Abstract
Species of the genus Acanthamoeba are free-living protozoans that occasionally act as parasites, causing a severe, progressive corneal infection termed Acanthamoeba keratitis (AK). The variable pathogenic potential among Acanthamoeba lineages has been shown by in vitro assays, but little is known about the behavior of different strains in animal models of AK. This work aimed to evaluate the infectivity of Acanthamoeba from distinct morphological groups and genotypes in a rat model of AK and apply an immunohistochemical technique for histological characterization of the lesions. Only a strain classified as group I/genotype T17, isolated from a soil source, caused ulcerated corneal lesions in two Wistar rats (n = 9) subjected to intrastromal inoculation. Two strains derived from AK human cases (group II/genotype T4 and group III/genotype T5) did not induce corneal lesions in the rats. A previous association of group II/genotype T4 trophozoites with lethally irradiated Escherichia coli did not influence the infectivity. A hyperimmune serum produced in Wistar rats was validated by an immunocytochemical technique using the three distinct strains and then applied for immunohistochemistry. The abundance of antigenic residues was observed in both corneas with keratitis, suggesting that the infectious process tended to resolve. Despite the low infection rate of the AK Wistar rat model, we produced an immunochemical tool with a potential diagnostic application. We also showed for the first time the ability of Acanthamoeba from T17 genotype to cause AK in experimental conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acanthamoeba keratitis (AK) is a painful, sight-threatening corneal infection caused by free-living protozoa found in virtually all terrestrial and aquatic environments (Siddiqui and Khan 2012). The contact of Acanthamoeba trophozoites with the injured cornea triggers the eventual amoeba parasitic behavior, which involves the interaction of amoebic surface mannose-binding proteins (MBP) with mannose residues on the host cells (Clarke and Niederkorn 2006; Garate et al. 2006; Guzmán-Téllez et al. 2020). Contact lens wears are the main group risk since the accessories promote corneal micro-abrasions and can also be a vehicle of contamination (Siddiqui and Khan 2012). Some predisposing factors for AK among contact lens wears include using homemade saline solutions or tap water to wash the lens, prolonged improper use of the disposable lens, and swimming while using the lens (Kofman and Guarner 2021). A lower proportion of cases occurs in non-contact lens wearers, usually individuals who suffered an accidental corneal injury during occupational activities or contamination after surgical procedures (Garg et al. 2017; Erdem et al. 2014; Aykur and Dagci 2021).
Early clinical presentation of human AK includes epitheliopathy, epithelial opacities, and perineural infiltrates, followed by typical ring infiltrate, ulceration, and uveitis in the later stages (Dart et al. 2009). Patients diagnosed early and promptly initiate the specific treatment within 3 weeks tend to present a less severe disease and a better outcome. Conversely, the delayed diagnosis contributes to a worse inflammatory picture, resulting in complications that can cause corneal collapse and visual impairment (Dart et al. 2009; Kofman and Guarner 2021; Lorenzo-Morales et al. 2015).
The genus Acanthamoeba includes at least 18 early described species classified into three morphological groups according to the cyst morphology and size (Pussard and Pons 1977). However, a current system for classifying new isolates relies on analyzing 18S rDNA sequences, determining which 23 genotypes (T1 to T23) (Putaporntip et al. 2021). The genotypic and morphological diversity seems to reflect, in part, the variability in the pathogenic potential of Acanthamoeba since the genotype T4 and the morphological group II are predominant in AK cases and other infections (Marciano-Cabral and Cabral 2003; Maciver et al. 2013; Aykur and Dagci 2021). This variability is corroborated by several studies showing differences among Acanthamoeba lineages concerning properties accessed in vitro, such as thermotolerance, osmotolerance, proteases profile, and cytopathogenicity to culture cells (Walochnik et al. 2000; da Rocha-Azevedo and Costa E Silva-Filho 2007; Possamai et al. 2018; Cirelli et al. 2020). In vivo assays, in turn, confirmed the ability of certain strains to cause infection and access aspects of AK pathogenesis. The pioneers’ works on experimental infection in animal cornea showed rats as a suitable model for AK, also investigating histological features of lesions induced by intrastromal inoculation (Font et al. 1982; Larkin and Easty 1990; Badenoch et al. 1990). Several subsequent reports used the rat model and other species such as rabbits, pigs, hamsters, and mice (Côte et al. 1991; He et al. 1992; Van Klink et al. 1993; Polat et al. 2007; Ren and Wu 2010). More usual infection methods in these animal models are the application of parasite-laden contact lens in the animals’ eyes (He et al. 1992; Van Klink et al. 1993, Feng et al. 2015) and intrastromal inoculation (Font et al. 1982; Larkin and Easty 1990; Polat et al. 2007). Comparing these methods in rats and mice along with the application of amoebic suspension in the scratched cornea, Ren and Wu (2010) showed that intrastromal inoculation results in higher infection rates. In general, all these animal models have a self-limited disease, an aspect that differs from human AK, but histopathological alterations in cornea are similar to those seen in humans. Additionally, these studies evaluate a single strain isolated from AK case to improve the chance of efficiency, but a comparative analysis of different Acanthamoeba genotypes has not been reported in the rat model of AK. Thus, this work aimed to evaluate three strains of Acanthamoeba from different groups and genotypes regarding their ability to cause keratitis in Wistar rats. Additionally, an Acanthamoeba antiserum was produced and used in an immunohistochemical technique to complement the histopathological characterization of the lesions.
Material and methods
Acanthamoeba cultures
Three Acanthamoeba strains, previously isolated and characterized by Possamai et al. (2018), were used in the attempts to induce keratitis in rats. Strains Krt2.AAO (morphological group II/genotype T4) and Krt16.PEN (morphological group III/genotype T5) were isolated from keratitis cases, while the source of the SoA1 strain (morphological group I/genotype T17) was a soil sample. The cultures stored in non-nutrient agar (NNA) (Page 1988) were reactivated by passages in plates with fresh NNA containing Escherichia coli and then subjected to axenization in PYG (protease, yeast extract, and glucose) as previously described (Possamai et al. 2018). Axenic cultures were incubated at 32 °C in tissue flasks and subcultured for up five passages before being used in the experiments. An additional sample termed Krt2.iBac was included to evaluate whether bacteria’s presence could increase the lesions’ severity. For this purpose, the Krt2.AAO culture was associated with E. coli previously inactivated by gamma radiation (10,000 Gy at the Nuclear Technology Development Center—Federal University of Minas Gerais). One hundred microliters of E. coli suspension was added to fresh PYG at an amoeba-bacteria ratio of 1:50. The co-culture was incubated at 32 °C for 72 h and then subcultured four times before the assays.
Experimental keratitis in Wistar rats
Trophozoites from cultures in exponential growth phase (72–96 h) were washed three times in Page’s saline (2.5 mM NaCl, 1 mM KH2PO4, 0.5 mM Na2HPO4, 40 mM CaCl2, and 20 mM MgSO4) by centrifugation (300 × g, 10 min), suspended in PBS pH 7.2, and quantified in Neubauer chamber. Viability checking was performed by trypan blue exclusion and samples with ≥ 98% of viable cells were then adjusted to the concentration of 1.25 × 107 trophozoites/mL. The culture with irradiated E. coli (termed Krt2-iBac) has the bacteria concentration evaluated to determine the inoculum in controls.
Forty-five male Wistar rats, 45 days old, were used in the experiments. The animals were raised in the Bioterium of Pharmacy Faculty, Federal University of Minas Gerais. All procedures were conducted under accepted guidelines for the care and use of laboratory animals for research and approved by the Ethical Committee for Animals of the Federal University of Minas Gerais, protocol number 265/2018. Inoculations were performed as previously described by Ren and Wu (2010), with modifications. The animals were anesthetized with 60 mg/kg ketamine HCl (Vetanarcol®, König do Brasil, Brazil) and 7.5 mg/kg xylazine (Dopaser®, Calier, Spain) by intraperitoneal injection. Sterilized physiological saline was used to wash the left eyes, which were then anesthetized with topical 2% lidocaine. A 31G needle with 2 μL suspension containing 2.5 × 104 trophozoites was used in the intrastromal inoculation in the left eye. The right eye was inoculated with 2 μL of PBS. Groups of nine animals were infected with each Acanthamoeba strain (Krt2.AAO; Krt16.PEN, SoA1, and Krt2.iBac). A fifth group was inoculated with 1.5 × 105 forms of inactivated E. coli as a control. Seven days after the inoculation, euthanasia was performed using a triple dose of anesthetics, and the lesions were evaluated concerning the damage presence or grade, as follows: grade I, point of opacity limited to the region of inoculum, > 1 mm in diameter; grade II, point of opacity > 1 mm, clearly surpassing the initial point of inoculum, occupying until 50% of the cornea; and grade III, damaged area with more than 50% of the cornea. The eyeballs were removed, fixed in 10% buffered formalin (in PBS pH 7.2), and subjected to conventional histological preparation (dehydration in alcoholic solutions, clarification in xylene, paraffin inclusion, and 4-µm thick section).
Acanthamoeba antiserum production
Antiserum against Acanthamoeba was produced in Wistar rats (male, 90 days old) with antigens of the A. castellanii strain ALX (morphological group II/genotype T4). Briefly, 2 × 107 trophozoites grown in PYG medium were washed by centrifugation and suspended in 2 mL of PBS pH 7.2. Raw antigen was produced by sonication, using a 5-pulse schedule of 99 watts of 1 min with 60-s intervals. The first immunization was performed intraperitoneally with 200 μL of the crude antigen. The second immunization was carried out 15 days after the first by subcutaneous route, with 100 μL of antigen and 100 μL of incomplete adjuvant of Freund.
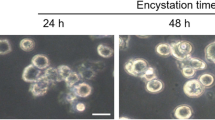
Immunocytochemical staining
Serum quality and reactivity were validated by immunocytochemical reaction, using trophozoites and cysts from the three strains (Krt2.AAO, Krt16.PEN, and SoA1). Cysts were induced in Neff’s encystment saline (95 mM NaCl, 5 mM KCl, 8 mM MgSO4, 0.4 mM CaCl2, 1 mM NaHCO3, and 20 mM Tris–HCl, pH 9.0). Smears of both amoebic stages in glass slides were fixed in 90% alcohol at room temperature for 72 h and then washed in saline solution PBS pH 7.2 for 5 min. After incubation with 0.2% peroxide hydrogen solution (20 min), the slides were incubated with the blocking solution “Animal-Free Blocker” (Vector Laboratories, Burlingame, USA) in a moist chamber for 1 h at 4 °C. Acanthamoeba antiserum at concentration 1:1000, previously diluted in bovine serum albumin (BSA) 5%, was used to react with the samples for 18 h at 8 °C. The slides were then washed in PBS pH 7.2 for 5 min and incubated for 1 h at room temperature with goat anti-mouse IgG biotinylated and streptavidin (Zymed Laboratories, San Francisco, CA, USA), both diluted in 5% BSA at concentration 1:100. The reaction was revealed using a solution of 0.05% diaminobenzidine and 0.2% peroxide hydrogen. The slides were then stained with Harris hematoxylin diluted 1:2 for 2 s. For the negative control, Acanthamoeba antiserum was replaced by PBS. After dehydration with alcoholic solutions and clarification in xylol, the slides were mounted with Entellan (Sigma-Aldrich, St. Louis, USA).
Histopathological and immunohistochemical analysis
Paraffin-embedded sections were processed for hematoxylin–eosin (HE) by standard techniques. For immunohistochemical staining, the sections were dewaxed in xylol, hydrated in decreasing gradient of alcoholic solutions, and washed in PBS pH 7.2. Subsequent treatments of immunochemical staining followed the procedures described in the previous subsection (“Immunocytochemical staining”). Histological evaluation was performed in an Axiolab microscope (Carl Zeiss, Oberkochen, Germany), and digitized images were taken with QColor3 Olympus attached micro camera (Tokyo, Japan).
Results
The strains Krt2.AAO and KRT16.PEN, as well as Krt2 associated with bacteria, did not induce typical AK lesions in the rat corneas, as shown in Table 1. In animals inoculated with these strains, the eyes were normal or presented a superficial ulcer at the inoculum point characterized as grade 0 (Fig. 1b). Inoculation of E. coli alone did not result in changes in the animals’ corneas either (Table 1). The right eyes inoculated with PBS as controls presented a normal condition (Fig. 1a). Only one eye among the controls exhibited ulceration, as seen in Fig. 1b, probably caused by physical trauma of the needle and without signs of inflammation.
Acanthamoeba keratitis induced in Wistar rats by intrastromal inoculation of 2.5 × 10.4 trophozoites. a Left eye of PBS-treated rat, with normal macroscopic appearance. b Right eye of a rat inoculated with the strain Krt2. AAO (group II/genotype T4), with a grade 0 superficial ulcer. c Right eye of a rat inoculated with the SoA1 strain (group I/genotype T17), with a 2-mm necrotic point of inoculation and superficial opacity in other areas occupying less than 50% of the cornea (grade II). d Right eye of a rat inoculated with the strain SoA1 with an extensive corneal opacity with a central area of necrosis (grade III lesion)
Only the SoA1 strain could induce AK in 2 out of 9 rats, representing an infectivity rate of 22% (Table 1). One of the animals presented opacity in less than 50% of the cornea, with an evident and delimited necrotic lesion of 2 mm, characterizing injury of grade II (Fig. 1c). The other animal presented a grade III lesion, occupying more than 75% of the cornea, with an extensive zone of corneal opacity with a necrosis center (Fig. 1d).
Histological analysis evidenced this necrotic central area, which showed corneal epithelium and Bowman’s membrane disappearance. It also showed large amounts of cell debris and deposited fibrin, bordered by abundant granulation tissue. Neutrophils and intervening macrophages were present in different areas of the ulcer (Fig. 2c–g). The inflammatory process was also seen in the ciliary body, ciliary muscle, and iris, characterizing anterior uveitis (Fig. 2h). The histological aspect of the grade II lesion was like the previous one, but the necrotic alteration occupied a more restricted area. Histology of eyes inoculated with PBS presented a regular aspect and absence of alteration in the corneal epithelium (Fig. 2a–b).
Histopathological aspects of Acanthamoeba keratitis induced in Wistar rats by intrastromal inoculation with 2.5 × 104. trophozoites (SoA1 strain, group I/genotype T17). a Panoramic view of an eye inoculated with PBS (control) and presenting a regular aspect, showing the corneal region (big arrow), anterior chamber (Ca), iris (small arrows), lens (C), sclera (E), posterior chamber (Cp), and retina (#). b Detail of the area delimited by the rectangle in the previous image, showing the normal corneal epithelium (Ep) and corneal stroma (Es), Bowman’s membrane (arrowheads), Descemet’s membrane (heads), and endothelium (En). c Panoramic view of a corneal ulcer induced by the SoA1 strain. Corneal epithelium had collapsed (arrows), and areas of necrosis (N) with granulation tissue (Tg). Other structures, such as the iris and ciliary body (U), ciliary muscle (M), and sclera (E), are inflamed. d Higher magnification of the previous image showing the necrotic (arrowhead) and non-necrotic (*) corneal epithelium, as well as other areas of necrosis (N) and with granulation tissue (Tg). e Detail of the area delimited by the square in the previous image, showing a higher magnification of epithelium necrosis (*), cellular debris, and granulocytes (#). f Hemorrhagic necrosis with fibrin deposition (*) separates an area of necrosis (N) and granulation tissue (Tg). g Area of inflammatory infiltrate showing hyperemia and edema of the ciliary body (Cc) and iris (#). Inflammatory cells, hemorrhage, and desquamated cells in the anterior chamber (arrowheads)
An Acanthamoeba antiserum was produced to validate immunocytochemical and immunohistochemical staining, as the trophozoites and cysts could not be visualized even in corneas with active lesions. Trophozoites and cysts of the three strains were positively marked by peroxidase in a brownish color (Fig. 3a–f), while the control samples had blue-gray coloration (Fig. 3g–h). Immunohistochemical analysis of lesions (SoA1 strain) indicated granular material and brown coloration in many areas of the corneal stroma, both in the extracellular environment and inside the inflammatory cells, proving the presence of Acanthamoeba antigens, probably derived from destroyed trophozoites (Fig. 4c–d). An immunolabeled trophozoite was found in the corneal stroma of a rat with a grade III lesion (Fig. 4d). Replacing polyclonal serum with PBS solution produced a negative reaction, as evidenced by the absence of brown coloration throughout the histological sections (Fig. 4a–b).
Anti-Acanthamoeba immunocytochemical reaction. A brownish coloration in trophozoites (a, c, e) and cysts (b, d, f) from the strains Krt2.AAO (group II/genotype T4) (a–b), Krt16.PEN (group III/genotype T5) (c–d), and SoA1 (group I/genotype T17) (e–f) characterized a positive reaction (a–f). Negative reaction: PBS replaced the anti-serum for samples with trophozoites (g) and cysts (h) of the strain Krt2.AAO. Bars = 20 μm
Immunohistochemical marking of Acanthamoeba antigens in the cornea of Wistar rats inoculated with the SoA1 (group I/genotype T17) strain. a–b Negative reaction control in which PBS replaced the anti-serum. Note the absence of brownish coloration. c Panoramic view of the stroma with positive marking evidenced by brownish coloration (*). d. High magnification image showing positive antigenic material (arrowheads) and a trophozoite in the corneal stroma (arrow). Bars = 50μm
Discussion
In the present work, we compared three Acanthamoeba strains from distinct morphological groups and genotypes regarding their ability to induce keratitis in Wistar rats. Evidence indicates that Acanthamoeba from genotype T4 or morphological group II is more prone to act as pathogens (Maciver et al. 2013). However, in vivo or in vitro pathogenicity traits can be detected in strains from other genotypes and groups isolated from patients or the environment (Walochnik et al. 2000; Maciver et al. 2013; Carlesso et al. 2014). Thus, we selected strains representing the phenotypic and genotypic diversity in the Acanthamoeba genus. The samples induced no or low infection rates, which were particularly unexpected for two strains isolated from AK cases. They belong to genotypes/morphological groups primarily (T4/II) or secondarily (T5/III) associated with pathogenicity (Maciver et al. 2013; Walochnik et al. 2000; Carlesso et al. 2014; Possamai et al. 2018). Both did not tolerate 1 M, but the T4 strain (Krt2.AAO) grew at 37 °C and caused cytopathic effect (CPE) upon MDCK cells in a low score ( +), while the T5/III strain (Krt16.PEN) grew up to 40 °C and had high score (+ + +) of CPE (Possamai et al. 2018). As reported in other studies, attenuation of virulence may occur due to prolonged axenic culture (Mazur and Hadas 1994, Koehsler et al. 2009; Veríssimo et al. 2013), but we still excluded this possibility by using cultures shortly after axenization. Additionally, we tested an induction of pathogenicity by associating the T4 strain (Krt2.AAO) with inactivated E. coli before infection. The rationale for this strategy relied on a previous study indicating increased virulence of axenic E. histolytica in contact with lethally irradiated bacteria (Wittner and Rosenbaum 1970). We also considered the exacerbation of Acanthamoeba pathogenic behavior reported after interaction with Corynebacterium xerosis (Badenoch et al. 1990; Puech et al. 2001). However, even after the association, Krt2.AAO did not cause AK in the rats, suggesting that distinct mechanisms for pathogenicity induction could occur with different protozoans and types of bacteria.
Despite several reports of successful experimental AK in rats and other animals, failures in inducing infection may occur, which is a situation not always published (Niederkorn et al. 1999). Additionally, infectivity may not reach 100% in an experimental group. In a previous study using the Chinese hamster as AK model, 30 to 40% of the animals did not develop lesions, which was attributed to a pre-exposition to Acanthamoeba (Van Klink et al 1993). Thus, variation in laboratory animal batch, or even the individual differences in regard to the resistance and immunity, could be factors affecting AK susceptibility. Inoculum dose can also be an intervening factor, since a higher number of trophozoites concur for the infection success. Indeed, in this study, we conducted a pilot infection using inoculum dose in the order of 103 trophozoites (data not shown), a cell quantity similar to that reported previously with the rat model (Polat et al. 2007; Ren and Wu 2010; Ávila-Blanco et al 2020). However, none of the three strains caused AK, which leads us to adopt the inoculum of 2.5 × 104 trophozoites. The possibility of higher inoculums resulting in an increased infection rate cannot be excluded and remains to be determined. Finally, another hypothesis to be considered for the infection failure is related to intrinsic unknown features of the strains, which could not cause AK in the rat model. The well succeed corneal infections in rats by intra-stromal via reported previously (Polat et al. 2007; Ren and Wu 2010; Ávila-Blanco et al. 2020), including one by our group using similar inoculum (Costa et al. 2017), suggest that variable infectivity can be, in part, depending on Acanthamoeba lineage.
Surprisingly, only the environmental origin SoA1 strain, belonging to a genotype (T17) and morphological group (I) unusual in human infections, induced a typical AK lesion in the rats. Group I Acanthamoeba is uncommonly implicated in human infection and encompasses the genotypes T7, T8, T9, T17, and T18 (Magliano et al. 2012; Possamai et al. 2018). Regarding genotype T17, it was reported once in a post-lung transplant patient who progressed to severe amoebic encephalitis (D’auria et al. 2012) but not in AK cases (Diehl et al. 2021). Interestingly, SoA1 induced a high score of CPE on MDCK cells (Possamai et al. 2018). Altogether, these data corroborate the T17 genotype as pathogenic and suggest it as a potential causative agent of AK.
The lesions induced by the SoA1 strain were compatible with those described by other authors, including developing a corneal ulcer and the typical inflammatory process (Larkin and Easty 1990, 1991; Ávila-Blanco et al. 2020). In Acanthamoeba infections, trophozoites and cysts can be found in infected tissues (Visvesvara et al. 2007; Visvesvara 2010) and in this work, immune-peroxidase reaction labeled these stages independently of the strain. Furthermore, the efficiency of the immunohistochemical technique was ratified by in situ labeling of antigenic material. The abundance of antigenic debris and rarity of amoebic forms is consistent with a tendency to resolution, a fact expected in the Wistar rat model for AK in which the lesions can be induced but regressed until healing (Polat et al. 2007; Ren and Wu 2010; Ávila-Blanco et al. 2020).
Usually, the routine hematoxylin and eosin (HE) complemented or not by special staining such as periodic acid-Schiff (PAS) allows visualizing the presence of amoebic stages in histological sections (Feng et al. 2015; Ávila-Blanco et al. 2020). Nevertheless, the identification may be impaired if the amoebic forms do not present structural integrity, as in our study. In this context, immunohistochemistry allows identifying both amebic stages and their antigenic residues. Immunohistochemistry was applied along HE and PAS by Ávila-Blanco et al. (2020), which used heterologous antiserum produced from Entamoeba histolytica antigens, showing these ameboid protists share antigenic components. However, the Acanthamoeba-specific antiserum from our study has applicability not only for in situ immunolabeling but also as a tool for other assays that demand higher specificity (e.g., immunogenic proteins identification), or even for diagnostic purposes. Indeed, the immunohistochemical technique had improved sensitivity compared to other diagnostic methods as the Calcofluor White stain and culture technique (Sharma et al. 2001).
In conclusion, although the AK model resulted in a low infective rate in the conditions adopted in this work, we showed for the first time the ability of Acanthamoeba from genotype 17 to cause AK in experimental conditions. The immunocytochemical and immunohistochemical methods proved effective for labeling distinct strains and stages of Acanthamoeba, with perspectives for laboratory diagnostic of AK.
Data availability
Not applicable
References
Ávila-Blanco ME, Martín-Pérez T, Ventura-Juárez J, Pérez-Serrano J (2020) Experimental keratitis in rats caused by Acanthamoeba griffini: a kinetic histopathological study. Parasite Immunol 42:e12692
Aykur M, Dagci H (2021) Evaluation of molecular characterization and phylogeny for quantification of Acanthamoeba and Naegleria fowleri in various water sources. Turkey Plos One 16:e0256659
Badenoch PR, Johnson AM, Christy PE, Coster DJ (1990) Pathogenicity of Acanthamoeba and a Corynebacterium in the rat cornea. Arch Ophthalmol 108:107–112
Carlesso AM, Mentz MB, da Machado ML, Carvalho A, Nunes TE, Maschio VJ, Rott MB (2014) Characterization of isolates of Acanthamoeba from the nasal mucosa and cutaneous lesions of dogs. Curr Microbiol 68:702–707
Cirelli C, Mesquita EIS, Chagas IAR, Furst C, Possamai CO, Abrahão JS, Dos Santos Silva LK, Grossi MF, Tagliati CA, Costa AO (2020) Extracellular protease profile of Acanthamoeba after prolonged axenic culture and after interaction with MDCK cells. Parasitol Res 119:659–666
Côte MA, Irvine JA, Rao NA (1991) Evaluation of the rabbit as a model of Acanthamoeba keratitis. Rev Infect Dis 13:443–444
Clarke DW, Niederkorn JY (2006) The pathophysiology of Acanthamoeba keratitis. Trends Parasitol 22:175–180
Costa AO, Furst C, Rocha LO, Cirelli C, Cardoso CN, Neiva FS, Possamai CO, Santos DA, Thomaz-Soccol V (2017) Molecular diagnosis of Acanthamoeba keratitis: evaluation in rat model and application in suspected human cases. Parasitol Res 116(4):1339–1344
Dart JKG, Saw VP, Kilvington S (2009) Acanthamoeba keratitis diagnosis and treatment update. Am J Ophthalmol 148:487–499
D’Auria A, Jaime L, Geiseler P, Qvarnstrom Y, Bandea R, Roy SL, Sriram R, Paddock C, Zaki S, Kim G, Visvesvara GS (2012) Cutaneous acanthamoebiasis with CNS involvement post-transplantation: implication for differential diagnosis of skin lesions in immunocompromised patients. J Neuro-Oncol 3:1–7
Diehl MLN, Paes J, Rott MB (2021) Genotype distribution of Acanthamoeba in keratitis: a systematic review. Parasitol Res 120(9):3051–3063
da Rocha-Azevedo B, Costa E Silva-Filho F (2007) Biological characterization of a clinical and an environmental isolate of Acanthamoeba polyphaga: analysis of relevant parameters to decode pathogenicity. Arch Microbiol 188:441–449
Erdem E, Evcil Y, Yagmur M, Eroglu F, Koltas S, Ersoz R (2014) Non-contact lens use-related Acanthamoeba Keratitis in southern Turkey: evaluation of risk factors and clinical features. Eur J Ophthalmol 24:164–172
Feng X, Zheng W, Wang Y, Zhao D, Jiang X, Lv S (2015) A rabbit model of Acanthamoeba keratitis that better reflects the natural human infection. Anat Rec (hoboken) 298:1509–1517
Font RL, Tapert MJ, Robinson NM, Visvesvara GS, Murphy D, Osato MS (1982) An animal model of Acanthamoeba keratitis. Further studies with emphasis on the early phase destruction of the trophozoites. Invest Ophthalmol Vis Sci 22:S163
Garate M, Marchant J, Cubillos I, Cao Z, Khan NA, Panjwani N (2006) In vitro pathogenicity of Acanthamoeba is associated with the expression of the mannose-binding protein. Invest Ophthalmol Vis Sci 47:1056–1062
Garg P, Kalra P, Joseph J (2017) Non-contact lens related Acanthamoeba keratitis. Indian J Ophthalmol 65:1079–1086
Guzmán-Téllez P, Martínez-Castillo M, Flores-Huerta N, Rosales-Morgan G, Pacheco-Yépez J, la Garza M, Serrano-Luna J, Shibayama M (2020) Lectins as virulence factors in Entamoeba histolytica and free-living amoebae. Microbiology 15:919–936
He YG, McCulley JP, Alizadeh H, Pidherney M, Mellon J, Ubelaker JE, Stewart GL, Silvany RE, Niederkorn JY (1992) A pig model of Acanthamoeba keratitis: transmission via contaminated contact lenses. Invest Ophthalmol vis Sci 33:126–133
Koehsler M, Leitsch D, Duchêne M, Nagl M, Walochnik J (2009) Acanthamoeba castellanii: growth on human cell layers reactivates attenuated properties after prolonged axenic culture. FEMS Microbiol Lett 299(2):121–127
Kofman A, Guarner J (2021) Free living amoebic infections: review. J Clin Microbiol 60:e0022821
Larkin DFP, Easty DL (1990) Experimental Acanthamoeba keratitis: I. Preliminary Findings. Br J Ophthalmol 74:551–555
Larkin DFP, Easty DL (1991) Experimental Acanthamoeba keratitis: II Immunohistochernical evaluation. Br J Ophthalmol 75:421–424
Lorenzo-Morales J, Khan NA, Walochnik J (2015) An update on Acanthamoeba keratitis: diagnosis, pathogenesis and treatment. Parasite 22:10
Marciano-Cabral F, Cabral G (2003) Acanthamoeba spp. as agents of disease in humans. Clin Microbiol Rev 16:273–307
Maciver SK, Asif M, Simmen MW, Lorenzo-Morales J (2013) A systematic analysis of Acanthamoeba genotype frequency correlated with source and pathogenicity: T4 is confirmed as a pathogen-rich genotype. Eur J Protistol 49:217–221
Magliano AC, Teixeira MM, Alfieri SC (2012) Revisiting the Acanthamoeba species that form star-shaped cysts (genotypes T7, T8, T9, and T17): characterization of seven new Brazilian environmental isolates and phylogenetic inferences. Parasitology 139:45–52
Mazur T, Hadas E (1994) The effect of the passages of Acanthamoeba strains through mice tissues on their virulence and its biochemical markers. Parasitol Res 80(5):431–434
Niederkorn JY, Alizadeh H, Leher H, McCulley JP (1999) The pathogenesis of Acanthamoeba keratitis. Microbes Infect 1(6):437–443
Page FC (1988) A new key to freshwater and soil Gymnamoebae with instructions for culture. Freshwater Biological Association Scientific Pubhcations, Cumbria, England, p 122
Polat ZA, Ozcelik S, Vural A, Yildiz E, Cetin A (2007) Clinical and histologic evaluations of experimental Acanthamoeba keratitis. Parasitol Res 101:1621–1625
Possamai CO, Loss AC, Costa AO, Falqueto A, Furst C (2018) Acanthamoeba of three morphological groups and distinct genotypes exhibit variable and weakly inter-related physiological properties. Parasitol Res 117:1389–1400
Puech V, Chami M, Lemassu A, Lanéelle MA, Schiffler B, Gounon P, Bayan N, Benz R, Daffé M (2001) Structure of the cell envelope of corynebacteria: importance of the non-covalently bound lipids in the formation of the cell wall permeability barrier and fracture plane. Microbiology 147:1365–1382
Pussard M, Pons R (1977) Morphologies de la paroi kystique et taxonomie du genre Acanthamoeba (Protozoa, Amoebida). Protistologica 13:557–610
Putaporntip C, Kuamsab N, Nuprasert W, Rojrung R, Pattanawong U, Tia T, Yanmanee S, Jongwutiwes S (2021) Analysis of Acanthamoeba genotypes from public freshwater sources in Thailand reveals a new genotype, T23 Acanthamoeba bangkokensis sp. nov. Sci Rep 11:1–13
Ren M, Wu X (2010) Evaluation of three different methods to establish animal models of Acanthamoeba keratitis. Yonsei Med J 51:121–127
Sharma S, Athmanathan S, Ata-Ur-Rasheed M, Garg P, Rao GN (2001) Evaluation of immunoperoxidase staining technique in the of Acanthamoeba Keratitis. Indian J Ophthalmol 49:181–186
Siddiqui R, Khan NA (2012) Biology and pathogenesis of Acanthamoeba. Parasit Vectors 5:6
Van Klink F, Alizadeh H, He Y, Mellon JA, Silvany RE, McCulley JP, Niederkorn JY (1993) The role of contact lenses, trauma and Langerhans cells in a Chinese hamster model of Acanthamoeba keratitis. Investig Ophthalmol vis Sci 34:1937–1944
Veríssimo CDM, Maschio VJ, Correa APF, Brandelli A, Rott MB (2013) Infection in a rat model reactivates attenuated virulence after long-term axenic culture of Acanthamoeba spp. Mem Inst Oswaldo Cruz 108:832–835
Visvesvara GS (2010) Amebic meningoencephalitides and keratitis: challenges in diagnosis and treatment. Curr Opin Infect Dis 23:590–594
Visvesvara GS, Booton GC, Kelley DJ, Fuerst P, Sriram R, Finkelstein A, Garner MM (2007) In vitro culture, serologic and molecular analysis of Acanthamoeba isolated from the liver of a keel-billed toucan (Ramphastos sulfuratus). Vet Parasitol 143:74–78
Walochnik J, Haller-Schober E, Kölli H, Picher O, Obwaller A, Aspöck H (2000) Discrimination between clinically relevant and nonrelevant Acanthamoeba strains isolated from contact lens-wearing keratitis patients in Austria. J Clin Microbiol 38:3932–3936
Wittner M, Rosenbaum RM (1970) Role of bacteria in modifying virulence of Entamoeba histolytica. Am J Trop Med Hyg 19:755–761
Acknowledgements
The authors thank Maria Adelaide Fernandes for providing technical support to care for and breed the animals.
Funding
This work was supported by grants from the Fundação de Amparo à Pesquisa do Estado de Minas Gerais-FAPEMIG, APQ-01100–14.
Author information
Authors and Affiliations
Contributions
Adriana Oliveira Costa, Marcelo Vidigal Caliari, and Cinthia Furst conceived and designed the study, contributed to the data analysis, and supervised the experiments and manuscript writing. Norberto de Souza Fernandes planned and performed all the experiments and drafted the first version of the manuscript. Fabrício Marcos Silva Oliveira contributed to rat immunization and conducted and interpreted the immunochemical reactions. Alexandre Batista Costa Neto and Isabela Aurora Rodrigues contributed to animal manipulation, corneal inoculation, and figure formatting. All authors read and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures were conducted under accepted guidelines for the care and use of laboratory animals for research and approved by the Animal Experimentation Ethics Committee of the Federal University of Minas Gerais, protocol number 265/2018.
Consent to participate
Not applicable
Consent for publication
All the authors consent to this publication.
Competing interests
The authors declare no competing interests.
Additional information
Section Editor: Sutherland Maciver
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Souza Fernandes, N., Caliari, M.V., Oliveira, F.M.S. et al. Experimental keratitis induced in rat by Acanthamoeba from distinct morphological groups/genotypes: a histological and immunohistochemical evaluation. Parasitol Res 122, 1167–1175 (2023). https://doi.org/10.1007/s00436-023-07817-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-023-07817-3