Abstract
Background
The comparative evidence regarding the outcomes of closure versus non-closure of mesenteric defects in laparoscopic Roux-en-Y gastric bypass (LRYGB) is poorly understood. We aimed to compare the outcomes of closure versus non-closure of mesenteric defects in LRYGB for morbid obesity.
Methods
We conducted a search of electronic information sources to identify all comparative studies investigating the outcomes of closure versus non-closure of mesenteric defects in patients undergoing LRYGB for morbid obesity. We used the Cochrane risk of bias tool and the ROBINS-I tool to assess the risk of bias of RCTs and observational studies, respectively. Random or fixed effects modelling was applied as appropriate.
Results
We included 10,031 patients from six observational studies and 2609 patients from two RCTs. Analysis of observational studies showed closure defects resulted in lower risks of internal hernia (OR 0.28, 95% CI 0.15, 0.54) and reoperation for small bowel obstruction (SBO) (OR 0.30, 95% CI 0.10, 0.83); no difference was found between the two groups in terms of SBO not related to internal hernia (OR 1.19, 95% CI 0.47, 2.99), early SBO (OR 0.74, 95% CI 0.04, 14.38), anastomotic leak (OR 0.84, 95% CI 0.45, 1.57), bleeding (OR 1.08, 95% CI 0.62, 1.89), and anastomotic ulcer (OR 2.08, 95% CI 0.62, 6.94). Analysis of RCTs showed closure of defects resulted in lower risks of internal hernia (OR 0.29, 95% CI 0.19,0.45) and reoperation for SBO (OR 0.51, 95% CI 0.38, 0.69) but higher risks of SBO not related to internal hernia (OR 1.90, 95% CI 1.09, 3.34) and early SBO (OR 2.63, 95% CI 1.16, 5.96); no difference was found between the two groups in terms of anastomotic leak (OR 1.95, 95% CI 0.80, 4.72), bleeding (OR 0.67, 95% CI 0.38, 1.17), and anastomotic ulcer (OR 2.08, 95% CI 0.62, 6.94).
Conclusions
Our results suggest that closure of mesenteric defects in LRYGB may be associated with lower risks of internal herniation and reoperation for SBO compared with non-closure of the defects (moderate certainty). The available evidence is inconclusive regarding the risks of SBO not related to internal hernia and early SBO (low certainty). More RCTs are needed to improve the robustness of the available evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic Roux-en-Y gastric bypass (LRYGB) is still regarded as one of the most popular surgical procedures for management of morbid obesity [1]. Although the laparoscopic approach is associated with lower risks of wound complications and incisional hernias compared with the open approach [2], the risk of internal hernias after LRYGB (ranging between 2 and 9%) remains a major concern [3,4,5] because they may result in potentially life-threatening small bowel obstruction, ischemia, and necrosis. Occurrence of internal hernias following LRYGB has been attributed to the absence of adhesions, loss of mesenteric fat, and use of different surgical techniques [6,7,8,9,10].
The LRYGB results in creation of mesenteric defects through which small bowel loops can herniate. These include jejuno-jejunal mesenteric defect, Petersen's defect (the potential defect between the alimentary Roux limb and the transverse mesocolon), or mesocolic defect (the opening in the transverse mesocolon when retrocolic gastrojejunostomy is created). The closure of the aforementioned mesenteric defects during LRYGB has been proposed as a strategy to reduce the risk of internal hernias. Although evidence from non-comparative studies suggests that closure of the mesenteric defects is associated with a lower risk of internal hernias after LRYGB [11], the comparative evidence regarding the outcomes of closure versus non-closure of mesenteric defects in LRYGB is poorly understood. In view of this, we aimed to perform a systematic review and meta-analysis to compare the outcomes of closure versus non-closure of mesenteric defects in patients undergoing LRYGB for morbid obesity.
Methods
This systematic review was performed according to an agreed predefined protocol (supplementary file) and was conducted and presented according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement standards [12].
Criteria for considering studies for this review
Types of studies
We included all randomized controlled trials (RCTs) and observational studies comparing closure and non-closure of mesenteric defects in patients undergoing LRYGB.
Types of participants
The study population comprised of adult participants of any gender undergoing LRYGB for morbid obesity. The LRYGB involved laparoscopic creation of gastric pouch, construction of antecolic or retrocolic gastrojejunostomy (between gastric pouch and Roux limb), and creation of jejunojejunostomy (between Roux limb and biliopancreatic limb).
Intervention of interest
The closure of mesenteric defects was considered as the intervention of interest. It was defined as complete closure of all defects including the jejuno-jejunal mesenteric defect, Petersen's defect, and the mesocolic defect (when retrocolic gastrojejunostomy was created) using sutures or staples.
Comparison of interest
Non-closure of mesenteric defect was considered as the comparison of interest. It was defined as leaving all the mesenteric defects open.
Types of outcome measures
Internal hernia and the site of internal herniation were considered as primary outcome measures. The secondary outcome measures included reoperation for suspected small bowel obstruction, small bowel obstruction not related to internal hernia, early small bowel obstruction, anastomotic leak, postoperative bleeding, and anastomotic ulcer.
Internal hernia was defined as operative finding of small bowel herniation through mesenteric defects including the jejuno-jejunal mesenteric defect, Petersen's defect, or the mesocolic defect. Reoperation due to suspected small bowel obstruction was defined as having an operation for small bowel obstruction due to any cause (adhesion, internal hernia, incisional hernia, intussusception, kinking of jejunojejunostomy, or narrow anastomosis) during the entire follow-up period. Small bowel obstruction not related to internal hernia was defined as small bowel obstruction due to adhesion, incisional hernia, intussusception, kinking of jejunojejunostomy, or narrow anastomosis. Early small bowel obstruction was defined as small bowel obstruction within 30 days postoperatively.
Search methods for identification of studies
Electronic searches
Two authors (MMM, KAK) independently searched the following electronic databases: MEDLINE, EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials (CENTRAL). The last search was run on 26 October 2019. Thesaurus headings, search operators, and limits in each of the above databases were adapted accordingly. The literature search strategy is outlined in Appendix 1. In addition, World Health Organization International Clinical Trials Registry (https://apps.who.int/trialsearch/), ClinicalTrials.gov (https://clinicaltrials.gov/), and ISRCTN Register (https://www.isrctn.com/) were searched for details of ongoing and unpublished studies. No language restrictions were applied in our search strategies.
Searching other resources
We searched the bibliographic lists of relevant articles and reviews for further potentially eligible trials.
Data collection and analysis
Selection of studies
The title and abstract of articles identified from the literature searches were assessed independently by two authors (KAK, MMM). The full-texts of relevant reports were retrieved and those articles that met the eligibility criteria of our review were selected. Any discrepancies in study selection were resolved by discussion between the authors. An independent third author (Shahab H) was consulted in the event of disagreement.
Data extraction and management
We created an electronic data extraction spreadsheet in line with Cochrane’s data collection form for intervention reviews. We pilot-tested the spreadsheet in randomly selected articles and adjusted it accordingly. Our data extraction spreadsheet included: study-related data (first author, year of publication, country of origin of the corresponding author, journal in which the study was published, study design, study size, clinical condition of the study participants, type of intervention and comparison), baseline demographic of the included populations (age, gender, body mass index, position of Roux limb, mesenteric defect closure method), and outcome data. Two review authors (MA, AS) independently collected and recorded data in the data extraction spreadsheet and disagreements were resolved by discussion. If no agreement could be reached, a third review author (Shahab H) was consulted.
Assessment of risk of bias in included studies
The Cochrane tool that categorizes studies into low, unclear, and high risk of bias in terms of selection bias, detection bias, performance bias, reporting bias, attrition bias, and other sources of bias was used for methodological quality assessment of RCTs. The Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS-I) assessment tool was used for methodological quality assessment of observational studies in terms of the following domains: bias due to confounding, bias in selection of participants into the study, bias in classification of interventions, bias due to deviations from intended intervention, bias due to missing data, bias in measurement of outcomes, and bias in selection of the reported result. Methodological quality assessment was performed by two independent reviewers (AS, Shahin H), and in case of disagreements a third independent reviewer (Shahab H) was consulted.
Data synthesis and statistical analyses
The odds ratio (OR) was calculated as summary measure for dichotomous outcome variables. An individual patient was counted as the unit of analysis. Information about dropouts, withdrawals, and other missing data was recorded and, if not reported, we contacted the study authors where possible. The analyses were based on intention to treat information from the individual studies. The Review Manager 5.3 (RevMan, Version 5.3. Copenhagen, 2014) software was used for data synthesis. The Cochran Q test (χ2) was used to evaluate statistical heterogeneity, and I2 was reported to quantify it. In terms of interpretation of I2, we considered I2 of 0–50% as low heterogeneity, 50–75% as moderate heterogeneity, and 75–100% as high heterogeneity. Clinical heterogeneity was assessed based on comparability of included population among the included studies in terms of baseline demographics (age, gender, BMI), position of Roux limb (antecolic or retrocolic), mesenteric defect closure method (suture or stapler), and outcome definition. Random or fixed effects modelling was utilized as appropriate for analyses; random effects models were applied when conspicuous heterogeneity existed. We aimed to generate funnel plots and assess their symmetry to examine the risk of publication bias for outcomes reported by at least 10 studies where possible. We performed and reported separate analyses for randomized controlled trials and observational studies.
Sensitivity and subgroup analyses
In order to explore potential sources of heterogeneity and assess the robustness of our results, additional analyses were conducted for the outcomes reported by at least four studies. We repeated the primary analysis using the random effects and fixed effect model. In addition, we calculated the risk ratio (RR) and risk difference (RD) for dichotomous outcomes. We assessed the effect of each study on the overall effect size and heterogeneity by repeating the analysis after removing one study at a time. Moreover, where possible, we aimed to perform subgroup analysis based on method of mesenteric defect closure (suture and stapler) and position of Roux limb (antecolic and retrocolic).
Summary of findings table
We constructed a table to compile and summarize the best evidence on relevant outcomes of comparison of closure versus non-closure of mesenteric defects in patients undergoing LRYGB for morbid obesity. Separate tables for randomized controlled trials and observational studies were constructed. We considered study population consisting of participants of any gender undergoing LRYGB for morbid obesity. We selected the most important and clinically relevant outcomes (both desirable and undesirable) thought to be essential for decision-making for inclusion in the 'Summary of findings' table. We have described these in the types of outcome measures section. We calculated assumed control intervention risks by using the mean number of events in control groups of selected studies for each outcome. We used the system developed by the Grading of Recommendation, Assessment, Development and Evaluation Working Group (GRADE Working Group) in grading the quality of evidence as high, moderate, low, and very low, based on within study risk of bias, directness of evidence, heterogeneity, precision of effects estimates, and risk of publication bias.
Results
Results of the search
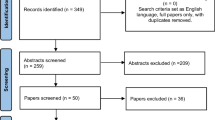
Searches of electronic databases identified 111 articles. Among the studies that were identified through search of electronic databases, 95 articles were not relevant to the topic of this study and were excluded directly. The remaining 16 studies were relevant to the topic of this study and after assessing their full-texts, 8 more articles were excluded; two articles were excluded as they were review articles; two articles were excluded as they were protocols; two articles were excluded as not all defects had been closed in the closure group; two articles were excluded as they did not provide adequate data about the included patients. Therefore, eight studies [13,14,15,16,17,18,19,20] were eligible for inclusion in this review. These included two RCTs [17, 18] and six retrospective cohort studies [13,14,15,16, 19, 20], enrolling a total of 12,640 patients. All patients underwent LRYGB for morbid obesity. The position of Roux limb was antecolic in 12,405 patients and retrocolic in 235 patients. Overall, 7662 patients were included in the closure group and 4978 patients were included in the non-closure group. The mesenteric defects were closed by suture in six studies [14, 16,17,18,19,20], by stapler in one study [15], and by suture or stapler in one study [13]. The median and mean follow-up were 4 and 4.5 years, respectively. In order to gain more information about the included studies, authors of two studies were contacted; none responded to the request. The literature search flowchart, baseline characteristics of the included studies and baseline characteristics of the included population are demonstrated in Fig. 1, Tables 1, and 2, respectively.
Risk of bias in included studies
The summary and results of methodological quality assessment of the two RCTs [17, 18] and six observational studies [13,14,15,16, 19, 20] are demonstrated graphically in Fig. 2.
Outcome synthesis
Observational studies
Internal hernia
Internal hernia was reported in six studies [13,14,15,16, 19, 20] enrolling 10,031 patients (Fig. 3). The closure of mesenteric defects was associated with a lower risk of internal hernia compared with non-closure of mesenteric defects (2% vs 10%, OR 0.28, 95% CI 0.15, 0.54). A high level of statistical heterogeneity among the studies existed (I2 = 83%, P < 0.00001). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 1). The quality of the evidence was downgraded due to risk of selection bias associated with retrospective nature of the included studies.
Forest plots of the comparisons of outcomes between the closure and non-closure groups reported by observational studies: A Internal hernia; B Reoperation for suspected small bowel obstruction; C Small bowel obstruction not related to internal hernia; D Early small bowel obstruction; E Anastomotic leak; F Bleeding; G Anastomotic ulcer
Internal herniation site
The site of internal herniation was reported in four studies [14,15,16, 19], enrolling 313 patients. In the closure group, 57% (50 out of 88) of internal hernias occurred at Petersen's defect, 37% (33 out of 88) at jejuno-jejunal mesenteric defect, and 6% (5 out of 88) at both Petersen's and jejuno-jejunal mesenteric defects. In the non-closure group, 46% (104 out of 225) of internal hernias occurred at Petersen's defect, 39% (88 out of 225) at jejuno-jejunal mesenteric defect, and 15% (33 out of 225) at both Petersen's and jejuno-jejunal mesenteric defects.
Reoperation for suspected small bowel obstruction
Reoperation for suspected small bowel obstruction was reported in three studies [14,15,16], enrolling 7682 patients (Fig. 3). The closure of mesenteric defects was associated with a lower risk of reoperation for suspected small bowel obstruction compared with non-closure of mesenteric defects (2% vs 12%, OR 0.30, 95% CI 0.10, 0.83). A high level of heterogeneity among the studies existed (I2 = 90%, P < 0.0001). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 1). The quality of the evidence was downgraded due to risk of selection bias associated with retrospective nature of the included studies and due to small number of studies reporting this outcome.
Small bowel obstruction not related to internal hernia
Small bowel obstruction not related to internal hernia was reported in two studies [13, 16], enrolling 2439 patients (Fig. 3). There was no difference in the risk of small bowel obstruction not related to internal between the two groups (0.7% vs 1.2%, OR 1.19, 95% CI 0.47, 2.99). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.53). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 1). The quality of the evidence was downgraded due to risk of selection bias associated with retrospective nature of the included studies and due to small number of studies reporting this outcome.
Early small bowel obstruction
Early small bowel obstruction was reported in one study [13], enrolling 863 patients (Fig. 3). There was no difference in the risk of early small bowel obstruction between the two groups (0% vs 0.4%, OR 0.74, 95% CI 0.04, 14.38). Heterogeneity could not be assessed. The certainty of the evidence was judged to be very low (Supplementary Table 1). The quality of the evidence was downgraded due to risk of selection bias associated with retrospective nature of the included study and due to the fact that only one study reported this outcome.
Anastomotic leak
Anastomotic leak was reported in three studies [13, 15, 16], enrolling 6452 patients (Fig. 3). There was no difference in the risk of anastomotic leak between the two groups (0.6% vs 0.7%, OR 0.84, 95% CI 0.45, 1.57). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.84). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 1). The quality of the evidence was downgraded due to risk of selection bias associated with retrospective nature of the included studies and due to small number of studies reporting this outcome.
Bleeding
Bleeding was reported in three studies [13, 15, 16], enrolling 6452 patients (Fig. 3). There was no difference in the risk of bleeding between the two groups (0.8% vs 0.9%, OR 1.08, 95% CI 0.62, 1.89). A low level of heterogeneity among the studies existed (I2 = 1%, P = 0.36). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 1). The quality of the evidence was downgraded due to risk of selection bias associated with retrospective nature of the included studies and due to small number of studies reporting this outcome.
Anastomotic ulcer
Anastomotic ulcer was reported in two studies [13, 16], enrolling 2439 patients (Fig. 3). There was no difference in the risk of anastomotic ulcer between the two groups (0.1% vs 0.4%, OR 0.82, 95% CI 0.12, 5.57). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.53). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 1). The quality of the evidence was downgraded due to risk of selection bias associated with retrospective nature of the included studies and due to small number of studies reporting this outcome.
Randomized controlled trials
Internal hernia
Internal hernia was reported in two studies [17, 18] enrolling 2609 patients (Fig. 4). The closure of mesenteric defects was associated with a lower risk of internal hernia compared with non-closure of mesenteric defects (2% vs 7%, OR 0.29, 95% CI 0.19, 0.45). A low level of statistical heterogeneity among the studies existed (I2 = 0%, P = 0.88). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 2). The quality of the evidence was downgraded due to risk of performance bias and due to small number of studies reporting this outcome.
Forest plots of the comparisons of outcomes between the closure and non-closure groups reported by randomized controlled trials: A Internal hernia; B Reoperation for suspected small bowel obstruction; C Small bowel obstruction not related to internal hernia; D Early small bowel obstruction; E Anastomotic leak; F Bleeding; G Anastomotic ulcer
Internal herniation site
The site of internal herniation was reported in two RCTs [17, 18], enrolling 120 patients. In the closure group, 68% (19 out of 28) of internal hernias occurred at Petersen's defect, 28% (8 out of 28) at jejuno-jejunal mesenteric defect, and 4% (1 out of 28) at both Petersen's and jejuno-jejunal mesenteric defects. In the non-closure group, 46% (60 out of 92) of internal hernias occurred at Petersen's defect, 39% (25 out of 92) at jejuno-jejunal mesenteric defect, and 15% (7 out of 92) at both Petersen's and jejuno-jejunal mesenteric defects.
Reoperation for suspected small bowel obstruction
Reoperation for suspected small bowel obstruction was reported in two RCTs [17, 18], enrolling 2609 patients (Fig. 4). The closure of mesenteric defects was associated with a lower risk of reoperation for suspected small bowel obstruction compared with non-closure of mesenteric defects (5.3% vs 9.8%, OR 0.51, 95% CI 0.38, 0.69). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.84). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 2). The quality of the evidence was downgraded due to risk of performance bias and due to small number of studies reporting this outcome.
Small bowel obstruction not related to internal hernia
Small bowel obstruction not related to internal hernia was reported in two RCTs [17, 18], enrolling 2609 patients (Fig. 4). The closure of mesenteric defects was associated with a higher risk of small bowel obstruction not related to internal hernia compared with non-closure of mesenteric defects (2.8% vs 1.5%, OR 1.90, 95% CI 1.09, 3.34). The level of statistical heterogeneity could not be estimated. The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be low (Supplementary Table 2). The quality of the evidence was downgraded due to risk of performance bias, due to small number of studies reporting this outcome, and due to inconsistency in findings of the included studies.
Early small bowel obstruction
Early small bowel obstruction was reported in two RCTs [17, 18], enrolling 2609 patients (Fig. 4). The closure of mesenteric defects was associated with a higher risk of early small bowel obstruction compared with non-closure of mesenteric defects (1.6% vs 0.6%, OR 2.63, 95% CI 1.16, 5.96). The level of statistical heterogeneity could not be estimated. The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be low (Supplementary Table S2). The quality of the evidence was downgraded due to risk of performance bias, due to small number of studies reporting this outcome and due to inconsistency in findings of the included studies.
Anastomotic leak
Anastomotic leak was reported in two RCTs [17, 18], enrolling 2609 patients (Fig. 4). There was no difference in the risk of anastomotic leak between the two groups (1% vs 0.5%, OR 1.95, 95% CI 0.80, 4.72). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.72). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 2). The quality of the evidence was downgraded due to risk of performance bias and due to small number of studies reporting this outcome.
Bleeding
Bleeding was reported in two RCTs [17, 18] enrolling 2609 patients (Fig. 4). There was no difference in the risk of bleeding between the two groups (1.5% vs 2.3%, OR 0.67, 95% CI 0.38, 1.17). A low level of heterogeneity among the studies existed (I2 = 3%, P = 0.31). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 2). The quality of the evidence was downgraded due to risk of performance bias and due to small number of studies reporting this outcome.
Anastomotic ulcer
Anastomotic ulcer was reported in two RCTs [17, 18] enrolling 2609 patients (Fig. 4). There was no difference in the risk of anastomotic ulcer between the two groups (0.6% vs 0.3%, OR 2.08, 95% CI 0.62, 6.94). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.58). The clinical heterogeneity was judged to be low. The certainty of the evidence was judged to be moderate (Supplementary Table 2). The quality of the evidence was downgraded due to risk of performance bias and due to small number of studies reporting this outcome.
Additional analyses
Sensitivity analyses
We performed sensitivity analyses for the primary and secondary outcomes reported by at least four studies. Removing one study at a time did not change the direction of the effect size and the overall heterogeneity for any of the outcomes. The direction of the effect size for each outcome remained unchanged when ORs, RRs or RDs were calculated separately. The use of random effects or fixed effect models did not affect the direction of the effect sizes.
Subgroup analyses
Mesenteric defect closure by suture
In six studies [14, 16,17,18,19,20], enrolling a total of 7764 patients, the mesenteric defects in the closure group were closed by suture. The closure of mesenteric defects was associated with lower risks of internal hernia (OR 0.34, 95% CI 0.25, 0.47) and reoperation for suspected small bowel obstruction (OR 0.50, 95% CI 0.39, 0.65) but higher risks of small bowel obstruction not related to internal hernia (OR 1.72, 95% CI 1.02, 2.91) and early small bowel obstruction (OR 2.63, 95% CI 1.16, 5.96) compared with non-closure of mesenteric defects. There was no difference in the risk of anastomotic leak (OR 1.17, 95% CI 0.70, 1.97), bleeding (OR 0.64, 95% CI 0.37, 1.11), and anastomotic ulcer (OR 2.05, 95% CI 0.66, 6.33) between the two groups.
Mesenteric defect closure by stapler
In one study [15], enrolling a total of 4013 patients, the mesenteric defects in the closure group were closed by stapler. The closure of mesenteric defects was associated with lower risks of internal hernia (OR 0.12, 95% CI 0.09, 0.16, P < 0.00001) and reoperation for suspected small bowel obstruction (OR 0.13, 95% CI 0.10, 0.17, P < 0.00001) compared with non-closure of mesenteric defects. There was no difference in the risk of anastomotic leak (OR 0.82, 95% CI 0.41, 1.66, P = 0.59) and bleeding (OR 1.03, 95% CI 0.54, 1.97, P = 0.93) between the two groups.
Antecolic LRYGB
In seven studies [13,14,15,16,17,18,19], enrolling a total of 11,726 patients, the position of Roux limb was antecolic. The closure of mesenteric defects was associated with lower risks of internal hernia (OR 0.26, 95% CI 0.15, 0.46, P < 0.00001) and reoperation for suspected small bowel obstruction (OR 0.34, 95% CI 0.15, 0.79, P = 0.01) but higher risks of small bowel obstruction not related to internal hernia (OR 1.69, 95% CI 1.05, 2.71) and early small bowel obstruction (OR 2.39, 95% CI 1.11, 5.15) compared with non-closure of mesenteric defects. There was no difference in the risk of adhesive small bowel obstruction (OR 1.45, 95% CI 0.74, 1.84, P = 0.28), anastomotic leak (OR 1.13, 95% CI 0.68, 1.87, P = 0.64), bleeding (OR 0.85, 95% CI 0.57, 1.26, P = 0.42), and anastomotic ulcer (OR 1.60, 95% CI 0.60, 4.28, P = 0.35) between the two groups.
Discussion
We performed a systematic review of literature and meta-analysis of outcomes to compare the outcomes of closure versus non-closure of mesenteric defects in patients undergoing LRYGB for morbid obesity. We identified two RCTs [17, 18] and six retrospective cohort studies [13,14,15,16, 19, 20], enrolling a total of 12,640 patients. The quality of the available evidence was moderate. The results of the analyses showed that the closure of mesenteric defects was associated with lower risks of internal hernia and reoperation for suspected small bowel obstruction compared with non-closure of mesenteric defects but may be associated with higher risks of small bowel obstruction not related to internal hernia and early small bowel obstruction. Internal herniation through Petersen's defect was more frequent than herniation through jejuno-jejunal mesenteric defect in both groups. There was no difference in the risk of anastomotic leak, bleeding, and anastomotic ulcer between the two groups. The results remained consistent through sensitivity analyses, separate analyses of randomized and non-randomized studies, and subgroup analyses based on method of mesenteric defect closure and position of Roux limb.
This study is the first meta-analysis in the literature providing comparative evidence on outcomes of closure versus non-closure of mesenteric defects in LRYGB. Meta-analysis of single-arm studies has been attempted by some authors [11]. Geubbels et al. [11] reported that closure of all mesenteric defects during antecolic LRYGB is associated with lowest incidence of internal hernias. Although the evidence provided in the study by Geubbels et al. [11] was not comparative and was limited to single-arm retrospective studies, it supports the findings of the current study.
The clinically significant internal hernias are those causing acute or subacute small bowel obstruction. Therefore, it is very important how to define clinically significant internal hernias. All of the internal hernias in the current study were diagnosed by surgical exploration for clinical or radiological suspicion of small bowel obstruction. This highlights that all of the internal hernias in both groups in this study were clinically significant.
The Petersen's defect was the most common site for internal herniation, being the site in more than 50% of the cases in either closure or non-closure group. The jejuno-jejunal mesenteric defect was the site of internal herniation in approximately 35% of cases in either group. This highlights that although internal herniation through the jejuno-jejunal mesenteric defect is less frequent than herniation through Petersen's defect, both defects contribute to significant proportion of internal hernias, and both should be closed during LRYGB. Considering that most of the included patients in this study had antecolic LRYGB, and that there was no data available on the site of herniation in patients who underwent retrocolic LRYGB, the role of a mesocolic defect in the formation of internal hernias remains unanswered in this study.
Although our results suggested that closure of mesenteric defects increases the risk of small bowel obstruction not related to internal hernia and early small bowel obstruction, definite conclusions cannot be made as these findings were based on the results of only two studies of which one showed no difference between the groups. The level and certainty of the evidence for these two outcomes were low; therefore, further studies are required to provide more robust evidence for definite conclusions.
In this review, we used a systematic approach to provide a summary of the best available comparative evidence and to assess the risk of bias of relevant studies. Our results remained consistent through sensitivity analyses, separate analyses of randomized and non-randomized studies, and subgroup analyses. All of these, together with a large sample size of homogenous population, would make our conclusions robust from the best available evidence. However, the reported outcomes of our review should be viewed and interpreted in the context of inherent limitations. Six of the included studies had non-randomized design and their results are subject to inevitable selection bias. The between-study heterogeneity was high for the primary outcomes. This can be explained by different sample sizes of the included studies and different techniques used for closure of the mesenteric defects. Nevertheless, subgroup analysis based on the closure technique of the mesenteric defects confirmed the consistency of our findings. As discussed above, most of the included patients in this study had antecolic LRYGB and there was no data available on the site of herniation in patients who underwent retrocolic LRYGB; therefore, the role of a mesocolic defect in the formation of internal hernias remains unanswered in this study. Finally, the number of eligible studies for this review was less than 10, not allowing formal assessment of publication bias as planned in our protocol; therefore, reporting bias cannot be excluded in this study.
Conclusions
The evidence from randomized and non-randomized studies suggest that closure of mesenteric defects in patients undergoing LRYGB may be associated with lower risks of internal herniation and reoperation for suspected small bowel obstruction compared with non-closure of the defects (moderate level of evidence with moderate certainty). The available evidence is inconclusive regarding the risks of small bowel obstruction not related to internal hernia and early small bowel obstruction (low level of evidence with low certainty). More randomized controlled trials are needed to improve the robustness of the available evidence.
References
Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, Buchwald H et al (2017) Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg 27(9):2279–2289
Nguyen NT, Goldman C, Rosenquist CJ, Arango A, Cole CJ, Lee SJ et al (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 234:279–289
Higa KD, Ho T, Boone KB (2003) Internal hernias after laparoscopic Roux en-Y gastric bypass: incidence, treatment and prevention. Obes Surg 13:350–354
Ahmed AR, Rickards G, Husain S et al (2007) Trends in internal hernia incidence after laparoscopic Roux-en-Y gastric bypass. Obes Surg 17(12):1563–1566
Iannelli A, Facchiano E, Gugenheim J (2006) Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg 16(10):1265–1271
Garrard CL, Clements RH, Nanney L, Davidson JM, Richards WO (1999) Adhesion formation is reduced after laparoscopic surgery. Surg Endosc 13:10–13
Schneider C, Cobb W, Scott J, Carbonell A, Myers K, Bour E (2011) Rapid excess weight loss following laparoscopic gastric bypass leads to increased risk of internal hernia. Surg Endosc 25:1594–1598
Bauman RW, Pirrello JR (2009) Internal hernia at Petersen’s space after laparoscopic Roux-en-Y gastric bypass: 62% incidence without closure—a single surgeon series of 1047 cases. Surg Obes Relat Dis 5:565–570
de la Cruz-Munoz N, Cabrera JC, Cuesta M, Hartnett S, Rojas R (2011) Closure of mesenteric defect can lead to decrease in internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis 7:176–180
Rodriguez A, Mosti M, Sierra M et al (2010) Small bowel obstruction after antecolic and antegastric laparoscopic Roux-en-Y gastric bypass: could the incidence be reduced? Obes Surg 20:1380–1384
Geubbels N, Lijftogt N, Fiocco M, van Leersum NJ, Wouters MW, de Brauw LM (2015) Meta-analysis of internal herniation after gastric bypass surgery. Br J Surg 102(5):451–460
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Nuytens F, D'Hondt M, Van Rooy F, Vansteenkiste F, Pottel H, Abasbassi M et al (2019) Closure of mesenteric defects is associated with a higher incidence of small bowel obstruction due to adhesions after laparoscopic antecolic Roux-en-y gastric bypass: a retrospective cohort study. Int J Surg 71:149–155
Amor IB, Kassir R, Debs T, Aldeghaither S, Petrucciani N, Nunziante M et al (2019) Impact of mesenteric defect closure during laparoscopic roux-en-y gastric bypass (LRYGB): a retrospective study for a total of 2093 LRYGB. Obes Surg 29(10):3342–3347
Aghajani E, Nergaard BJ, Leifson BG, Hedenbro J, Gislason H (2017) The mesenteric defects in laparoscopic Roux-en-Y gastric bypass: 5 years follow-up of non-closure versus closure using the stapler technique. Surg Endosc 31(9):3743–3748
Chowbey P, Baijal M, Kantharia NS, Khullar R, Sharma A, Soni V (2016) Mesenteric defect closure decreases the incidence of internal hernias following laparoscopic roux-En-Y gastric bypass: a retrospective cohort study. Obes Surg 26(9):2029–2034
Stenberg E, Szabo E, Ågren G, Ottosson J, Marsk R, Lönroth H et al (2016) Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet 387(10026):1397–1404
Rosas U, Ahmed S, Leva N, Garg T, Rivas H, Lau J et al (2015) Mesenteric defect closure in laparoscopic Roux-en-Y gastric bypass: a randomized controlled trial. Surg Endosc 29(9):2486–2490
Ribeiro-Parenti L, Arapis K, Chosidow D, Dumont JL, Demetriou M, Marmuse JP (2015) Gastrojejunostomy stricture rate: comparison between antecolic and retrocolic laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 11(5):1076–1084
Obeid A, McNeal S, Breland M, Stahl R, Clements RH, Grams J (2014) Internal hernia after laparoscopic Roux-en-Y gastric bypass. J Gastrointest Surg 18(2):250–255 (discussion 255–256)
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RM and SH contributed to conception and design. MA, AS, KAK, MMM, and SH helped with data collection. SH and SH contributed to analysis and interpretation. SH, SH, and RM involved in writing the article. All authors contributed to critical revision of the article and final approval of the article. SH and SH helped with statistical analysis.
Corresponding author
Ethics declarations
Disclosure
Shahab Hajibandeh, Shahin Hajibandeh, Mostafa Abdelkarim, Ahmad Shehadeh, Muhammad Mahid Mohsin, Khursheed Ahmed Khan and Richard Morgan have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
Search no. | Search strategy† |
|---|---|
#1 | MeSH descriptor: [bypass, roux en y gastric] explode all trees |
#2 | MeSH descriptor: [ anastomosis, roux en y] explode all trees |
#3 | Roux en y near2 bypass: TI,AB,KW |
#4 | Roux-en-y near2 bypass: TI,AB,KW |
#5 | #1 OR #2 OR #3 OR #4 |
#6 | Mesenteric defect: TI,AB,KW |
#7 | Petersen's defect: TI,AB,KW |
#8 | Jejunojejunal defect: TI,AB,KW |
#9 | #6 OR #7 OR #8 |
#10 | #5 AND #9 |
Combination of key words to be used in databases:
((("gastric bypass"[MeSH Terms] OR "anastomosis, roux-en-y"[MeSH Terms]) OR ("anastomosis, roux-en-y"[MeSH Terms] OR ("anastomosis"[All Fields] AND "roux-en-y"[All Fields]) OR "roux-en-y anastomosis"[All Fields] OR "roux en y bypass"[All Fields])) OR ("anastomosis, roux-en-y"[MeSH Terms] OR ("anastomosis"[All Fields] AND "roux-en-y"[All Fields]) OR "roux-en-y anastomosis"[All Fields] OR "roux en y bypass"[All Fields])) AND ((((("mesentery"[MeSH Terms] OR "mesentery"[All Fields] OR "mesenteric"[All Fields]) AND defect[All Fields]) OR (petersen's[All Fields] AND defect[All Fields])) OR (jejunojejunal[All Fields] AND defect[All Fields])) OR defect[All Fields]).
Rights and permissions
About this article
Cite this article
Hajibandeh, S., Hajibandeh, S., Abdelkarim, M. et al. Closure versus non-closure of mesenteric defects in laparoscopic Roux-en-Y gastric bypass: a systematic review and meta-analysis. Surg Endosc 34, 3306–3320 (2020). https://doi.org/10.1007/s00464-020-07544-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07544-1