Abstract
Background
Duration of convalescence after inguinal hernia repair is of major socio-economic interest and an often reported outcome measure. The primary aim was to perform a critical analysis of duration of convalescence from work and activity and secondary to identify risk factors for unexpected prolonged convalescence after laparoscopic inguinal hernia repair.
Methods
A qualitative systematic review was conducted. PubMed, Embase and the Cochrane database were searched for trials reporting convalescence after laparoscopic inguinal hernia repair in the period from January 1990 to January 2016. Furthermore, snowball search was performed in reference lists of identified articles. Randomized controlled trials and prospective comparative or non-comparative trials of high quality were included. Trials with ≥100 patients, >18 years of age and manuscripts in English were included. Scoring systems were used for assessment of quality.
Results
The literature search identified 1039 papers. Thirty-four trials were included in the final review including 14,273 patients. There was overall a large variation in duration of convalescence. Trials using non-restrictive recommendations of 1–2 days or “as soon as possible to return to all activities” reported overall a shorter duration of convalescence compared with trials not using recommendations for convalescence. Strenuous physical activity at work, strenuous leisure activity and patients with expectations of a prolonged period of convalescence may be risk factors for prolonged convalescence extending more than a few days after laparoscopic inguinal hernia repair.
Conclusions
Patients should be recommended a duration of 1–2 days of convalescence after laparoscopic inguinal hernia repair. Short and non-restrictive recommendations may reduce duration of convalescence without increasing risk of pain, complications or recurrence rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Surgical repairs of inguinal hernia are performed frequently, and patients are often in their working age [1]. Thus, duration of convalescence after inguinal hernia repair is of major socio-economic interest. Also, duration of convalescence in patients undergoing inguinal hernia repair is often an outcome in randomized clinical trials investigating interventions to improve quality of surgical treatment. Duration of convalescence may depend on factors related to the patient, surgical technique and other factors including analgesic treatment and sociocultural factors such as sick leave compensation. Laparoscopic technique compared with open repair [2–6] may shorten duration of convalescence although the difference may diminish when using short non-restrictive recommendations [7, 8]. So far no correlation has been found between non-restrictive physical activity and recurrence rate after inguinal herniotomy [9]. Often when no recommendations are given, convalescence may last 2–4 weeks after laparoscopic inguinal hernia repair [10–12]. Due to the minimally invasive nature of laparoscopic inguinal hernia repair only a few days of convalescence would be expected.
The primary aim of this review was to analyse and estimate the duration of convalescence after laparoscopic inguinal hernia repair and, secondly, to detect important risk factors for prolonged convalescence after laparoscopic inguinal hernia repair.
Methods
We defined convalescence as number of postoperative days before resuming work and normal activities [such as domestic activities (cooking, etc.), light physical activity (walking, biking, etc.) and heavy physical activity (running, etc.)] [13]. Thus, a one-day convalescence was defined as operation performed for instance Tuesday with return to normal activities on Wednesday. Convalescence is often reported as median or mean. To estimate duration of convalescence reported values of mean and median were combined as “average”. Thus, medians and means were added up and a mean was calculated and named “average”. Based on the reported values of mean and median in the included trials a “range” was also reported and should not be confused with range within the different trials.
Given recommendations in the different trials were divided into three groups: (1) no standardized recommendations given or recommendations not mentioned in the method section, (2) non-restrictive recommendations on physical activity defined as 1–2 days of convalescence or as soon as possible to return to all activities and (3) restrictive recommendations on physical activity defined as >2 days of convalescence/restriction of activity.
A literature search in PubMed, Embase and the Cochrane databases were conducted for relevant studies on duration of convalescence after laparoscopic inguinal hernia repair [transabdominal preperitoneal hernia repair (TAPP) and/or total extraperitoneal hernia repair (TEP)]. The process of reviewing papers was done as recommended by the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [14]. The literature was searched from January 1990 to January 2016. The PubMed search strategy was constructed by using the Medical Subject Headings (MeSH) “hernia, inguinal” combined with “laparoscopy”. The search was limited by activating the following three filters in PubMed: Humans, English and Adult 19+ years. Embase was searched using the following terms: “inguinal hernia” AND “laparoscopy” AND “convalescence”. Limits were humans and English language. Cochrane database was searched using the term “inguinal hernia”.
Available articles were assessed for quality and categorized according to level of evidence (see below). Randomized controlled trials (RCT), high-quality prospective non-randomized comparative and non-comparative trials were included. Results from trials were not included if study population was less than 100 patients undergoing laparoscopic repair (TAPP or TEP) or if other surgical procedures such as cholecystectomy were performed during the same procedure. Furthermore, we did not include trials not reporting duration of convalescence as mean or median. Letters to the editor, abstracts presented at national and international meetings and experimental animal models were also not included. Reference lists of identified articles were hand searched to find articles not identified in the electronic search. The following information was retrieved from the included studies: type of study (RCT, comparative or non-comparative trials), number of patients, gender, number of patients employed, surgical procedure, given recommendations, duration of convalescence from work and normal/physical activities (mean or median) and risk factors prolonging duration of convalescence.
RCTs and comparative or non-comparative non-randomized trials were assessed for quality by two assessors and agreement was obtained. An 11-item scoring system for RCTs was used [15]. The scoring system involved a stating of aim, control group, statistics, randomization process, defined study endpoint, unbiased assessment, description of the intervention and adequate follow-up. Each RCT was then categorized into three quality groups: A = high quality, B = moderate quality and C = poor quality [15]. In addition, comparative or non-comparative prospective trials were evaluated with MINORS [16] consisting of 12 items (only eight items for non-comparative trials) about stated aim, inclusion, collection of data, endpoints, assessment of endpoints, follow-up, loss to follow-up, study size and control group, time periods, baseline equivalence and statistical analyses. Each item was scored 0 (not reported), 1 (inadequately reported) or 2 (adequately reported). Thus, the maximum score was 16 for non-comparative trials and 24 for comparative trials [16]. In this review the non-comparative trials were categorized into high quality = score 12–16, moderate to low quality = 0–11, and the comparative trials into high quality = score 17–24 and moderate to low quality = 0–16.
Evidence levels were categorized on the classification described by Eccles et al. [17] (Ia–IV), where Ia equals highest evidence level and IV equals lowest evidence level. An included trial by the present authors [18] was evaluated by an independent assessor.
In search of evidence meta-analysis was planned to be conducted in the evaluation of patient- and surgery-related risk factors for prolonged duration of convalescence from work. Unfortunately, the sparse volume of high-quality trials with large cohort size made it not feasible to perform meta-analysis on risk factors for prolonged convalescence from work. Furthermore, only few trials presented data amenable to meta-analysis and were therefore not performed in this review.
Results
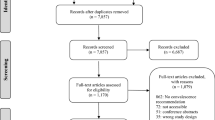
The literature search is shown in Fig. 1. Our database search identified 1039 possible trials and of these 990 trials did not meet the inclusion criteria. Furthermore, 15 non-randomized trials of moderate or low quality were excluded. Thus, in total 34 trials were included in the review. The studies included 14,273 patients undergoing laparoscopic groin hernia repair. The papers consisted of 34 original articles (23 RCTs and 11 high-quality prospective trials). The high-quality prospective trials consisted of 10 comparative and 1 non-comparative trials. Trials varied extensively regarding recommendations of convalescence ranging from no recommendations/not described, to recommendations of 1-day convalescence or as soon as possible to return to normal activities and up to 3–7-day convalescence with restriction of strenuous activities for a variable additional amount of time.
Work
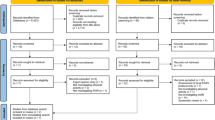
Fifteen trials reported duration of convalescence from work. When patients (n = 2718) were given non-restrictive recommendations, convalescence from work was average 10 days (range 5–15 days) after laparoscopic repair [18–26]. One study recommended 1 day of convalescence to all patients resulting in median 5 days of convalescence from work [18]. Trials not using standardized recommendations (n = 1078) showed a tendency towards a longer duration of convalescence from work with average 16 days (range 8–28 days) [27–31]. Only one trial (n = 103) used restrictive recommendations (3–7 days of sick leave) and reported mean 6 days duration of convalescence from work [32]. Figure 2 illustrates mean or median duration of convalescence from work in the different trials.
Duration of convalescence from work in randomized clinical trials (RCTs) (vs. open repair), comparative prospective trials (CP) and non-comparative prospective trials (P). Black dot mean, white dot median. Some trials reported convalescence from work for TAPP and TEP and this is shown with two spots in a row. Trials are stratified between no recommendations, non-restrictive recommendations (1–2 days or as soon possible to return to all activities) and restrictive recommendations (>2 days of convalescence/restriction of activities). n = number of patients
Normal activities (domestic activities, light physical activity)
Seven trials reported duration of convalescence from normal activities (domestic activities, walking, indoor activities, etc.). The absence from normal activities was average 5 days (range 3–7 days) with non-restrictive recommendations (n = 1278) [1, 18, 22, 26]. Again, duration of convalescence was prolonged in trials (n = 616) with no standardized recommendations with average 7 days (range 3–10 days) of convalescence from normal activities [27, 31, 33]. No trials used restrictive recommendations regarding convalescence from normal activities.
Physical activity
Eight trials reported duration of convalescence from physical activity (sport, running, biking, etc.). An average of 18 days (range 9–24) was found in trials using non-restrictive recommendations (n = 800) [21–23, 25], while trials with no standardized recommendations (n = 728) had an average of 20 days (range 14–23 days) [27–29]. One trial (n = 103) used restrictive recommendations and found mean 14 days of convalescence from physical activity [32].
In two trials convalescence was defined as returning to both work and physical activity (completely normal activity). The two trials included 896 patients and duration of convalescence again showed a tendency towards a shorter convalescence of average 17 days (range 13–20 days) in trials giving non-restrictive recommendations [20, 34].
In conclusion, duration of convalescence from work, normal activity and physical activity may overall be prolonged after laparoscopic inguinal hernia repair when not using short standardized recommendations of 1–2 days or “as soon as possible to return to all activities”. However, even with non-restrictive recommendations convalescence after hernia repair is surprisingly prolonged with average 10 days (range 5–15 days) from work.
Patient-related risk factors for prolonged convalescence
Only eight trials including 7356 patients assessed patient-related risk factors for prolonged convalescence.
Age did not seem to be a risk factor for prolonged convalescence in a non-comparative trial with patients in the range of 20–85 years of age (n = 185) [18].
The majority of trials investigating convalescence after bilateral versus unilateral hernia repair found that bilateral hernia compared with unilateral repair was not a risk factor for prolonged convalescence from work [18, 35, 36] or normal activities (n = 6785) [37, 38]. Only two trials (n = 604) found that patients with bilateral hernia may be in risk of prolonged convalescence from work [38] or normal activities [18]. However, the duration of convalescence from work was only slightly prolonged (unilateral median 7 days vs. bilateral median 8 days, p = 0.04) [38]. Furthermore, results from one non-randomized trial (n = 150) emphasized the need for standardized recommendation in trials investigating duration of convalescence [39]. The investigators only motivated and encouraged the patients with bilateral hernia to early resumption of work and normal activity and found not surprisingly a significantly shorter convalescence in patients with bilateral hernia compared with unilateral hernia [39].
Results from trials exploring convalescence after repair of recurrent hernia versus primary hernia were in favour of no difference in duration of convalescence between recurrent versus primary hernia. Three trials (n = 606, of these were 164 recurrent hernias) found that recurrent hernia (vs. primary hernia) was not a risk factor for prolonged convalescence from work [18, 40] or normal activities [18, 41], while one trial (n = 426, of these were 100 recurrent hernias) found recurrent hernia to be a risk factor for prolonged convalescence from work (mean 11 vs. 15 days, p = 0.03) [35]. However, the latter trial reports data from a period where laparoscopic repair was introduced to their department with learning curve, surgical difficulties and overall a high complication rate [35].
Patients with strenuous physical activity at work (vs. sedentary) may have prolonged duration of convalescence as observed in an RCT including 758 patients after laparoscopic repairs [20]. The authors reported a significant difference in duration of convalescence between light versus moderate versus heavy workload. Duration of convalescence from leisure activity may also be prolonged in patients with strenuous leisure activities (vs. sedentary) [18].
In conclusion, only few high-quality trials have assessed patient-related risk factors for prolonged convalescence. Strenuous physical activity at work and strenuous leisure activity may be risk factors for prolonged duration of convalescence after laparoscopic inguinal hernia repair. However, these results need to be confirmed in future studies.
Social and cultural factors
The influence of patients’ preoperative expectations on postoperative convalescence after laparoscopic inguinal hernia repair was studied in one prospective non-comparative trial (n = 185) [18]. Preoperative expectations of an extended duration of convalescence from work may be a risk factor for prolonged convalescence from work [18].
In conclusion, expectations of a prolonged period of convalescence may be a risk factor for prolonged duration of convalescence after laparoscopic inguinal hernia repair.
Surgery-related risk factors for prolonged convalescence
Nine RCTs assessed surgery-related risk factors for convalescence. The trials included 1863 patients (Table 1).
The use of lightweight versus heavyweight mesh showed no difference regarding duration of convalescence from work in 3 RCTs of primarily ideal quality (Prolene® mesh versus Vypro®, Vypro II®, Serapren® or Ultrapro® mesh, n = 682) [42–44] while one RCT of ideal quality including 180 patients demonstrated a significantly longer convalescence from work in patients receiving a heavyweight mesh (Prolene® mesh) compared with a lightweight mesh (Vypro II®) [45]. Weight of the mesh showed conflicting results when evaluating convalescence from normal activities with one RCT of ideal quality finding no difference between lightweight and heavyweight mesh (n = 140) [42], and one RCT of low quality reporting a prolonged duration of convalescence in the heavyweight group (n = 402) [44].
One RCT compared fixation of mesh with non-fixation in TEP (n = 104) and found no difference between groups in duration of convalescence [46]. Fixation of mesh with tacks/staples versus fibrin sealant was assessed in 2 RCTs on TAPP (n = 797) [47, 48] and identified a significantly prolonged duration of convalescence from work [48] or normal activities in the tacks/staples group compared with fibrin sealant group [47].
Single-incision laparoscopic surgery (SILS) TEP repair was compared with multiport TEP repair (n = 100) in a RCT and found median 7 days duration of convalescence after SILS TEP compared with 14 days after multiport TEP (p < 0.001) [49]. There was nothing stated about given recommendations in this trial.
In summary, data do not permit final conclusions on surgical risk factors to explain prolonged convalescence after laparoscopic inguinal hernia repair.
Miscellaneous
Bupivacaine versus saline in the preperitoneal space during laparoscopic inguinal hernia repair was investigated in a RCT and found no difference between groups in duration of convalescence from work or normal activities (n = 100) [50].
Discussion
In the present analysis we found a large variation in duration of convalescence with 5–28 days of convalescence from work, 3–10 days from normal activities and 9–24 days from physical activities after laparoscopic inguinal hernia repair. Although trials were not uniform there was a tendency towards a prolonged duration of convalescence in the trials giving “no recommendations” compared with the two groups giving recommendations. In trials assessing convalescence and not using non-restrictive recommendations or using restrictive recommendations of multiple days or weeks the outcome is not reliable because this may create an information bias in itself causing prolonged convalescence. Using non-restrictive recommendations duration of convalescence from work was average 10 days (range 5–15 days) but in a trial recommending only 1 day, convalescence from work was median 5 days [18]. By giving well-defined, standardized, short non-restrictive recommendations, duration of convalescence can be reduced as it has been shown in other trials with different surgical procedures (open inguinal hernia repair, laparoscopic cholecystectomy and vaginal prolapse surgery [7, 8, 51, 52]). Furthermore, limiting factors for a short convalescence may be exposed by patients failing to meet the recommendations. One important limiting factor of short convalescence from laparoscopic hernia repair is pain [18]. Even with the use of non-restrictive recommendations duration of convalescence after laparoscopic inguinal hernia repair seems remarkably elongated, and future trials are needed on how to further reduce duration of convalescence. The available studies using non-restrictive recommendations have not demonstrated adverse outcomes regarding pain, complications and recurrence rate compared with studies not using recommendations [52, 53]. One trial including patient undergoing open inguinal hernia repair has compared different recommendations (non-restrictive (n = 1069) vs. restrictive (n = 1306) vs. no specific recommendations (8297) and found no significant difference between groups in terms of hernia recurrence [7]. Thus, non-restrictive recommendations of 1–2 days or “as soon as possible” should be used in order to shorten convalescence as much as possible. However, some patients may have prolonged convalescence up to 2 weeks or even more before convalescence is ended.
The strength of this review was that it only included RCTs and high-quality non-randomized trials. However, there are also some limitations. Duration of convalescence is almost never the primary outcome in trials increasing the risk of underpowering. Included trials reporting convalescence after laparoscopic inguinal hernia repair were highly heterogeneous regarding given recommendations, reflecting the overall low quality of evidence in the literature. We chose to group trials recommending 1 day of convalescence together with trials recommending “as soon as possible to return to all activities”. The latter was a recommendation of short convalescence but not well defined. This could have affected the results of the “non-restrictive” recommendation group. The definition of work and leisure activities also varied. Furthermore, the outcome parameter convalescence was assessed prospectively in some trials, while many trials assessed convalescence retrospectively and therefore may have introduced a risk of recall bias. Because of the heterogeneous and sparse studies a meta-analysis was not performed.
In conclusion, it seems reasonable to recommend 1–2 days duration of convalescence after laparoscopic inguinal hernia repair. Short duration of convalescence does not increase pain, induce complications or increase recurrence rate. Future research should identify risk factors for prolonged convalescence in order to optimize the postoperative course. Trials assessing convalescence as an outcome parameter should use well-defined, short and non-restrictive recommendations of 1–2 days and take risk factors into consideration to avoid unnecessary bias.
References
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Rosenberg J, Bisgaard T, Kehlet H, Wara P, Asmussen T, Juul P, Strand L, Andersen FH, Bay-Nielsen M (2011) Danish Hernia Database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull 58:C4243
Bracale U, Melillo P, Pignata G, Di Salvo E, Rovani M, Merola G, Pecchia L (2012) Which is the best laparoscopic approach for inguinal hernia repair: TEP or TAPP? A systematic review of the literature with a network meta-analysis. Surg Endosc 26:3355–3366
McCormack K, Scott NW, Go PM, Ross S, Grant AM (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev CD001785. doi:10.1002/14651858.CD001785
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, Kukleta J, Lomanto D, Misra MC, Montgomery A, Morales-Conde S, Reinpold W, Rosenberg J, Sauerland S, Schug-Pass C, Singh K, Timoney M, Weyhe D, Chowbey P (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25:2773–2843
Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR (2003) Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90:1479–1492
Bay-Nielsen M, Thomsen H, Andersen FH, Bendix JH, Sorensen OK, Skovgaard N, Kehlet H (2004) Convalescence after inguinal herniorrhaphy. Br J Surg 91:362–367
Callesen T, Klarskov B, Bech K, Kehlet H (1999) Short convalescence after inguinal herniorrhaphy with standardised recommendations: duration and reasons for delayed return to work. Eur J Surg 165:236–241
Buhck H, Untied M, Bechstein WO (2012) Evidence-based assessment of the period of physical inactivity required after inguinal herniotomy. Langenbeck’s Arch Surg 397:1209–1214
Hamza Y, Gabr E, Hammadi H, Khalil R (2010) Four-arm randomized trial comparing laparoscopic and open hernia repairs. Int J Surg 8:25–28
Lorenz D, Stark E, Oestreich K, Richter A (2000) Laparoscopic hernioplasty versus conventional hernioplasty (Shouldice): results of a prospective randomized trial. World J Surg 24:739–745
Velasco JM, Gelman C, Vallina VL (1996) Preperitoneal bilateral inguinal herniorrhaphy evolution of a technique from conventional to laparoscopic. Surg Endosc 10:122–127
Bisgaard T, Kehlet H, Rosenberg J (2001) Pain and convalescence after laparoscopic cholecystectomy. Eur J Surg 167:84–96
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Slim K, Bousquet J, Kwiatkowski F, Pezet D, Chipponi J (1997) Analysis of randomized controlled trials in laparoscopic surgery. Br J Surg 84:610–614
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Eccles M, Freemantle N, Mason J (1998) North of England evidence based guidelines development project: methods of developing guidelines for efficient drug use in primary care. BMJ 316:1232–1235
Tolver MA, Strandfelt P, Forsberg G, Hjorne FP, Rosenberg J, Bisgaard T (2012) Determinants of a short convalescence after laparoscopic transabdominal preperitoneal inguinal hernia repair. Surgery 151:556–563
Berndsen F, Arvidsson D, Enander LK, Leijonmarck CE, Wingren U, Rudberg C, Smedberg S, Wickbom G, Montgomery A (2002) Postoperative convalescence after inguinal hernia surgery: prospective randomized multicenter study of laparoscopic versus Shouldice inguinal hernia repair in 1042 patients. Hernia 6:56–61
Eklund A, Rudberg C, Smedberg S, Enander LK, Leijonmarck CE, Osterberg J, Montgomery A (2006) Short-term results of a randomized clinical trial comparing Lichtenstein open repair with totally extraperitoneal laparoscopic inguinal hernia repair. Br J Surg 93:1060–1068
Fleming WR, Elliott TB, Jones RM, Hardy KJ (2001) Randomized clinical trial comparing totally extraperitoneal inguinal hernia repair with the Shouldice technique. Br J Surg 88:1183–1188
Fujita F, Lahmann B, Otsuka K, Lyass S, Hiatt JR, Phillips EH (2004) Quantification of pain and satisfaction following laparoscopic and open hernia repair. Arch Surg 139:596–600
Johansson B, Hallerback B, Glise H, Anesten B, Smedberg S, Roman J (1999) Laparoscopic mesh versus open preperitoneal mesh versus conventional technique for inguinal hernia repair: a randomized multicenter trial (SCUR Hernia Repair Study). Ann Surg 230:225–231
Langeveld HR, van’t Riet M, Weidema WF, Stassen LP, Steyerberg EW, Lange J, Bonjer HJ, Jeekel J (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 251:819–824
Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, Stassen LP, Vente JP, Weidema WF, Schrijvers AJ, van Vroonhoven TJ (1997) Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med 336:1541–1547
Wilson MS, Deans GT, Brough WA (1995) Prospective trial comparing Lichtenstein with laparoscopic tension-free mesh repair of inguinal hernia. Br J Surg 82:274–277
The MRC Laparoscopic Groin Hernia Trial Group (1999) Laparoscopic versus open repair of groin hernia: a randomised comparison. Lancet 354:185–190
Bansal VK, Misra MC, Babu D, Victor J, Kumar S, Sagar R, Rajeshwari S, Krishna A, Rewari V (2013) A prospective, randomized comparison of long-term outcomes: chronic groin pain and quality of life following totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) laparoscopic inguinal hernia repair. Surg Endosc 27:2373–2382
Kald A, Anderberg B, Carlsson P, Park PO, Smedh K (1997) Surgical outcome and cost-minimisation-analyses of laparoscopic and open hernia repair: a randomised prospective trial with one year follow up. Eur J Surg 163:505–510
Khoury N (1998) A randomized prospective controlled trial of laparoscopic extraperitoneal hernia repair and mesh-plug hernioplasty: a study of 315 cases. J Laparoendosc Adv Surg Tech A 8:367–372
Wellwood J, Sculpher MJ, Stoker D, Nicholls GJ, Geddes C, Whitehead A, Singh R, Spiegelhalter D (1998) Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. BMJ 317:103–110
Savarise MT, Simpson JP, Moore JM, Leis VM (2001) Improved functional outcome and more rapid return to normal activity following laparoscopic hernia repair. Surg Endosc 15:574–578
Gong K, Zhang N, Lu Y, Zhu B, Zhang Z, Du D, Zhao X, Jiang H (2011) Comparison of the open tension-free mesh-plug, transabdominal preperitoneal (TAPP), and totally extraperitoneal (TEP) laparoscopic techniques for primary unilateral inguinal hernia repair: a prospective randomized controlled trial. Surg Endosc 25:234–239
Juul P, Christensen K (1999) Randomized clinical trial of laparoscopic versus open inguinal hernia repair. Br J Surg 86:316–319
Kald A, Anderberg B, Smedh K, Karlsson M (1997) Transperitoneal or totally extraperitoneal approach in laparoscopic hernia repair: results of 491 consecutive herniorrhaphies. Surg Laparosc Endosc 7:86–89
Schmedt CG, Daubler P, Leibl BJ, Kraft K, Bittner R (2002) Simultaneous bilateral laparoscopic inguinal hernia repair: an analysis of 1336 consecutive cases at a single center. Surg Endosc 16:240–244
Lau H, Patil NG, Yuen WK (2003) A comparative outcome analysis of bilateral versus unilateral endoscopic extraperitoneal inguinal hernioplastics. J Laparoendosc Adv Surg Tech A 13:153–157
Kald A, Domeij E, Landin S, Wiren M, Anderberg B (2000) Laparoscopic hernia repair in patients with bilateral groin hernias. Eur J Surg 166:210–212
Pawanindra L, Philips P, Chander J, Ramteke VK (2010) Is unilateral laparoscopic TEP inguinal hernia repair a job half done? The case for bilateral repair. Surg Endosc 24:1737–1745
Knook MT, Weidema WF, Stassen LP, van Steensel CJ (1999) Endoscopic total extraperitoneal repair of primary and recurrent inguinal hernias. Surg Endosc 13:507–511
Lau H (2004) Endoscopic totally extraperitoneal inguinal hernioplasty for recurrence after open repair. ANZ J Surg 74:877–880
Bringman S, Wollert S, Osterberg J, Heikkinen T (2005) Early results of a randomized multicenter trial comparing Prolene and VyproII mesh in bilateral endoscopic extraperitoneal hernioplasty (TEP). Surg Endosc 19:536–540
Heikkinen T, Wollert S, Osterberg J, Smedberg S, Bringman S (2006) Early results of a randomised trial comparing Prolene and VyproII-mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia 10:34–40
Chowbey PK, Garg N, Sharma A, Khullar R, Soni V, Baijal M, Mittal T (2010) Prospective randomized clinical trial comparing lightweight mesh and heavyweight polypropylene mesh in endoscopic totally extraperitoneal groin hernia repair. Surg Endosc 24:3073–3079
Langenbach MR, Schmidt J, Ubrig B, Zirngibl H (2008) Sixty-month follow-up after endoscopic inguinal hernia repair with three types of mesh: a prospective randomized trial. Surg Endosc 22:1790–1797
Garg P, Nair S, Shereef M, Thakur JD, Nain N, Menon GR, Ismail M (2011) Mesh fixation compared to nonfixation in total extraperitoneal inguinal hernia repair: a randomized controlled trial in a rural center in India. Surg Endosc 25:3300–3306
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245:222–231
Olmi S, Scaini A, Erba L, Guaglio M, Croce E (2007) Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery 142:40–46
Tran H, Turingan I, Tran K, Zajkowska M, Lam V, Hawthorne W (2014) Potential benefits of single-port compared to multiport laparoscopic inguinal herniorraphy: a prospective randomized controlled study. Hernia 18:731–744
Deans GT, Wilson MS, Brough WA (1998) Controlled trial of preperitoneal local anaesthetic for reducing pain following laparoscopic hernia repair. Br J Surg 85:1013–1014
Bisgaard T, Klarskov B, Rosenberg J, Kehlet H (2001) Factors determining convalescence after uncomplicated laparoscopic cholecystectomy. Arch Surg 136:917–921
Ottesen M, Sorensen M, Kehlet H, Ottesen B (2003) Short convalescence after vaginal prolapse surgery. Acta Obstet Gynecol Scand 82:359–366
Tolver MA, Strandfelt P, Bryld EB, Rosenberg J, Bisgaard T (2012) Randomized clinical trial of dexamethasone versus placebo in laparoscopic inguinal hernia repair. Br J Surg 99:1374–1380
Currie A, Andrew H, Tonsi A, Hurley PR, Taribagil S (2012) Lightweight versus heavyweight mesh in laparoscopic inguinal hernia repair: a meta-analysis. Surg Endosc 26:2126–2133
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Rosenberg reports Grants from Baxter Healthcare, Grants from Johnson & Johnson, Grants and personal fees from Bard, personal fees from Merck, outside the submitted work. Dr. Bisgaard reports Grants from Johnson & Johnson, Covidien, Baxter Healthcare and travel/accommodation expenses for international meetings covered by Baxter Healthcare. Mette A. Tolver has no conflicts of interest or financial ties to disclose
Rights and permissions
About this article
Cite this article
Tolver, M.A., Rosenberg, J. & Bisgaard, T. Convalescence after laparoscopic inguinal hernia repair: a qualitative systematic review. Surg Endosc 30, 5165–5172 (2016). https://doi.org/10.1007/s00464-016-4863-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4863-4