Abstract
Purpose
Onflex™ mesh has replaced Polysoft™ patch on the market, without being clinically evaluated thus far in the transinguinal preperitoneal (TIPP) technique.
Methods
All consecutive TIPP registered in our registry during the overlap period of availability of both meshes were included and studied with the chronic postoperative inguinal pain (CPIP) as primary endpoint, assessed with a verbal rating scale (VRS), and included in a patient-related outcome measurement (PROM) phone questionnaire.
Results
A total of 181 Onflex cases vs 182 Polysoft cases were studied with a 2-year follow-up rate of 92% vs 88%. The overall rate of pain or discomfort was not statistically different in the 2 studied subgroups (16.5% vs 17.6%; p = 0.71), while moderate or severe pain were significantly more frequent in the Polysoft subgroup (5.5% vs 11.6%; p = 0.01). These symptoms did not interfere with the patient daily life in 16% vs 16.5% of cases, and they were self-assessed as more bothersome than the hernia in only 0.5% vs 0.5% of cases, suggesting an overestimation of the pain by the VRS. Patients assessed the result of their hernia repair as excellent or good in 97.8% vs 96.7% and medium or bad in 2.2% vs 3.3% (p = 0.53). The cumulative recurrence rate was 0% vs 2.2%. Two reoperations (one for early and one for late recurrence) were reported in the Polysoft subgroup (1%), none related to the non-absorbable memory ring.
Conclusions
These results suggest that TIPP with Onflex provides results at least similar than those with Polysoft.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many years after the pioneers’ publications on preperitoneal repair of inguinal hernia [1,2,3], minimally invasive open mesh techniques were described, such as Ugahary [4], TREPP [5], Kugel [6], TIPP [7], and ONSTEP [8] procedures.
The two latter techniques both use a minimally invasive inguinal route but are completely different in their concept and design.
In the TIPP (transinguinal preperitoneal) technique, the mesh, totally preperitoneal, is inserted between the peritoneum and the parietalized [9, 10] cord elements through the hernia defect or more often through the internal ring [11], preserving thus the integrity of the transversalis fascia. According to the Laplace’s law, no mesh fixation is usually required.
In the ONSTEP (open new simplified totally extraperitoneal) technique [8], only the medial part of the mesh is placed in the preperitoneal space, introduced in the Retzius space through the transversalis fascia. Its lateral part is inserted between the internal oblique muscle and the external oblique aponeurosis [12], and the cord runs through a split created in the mesh as in the Lichtenstein technique.
Among different meshes or patches designed for TIPP, Surgimesh™, Rebound Shield™ mesh, Polysoft™, all three are completed with a permanent memory ring (not woven polypropylene hemline; not interrupted nitinol memory frame; interrupted polypropylene ring; respectively) facilitating their preperitoneal positioning and deployment. Polysoft patch was the first available on the market [13] and the most widely used, even for the ONSTEP first cases [8].
TIPP with Polysoft was associated with good clinical results, both in observational [10, 14, 15] and randomized (RCT) studies [16,17,18]: Compared with the Lichtenstein technique, fewer patients experienced chronic pain 1 year after a TIPP repair [18] with better SF-36 dimensions [19]. The difference in the incidence of chronic pain at 1Y-Fu was not significant in another RCT [20] possibly in relation with a high percentage (37.4%) of lost to follow-up [21], while in the short term (with a good follow-up), the percentage of pain (VAS > 3) was significantly less in TIPP.
ONSTEP with Polysoft was not found superior to the Lichtenstein technique regarding chronic pain [22]. A large case series of 565 patients [23] showed a recurrence rate of 4.6%, and 30 (5.3%) patients had complaints attributed to the permanent memory ring, especially its lateral part, superficial in the ONSTEP technique. Fifteen of these 30 patients have had the ring removed. To our knowledge, such complications have not been published in TIPP.
With the aim to reduce these complications, a new mesh, Onflex™ (Bard Product, Davol, Warwick, RI, 02886, USA), specifically designed for the ONSTEP technique, reshaped, and completed with an absorbable memory ring was then introduced on the market.
After an overlap period of nearly 1 year, Polysoft was no more distributed on the market.
Some TIPP surgeons quickly adopted the new mesh, while some others were disappointed about the withdrawal of the patch to which they were accustomed and have been waiting for comparative results of these two meshes.
As an RCT was no more possible, we decided to conduct a registry-based comparative study, focusing on the overlap period during which the two meshes were available. As a decrease of chronic pain due to the absorbable ring could be hypothesized, our primary endpoint was the chronic pain at 2-year follow-up; our secondary endpoint was the reoperation rate.
Material and methods
Study design
This is a registry-based study on prospectively collected data. The study period, from September 2016 to October 2017, was the overlap period during which the two studied meshes were available on the market and registered in our registry. All consecutive patients operated on groin hernias using Polysoft or Onflex TIPP were included and followed 2 years. Five surgeons participated in the study. The choice of the mesh was let at the surgeon preference.
Studied meshes
Onflex™ (Bard Product, Davol, Warwick, RI, 02886, USA) is a 192.1 g/m2 before resorption, large pore, 61.0 × 10−4 in.2 monofilament polypropylene mesh with an absorbable (in 6 to 8 months by hydrolysis) memory ring (polydioxanone monofilament).
Polysoft™ (Bard Product, Davol, Warwick, RI, 02886, USA) is a 45 g/m2, small pore 6.9 × 10−4 in.2 monofilament polypropylene mesh with a permanent memory ring.
Onflex™ large is 10.2 cm wide × 15.7 cm long, and medium is 8.6 cm × 14.2 cm.
Polysoft™ large is 9.5 cm × 16 cm, and medium is 7.5 cm × 16 cm.
Collected parameters
The collected parameters, de-identified, were prospectively registered in real time, by the operating surgeon, in closed-ended input boxes in an electronic database including demographics, hernia, and operative characteristics, according to the EHS (European Hernia Society) groin hernia classification [24]; operating time and length of stay according to VAS11 (0–10 visual analogue scale); and postoperative pain, 30-day postoperative outcomes, and complications graded according to the Clavien classification [25].
Clinical controls were performed by the operating surgeon at discharge and at first month clinical visit. In case of any symptom, an additional visit was scheduled between the third and the sixth month after surgery.
Follow-up
The follow-up consisted in a systematic telephone interview scheduled at 2 years postoperatively, based on a validated questionnaire, which we have been using since our first studies in 1999 [26], performed by a dedicated clinical research assistant (CRA), independent from the surgical team.
Postoperative chronic pain, defined as a pain lasting for longer than 3 months [27], was assessed with a four-level VRS (verbal rating scale). The wording of the VRS was in the common language: no pain, mild pain, moderate pain, and severe pain [28]. The impact of pain on daily life was self-assessed by the patient himself, using a patient-related outcome measure (PROM) questionnaire.
Answers were recorded verbatim, without any medical adjustment according to our PROM policy. The CRA was aware of avoiding any response bias. In case of any reported event, the patient was strongly recommended to schedule a clinical visit.
Any reoperation, either in the same hospital or in another team, was looked for and registered in the questionnaire.
Additionally, a retro-control of the registered outcomes was done during the phone interview [29]. In case of discrepancy, the medical chart was reviewed with the operating surgeon. Patients were considered lost to follow-up after five failed attempts to contact them at different moments of different days. Patients who declined to participate in the telephone interview were considered lost to follow-up and were recorded separately as potentially bad results.
Ethics
In this observational study, patients received a non-opposition form informing them that their de-identified data were registered in an electronic database and that they would be offered a phone questionnaire at different steps of their follow-up. Patients’ telephone details were not stored in the database but in the operating surgeon’s office. Only the operating surgeon and the CRA were able to link the randomly allocated identifying number and the patient. The data were stored in a specialized data center where they were protected against network intrusion. The database complies with the requirements of the General Data Protection Regulation (GDPR), the French “Méthodologies de référence de la Commission Nationale Informatique et Liberté” (MR003), and the different specific French ethics committees.
Statistical analysis
Categorical variables were reported as frequencies and percentages. The chi-square test was used for comparative analysis. Continuous variables were reported as mean ± standard deviation (SD), range, or interquartile range (IQR). Comparisons used the Student’s t test.
Results
Flow chart and study period
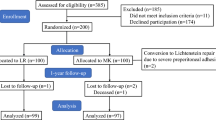
Among 30,488 groin hernia repairs registered in our Club-Hernie registry from September 2011 to June 2020, 4008 consisted in TIPP repairs, using Polysoft in 2106 cases, Onflex in 937 cases, Surgimesh in 935, and other meshes in 30 cases (Fig. 1).
No Rebound Shield was registered in our database, and Surgimesh was withdrawn from the market by the manufacturer a few months before the introduction of Onflex (Fig. 2).
During the study period (overlap period of Onflex and Polysoft), from September 2016 to October 2017, 258 TIPP repairs in 170 patients used an Onflex patch, and 266 TIPP repairs in 190 patients used a Polysoft patch, of whom 156 patients (181 cases) in the studied group and 166 patients (182 cases) in the control group were followed 2 years postoperatively (Fig. 1).
Patients’ characteristics (Table 1)
No significant difference appeared in the two groups of patients except a one-point difference in the mean BMI with a low clinical relevance.
Hernias characteristics (Table 2)
No significant difference was found between the two groups regarding Altemeier classification, emergency repairs, recurrent hernias, and scrotal hernias.
Large hernias (L3 or M3), combined hernias (lateral + medial), and mesh fixation were significantly more frequent in the Polysoft group. Conversely large meshes were significantly used more frequently in the Onflex group, and the operating time (skin to skin) was 10 min longer in this group.
Postoperative course and early outcomes (up to D30)
Postoperative course and early outcomes (up to 30 days) are shown in Table 3.
No statistical difference was found between the two groups regarding the surgical site occurrences (6.2% vs 5.3%), mainly seromas, which healed without needle aspiration, and 3 cases of minimal subcutaneous infected collection, which healed without reoperation.
In the Polysoft group, two other surgical complications occurred: one orchitis without further testicular atrophy and one early recurrence (0.5%), reoperated at D17 with uneventful further outcomes.
Except the later (Clavien IIIb), all postoperative complications were classified as Clavien I/II.
The early postoperative pain, assessed with 0–10 VAS (Table 3), was significantly higher in the Onflex group at D0 (4.34 ± 2.0 [3,4,5,6] vs 2.14 ± 1.8 [1,2,3]; p < 0.0001), at D1 (4.27 ± 2.1 [3,4,5,6] vs 2.19 ± 1.7 [1,2,3]; p < 0.0001), at D8 (1.87 ± 1.6 [1,2,3] vs 0.82 ± 1.5 (0–1); p < 0.0001), and at D30 (0.64 ± 1.2 (0–1) vs 0.04 ± 0.2 (0–0); p < 0.0001). The mean VAS pain, less than 5 at D0 and D1, did not impair an outpatient care in 96% in this group. The mean VAS pain was less than 1 at D30 in both groups.
Two-year follow-up, late outcomes, and PROM telephone questionnaire
Follow-up data are detailed per patients (Table 4) and per operated groins (Tables 5 and 6).
The follow-up consisted in a phone questionnaire done by an independent CRA.
None of the reached patients declined to answer the questionnaire.
Four deaths were reported by the relatives, all four unrelated to the hernia repair.
Respectively 14 vs 24 patients were lost to follow-up including 3 vs 1 unrelated deaths.
No statistical difference was found between the two groups regarding the follow-up rate (92% vs 88%; p = 0.17), while the mean follow-up duration was 1 month longer in the Polysoft group (721 ± 123 (IQR: 695–753) days vs 748 ± 62 (IQR: 732–762) days; p < 0.0001).
One reoperation was reported in the Polysoft group for hernia recurrence, none related to the permanent ring. When taking into consideration the early reoperation for recurrence, the cumulative reoperation rate is 0% in the Onflex group vs 1% in the Polysoft group.
Three recurrences were identified in the Polysoft group and none in the Onflex group.
When taking into account the early recurrence (reoperated at D17, without further re-recurrence), the cumulative recurrence rate in the Polysoft group was 2.2% (4/182) vs 0% in the Onflex group.
Symptomatic patients detected during the PROM questionnaire (Table 5) were offered a clinical visit, especially those 5 patients who reported a bulge or a non-solid groin. Three of them attended the clinical control, only one in three presented with a recurrence, known before, two others did not attend the proposed clinical visit. Both had assessed the result of their surgery as good in the question Q9 (Table 5).
Looking at the VRS (Q3), no statistically significant difference was found between the two groups regarding the overall incidence of symptomatic cases (16.5% vs 17.6%; p = 0.71), while moderate or severe pain were less frequent in the Onflex group than in the Polysoft group (10 cases, 5.5% vs 21 cases, 11.6%; p = 0.01). None of the patients reporting severe pain regularly took analgesics nor was referred in a pain center.
In our questionnaire, the questions Q5, Q6, and Q7 have been designed to put the VRS pain scores in perspective with their impact on patients’ daily life: While an overall pain or discomfort was reported in about 17% of cases, all but three of these symptoms did not interfere with patients’ daily life, and these symptoms were self-assessed as more bothersome than the hernia in only 0.5% of cases.
Among the whole cohort (Onflex + Polysoft), preoperative pain or discomfort were reported (Table 6) in 82% (57 + 235 of 62 + 296) of cases compared with 17% (62 of 62 + 296) of cases at 2 years postoperatively. Significantly more preoperative symptomatic cases were found in the subgroup of symptomatic cases at 2 years (p = 0.021).
Discussion
This registry-based study on prospectively collected data is the first one comparing Onflex vs Polysoft when used in TIPP technique. At 2-year-Fu, the overall rate of pain (including mild pain or discomfort) was similar in both groups (16.5% vs 17.6%; p = 0.71). Moderate or severe pain assessed with VRS were less frequent in the Onflex group than in the Polysoft group (5.5% vs 11.6%; p = 0.05). The identified recurrences and the reoperation (related to the hernia repair) rate were 0% vs 2.2% and 0% vs 1.0%, respectively. No reoperation related to the memory ring was reported.
The main concern with the VRS [28] is the tendency to overestimate pain: Patients who describe a simple discomfort or “a feeling different than before,” not necessarily a pain, are classified as a mild pain. This is an important issue especially in our series in which more than 50% of the VRS pain was classified as mild pain or discomfort. At the opposite side of the VRS pain spectrum, severe pain has not been precisely defined. As an example, in our series, none of the patients reporting severe pain regularly used analgesics nor attended pain centers. VAS (visual analogue scale) evaluation requiring in principle a face to face clinical visit is not applicable in a phone questionnaire setting. The impact of pain on daily activities [30] and the psychological considerations are of major relevance. There is a need for a uniform and validated assessment of chronic postoperative inguinal pain (CPIP). In a recent systematic review [31], 33 different instruments to quantify CPIP were investigated. Some of them are dedicated to the hernia repair such as the Carolina Comfort Scale [32] or the Inguinal Pain Questionnaire; some of them are too sophisticated to be used in daily practice, which suggests to propose simplified versions such as the short form Inguinal Pain Questionnaire SF-IPQ [33] or the SF-36 [19].
The overall pain rate in our series, around 17%, is in line with what has been reported both in randomized studies (overall pain 12% including pain during activity, 8.5% and continuous chronic pain, 3.5%), in the first one [18] (overall pain or discomfort, 25.3% including moderate or severe pain; VDS 3, 4, 5.3%), in a second one [20] using, among other tools, a verbal descriptor scale (VDS), and in a large prospective study using a PROM questionnaire (“significant pain”, 15.2%) based on the national Sweden registry [34]. More precise comparisons are not accurate because the instruments used for the pain assessment are different.
In our registry VRS pains reported by the patients were recorded verbatim without any medical adjustment but amended with additional questions, assessing their impact on daily life, and compared with the preoperative pain scores at baseline.
While an overall pain or discomfort was reported in about 17% (62 in 363) of cases (Table 5), all but three of these symptoms did not interfere with patients’ daily life (Q6), and these symptoms were self-assessed as more bothersome than the hernia in only 0.5% of cases (Q7).
Moreover, the comparison of these figures with the VRS baseline status (Table 6) in which pain or discomfort were reported preoperatively in 82% of cases suggests that VRS probably overestimates pain, that surgeons participating in this study mainly operated symptomatic hernias, and finally, that the hernia repair resulted in a dramatic improvement of the VRS.
The preoperative pain is a well-known risk factor for CPIP [35, 36]. Accordingly, in our study (Table 6), more preoperative symptomatic cases were found in the subgroup of symptomatic cases at 2 years (p = 0.021).
The secondary endpoint of this study was the reoperation rate. One reoperation for recurrence was reported by the patient in the Polysoft group. None is related to the permanent ring. When taking into consideration the early reoperation for recurrence, the reoperation rate is 0% in the Onflex group vs 1% in the Polysoft group.
As they provide valuable additional information concerning postoperative complications, self-reported adverse events questionnaires are recommended as part of routine postoperative assessment [29]. In our registry, a retro-control of the outcomes is systematic during the phone interview done by an independent CRA.
At 2-year follow-up, three recurrences were identified in the Polysoft group, none in the Onflex group. When taking into account the early recurrence (reoperated at D17, without further re-recurrence), the cumulative recurrence rate in the Polysoft group was 2.2% (4/182) vs 0% in the Onflex group. Although not statistically significant (chi-square test non-applicable), this difference in the recurrence rate might be related to a higher number of large meshes (83% vs 47%; p < 0.0001) and a lower number of large and combined hernias (3% vs 20%; p < 0.0001) in the Onflex than in the Polysoft subgroup (Table 2). No registered information indicates whether the participating surgeons chose Polysoft in those large hernias because of being more confident in the classic patch with a non-absorbable ring. The mesh choice, let at the own convenience of the surgeon, is not detailed in our registry.
As shown by Helgstrand et al. [37], the reoperation rate for recurrence may underestimate the overall risk of recurrence by four- to fivefold.
On the other hand, the predictive value of a PROM questionnaire in detecting recurrences has been underlined by Baucom et al. [38] in their hernia registry: “A patient-reported bulge was 85% sensitive, and 81% specific to detect recurrence. Patients reporting no bulge and no pain had 0% chance of recurrence. In multivariable analysis, patients reporting a bulge were 18 times more likely to have a recurrence than those without (95% confidence interval, 3.7 to 90.0; P < .001)”.
A phone questionnaire [39] probably has a better response rate than a postal one [40] and could be highly predictive especially when asking the patient to put his hand to his mouth and blow, exercise described as the PINQ-PHONE [41].
Symptomatic patients detected during our PROM questionnaire (Table 5) were offered a clinical visit, especially those 5 patients who reported a bulge or a feeling of non-solid groin. In the three of them who attended the clinical control, only one presented with a recurrence, known before, and two others did not attend the proposed clinical visit. Both of them had before assessed the result of their surgery as good in the question Q9 (Table 5).
The early postoperative pain, assessed with 0–10 VAS (Table 3), was significantly higher in the Onflex group at D0 (4.34 ± 2.0 [3,4,5,6] vs 2.14 ± 1.8 [1,2,3]; p < 0.0001), at D1 (4.27 ± 2.1 [3,4,5,6] vs 2.19 ± 1.7 [1,2,3]; p < 0.0001), at D8 (1.87 ± 1.6 [1,2,3] vs 0.82 ± 1.5 (0–1); p < 0.0001), and at D30 (0.64 ± 1.2 (0–1) vs 0.04 ± 0.2 (0–0); p < 0.0001). The mean VAS pain, less than 5 at D0 and D1, did not impair an outpatient care in 96% in this group. The mean VAS pain was less than 1 at D30 in both groups. Among the potential explanations, we could underline, as potential confounders, that in the Onflex group, bilateral repairs (25% vs 16%; p = 0.02) and large meshes (83% vs 47%; p < 0.0001) requiring wider dissections, resulting in longer operating time (40.8 ± 15 (20–112) min vs 30.3 ± 8 (15–45) min; p < 0.0001), were significantly more frequent.
Other meshes have been designed for TIPP techniques. With the aim to facilitate the lateral insertion of the mesh and avoid that the extremity of the interrupted memory ring remains unfold and sharp, a mesh equipped with a continuous Nitilol memory ring was created (Rebound Shield™ mesh; Minnesota Medical Development Inc., Plymouth, MN, USA) and studied [11], showing good results at 21.2-month follow-up (recurrences, 2.9%; VAS > 3 chronic pain, 5.0%).
The Onflex patch, specifically designed for the ONSTEP technique, has an interrupted memory ring although some TIPP surgeons would have dreamt of an absorbable but continuous memory ring, therefore equipping another mesh, designed for TIPP, which remains to be created.
With the aim to replace the double-layered polypropylene and reduce the heavy polypropylene load of the Kugel patch, a single layer polypropylene flat mesh (Supromesh; Sayin Tip, Istanbul, Turkey) equipped with 4 arrays of memory recoil rings using a PDS No. 1 was created and randomly compared with the Lichtenstein technique [42] with significantly lower chronic pain score at 2 years.
A flat polypropylene mesh equipped with a continuous not woven polypropylene hemline (Surgimesh™: Aspide Médical, 246, allée Lavoisier, 42350 La Talaudière, France) was withdrawn from the market by the manufacturer in 2016, despite many years of good results [43].
All these meshes are equipped with a memory ring which helps, after a wide enough dissection and cord parietalization, the preperitoneal deployment of the mesh through a minimal invasive inguinal route. In TIPP, a mesh fixation is rarely (as in our series) needed, the mesh being firmly applied by the abdominal pressure to the deep aspect of the inguinal floor as in laparoscopic totally extraperitoneal (TEP) technique. But TIPP technique does not require laparoscopic nor robotic specific devices [44, 45].
This study is not without limitations. This is a non-randomized study, and our two subgroups are not completely similar. But as an RCT was not possible, because Polysoft was no more available on the market, we decided to conduct this registry-based comparative study. Not all the patients attended a clinical visit, but our primary endpoint (chronic pain) and secondary endpoint (reoperation rate) can be assessed by a systematic phone questionnaire.
Conclusion
The results of this study must be interpreted cautiously because the study is not randomized, but they suggest that TIPP with Onflex provides results at least similar than those with Polysoft.
Data availability
De-identified Excel download of the database is available for double check if needed.
References
Stoppa RE, Rives JL, Warlaumont CR, Palot JP, Verhaeghe PJ, Delattre JF (1984) The use of Dacron in the repair of hernias of the groin. Surg Clin North Am 64(2):269–285. https://doi.org/10.1016/s0039-6109(16)43284-6
Read RC, Barone GW, Hauer-Jensen M, Yoder G (1993) Properitoneal prosthetic placement through the groin. The anterior (Mahorner-Goss, Rives-Stoppa) approach. Surg Clin North Am 73(3):545–555. https://doi.org/10.1016/s0039-6109(16)46036-6
Alexandre JH, Bouillot JL, Dupin P, Aouad K, Bethoux JP (2006) Cure of inguinal hernias with large preperitoneal prosthesis: experience of 2,312 cases. J Minim Access Surg 2(3):134–138. https://doi.org/10.4103/0972-9941.27725
Ugahary A, Ugahary F (2010) Technique De Grid-Iron Ugahary®. In: Vidèo-Atlas Chirurgie Herniaire Tome 1. Springer, Paris. Vidèo-Atlas Chirurgie Herniaire Tome 1 Springer, Paris: Springer, Paris; 2010
Lange JF, Lange MM, Voropai DA, van Tilburg MW, Pierie JP, Ploeg RJ et al (2014) Trans rectus sheath extra-peritoneal procedure (TREPP) for inguinal hernia: the first 1,000 patients. World J Surg 38(8):1922–1928. https://doi.org/10.1007/s00268-014-2475-5
Kugel RD (2003) The Kugel repair for groin hernias. Surg Clin North Am 83(5):1119–1139. https://doi.org/10.1016/S0039-6109(03)00123-3
Pelissier EP, Blum D, Marre P, Damas JM (2001) Inguinal hernia: a patch covering only the myopectineal orifice is effective. Hernia. 5(2):84–87. https://doi.org/10.1007/s100290100002
Lourenco A, da Costa RS (2013) The ONSTEP inguinal hernia repair technique: initial clinical experience of 693 patients, in two institutions. Hernia. 17(3):357–364. https://doi.org/10.1007/s10029-013-1057-z
Alexandre JH, Dupin P, Levard H, Billebaud T (1984) Treatment of inguinal hernia with unsplit mersylene prosthesis. Significance of the parietalization of the spermatic cord and the ligation of epigastric vessels. Presse Med 13(3):161–163
Berrevoet F, Maes L, Reyntjens K, Rogiers X, Troisi R, de Hemptinne B (2010) Transinguinal preperitoneal memory ring patch versus Lichtenstein repair for unilateral inguinal hernias. Langenbeck's Arch Surg 395(5):557–562. https://doi.org/10.1007/s00423-009-0544-2
Berrevoet F, Vanlander A, Bontinck J, Troisi RI (2013) Open preperitoneal mesh repair of inguinal hernias using a mesh with nitinol memory frame. Hernia. 17(3):365–371. https://doi.org/10.1007/s10029-013-1110-y
Rosenberg J, Andresen K (2018) Open new simplified totally extraperitoneal (ONSTEP) technique for inguinal hernia repair. In: Campanelli G (ed) The art of hernia surgery. Springer International Publishing AG, pp 301–306. https://doi.org/10.1007/978-3-319-72626-7_30
Pelissier EP, Monek O, Blum D, Ngo P (2007) The Polysoft patch: prospective evaluation of feasibility, postoperative pain and recovery. Hernia. 11(3):229–234. https://doi.org/10.1007/s10029-007-0203-x
Pelissier EP (2006) Inguinal hernia: preperitoneal placement of a memory-ring patch by anterior approach. Preliminary experience. Hernia 10(3):248–252. https://doi.org/10.1007/s10029-006-0079-1
Gillion JF, Chollet JM (2013) Chronic pain and quality of life (QoL) after transinguinal preperitoneal (TIPP) inguinal hernia repair using a totally extraperitoneal, parietalized, Polysoft (R) memory ring patch : a series of 622 hernia repairs in 525 patients. Hernia. 17(6):683–692. https://doi.org/10.1007/s10029-013-1121-8
Sajid MS, Craciunas L, Singh KK, Sains P, Baig MK (2013) Open transinguinal preperitoneal mesh repair of inguinal hernia: a targeted systematic review and meta-analysis of published randomized controlled trials. Gastroenterol Rep (Oxf) 1(2):127–137. https://doi.org/10.1093/gastro/got002
Djokovic A, Delibegovic S (2019) Tipp versus the Lichtenstein and Shouldice techniques in the repair of inguinal hernias - short-term results. Acta Chir Belg:1–7. https://doi.org/10.1080/00015458.2019.1706323
Koning GG, Keus F, Koeslag L, Cheung CL, Avci M, van Laarhoven CJ et al (2012) Randomized clinical trial of chronic pain after the transinguinal preperitoneal technique compared with Lichtenstein’s method for inguinal hernia repair. Br J Surg 99(10):1365–1373. https://doi.org/10.1002/bjs.8862
Koning GG, de Vries J, Borm GF, Koeslag L, Vriens PW, van Laarhoven CJ (2013) Health status one year after TransInguinal PrePeritoneal inguinal hernia repair and Lichtenstein’s method: an analysis alongside a randomized clinical study. Hernia. 17(3):299–306. https://doi.org/10.1007/s10029-012-0963-9
Cadanova D, van Dijk JP, Mollen R (2017) The transinguinal preperitoneal technique (TIPP) in inguinal hernia repair does not cause less chronic pain in relation to the ProGrip technique: a prospective double-blind randomized clinical trial comparing the TIPP technique, using the PolySoft mesh, with the ProGrip self-fixing semi-resorbable mesh. Hernia. 21(1):17–27. https://doi.org/10.1007/s10029-016-1522-6
Pelissier EP, Koning GG, Ngo P (2017) Comment to: The transinguinal preperitoneal technique (TIPP) in inguinal hernia repair does not cause less chronic pain in relation to the ProGrip technique: a prospective double-blind randomized clinical trial comparing the TIPP technique, using the PolySoft mesh, with the ProGrip self-fixing semi-resorbable mesh. D. Cadanova, J. P. van Dijk, R. M. H. G. Mollen. Hernia. https://doi.org/10.1007/s10029-017-1584-0
Andresen K, Burcharth J, Fonnes S, Hupfeld L, Rothman JP, Deigaard S, Winther D, Errebo MB, Therkildsen R, Hauge D, Sørensen FS, Bjerg J, Rosenberg J (2017) Chronic pain after inguinal hernia repair with the ONSTEP versus the Lichtenstein technique, results of a double-blinded multicenter randomized clinical trial. Langenbeck's Arch Surg 402(2):213–218. https://doi.org/10.1007/s00423-016-1532-y
Oberg S, Andresen K, Hauge D, Rosenberg J (2016) Recurrence mechanisms after inguinal hernia repair by the ONSTEP technique: a case series. Hernia. 20(5):681–685. https://doi.org/10.1007/s10029-016-1496-4
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RKJ, Stoppa R, Flament JB (2007) The European Hernia Society groin hernia classification: simple and easy to remember. Hernia. 11(2):113–116. https://doi.org/10.1007/s10029-007-0198-3
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Gillion JF, Fagniez PL (1999) Chronic pain and cutaneous sensory changes after inguinal hernia repair: comparison between open and laparoscopic techniques. Hernia. 3:75–80
Aasvang E, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95(1):69–76. https://doi.org/10.1093/bja/aei019
Loos MJ, Houterman S, Scheltinga MR, Roumen RM (2008) Evaluating postherniorrhaphy groin pain: visual analogue or verbal rating scale? Hernia. 12(2):147–151. https://doi.org/10.1007/s10029-007-0301-9
Franneby U, Sandblom G, Nyren O, Nordin P, Gunnarsson U (2008) Self-reported adverse events after groin hernia repair, a study based on a national register. Value Health 11(5):927–932. https://doi.org/10.1111/j.1524-4733.2008.00330.x
Staal E, Nienhuijs SW, Keemers-Gels ME, Rosman C, Strobbe LJ (2008) The impact of pain on daily activities following open mesh inguinal hernia repair. Hernia. 12(2):153–157. https://doi.org/10.1007/s10029-007-0297-1
Molegraaf M, Lange J, Wijsmuller A (2017) Uniformity of chronic pain assessment after inguinal hernia repair: a critical review of the literature. Eur Surg Res 58(1–2):1–19. https://doi.org/10.1159/000448706
Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, Sing RF, Augenstein VA (2018) Carolinas comfort scale as a measure of hernia repair quality of life: a reappraisal utilizing 3788 international patients. Ann Surg 267(1):171–176. https://doi.org/10.1097/SLA.0000000000002027
Olsson A, Sandblom G, Franneby U, Sonden A, Gunnarsson U, Dahlstrand U (2019) The short-form inguinal pain questionnaire (sf-IPQ): an instrument for rating groin pain after inguinal hernia surgery in daily clinical practice. World J Surg 43(3):806–811. https://doi.org/10.1007/s00268-018-4863-8
Lundstrom KJ, Holmberg H, Montgomery A, Nordin P (2018) Patient-reported rates of chronic pain and recurrence after groin hernia repair. Br J Surg 105(1):106–112. https://doi.org/10.1002/bjs.10652
Tsirline VB, Colavita PD, Belyansky I, Zemlyak AY, Lincourt AE, Heniford BT (2013) Preoperative pain is the strongest predictor of postoperative pain and diminished quality of life after ventral hernia repair. Am Surg 79(8):829–836
Niebuhr H, Wegner F, Hukauf M, Lechner M, Fortelny R, Bittner R et al (2018) What are the influencing factors for chronic pain following TAPP inguinal hernia repair: an analysis of 20,004 patients from the Herniamed Registry. Surg Endosc 32(4):1971–1983. https://doi.org/10.1007/s00464-017-5893-2
Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2012) Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg 256(6):955–958. https://doi.org/10.1097/SLA.0b013e318254f5b9
Baucom RB, Ousley J, Feurer ID, Beveridge GB, Pierce RA, Holzman MD, Sharp KW, Poulose BK (2016) Patient reported outcomes after incisional hernia repair-establishing the ventral hernia recurrence inventory. Am J Surg 212(1):81–88. https://doi.org/10.1016/j.amjsurg.2015.06.007
Tastaldi L, Barros PHF, Krpata DM, Prabhu AS, Rosenblatt S, Petro CC, Alkhatib H, Szutan LA, Silva RA, Olson MA, Stewart TG, Roll S, Rosen MJ, Poulose BK (2019) Hernia recurrence inventory: inguinal hernia recurrence can be accurately assessed using patient-reported outcomes. Hernia 24:127–135. https://doi.org/10.1007/s10029-019-02000-z
Lopez-Cano M, Vilallonga R, Sanchez JL, Hermosilla E, Armengol M (2007) Short postal questionnaire and selective clinical examination combined with repeat mailing and telephone reminders as a method of follow-up in hernia surgery. Hernia. 11(5):397–402. https://doi.org/10.1007/s10029-007-0239-y
Bakker WJ, Roos MM, Kerkman T, Burgmans JPJ (2019) Experience with the PINQ-PHONE telephone questionnaire for detection of recurrences after endoscopic inguinal hernia repair. Hernia. 23(4):685–691. https://doi.org/10.1007/s10029-019-01909-9
Arslan K, Erenoglu B, Turan E, Koksal H, Dogru O (2015) Minimally invasive preperitoneal single-layer mesh repair versus standard Lichtenstein hernia repair for inguinal hernia: a prospective randomized trial. Hernia. 19(3):373–381. https://doi.org/10.1007/s10029-014-1306-9
Soler M (2018) Minimal Open Preperitoneal (MOPP) Technique. In: Campanelli G (ed) The art of hernia surgery. Springer, pp 319–326
Ohmura Y, Suzuki H, Kotani K, Teramoto A (2019) Laparoscopic inguinal hernia repair with a joystick-guided robotic scope holder (Soloassist II(R)): retrospective comparative study with human assistant. Langenbeck's Arch Surg 404(4):495–503. https://doi.org/10.1007/s00423-019-01793-y
Muysoms F, Van Cleven S, Kyle-Leinhase I, Ballecer C, Ramaswamy A (2018) Robotic-assisted laparoscopic groin hernia repair: observational case-control study on the operative time during the learning curve. Surg Endosc 32(12):4850–4859. https://doi.org/10.1007/s00464-018-6236-7
Acknowledgments
The authors want to thank the Club-Hernie members and the dedicated CRA for their highly scientific behavior and involvement in the registry.
Author information
Authors and Affiliations
Consortia
Contributions
The three authors have contributed to the present study and reviewed the present article. Operating surgeons: JMC, JFG, and MS. Study design, data management, and article writing: JFG.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare conflict of interest not directly related to the submitted work: they were given honorarium for TIPP pilot centers (JFG, JMC, MS) and expert honorarium (JFG), but no financial support from industry was provided for this article.
The Hernia-Club is an independent scientific institution whose objective is to assess the results of different techniques and medical devices for hernia repair. It therefore has relationships with many companies having an interest in independent evaluation of their products.
Ethical approval
The patients are informed that their de-identified data are registered and that they will be offered a phone questionnaire at different steps of their follow-up. Only the operating surgeon and the clinical research assistant are able to link the randomly allocated identifying number and the patient. The data are stored in a specialized Swiss data bank where they are protected against network intrusion. The registry complies with the requirements of the General Data Protection Regulation (GDPR), the French “Méthodologies de référence de la Commission Nationale Informatique et Liberté” (MR001, MR003) and the different specific French ethics committees.
Consent for publication
The three authors consent for publication of this article. Patients give their non-opposition (observational study) at the registration in an online database of their de-identified data further used for studies and scientific publications as displayed on the public frontpage of club-hernie.com.
Code availability
Download in Excel shape.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gillion, J.F., Soler, M., Chollet, J.M. et al. A registry-based 2-year follow-up comparative study of two meshes used in transinguinal preperitoneal (TIPP) groin hernia repair. Langenbecks Arch Surg 406, 197–208 (2021). https://doi.org/10.1007/s00423-020-01993-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01993-x