Abstract
The purpose of this study was to compare a lightweight mesh to a standard polypropylene hernia mesh in endoscopic extraperitoneal hernioplasty in recurrent hernias. A total of 140 men with recurrent unilateral inguinal hernias were randomised to a totally extraperitoneal endoscopic hernioplasty (TEP) with Prolene or VyproII in a single-blinded multi-center trial. The randomisation and all data handling were performed through the Internet. 137 patients were operated as allocated. Follow-up was completed in 88% of the patients. The median operation times were 55 (24–125) min and 53.5 (21–123) min for the Prolene and VyproII groups, respectively. The meshes had comparable results in the surgeon’s assessment of the handling of the mesh, return to work, return to daily activities, complications, postoperative pain and quality of life during the first 8 weeks of rehabilitation, except in General Health (GH) SF-36, where the VyproII-group had a significantly better score (P=0.045). The use of Prolene and VyproII-meshes in endoscopic repair of recurrent inguinal hernia seems to result in similar short-term outcomes and quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of prosthetic meshes in the treatment of primary and especially in recurrent inguinal hernias has increased significantly due to improved results especially in the durability of the repair [1]. An open re-operation after an open primary hernioplasty has been shown to increase the incidence of chronic pain [1], whereas the risk of chronic pain after laparoscopic hernioplasties seems to be lower compared to open repairs [2, 3]. The possibility of avoiding scar tissue as well as promising results has made laparoscopic surgery recommendable in recurrent cases [4–6].
The material in the most commonly used mesh, polypropylene, is associated with a strong foreign-body reaction with such potentially harmful side effects as chronic inflammation and decreased abdominal wall compliance [7]. The extent of the foreign-body reaction with its provoked scar tissue formation depends on the amount and structure of the incorporated material [8]. A mesh with 30% polypropylene, higher elasticity, and larger pores (VYPRO; Ethicon GmbH, Hamburg, Germany) has been developed for incisional hernia repair [9]. This mesh proved to be favourable in both experimental and clinical studies with a reduced inflammatory reaction and a better abdominal wall function [10, 11]. In consideration of the benefits of this mesh, a new mesh with temporarily increased stiffness has been developed for inguinal tension-free repair (VYPROII; Ethicon GmbH, Hamburg, Germany). This mesh consists of 50% polyglactin and 50% polypropylene. It has been proven favourable in experimental studies [8], but not yet in a clinical setting.
The effectiveness of lightweight meshes in the group of recurrent inguinal hernias has not been studied yet. We designed an Internet-based, multicenter study to compare the outcomes in patients operated either with a standard polypropylene mesh or a new polypropylene/polyglactin mesh, VyproII, in extraperitoneal endoscopic hernioplasty (TEP) of recurrent inguinal hernias. This paper reports the short-term results.
Patients and methods
We created a website and a database developed on a MSSQL 2000 platform, using active secure pages (ASP) on a Secure Server from Medscinet (Medscinet AB, Stockholm, Sweden) connected to the Internet by SSL (128 bits encryption) and secured behind password. Registration, confirming the patient’s eligibility, randomisation and filling of the follow-up data was done directly to the database with on-line validation of the data filling. The patients were blinded to which mesh they received.
Male patients over 25 years of age with a unilateral recurrent inguinal hernia were eligible to participate in the study. Patients not able to walk 500 m and patients not assumed to cooperate in the follow-up (e.g., due to language difficulties or drug abuse) were excluded. The patients were recruited and operated in the Surgical Departments of two Swedish and one Finnish University Hospitals and two Swedish County Hospitals. All patients had given their informed consent. The ethics committees in each of the participating hospitals approved the study.
The patients were operated on with totally extraperitoneal endoscopic inguinal hernioplasty (TEP) by surgeons with considerable experience in laparoscopic hernia surgery. A 12×15 cm piece of mesh (PROLENE, Ethicon GmbH, Hamburg, Germany or VYPROII, Ethicon GmbH, Hamburg, Germany) was used according to the assignment. The use of a balloon expander or fixation of the mesh with staples as well as prophylactic antibiotics, infiltration of local anaesthetics and postoperative analgesics were not stated in the protocol.
The patients received a diary assessing pre- and postoperative pain as well as health-related quality of life measured using SF-36 Health Survey [12, 13] for 8 weeks. Pain was assessed in four different positions (resting in bed, standing, walking, and in light straining while rising from horizontal to vertical position) on a 100 mm visual analogue scale (VAS). The measurements were performed preoperatively, on the first postoperative day and after 1, 2, 3, 4 and 8 weeks (SF-36 standard preoperatively and after 8 weeks, SF-36 acute on the other occasions). The patients were encouraged to return to work and normal activities as soon as possible and to enter the data and possible complications in the diary. They were advised to contact their surgeon if there were any postoperative problems or complications. After follow-up, all patient records were checked in the respective hospital to find possible additional complications.
We hypothesized that the use of the VyproII-mesh results in faster convalescence and less pain during the postoperative period. The follow-up time in this early study was 8 weeks, which is the time of absorption of polyglactin [14]. Randomisation was done immediately prior operation through a computer algorithm in blocks of four. The patients were blinded to which mesh they received, whereas the clinicians doing the follow-up examinations were aware of the patient’s allocation. The recurrence rate and long-term pain, will be addressed later after 1 and 5 years follow-up.
A ten-point difference in VAS-score (0–100) was chosen as clinically significant difference between the groups. Sixty-three patients were calculated to be needed in each group to have an 80% power to detect this difference (α=0.05, β=0.20). We estimated a 10% loss of patients during follow-up. Thus, the sample size was calculated to be a total of 140 patients.
The data were analysed using Statistica (v 6.0, StatSoft Inc., Tulsa, Oklahoma, USA), Statxact (v5, Cytel, Cambridge, Mass, USA) and the Statistical Package for Social Sciences for Windows, version 11.0 (SPSS, Chicago, Illinois, USA). The Standard Normal Deviate (SND-test), χ2 - tests and Fisher’s Exact-tests were used to assess the differences between categorical data. Continuous data was analysed using Mann–Whitney U-test. SF-36 and VAS is ordinal data, illustrated in box-plots and analysed using a stratified Mann-Whitney test. Confidence intervals were used as appropriate. A P-value < 0.05 was considered statistically significant. The results are given as median and range if not stated otherwise.
Results
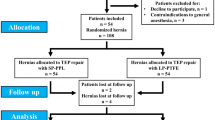
A total of 140 patients were recruited between March 2001 and December 2003, of whom 137 were operated as allocated (Fig. 1). There were three postrandomisation exclusions due to the use of wrong mesh (1 patient) and due to incorrect randomisation (2 patients). Follow-up with returned diaries was complete in 59/69 (87%) in the Prolene group and in 62/68 (91%) in the VyproII group. Follow-up was ended in February 2004 when all possible diaries were returned. The baseline variables between the groups were almost identical (Table 1). Testicular atrophy due to previous hernia surgery was seen with two patients (3%) in each group in the preoperative clinical examination.
The median (range) operation times (skin-to-skin) were 55 (24–125) min and 53.5 (21–123) min in the Prolene and VyproII groups, respectively (P=0.9). The use of a balloon expander was similar between the groups, Prolene 37 (54%) and VyproII 34 (50%) (P=0.6). A stapler was used to fix the mesh in 33 (48%) and 38 (56%) patients, respectively (P=0.3). An asymptomatic contralateral hernia was discovered in four patients (Prolene: one, VyproII: three). There were no significant differences between the groups in terms of surgeons’ subjective assessment of technical difficulty of the operation or placement of the mesh (Fig. 2).
Forty-six (67%) patients in the Prolene group and 51 (75%) in the VyproII group were operated as outpatients (P=0.3). The median hospital stay in the admitted patients was 1 (1–2) and 1 (1–3) days, respectively (P=0.4). The time to return to work was 13 (3–32) days in the Prolene group and 12 (0–31) days in the VyproII group (P=0.7). The time to return to normal daily activities was 13 (1–67) days in the Prolene group and 15 (2–74) days in the VyproII group (P=0.6).
There were no major operative complications. Minor complications included significant peritoneal tears (five cases), diffuse bleeding (two) and inferior epigastric vessel injury (one). Postoperative complications within 8 weeks were rare and similar between the groups (Table 2). One operation (Prolene-group) was converted to an open mesh hernioplasty due to dense adhesions in the preperitoneal space. The only reported infections were a superficial infection at the umbilical wound site and infection of the urinary tract. There were no differences between the groups concerning VAS- and SF-36-scores (Figs. 3, 4), except in General Health (GH) and bodily pain (BP), where the score was significantly higher in the VyproII group (P=0.05).
Discussion
In this Internet based, multicenter study, we were able to demonstrate that the short-term results of TEP with either Prolene or VyproII in recurrent unilateral hernias are comparable. Carrying through this study was significantly facilitated by the use of database through the Internet, as also previously described [15, 16]. The participating surgeons and staff appreciated the possibility for each centre to enter their own data directly in the database, simplicity of data handling, study monitoring, continuous feedback through the internet, which enhanced the security, validity and data management. There were no unnecessary delays as the data was immediately ready for statistical analysis.
VyproII is significantly smoother than Prolene, thus the handling of the mesh is different compared to Prolene. However, we found no difference between the meshes in the operation times or the surgeons’ subjective assessment of difficulty of mesh placement, which is consistent with the results of our previously published trial in open Lichtenstein hernioplasty [15].
The complications were few and did not differ significantly between the groups. Peroperative complications occurred more often in Prolene group, however, none of those were mesh related. Laparoscopic hernia operations have been criticized due to higher risk for major intraabdominal complications and recurrencies [17, 18] as compared to open hernia repair. There were no intraabdominal complications in this study even though the study population was more challenging due to recurrent disease. In larger series the TEP technique has been associated with extremely low risk for peroperative complications [6, 19]. The TEP technique seems also to be superior to transabdominal laparoscopic hernioplasty (TAPP) in this respect [20, 21]. The only reported infectious complications in this series were one urinary tract and one umbilical wound infection.
Even though there is data showing that the risk of long-term or chronic pain with mesh repairs is actually decreased compared to non-mesh repairs [2], there are also concerns that the use of mesh could actually increase chronic discomfort and pain in the operated groin [22–24]. According to the Swedish hernia registry, the incidence of chronic pain seems to be significantly higher after an open re-operation of recurrent inguinal hernia [1]as compared to a primary open operation. The risk of chronic pain after laparoscopic hernioplasties seems to be lower compared to open repairs [2, 3]. Thus, it is possible that the advantages of endoscopic techniques in this respect in recurrent hernias could be even greater. The risk for hernia recurrence after repair of recurrent hernia seems to be similar after open mesh and laparoscopic hernias repair according to data from Swedish hernia registry [1], whereas Neumayer and colleagues reported that laparoscopic repair is slightly better in this aspect [18].
Theoretically a lighter and softer mesh might be beneficial concerning nerve entrapment and/or pain by creating less fibrosis [8], and also appear softer against the surrounding tissues. Since the incidence of prolonged or chronic pain after laparoscopic repair is low [25], the possible difference between these two meshes can be extremely difficult to demonstrate requiring a significantly larger study population.
In our study there were only two patients reporting some discomfort or pain in the operated area. Postoperative pain and function did not differ between the groups as measured with VAS or SF-36 except in GH and BP SF-36, where the VyproII group had a better score than the Prolene group. However, the clinical significance of this finding is questionable as shown in Fig. 4. This interpretation is supported by author similar other trial (in press) carried out by our group, where no differences were found in bilateral hernia operated using Prolene or VyproII using TEP-technique. The laparoscopic approach in recurrent hernias resulted in equivalent or superior scores in pain (VAS) and quality of life (SF-36) than a Lichtenstein method in unilateral primary hernias, when comparing these results to our previous study [15]. Thus, laparoscopic approach is definitely a valid method in recurrent hernias.
In conclusion, the short-term results of an extraperitoneal endoscopic repair of recurrent unilateral hernias with either Prolene or VyproII were similar, with some advantages in the VyproII group. However long-term results are needed to be able to establish whether the lightweight meshes carry similarly low recurrence rates than standard meshes and whether or not they lower the risk for chronic groin pain.
References
Haapaniemi S, Gunnarsson U, Nordin P, Nilsson E (2001) Reoperation after recurrent groin hernia repair. Ann Surg 234:122–126
Collaboration EHT (2002) Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg 235:322–332
Kumar S, Wilson RG, Nixon SJ, Macintyre IM (2002) Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg 89:1476–1479
Frankum CE, Ramshaw BJ, White J, Duncan TD, Wilson RA, Mason EM, Lucas G, Promes J (1999) Laparoscopic repair of bilateral and recurrent hernias (discussion 842–843). Am Surg 65:839–842
Kumar S, Nixon SJ, MacIntyre IM (1999) Laparoscopic or Lichtenstein repair for recurrent inguinal hernia: one unit’s experience. J R Coll Surg Edinb 44:301–302
Tamme C, Scheidbach H, Hampe C, Schneider C, Kockerling F (2003) Totally extraperitoneal endoscopic inguinal hernia repair (TEP). Surg Endosc 17:190–195
Klinge U, Klosterhalfen B, Muller M, Schumpelick V (1999) Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg 165:665–673
Junge K, Klinge U, Rosch R, Klosterhalfen B, Schumpelick V (2002) Functional and morphologic properties of a modified mesh for inguinal hernia repair. World J Surg 26:1472–1480
Klinge U, Klosterhalfen B, Muller M, Anurov M, Ottinger A, Schumpelick V (1999) Influence of polyglactin-coating on functional and morphological parameters of polypropylene-mesh modifications for abdominal wall repair. Biomaterials 20:613–623
Junge K, Klinge U, Prescher A, Giboni P, Niewiera M, Schumpelick V (2001) Elasticity of the anterior abdominal wall and impact for reparation of incisional hernias using mesh implants. Hernia 5:113–118
Welty G, Klinge U, Klosterhalfen B, Kasperk R, Schumpelick V (2001) Functional impairment and complaints following incisional hernia repair with different polypropylene meshes. Hernia 5:142–147
Sullivan M, Karlsson J (1994) SF-36 Hälsoenkät Manual och tolkningsguide, Sahlgrenska sjukhuset, Göteborg, Sweden
Sullivan M, Karlsson J (1998) The Swedish SF-36 Health Survey III. Evaluation of criterion-based validity: results from normative population. J Clin Epidemiol 51:1105–1113
Matlaga BF, Salthouse TN (1983) Ultrastructural observations of cells at the interface of a biodegradable polymer: Polyglactin 910. J Biomed Mater Res 17:185–197
Bringman S, Heikkinen TJ, Wollert S, Osterberg J, Smedberg S, Granlund H, Ramel S, Fellander G, Anderberg B (2004) Early results of a single-blinded, randomized, controlled, Internet-based multicenter trial comparing Prolene and Vypro II mesh in Lichtenstein hernioplasty. Hernia 8:127–134
Bringman S, Wollert S, Österberg J, Smedberg S, Granlund H, Felländer G, Heikkinen T (2004) One year results of a single-blinded, randomised, controlled, Internet-based multi-centre trial comparing Prolene and VyproII-mesh in Lichtenstein hernioplasty. Hernia (submitted)
McCormack K, Scott NW, Go PM, Ross S, Grant AM (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev:CD001785
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R, Jr., Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Ramshaw B, Shuler FW, Jones HB, Duncan TD, White J, Wilson R, Lucas GW, Mason EM (2001) Laparoscopic inguinal hernia repair: lessons learned after 1224 consecutive cases. Surg Endosc 15:50–54
Ramshaw BJ, Tucker JG, Conner T, Mason EM, Duncan TD, Lucas GW (1996) A comparison of the approaches to laparoscopic herniorrhaphy. Surg Endosc 10:29–32
Felix EL, Michas CA, Gonzalez MH Jr (1995) Laparoscopic hernioplasty. TAPP vs TEP. Surg Endosc 9:984–989
Heise CP, Starling JR (1998) Mesh inguinodynia: a new clinical syndrome after inguinal herniorrhaphy? J Am Coll Surg 187:514–518
Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19:48–54
Callesen T, Bech K, Kehlet H (1999) Prospective study of chronic pain after groin hernia repair. Br J Surg 86:1528–1531
Collaboration EH (2000) Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87:860–867
Acknowledgements
The authors are grateful to RN Cajsa Barthelsson, RN Christina Lindblom, RN Sirpa Jämsä and secretary Lise-Lotte Lindh for their skillful work on the study. The study was supported by a grant from Ethicon Scandinavia and from the County Council of Stockholm.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heikkinen, T., Wollert, S., Österberg, J. et al. Early results of a randomised trial comparing Prolene and VyproII-mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia 10, 34–40 (2006). https://doi.org/10.1007/s10029-005-0026-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-005-0026-6