and methods
Data were obtained from the American College of Surgeons’ National Surgical Quality Improvement Program (ACS-NSQIP) registry, a risk-adjusted, outcomes-based database, using the Hepatectomy Procedure Targeted Participant User File (PUF). As the ACS-NSQIP database is de-identified and publicly available, Institutional Review Board approval was not required.
Study design and cohort definitions
Data were assessed between the years of 2015–2019. Patients older than 18 undergoing hepatectomy (CPT 47120, 47125, 47122, 47130) for a known diagnosis of metastatic colorectal cancer, defined as a categorical variable within the Hepatectomy PUF, were included. All patients had an operative approach (MIS or open) recorded. Patients were defined as undergoing MIS if they underwent laparoscopic, laparoscopic with open assist, robotic with open assist, or other minimally invasive approach. Patients were defined as undergoing an open approach if they underwent a planned open resection or unexpected conversion from an initial MIS approach.
Patients were assigned to either an anatomic (CPT 47125, 47122, or 47130) or partial resection (CPT 47120) study group based on procedure coding. It was noted if one or greater concurrent partial hepatectomies were performed. In this study a partial hepatectomy was considered a PSH, though some exceptions to this generalization exist, which nevertheless aligns with most literature and was necessary within the constraints of the dataset [5, 12, 13].
Variables
Baseline demographic details were collected including age, sex, body mass index (BMI), functional status prior to surgery, and comorbidities such as diabetes, bleeding disorders, and pre-existing hepatitis. Pre-operative lab values and year of resection were additionally assessed. Relevant operative details analyzed included principle operative procedure, adjunct procedures, case urgency, and operative time. Liver-specific preoperative factors such as neoadjuvant therapy and biliary stenting were considered, as well as intraoperative details of hepatectomy including concurrent ablation, inflow occlusion during resection (i.e., Pringle maneuver), biliary reconstruction, and size and number of hepatic lesions treated.
Predictors of undergoing open or MIS resection were evaluated based on the above clinicopathologic factors.
Analysis of trends
To examine trends in management of CRLM over time, we evaluated frequency over the years of partial versus anatomic resection, and whether resection was performed via a MIS or open approach. Specifics of treatment over time were assessed, including receipt of neoadjuvant therapy, tumor size, concurrent partial hepatectomy, and intraoperative ablation.
Statistical analysis
Statistics were calculated using SPSS (version 22, IBM Corp, Released 2013, Armonk, NY) and SAS Software v9.4 (SAS Institute Inc., Cary, NC). Clinicopathologic data and trends were analyzed via either student’s T-test or Mann–Whitney U-test for continuous variables and Chi-square test for categorical variables. Rate of change was evaluated with a student’s T-test. Multivariable logistic regression was performed to evaluate predictors of undergoing open versus MIS resection based on preoperative patient and disease characteristics.
Results
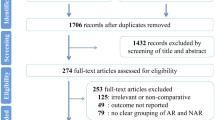
A total of 22,531 patients underwent hepatectomy at participating ACS-NSQIP institutions between 2012 and 2019. After applying our study criteria, a total of 7457 patients underwent either MIS (n = 1367) or open (n = 6090) hepatectomy for CRLM and were included in our analysis (Fig. 1). Of note, 4.22% (n = 257) of the open hepatectomies were due to conversion from MIS. This subgroup was included in the open group as per our predefined cohorts in the methods section.
Clinicopathologic factors and treatments
Univariate analysis of demographics, pre-operative characteristics, and hepatic-specific variables for patients undergoing an MIS versus open resection are summarized in Table 1. Demographics and comorbidities of patients in either resection group were similar, though a greater proportion of patients in the open resection group had a pre-operative bleeding disorder (4.2% vs. 2.6%, p = 0.01). While several differences in pre-operative laboratory values were noted, these do not appear to be clinically significant. A greater proportion of patients undergoing an open resection received neoadjuvant therapy (NAT) (64.0% vs 51.1%, p < 0.001), with larger (> 5 cm, 22.3% vs 12.8%, p < 0.001) and more numerous tumors (> 2 tumors, 35.0% vs 17.2%, p < 0.001).
Regarding operative factors, a greater proportion of patients undergoing an MIS resection underwent a partial versus anatomic hepatectomy as the principle operative procedure than patients receiving an open resection (83.6% vs. 65.1%, p < 0.001). The most common principle operative procedure after partial hepatectomy was a right hepatectomy for both open (18.5%) and MIS (8.9%) resections. While additional procedures were numerous, concurrent partial hepatectomy (15.1% and 6.1%), cholecystectomy (20.9% and 3.5%), and diagnostic ultrasound (7.5% and 7.6%) were frequently reported for open and MIS resections, respectively. A greater proportion of open than MIS resections included > 1 concurrent partial hepatectomies (31.5% vs. 22.2%, p < 0.001) and ablation (21.3% vs. 15.0%, p < 0.001). More patients undergoing open resection required inflow occlusion during the operation (31.5% vs. 16.4%, p < 0.001) and biliary reconstruction (1.9% vs. 0.9%, p = 0.01) than the MIS group.
Multivariable logistic regression modeling was used to determine independent predictors of operative approach (Table 2). Asian race was independently associated with receiving an MIS resection (OR 2.13, 95% CI 1.56–2.91), as was undergoing a single partial hepatectomy (OR 2.33, 95% CI 1.74–3.12), and having a tumor < 2 cm (OR 1.58, 95% CI 1.22–2.04). However, receiving neoadjuvant chemotherapy (OR 0.73, 95% CI 0.62–0.87), undergoing concurrent intraoperative ablation (0.71, 95% CI 0.56–0.89), or requiring inflow occlusion during resection (OR 0.43, 95% CI 0.35–0.53) were associated with decreased odds of an MIS approach. Other factors, including number of CRLM, were not independently associated with operative approach.
Analysis of trends over time
Trends in management of CRLM were examined by year (Table 3). Both MIS (p = 0.001) and open (p = 0.034) partial hepatectomy increased in frequency during the study period, though open partial hepatectomy increased at a greater rate (p < 0.001) (Fig. 2). Meanwhile, rates of anatomic resections did not change over the study period for either an MIS (p = 0.9) or open (p = 0.5) approach. Rates of ≥ 1 concurrent partial hepatectomy were stable over the study period for both MIS (p = 0.9) and open (p = 0.5) resections, but as discussed previously comprise a greater proportion of open than MIS resections (p < 0.001).
Though a greater proportion of patients undergoing open versus MIS resection had a concurrent intraoperative ablation, only rates of MIS ablation significantly increased in time (p = 0.04). Similarly, only rates of MIS resection of mid-sized tumors (2–5 cm) increased (p = 0.01), though large tumors (> 5 cm) favor open resection and these rates did not change over time for either approach. Rates of neoadjuvant therapy increased for patients receiving an open resection only (p < 0.001).
Discussion
In this study, we examined a nationwide cohort of 7457 patients who underwent an open or MIS hepatectomy for CRLM. While patients undergoing either approach had similar demographics and preoperative comorbidities, patients undergoing open resection had larger, more numerous tumors. Additionally, a greater proportion of patients undergoing open hepatectomy received NAT and concurrent intraoperative ablation. Overall, hepatectomies increased in number over the years, but open partial hepatectomy increased at a greater rate than MIS (p < 0.001). Despite an overall increase in frequency of hepatectomy, anatomic resections have remained stable in number over the study period regardless of operative approach, with open resection predominating.
In recent years, there has been an increase in the proportion of patients with CRLM who are eligible to undergo curative-intent hepatectomy [14]. This is, in part, due to improvements in perioperative management and more effective chemotherapeutic regimens, but also because of an expanded use of PSH, which allows for resection of bilobar disease while retaining an adequate future liver remnant [3, 7, 12,13,14,15,16]. In our examination of the ACS-NSQIP database, the total number of hepatectomies significantly increased over the study period, but interestingly anatomic resections remained stable. Thus, the overall increase in hepatectomies can be likely attributed to a rise in non-anatomic resections or partial hepatectomies, and could be related to the wider trend of increased use of PSH. In this context, it is particularly notable that open partial hepatectomy is increasing at a faster rate than MIS. Furthermore, the majority of concurrent partial hepatectomies performed over the study period were completed open, and 31.5% of open cases required multiple concurrent partial hepatectomies versus only 22.2% of MIS cases. In total, these trends possibly reflect the increasing use of PSH across the field and demonstrate that most of these cases are done open. Certain partial hepatectomies, particularly single, peripheral lesions, may be less technically demanding than an anatomic resection, and therefore feasibly accomplished with any approach, MIS or open. Performing PSH for multiple, deep lesions within the liver, however, can be technically very challenging and time consuming, especially with an MIS approach. This situation often leads surgeons to choose open hepatectomy [17].
In a similar trend, our data indicate greater disease complexity among patients receiving an open resection. Patients in the open resection cohort had larger and more numerous tumors, as well as increased use of preoperative chemotherapy and/or concurrent intraoperative ablation. The higher proportion of patients who underwent NAT in the open resection cohort is likely related to efforts at conversion to resectable from borderline or unresectable disease, and these cases are technically demanding even if converted to resectable disease [18, 19]. Operative time was also longer for an open hepatectomy, potentially another marker of greater disease burden, as this is in contrast to most literature citing longer operative times in MIS groups [20, 21].
Multivariable analysis demonstrated several independent predictors of undergoing a minimally invasive operation, including performance of partial hepatectomy (OR 2.3) as the principle operative procedure. MIS resections appear to be preferentially performed for small tumors (< 2 cm, OR 1.6) as a single partial hepatectomy (OR 1.4). As discussed previously and in concordance with prior literature, PSH can be technically difficult, often requiring deep and accurate dissection with ultrasound guidance, and therefore such resections may be more difficult to perform via a MIS approach [16, 22]. In addition, the need for variable port placements in bilobar or multiple PSH can additionally make the MIS approach less optimal. Unfortunately, we are unable to comment on the depth or anatomic location of hepatic metastases, as neither are collected variables of the ACS-NSQIP database, but these are certainly other aspects which may impact choice of operative approach [5]. Therefore, while multiple single institution reports are focused on expanding the reach of MIS hepatectomy, this nationwide observational cohort demonstrates that the majority of complex hepatectomies, to include multiple PSH, appear to be performed open [23, 24].
As the field attempts to broaden the application of MIS hepatectomy, there have been multiple initiatives from organizations such as the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and the International Laparoscopic Liver Society (ILLS) to expand MIS capabilities. Given the intentional move towards PSH for resection of CRLM, our findings support a clear need for greater educational efforts promoting minimally invasive PSH. For minimally invasive PSH to have an expanded role in the management of CRLM, it is necessary for surgeons to improve proficiency with ultrasound-guided, precise parenchymal dissection. Modern laparoscopic tools such as the ultrasonic surgical aspirator (CUSA®, Plainsboro, NJ, USA) facilitate fine dissection deep in the parenchyma for isolation of vessels and biliary structures to avoid major hepatectomy [25]. Without utilizing such techniques and technology to facilitate dissection, an MIS anatomic major hepatectomy may be technically easier than a deep PSH, and surgeons may have to choose between MIS major hepatectomy or open PSH. Robotic surgery may have the potential to expand MIS resections for CRLM in the setting of comparable oncologic outcomes, with purported benefits including improved visualization, articulating instruments, and a potentially shorter learning curve compared to laparoscopy [26,27,28,29]. For robotic surgery to gain a more widespread role in the management of CRLM, however, future education must be directed at development of techniques for performing multiple deep partial hepatectomies, just as with laparoscopic surgery.
Our study has several limitations. The ACS-NSQIP lacks granularity regarding certain aspects of management of CRLM, including specific chemotherapy regimens and clinical decision-making guiding treatment selection. This registry does not include important hepatic disease characteristics, such as depth, Couinaud segment, relation to vascular or biliary structures, and molecular biology of the tumor(s) that may inform decisions on operative approach. It similarly does not include post-excisional data about the specimen to include margin status. These missing factors are especially limiting when discussing selection of a minimally invasive and/or parenchymal-sparing operation, which may favor superficial tumors in anterior segments. However, the intent of this study was to characterize national trends in operative approach, and surrogates for disease complexity in the context of available procedure coding were used and provide valuable insight into selection for MIS and/or partial hepatectomy. In addition, the CPT codes used to characterize the types of hepatectomies performed similarly lack granularity and thus we made extrapolations between partial hepatectomy and PSH given the data available. Finally, the ACS-NSQIP registry is not a perfect indicator of proportion of procedures per year from participating institutions, and findings are not necessarily generalizable to non-participating institutions. Nevertheless, this analysis of trends across such a large cohort, including data from institutions of varied volume and geographic region, provides valuable and updated information about trends in CRLM management across the USA.
In conclusion, in this study we demonstrate an increase in hepatectomy for CRLM over the 2015–2019 study period of the ACS-NSQIP database, largely due to a rise in PSH in the form of partial hepatectomy. While MIS operations increased in number during this time, these approaches seem to be preferentially utilized for patients with less technically demanding disease characteristics such as small and/or few tumors requiring single partial hepatectomy. These results represent a call to action for further development and dissemination of parenchymal-sparing MIS techniques for more complex resections.
References
National Cancer Institute. Cancer Statistics. https://www.cancer.gov/about-cancer/understanding/statistics Accessed 12 Jan 2022
Smith JJ, D’Angelica MI (2015) Surgical management of hepatic metastases of colorectal cancer. Hematol Oncol Clin North Am 29(1):61–84. https://doi.org/10.1016/j.hoc.2014.09.003
Nathan H et al (2010) Conditional survival after surgical resection of colorectal liver metastasis: an international multi-institutional analysis of 949 patients. J Am Coll Surg 210(5):755–764. https://doi.org/10.1016/j.jamcollsurg.2009.12.041
Orcutt ST et al (2017) Patterns of care for colorectal liver metastasis within an integrated health system: secular trends and outcomes. Ann Surg Oncol 24(1):23–30. https://doi.org/10.1245/s10434-016-5351-8
Nelson D, Vreeland T (2022) Parenchymal preservation in the operative management of colorectal liver metastases. In: Vauthey JN, Kawaguchi Y, Adam R (eds) Colorectal liver metastasis. Springer
Parikh AA, Ni S, Koyama T, Pawlik TM, Penson D (2013) Trends in the multimodality treatment of resectable colorectal liver metastases: an underutilized strategy. J Gastrointest Surg 17(11):1938–1946. https://doi.org/10.1007/s11605-013-2325-z
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C (2016) Parenchymal-sparing hepatectomy in colorectal liver metastasis improves salvageability and survival. Ann Surg 263(1):146–152. https://doi.org/10.1097/sla.0000000000001194
Tian ZQ, Su XF, Lin ZY, Wu MC, Wei LX, He J (2016) Meta-analysis of laparoscopic versus open liver resection for colorectal liver metastases. Oncotarget 7(51):84544–84555. https://doi.org/10.18632/oncotarget.13026
Bonjer HJ et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332. https://doi.org/10.1056/NEJMoa1414882
A. Fretland Å, et al (2018) Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled Trial. Ann Surg 267(2):199–207. https://doi.org/10.1097/sla.0000000000002353
Gani F, Thompson VM, Bentrem DJ, Hall BL, Pitt HA, Pawlik TM (2016) Patterns of hepatic resections in North America: use of concurrent partial resections and ablations. HPB (Oxford) 18(10):813–820. https://doi.org/10.1016/j.hpb.2016.06.002
Andreou A et al (2021) Parenchymal-sparing hepatectomy for colorectal liver metastases reduces postoperative morbidity while maintaing equivalent oncologic outcomes compared to non-parenchymal-sparing resection. J Surg Oncol 38(1):101631. https://doi.org/10.1016/j.suronc.2021.101631
Okumura S et al (2019) Laparoscopic parenchymal-sparing hepatectomy for multiple colorectal liver metastases improves outcomes and salvageability: a propensity score-matched analysis. Ann Surg Oncol 26(1):4576–4586. https://doi.org/10.1245/s10434-019-07902-x
Moris D et al (2017) Parenchymal-sparing hepatectomy as the new doctrine in the treatment of liver-metastatic colorectal disease: beyond oncological outcomes. Anticancer Res 37(1):9
NCCN Clinical Practice Guidelines in Oncology: Colon Cancer. https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf. Accessed 3 Feb 2021
Kalil JA, Poirier J, Becker B, Van Dam R, Keutgen X, Schadde E (2019) Laparoscopic parenchymal-sparing hepatectomy: the new maximally minimal invasive surgery of the liver-a systematic review and meta-analysis. J Gastrointest Surg 23(4):860–869. https://doi.org/10.1007/s11605-019-04128-w
Torzilli G et al (2009) One-stage ultrasonographically guided hepatectomy for multiple bilobar colorectal metastases: a feasible and effective alternative to the 2-stage approach. Surgery 146(1):60–71. https://doi.org/10.1016/j.surg.2009.02.017
Aigner F, Pratschke J, Schmelzle M (2017) Oligometastatic disease in colorectal cancer—how to proceed? Visc Med 33(1):23–28. https://doi.org/10.1159/000454688
Iida H et al (2018) Prognostic factors of hepatectomy in initially unresectable colorectal liver metastasis: indication for conversion therapy. Mol Clin Oncol 9(5):545–552. https://doi.org/10.3892/mco.2018.1707
Kasai M et al (2018) Laparoscopic versus open major hepatectomy: a systematic review and meta-analysis of individual patient data. Surgery 163(5):985–995. https://doi.org/10.1016/j.surg.2018.01.020
Clark J et al (2020) Intention to treat laparoscopic versus open hemi-hepatectomy: a paired case-matched comparison study. Scand J Surg 109(3):211–218. https://doi.org/10.1177/1457496919851610
Alvarez FA, Sanchez Claria R, Oggero S, de Santibañes E (2016) Parenchymal-sparing liver surgery in patients with colorectal carcinoma liver metastases. World J Gastrointest Surg 8(6):407–423. https://doi.org/10.4240/wjgs.v8.i6.407
Cipriani F et al (2015) Laparoscopic parenchymal-sparing resections for nonperipheral liver lesions, the diamond technique: technical aspects, clinical outcomes, and oncologic efficiency. J Am Coll Surg 221(2):265–272. https://doi.org/10.1016/j.jamcollsurg.2015.03.029
Conrad C, Ogiso S, Inoue Y, Shivathirthan N, Gayet B (2015) Laparoscopic parenchymal-sparing liver resection of lesions in the central segments: feasible, safe, and effective. Surg Endosc 29(8):2410–2417. https://doi.org/10.1007/s00464-014-3924-9
D’Hondt M et al (2020) Laparoscopic liver resection for liver tumours in proximity to major vasculature: a single-center comparative study. Eur J Surg Oncol 46(4):539–547. https://doi.org/10.1016/j.ejso.2019.10.017
Navarro J, Rho SY, Kang I, Choi GH, Min BS (2019) Robotic simultaneous resection for colorectal liver metastasis: feasibility for all types of liver resection. Langenbecks Arch Surg 404(7):895–908. https://doi.org/10.1007/s00423-019-01833-7
Lai ECH, Tang CN (2017) Training robotic hepatectomy: the Hong Kong experience and perspective. Hepatobiliary Surg Nutr 6(4):222–229. https://doi.org/10.21037/hbsn.2017.01.21
McGuirk M et al (2021) Simultaneous robot assisted colon and liver resection for metastatic colon cancer. J Soc Laparosc Robot Surg 25:2. https://doi.org/10.4293/jsls.2020.00108
Hu Y et al (2021) Robotic versus laparoscopic hepatectomy for malignancy: a systematic review and meta-analysis. Asian J Surg 44(4):615–628. https://doi.org/10.1016/j.asjsur.2020.12.016
Funding
There were no external or internal sources of funding for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the US Army Medical Department, the Department of the Army, Department of the Air Force, Department of Defense, or the US Government. The voluntary, fully informed consent of the subjects used in this research was obtained as required by 32 CFR 219 and DODI 3216.02_AFI40-402. None of the authors including Drs. Carpenter, Thomas, Adams, Valdera, Chick, Kemp Bohan, Spitzer, Bader, Clifton, Nelson or Vreeland have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
ACS-NSQIP Disclaimer: The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carpenter, E.L., Thomas, K.K., Adams, A.M. et al. Modern trends in minimally invasive versus open hepatectomy for colorectal liver metastasis: an analysis of ACS-NSQIP. Surg Endosc 37, 5591–5602 (2023). https://doi.org/10.1007/s00464-022-09749-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09749-y