Abstract
Background
Position of the mesh and the method of fixation are important in the occurrence of chronic pain in inguinal herniorrhaphy. An RCT was conducted to evaluate chronic pain after transinguinal preperitoneal (TIPP) repair compared with a Lichtenstein-like repair with a semi-resorbable self-fixing mesh (ProGrip).
Methods
Patients with a primary unilateral inguinal hernia were randomized either to the TIPP (PolySoft mesh) or to repair with a ProGrip mesh. Primary objective was the occurrence of chronic pain after surgery. Secondary objectives were, i.e., recurrences, complications, and quality of life. Follow-up occurred after 2 weeks, 3 months, and 1 year. Patients and physicians were blinded.
Results
Two hundred and fifty-eight patients were randomized to TIPP or ProGrip mesh repair. Two hundred and thirty-eight were included in the analysis: 122 in the TIPP group and 116 in the ProGrip group. Baseline characteristics were compatible. After 2 weeks and 3 months, there was significantly more moderate and severe pain in the ProGrip group on different pain scores. Median pain scores were very low in both groups after 3 months and 1 year (0–0.5 on a scale of 0–10). There was no difference in pain scores between both groups after 1 year. Recurrence rates were low; three patients in each group (2.6 % ProGrip and 2.5 % TIPP).
Conclusion
There was no significant difference in chronic pain between the inguinal repairs with the use of a ProGrip mesh compared with a TIPP repair at 1 year after surgery. In both groups, the occurrence of chronic pain was low.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair is a common surgical procedure performed worldwide. Over 28,000 inguinal hernia operations were performed in the Netherlands annually [1]. Mesh-based repair has been proved to give the lowest recurrence rate [2].
To prevent a recurrence after inguinal hernia surgery, the Lichtenstein technique, performed with the use of prosthesis material, has been established as the standard of care for inguinal hernia repair. Thereafter, the polypropylene mesh has become the first choice prosthesis in most hospitals in the Netherlands. Through this technique, the inguinal hernia recurrence rate has been successfully reduced to 2–5 % [3]. Chronic pain has subsequently been identified as the most important complication after inguinal hernia surgery [3–6]. Several causes can lead to chronic pain. One of them is fixing the mesh with sutures [7–9].
Lightweight prosthesis material has been developed to reduce fibrosis and thus to try to prevent chronic pain. Previous studies have demonstrated that the use of lightweight prosthesis material can possibly lead to a reduction of chronic pain [10, 11].
Previously, both the ProGrip repair and the transinguinal preperitoneal (TIPP) repair with the use of a PolySoft mesh have been proved to cause less chronic pain than the Lichtenstein technique [12, 13]. This is without the high cost and learning curve of the TEP procedure [12, 13]. The ProGrip is a lightweight, self-gripping semi-resorbable polypropylene mesh [14]. The PolySoft mesh is a lightweight polypropylene mesh, tailored in asymmetric oval shape that contains a recoil ring, providing memory of shape to facilitate placement and spreading of the mesh. In this procedure, the patch is placed in the preperitoneal space through the hernial orifice in the transversalis fascia in direct hernias and through the deep inguinal ring in indirect ones [15, 16].
However, a prospective randomized clinical trial comparing the influence of placement of the PolySoft mesh and the ProGrip mesh on chronic groin pain has not yet been performed. Because we hypothesize that a mesh placed in direct contact with the inguinal nerves would lead to more chronic pain, our hypothesis is that the TIPP repair in inguinal herniorrhaphy causes less chronic pain than the repair with the use of the ProGrip mesh. Therefore, our aim was to investigate the extent of long-term pain reduction.
Methods
Prior to the start of the study, the SoftGrip trial has been registered with the Netherlands Trial Register with the following trial ID: NTR1965.
Study design
This trial has been designed as a double-blind randomized clinical trial. Accrual started in November 2009, was completed in November 2011, and the trial finished in November 2012. The TIPP technique using the PolySoft mesh and the herniorrhaphy using the ProGrip mesh were compared. Patients were informed about the trial, when an informed consent was obtained, included by surgeons, surgical residents and junior doctors at the outpatient department of the Ziekenhuis Gelderse Vallei hospital in Ede, the Netherlands. Randomized patients were operated on by two dedicated hernia surgeons, who used the same techniques for both procedures. The study protocol has been approved by the local ethics committee.
Patients
We included America Society of Anesthesiologists (ASA) category I–III, adult patients, with a unilateral primary inguinal hernia after an informed consent was obtained. A large set of data was recorded in the baseline characteristics, such as body mass index, gender, side of hernia, and type of complaints. Exclusion criteria were an incarcerated inguinal hernia, a recurrent inguinal hernia, local inguinal inflammation, ASA 4 or more, previous inguinal or preperitoneal surgery, and the impossibility of an adequate follow-up, i.e., due to psychiatric problems.
Randomization and blinding
Patients were randomized to either ProGrip or the TIPP hernia repair using the PolySoft mesh. Allocation concealment was performed by computer-generated allocation sequence and was stratified by gender, age, BMI, and surgeon. At the outpatient clinic, patients received their randomization numbers by telephone after an informed consent was obtained. In the operation room prior to incision, the type of repair was revealed. The patients remained unaware of the type of technique used. The resident in the outpatient clinic had no access to the surgical reports and thus remained blinded to the type of mesh used.
Anesthesia and analgesia
Spinal or general anesthesia was used. The choice was left up to the recommendation of the anesthetist together with the preference of the patient. No additional inguinal block or local anesthesia was used. Postoperatively, all patients received a prescription for analgesics (paracetamol and diclofenac) to use at home if necessary.
Intervention
The operations were performed by two dedicated surgeons with a large experience for these procedures. In both procedures, the herniorrhaphy was performed through an open anterior approach. Parallel to the groin, an incision of 5 cm was made over the hernia. The hypodermis was diathermically dissected as far as the aponeurosis of the external oblique muscle. This fascia was opened, and the spermatic cord (in men) along with the direct or in-direct inguinal hernia was visualized. After the nerves were identified and spared, either the ProGrip or the TIPP repair was performed. The aponeurosis of the external oblique muscle and Scarpa’s fascia were closed with Vicryl® 3.0. The skin was closed intracutaneously with Monocryl® 4.0.
Inguinal hernia repair with the Parietex ProGrip™ self-fixating semi-resorbable mesh
Herniorrhaphy using the ProGrip mesh is a Lichtenstein-like repair without the need of fixating the mesh with sutures, because the ProGrip mesh is self-fixating. The spermatic cord is dissected and the cremasteric muscle separated (in men). The inguinal ligament is dissected toward the pubis up to the anterior superior iliac spine. A dissection of the conjoint tendon and the rectus muscle aponeurosis is performed as to create the space required to spread out the mesh. The pubic bone is dissected and bared about 2 cm. The direct or oblique external sac is reduced. The self-gripping flap of the ProGrip mesh is opened and closed around the cord outside the operating area to avoid any untimely side-by-side placement. The mesh is then spread down carefully to its final position, and its fixation starting inferiorly to the high right muscle and to the adjacent inguinal ligament. Because of the micro hooks grip, mesh fixation is immediate, no additional fixation suture of the mesh to the pubic bone is required, and thus was not performed [14].
Transinguinal preperitoneal (TIPP) repair with the PolySoft™ preperitoneal mesh
The Polysoft repair was carried out as described by Pélissier [15]. In the case of a lateral hernia, the spermatic cord was mobilised and the cremasteric fibers were separated (in men). The hernia sac was dissected from the cord structures and reduced in the preperitoneal space through the internal ring. A dissection gauze was inserted through the internal ring to create the preperitoneal space. The medial border of the internal ring and the epigastric vessels were lifted with a refractor and blunt digital dissection was carried out in the preperitoneal space in all directions. A pocket was created to allow a complete expansion of the mesh. The PolySoft mesh (16 × 9.5 cm) was introduced with blunt forceps and, after the gauze has been removed, positioned in the preperitoneal space, just like the preperitoneal placement in the TEP procedure. In the case of a medial hernia, the preperitoneal space was reached by incising the transversalis fascia around the base of the sac. Completion of the repair is the same as the lateral hernia procedure.
Data recording and follow-up
In the outpatient clinic, after the informed consent was obtained, baseline characteristics were recorded and patients were asked to fill out the Visual Analog Scale (VAS), the Verbal Descriptor Scale (VDS), and the Leeds Assessment of Neuropathic Symptoms and Signs (LANSS) pain scale questionnaires according pain complaints. The VAS and the Verbal Descriptor Scale (VDS) are validated instruments for evaluation of postoperative pain [17–19]. In the VAS questionnaire, the patients were asked to indicate the amount of pain they were experiencing on a scale of zero to ten. The Verbal Descriptor Scale makes use of seven verbal terms to express the level of pain. This is on a scale of no pain to most intense pain imaginable. The LANSS pain scale is a validated tool for identifying pain experience dominated by neuropathic mechanisms. It is a 7-item pain scale that consists of grouped sensory description and sensory examination with a simple scoring system. The first five questions ask for the presence of unpleasant skin sensations (pricking, tingling, pins, and needles), appearance of the skin (mottled, red, or pink), increased sensitivity of the skin to touch, sudden bursts of electric shock sensations, and hot or burning skin sensations. The last two questions involve sensory testing for the presence of allodynia and altered pinprick threshold. Different numbers of points, relative to their significance to neuropathic pain, are given to positive answers for a maximum of 24 points. A score of <12 makes it unlikely that the patient’s symptoms are neuropathic in nature, whereas a score >12 makes neuropathic mechanisms likely to be contributing to the patient’s pain [20].
Operation and hernia characteristics were added to the database postoperatively. Follow-up, including physical examination, VAS, VDS, and LANSS questionnaires, was scheduled at 14 days, 3 months, and 1 year postoperatively. Patients were blinded to the intervention, and they were investigated by a blinded surgical resident in the outpatient department.
Outcome measures
The primary end point was the number of patients with chronic inguinal pain 1 year after herniorrhaphy. Secondary end points were recurrence, numbness, complications (such as wound infection, hematoma, and seroma), quality of life, resume of work, and the use of analgesics. By the European Hernia Society Guidelines, a recurrence is defined as a swelling (whether or not palpable during Valsalva’s manoeuver) or defect in the groin where an inguinal hernia operation has been carried out [21].
Statistical analysis
The effect of both therapeutic approaches is estimations based on the comparison with comparable procedures, such as Lichtenstein [3–6] and TEP [13, 22, 23]. We estimated that chronic pain after the use of a ProGrip mesh would occur in 25 % of cases, as in the Lichtenstein procedure. The occurrence of chronic pain after TIPP repair with the use of a PolySoft mesh was estimated at 10 %, as in the TEP procedure [13, 22, 23].
Sample size calculation was based on the formula for the difference between two independent proportions with a continuity correction. The two-sided significance level was set to 0.05, the power was set to 80 %, and equal numbers of patients in both groups were assumed. The expected difference in chronic pain was as described: 15 %.
This resulted in a sample size in each group of 112 patients (224 in total). To account for losses to follow up, this number was multiplied by 1.15, resulting in a total sample size of 258 patients (i.e., 129 patients in each group). Sample size calculation was conducted with G * Power (version 3.0.10).
Median scores were used as reference to create binary values for pain scores. Binary outcomes were analyzed with the Chi-square test. Continues variables were analyzed with Student’s T test. Time-dependent variables were analyzed with the use of the Kaplan–Meier method and log-rank test. P values of less than 0.05 were considered as significant. Statistics were performed with the use of Stata version 10.1 (StataCorp, College Station, TX, USA).
Results
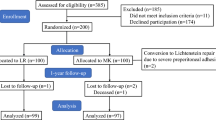
Between November 2009 and November 2011, 258 patients consented to participation into the study and were randomized. 20 patients were excluded from the analyses, because of various reasons: they declined surgery, they did not show up for their first follow-up visit (2 weeks after surgery) or they did not receive the assigned treatment due to logistic reasons. The 238 evaluable patients were distributed equally across the groups: 116 in the ProGrip group vs. 122 in the TIPP group. Follow-up was 99.6 % after 2 weeks, 79.0 % after 3 months and 62.6 % after 1 year (Fig. 1).
Baseline characteristics
Out of the 238 patients, 14 were women (5.9 %). There were no differences between the study groups with respect to gender, age, BMI and surgeon, which confirm an adequate stratification and randomization (Table 1). There were no differences between both groups regarding preoperative distribution of cardiovascular disease, diabetes, COPD, constipation, prostatism, obesity, smoking, heavy labor or medication use. Similarly, there were no differences with regard to the duration, location, frequency, course of complaints, although in the TIPP group more patients characterized their complaints as rarely compared to slightly more daily and weekly complaints in the ProGrip group (P = 0.062).
Perioperative characteristics
Table 2 shows the distribution of perioperative characteristics for the two groups. Again, there were no statistically significant differences between the groups. Most patients had a lateral hernia, and were treated in an ambulatory setting, under general anesthesia with an average operation time (skin to skin) of 30 min.
Recurrences and complications
Recurrence rates were low for both groups (Table 3). There was one early recurrence after 2 weeks, in the TIPP group. After 3 months, there was an additional 1 vs. 1 recurrence for ProGrip and TIPP patients, respectively. After 1 year, a total of 6 recurrences (2.6 and 2.5 %) were seen, 3 in each group; 2 additional in the ProGrip group; and 1 additional in the TIPP group (P = 0.950).
There was no difference in complication rates between the two study groups, as noted by the physician during follow-up (no differences in seromas, hematomas, wound infections, etc.).
However, there was a significant difference in complication rates after 2 weeks and in total as retrieved from the patient’s perspective questionnaires (Table 4). After 2 weeks, 50.4 % of the ProGrip vs. 32.5 % of the TIPP patients reported complications (P = 0.005). Mostly, they complained of postoperative haematomas, hypersensitivity, and scrotal pain, as shown in Table 5. During the total follow-up period, 56.9 % of ProGrip patients vs. 36.1 % of TIPP patients complained to have had a complication at some time-point (P = 0.001).
However, after 1 year, 13.9 % of ProGrip vs. 14.7 % of TIPP patients reported to have had a complication at some time-point after their surgery (P = 0.893). Table 6 shows the distribution of complications observed by the patients at 1 year of follow-up. The most reported complications were hypersensitivity, scrotal pain, and other complaints. In the ProGrip group six patients defined their complaints as other complications. These contained pain during certain movements, swelling without abnormalities on the ultrasound (twice), painful adductor attachment to the pubic bone, swelling with physiological lymph nodes on ultrasound and transient pain in the groin. In the TIPP group, seven patients reported other complications. These were stomach ache, sensation of the mesh (twice), groin pain, piercing pain in the scar, hyposensitivity (twice), and still the same groin pain as before surgery.
Pain outcomes
In general, pain scores were low throughout the entire period of the study, and the median VAS scores were 1.5–3.0 prior to and 2 weeks after surgery. After 3 months and 1 year, median VAS scores were as low as 0–0.5 on a scale. The median VDS score was 2 prior to surgery and also 2 weeks after surgery. This dropped to a median of 0 (no pain) at 3 months and 1 year after surgery (Tables 7, 8, 9, 10, 11). There were no preoperative differences regarding VAS (per category: in rest, daily activity, sports/heavy lifting, and maximum score during last week) or VDS scores between both study groups.
After 2 weeks and 3 months, patients in the ProGrip group reported significantly more moderate (VAS 4–6; VDS moderate) and severe (VAS 7–10; VDS severe, extreme or the most intense pain imaginable) pain compared with the TIPP group (Tables 7–11). In both groups, a significant decrease in pain scores occurred after 2 weeks of follow-up.
Tables 7–11 show the various pain scores after 1 year. Three (4.2 %) patients in the ProGrip group and five (6.7 %) in the TIPP group complained of moderate-to-severe pain in rest (P = 0.504), three ProGrip patients (4.2 %) vs. six (8.0 %) TIPP patients during daily activity, sports or heavy lifting (P = 0.332). In the ProGrip group, five (6.9 %) patients and ten (13.3 %) patients in the TIPP group reported to have experienced moderate or severe pain at some point in the last week (P = 0.201), 1 year after surgery. According to the Verbal Descriptor Scale, four (5.6 vs. 5.3 %) patients in each group experienced moderate or severe pain 1 year after surgery (P = 0.953).
When sorted by the severity of pain at 1 year with the use of the Visual Analog Scale, ten to fourteen (13.9–19.4 %) of the ProGrip patients reported mild pain, two to four (2.8–5.6 %) patients reported moderate pain, and no patient reported severe pain. In the TIPP group, 8 to 13 (10.7–17.3 %) patients complained of mild pain, 3 to 6 (4.0–8 %) of moderate pain, and nil to three (0.0–4.0 %) of severe pain at some point 1 year after the herniorrhaphy. The Verbal Descriptor Scale reports 15 (20.8 vs. 20.0 %) patients in each group with mild pain, four (5.6 %) patients in the ProGrip group, and three (4.0 %) patients in the TIPP group with moderate pain and one (1.3 %) patient in the TIPP group with severe pain. There were no statistical differences between the two groups (Tables 12, 13, 14, 15, 16).
In the Leeds Assessment of Neuropathic Symptoms an Signs (LANSS) score, already a preoperative difference was seen between the ProGrip (23.5 %) and the TIPP (12.3 %) group (P = 0.024) (Table 17). This was mostly due to allodynia in the painful area after superficial rubbing. This statistical difference persisted between the two groups after 2 weeks and 3 months, but disappeared after 1 year of follow-up. In general, an increase in LANSS scores was seen in both groups 2 weeks after surgery, although the significant difference between the two mesh types remained present. Most neuropathic complaints were due to a burning sensation and numbness. After 3 months, the scores dropped below the baseline values in both groups. The persisting complaints were mostly due to allodynia, hyperesthesia and numbness.
After 1 year, eleven (15.5 %) of the ProGrip and eight (10.5 %) of the TIPP patients reported neuropathic complaints according to the LANSS scores, this difference was statistically non-significant (P = 0.370) (Table 17).
Discussion
This prospective randomized double-blind clinical trial was designed to investigate the difference in occurrence of chronic pain after inguinal hernia repair between the TIPP technique with the use of a PolySoft mesh and a Lichtenstein like repair with the use of a ProGrip semi-resorbable self-fixing mesh.
After 1 year, 62.6 % of the patients could be examined and thus 37.4 % were lost to follow up. A few patients had deceased due to non-procedure-related reasons (very high age, cardial dysfunction, vascular problems or carcinomas), one patient was excluded due to a mental disorder, but most of the patients just did not appear at their appointment of 1 year after surgery.
Patients of both groups reported similarly low rates of chronic pain, with moderate pain scores between 1.3 and 8.0 % and severe pain scores between 0.0 and 4.0 %, 1 year after surgery. The ProGrip patients did report significantly more pain compared to TIPP patients at 2 weeks and 3 months of follow-up. After 2 weeks, a large proportion of patients (n = 50) did not report on their VAS with respect to heavy lifting and/or sports, because they had not yet performed such activities by that time due to the fact that they thought they were not yet allowed to do so.
However, there were no statistically significant differences between both groups in the long-term outcomes. The Leeds Assessment of Neuropathic Symptoms and Signs (LANSS) scale allows to differentiate between neuropathic and other of complaints [20]. Surprisingly, ProGrip patients reported to have significantly more neuropathic complaints prior to surgery compared with TIPP patients. Although the occurrence of neuropathic complaints increased in the short term (2 weeks), after 3 months, a decrease was seen, not only compared to the increased LANSS results after 2 weeks, but the scores even dropped below the baseline values in both groups, although only slightly for the Progrip patients. After 1 year of follow-up, no significant differences were established. Eleven (15.5 %) of the ProGrip patients and eight (10.5 %) of the TIPP patients persisted to report some neuropathic complaints. Mostly, this was due to numbness around the surgical scar and not any pain.
Although we did not observe any significant differences in chronic and/or severe pain between the two study groups, the current study might have been underpowered to demonstrate this, since the incidence of chronic and/or severe pain was very low in both groups.
ProGrip patients reported to have had more complications compared with TIPP patients (56.9 vs. 36.1 %; P = 0.001). This was mostly after 2 weeks (50.4 vs. 32.5 %; P = 0.005) and consisted of hypersensivity, postoperative haematomas and scrotal pain. Only a very few patients developed other complaints during follow-up beyond 2 weeks. The short-term statistically significant difference, as encountered by the patients at 2 weeks, disappeared 1 year after surgery (ProGrip 13.9 % vs. TIPP 14.7 %; P = 0.893).
Objectively, the physician did not concur with these questionnaires, since no differences in seromas, haematomas, swelling, wound infections, and recurrences were seen during follow-up. We assume, therefore, that the use of a ProGrip mesh for inguinal hernia repair is associated with significantly more short-term complaints compared with the TIPP repair.
Recurrence rates were acceptably low during long-term follow-up of the trial. In each group, three patients developed a recurrence (ProGrip 2.6 % vs. TIPP 2.5 %; P = 0.950). All recurrences were identified during physical examination by the physician in the outpatient clinic and in some cases confirmed with an ultrasound. Only one of these three ProGrip patients with a recurrence has been reoperated and turned out to have a medial recurrence. One patient passed away due to a non-procedure-related death (OHCA), and the other patient did not wish to undergo a reoperation due to the fact that there were no complaints of pain, no inconvenience or other complaints and high age. All three TIPP patients with a recurrence were reoperated, and all had a medial recurrence. Furthermore, one female patient in the ProGrip group developed a femoral hernia after 1 year.
Studies have shown that approximately 30 % of patients still experience some sort of pain 1 year after Lichtenstein inguinal hernia repair, 12 % of patients experience mild-to-severe chronic groin pain and for approximately 17 % of patients this limits their daily functioning [3–6]. A number of different causes can lead to the occurrence of chronic pain, i.e., curling up of the mesh (meshoma), a suture in the periost of the pubic bone, or the compression, incarceration or damage of one of the following nerves: the n. ilio-hypogastricus, n. ilio-inguinalis or the n. genito-femoralis [7–9]. From a pathophysiologic point of view, the incarceration and damage of inguinal nerves play a large role. Both are caused by extensive fibrosis and/or the fixation (with sutures) of the implanted prosthesis. The same mesh-induced tissue reaction could possibly also lead to the nociceptive (=non-nerve related) pain, which is characterized by a diffusely painful spermatic cord [9].
Very recently, Bendavid et al. analyzed 17 meshes that were removed for pain and 14 for recurrence (and two for both pain and recurrence). They found with S100b staining that significantly more density in nerve tissue was found in the pain cases compared to the recurrent ones (P < 0.001). They hypothesize that this is not only due to the larges nerves, but might also be especially caused by regeneration of small branches.
Since these causes of chronic pain could theoretically be avoided, alternative fixation techniques, such as the ProGrip self-gripping semi-resorbable mesh, have been developed. Studies have demonstrated that besides an adequate inguinal hernia repair, there was also a significant reduction in pain [12, 14]. Our study shows similar outcomes of chronic pain. One year after the inguinal hernia repair, in the ProGrip group, only two patients reported moderate pain in rest and daily activities (2.8 %) and none suffered from severe pain. Three patients complained of moderate pain (4.2 %) and none of severe pain, during sports or heavy lifting. When asked about the most pain during some point in the last week, four patients reported to have experienced moderate (5.6 %) pain and none severe pain. The clinical relevance of this last question is debatable in this case, since it is somewhat contradicted by the answers to the other questions with respect to rest, daily activities, sports, and heavy lifting. However, it might be the only question to pinpoint a difference in chronic pain. Judging by the Verbal Descriptor Scale, four patients reported moderate pain (5.6 %), and none reported severe, extreme or most intense pain imaginable.
A large mesh placed in the preperitoneal space with a sufficient medial overlap can close the whole triangle of Fruchaud from the inside. Theoretically, this seems to be the best treatment for groin hernia. The force that causes the abdominal wall to herniate, can, therefore, keep the mesh in place due to Pascal’s law.
With this in mind, the laparoscopic repair of inguinal hernia has been developed. The most common laparoscopic techniques for groin hernia repair are transabdominal preperitoneal repair (TAPP) and totally extra peritoneal repair (TEP). The TAPP technique requires entering the peritoneal cavity and placing the mesh over possible hernia sites through a peritoneal incision. The TEP procedure does not enter the peritoneal cavity. The mesh is used to seal the hernia from the outside of the peritoneum. Both procedures require the use of general anesthesia and, although rarely, they can be associated with severe complications [24].
Studies have demonstrated no significant difference with regard to recurrence rates between open or laparoscopic hernia surgeries. Laparoscopic surgery did show less persisting pain than with the open surgery. There was an average occurrence of chronic pain after a TEP of less than 10 % [25–30]. However, operation times are longer, there is a longer learning curve, and the costs are higher for this procedure [25].
The transinguinal preperitoneal (TIPP) technique has been developed, using the PolySoft mesh, to associate the advantages of the placement of the patch in the preperitoneal space and simplicity of the inguinal incision. The occurrence rate of chronic groin pain after this surgery appears to be similar to the TEP procedure. Recent studies have reported an occurrence of chronic pain in less than 10 % [13, 22, 23]. Our study presents similar outcomes on chronic pain after inguinal hernia TIPP repair with the use of a PolySoft mesh. After 1 year, only three patients (4.0 %) still experienced moderate, and none had severe pain in rest. During daily activities, one patient complained of moderate and one of severe pain (1.3 %). During sports or heavy lifting, three patients reported moderate (4.0 %) and one severe (1.3 %) pain. When asked about the most pain during some point in the last week, six patients reported to have experienced moderate (8.0 %) pain and three severe (4.0 %) pain. Again, whether the scores of this last question are clinically relevant is debatable. The Verbal Descriptor Scale demonstrates that three patients complained of moderate (4.0 %) and one of severe (1.3 %) pain (Tables 12–16).
Our study hypothesis that the TIPP repair would cause less chronic pain in relation to the ProGrip repair was rejected as the results did not show any significant difference in chronic pain between the two techniques. The Lichtenstein technique is widely still considered to be the golden standard in inguinal hernia repair. As compared to the occurrence of chronic pain after the Lichtenstein repair described by the literature [3–6], both techniques do appear to be superior, with very low median pain scores of 0–0.5 on a scale of 0–10, and therefore should be considered as good alternatives for this standard technique. Although no significant differences could be identified between the two techniques, the ProGrip repair seems to cause even less chronic pain than the TIPP repair, and it is easier to learn for residents. This allows us to conclude that a herniorrhaphy with the use of a ProGrip mesh may be the best choice in the daily practice of inguinal hernia repair or in teaching hospitals with regard to reduction of chronic pain after surgery. However, the ProGrip mesh will not prevent a femoral hernia in contrast to the TIPP technique. Therefore, TIPP is more useful in female patients. The use of a PolySoft mesh also causes significantly less neuropathic complaints after 2 weeks and 3 months. It is feasible that the difference of dissection may contribute to this. Nevertheless, this statistical difference disappears after 1 year.
In conclusion, this prospective randomized controlled study showed no statistical differences in chronic pain at 1 year after surgery between the TIPP (PolySoft) and the ProGrip technique.
References
Statline. http://statline.cbs.nl/StatWeb/publication/?VW=T&DM=SLNL&PA=80386NED&LA=NL. Centraal Bureau voor de Statistiek
Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM (2002) Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev 4:CD002197
EU Hernia Trialists Collaboration (2002) Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg 235:322–332
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
Courtney CA, Duffy K, Serpell MG, O’Dwyer PJ (2002) Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg 89:1310–1314
Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88:1122–1126
Amid PK (2004) Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia 8:343–349
Amid PK (2004) Radiologic images of meshoma: a new phenomenon causing chronic pain after prosthetic repair of abdominal wall hernias. Arch Surg 139:1297–1298
Loos MJ, Roumen RM, Scheltinga MR (2007) Classifying post-herniorrhaphy pain syndromes following elective inguinal hernia repair. World J Surg 31:1760–1765 (discussion 1766–1767)
O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G (2005) Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg 92:166–170
Post S, Weiss B, Willer M, Neufang T, Lorenz D (2004) Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg 91:44–48
Kingsnorth A, Gingell-Littlejohn M, Nienhuijs S, Schule S, Appel P, Ziprin P et al (2012) Randomized controlled multicenter international clinical trial of self-gripping Parietex ProGrip polyester mesh versus lightweight polypropylene mesh in open inguinal hernia repair: interim results at 3 months. Hernia 16:287–294
Koning GG, Keus F, Koeslag L, Cheung CL, Avci M, van Laarhoven CJ et al (2012) Randomized clinical trial of chronic pain after the transinguinal preperitoneal technique compared with Lichtenstein’s method for inguinal hernia repair. Br J Surg 99:1365–1373
Chastan P (2006) Tension free open inguinal hernia repair using an innovative self gripping semi-resorbable mesh. J Minim Access Surg 2:139–143
Pelissier EP (2006) Inguinal hernia: preperitoneal placement of a memory-ring patch by anterior approach. Preliminary experience. Hernia 10:248–252
Pelissier EP, Monek O, Blum D, Ngo P (2007) The Polysoft patch: prospective evaluation of feasibility, postoperative pain and recovery. Hernia 11:229–234
McCarthy M Jr, Chang CH, Pickard AS, Giobbie-Hurder A, Price DD, Jonasson O et al (2005) Visual analog scales for assessing surgical pain. J Am Coll Surg 201:245–252
Herr KA, Spratt K, Mobily PR, Richardson G (2004) Pain intensity assessment in older adults: use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clin J Pain 20:207–219
Loos MJ, Houterman S, Scheltinga MR, Roumen RM (2008) Evaluating postherniorrhaphy groin pain: visual analogue or verbal rating scale? Hernia 12:147–151
Bennett M (2001) The LANSS Pain Scale: the Leeds assessment of neuropathic symptoms and signs. Pain 92:147–157
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Berrevoet F, Sommeling C, De Gendt S, Breusegem C, de Hemptinne B (2009) The preperitoneal memory-ring patch for inguinal hernia: a prospective multicentric feasibility study. Hernia 13:243–249
Pelissier EP, Blum D, Ngo P, Monek O (2008) Transinguinal preperitoneal repair with the Polysoft patch: prospective evaluation of recurrence and chronic pain. Hernia 12:51–56
McCormack K, Wake BL, Fraser C, Vale L, Perez J, Grant A (2005) Transabdominal pre-peritoneal (TAPP) versus totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair: a systematic review. Hernia 9:109–114
McCormack K, Scott NW, Go PM, Ross S, Grant AM (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev CD001785
Hallen M, Bergenfelz A, Westerdahl J (2008) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: long-term follow-up of a randomized controlled trial. Surgery 143:313–317
Kumar S, Wilson RG, Nixon SJ, Macintyre IM (2002) Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg 89:1476–1479
Lau H, Patil NG, Yuen WK, Lee F (2003) Prevalence and severity of chronic groin pain after endoscopic totally extraperitoneal inguinal hernioplasty. Surg Endosc 17:1620–1623
Sayad P, Hallak A, Ferzli G (1998) Laparoscopic herniorrhaphy: review of complications and recurrence. J Laparoendosc Adv Surg Tech A 8:3–10
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:188–199
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
DC declares no conflict of interest. JPvD declares no conflict of interest. RMHGM declares no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Čadanová, D., van Dijk, J.P. & Mollen, R.M.H.G. The transinguinal preperitoneal technique (TIPP) in inguinal hernia repair does not cause less chronic pain in relation to the ProGrip technique: a prospective double-blind randomized clinical trial comparing the TIPP technique, using the PolySoft mesh, with the ProGrip self-fixing semi-resorbable mesh. Hernia 21, 17–27 (2017). https://doi.org/10.1007/s10029-016-1522-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1522-6