Abstract
Purpose
Inguinal hernia repairs should have few complications and a short learning curve. A new operation called Onstep has promising results, but still some recurrences. The aim of the study was to find reasons for recurrence, by studying the re-operations.
Methods
The study is a case series, where 565 patients operated with Onstep at six hospitals between December 2011 and April 2015 were identified. If a recurrence had occurred, the description of the re-operation was studied and compared to the primary Onstep operation.
Results
We found 26 inguinal hernia recurrences, giving a recurrence rate of 4.6 %. The reasons for recurrence were a cranial displacement of the mesh in five patients, a caudal displacement in three patients, a folded mesh in one patient, and broken sutures in the mesh laterally in six patients. We found indications of a learning curve, since 70 % of the recurrences had their primary operation among the first half of the total Onstep procedures. Another finding was that 30 patients had complaints from the ring in the mesh, and most of these patients were slender. Fifteen patients have had the ring removed, and for six patients with a follow-up, the complaints have been reduced or disappeared.
Conclusions
The main reasons for recurrence may be broken sutures in the mesh laterally or a suboptimal size of the opening in fascia transversalis medially, enabling the mesh to displace. Furthermore, the results suggest a learning curve. These findings may guide further improvement in the Onstep method for inguinal hernia repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair should have few complications, a short learning curve, and few recurrences [1]. Since 2005, some surgeons have been practicing a new operation called Onstep, but only two studies reported in English have investigated the results of the technique [2, 3]. The operative technique has been described in detail previously [2], and the results have been promising with few recurrences and chronic pain ranging from zero to a few per cent [2, 3]. Although promising, recurrences after Onstep have now occurred in Danish and Swedish departments.
The purpose of this study was to investigate recurrences after Onstep operation for inguinal hernias, and thus suggest methods to improve the technique.
Methods
This is a case series where we identified all patients operated with the Onstep technique at five Danish and one Swedish surgical department. The first registered operation was in December 2011, but start date varied between the hospitals. The last date gathering data also varied between the hospitals, ranging from August 2014 until April 2015. The medical files of all patients were studied, and primary operation date, age at the time of primary repair, and sex were recorded. For the patients with an inguinal hernia recurrence, we recorded details of the primary operation as well as the re-operation, and body mass index (BMI). The size of the primary hernia was classified according to the European Hernia Society classification [4]. Recurrence was defined as the occurrence of any inguinal hernia in the same side as the primary hernia, following the initial repair.
It came to our knowledge that a small part of the patients, especially slender ones, developed pain from the ring in the mesh. We recorded BMI and follow-up consultations for these patients.
The study was approved by the Danish Data Protection Agency (Journal number 03142, ID: HEH-2014-084). The study did not need ethical approval according to the Danish law.
Results
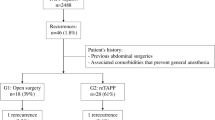
We identified a total of 565 male patients with 569 inguinal hernias who received the Onstep repair from the six departments. The recurrence rate was 4.6 % (26/569). Each department conducted median 107 (range 22–155) procedures in the study period. The department with the highest number of procedures had the lowest recurrence rate (3.2 %) and the department that conducted the fewest operations had the highest rate (9.1 %), p = 0.187. Age was similar in the recurrence group compared to all Onstep operations, with a median age among recurrences of 64 years (range 22–84) compared with 60 years in total (range 17–94) (p value = 0.133, Mann–Whitney U test). The median BMI among patients with recurrences was 26.2 kg/m2 (range 18–34). Regarding the size of the primary hernias, three patients had a size 1 hernia, three size 2, and four size 3, according to the EHS classification based on the size of the hernia orifice [4]. Seven hernias were between 2 and 5 cm in diameter, and another six hernias were described as quite large to very large, but without a description of the hernia orifice. Of the hernia types that were described in the surgical records (92 %), 67 % were medial, 25 % lateral, and 8 % pantaloons.
A total of 21 patients had received a re-operation for their recurrence. The location of the mesh was described in 15 of the 21 re-operations. The types of re-operations were 16 laparoscopic operations (14 TAPP and 2 TEP), 2 Lichtenstein, 2 modified open operations, and 1 re-Onstep operation. The Onstep mesh (Polysoft® mesh) is medially placed through an opening in fascia transversalis and laterally, it is sutured around the spermatic cord. The observed reasons for recurrences during the re-operations were a displaced mesh cranially to the hernia and pecten ossis pubis in six patients (in one of which the mesh also was displaced medially), caudally to the hernia in four patients (in one of which the patient also had a laterally displaced mesh), and laterally to the hernia in two patients. For two other patients, the sutures around the spermatic cord were broken, where one of them had Vicryl® (absorbable) sutures resulting in a recurrence through the open mesh laterally without displacement of the mesh, and the other had a medially displaced mesh. For the last patient, the mesh was extremely folded, and the mesh lay laterally to the hernia. The size of mesh, either medium or large, was not available for all patients and has, therefore, not been analysed.
Seven of the 26 patients with a recurrence either suspected a recurrence few days postoperatively, or had it confirmed by clinical examinations. Four of them developed a recurrence on the same day as the primary Onstep operation, and the three remaining developed a recurrence 1–3 days postoperatively. At the time of data collection, six patients had been re-operated. The reasons for early recurrence for the six patients were broken sutures in the mesh laterally without displacement of the mesh (n = 1), broken sutures with lateral and caudal/lateral displacement of the mesh (n = 2), and displacement of the mesh cranially to the hernia (n = 3).
In 81 % (17/21) of the re-operated patients, both the primary and recurrent hernias were described. Two patients had a different type of hernia at recurrence (medial and lateral primary hernias recurred as lateral and medial hernias), and one patient with a giant primary pantaloon hernia had a lateral recurrence. For the remaining patients, the primary and recurrent hernias were the same (lateral to lateral n = 3 and medial to medial n = 11).
Median time from primary operation until diagnosis of a recurrence was 2.2 months (range 0–17.1), and 18 of the recurrences (70 %) had their primary Onstep operation in the first half of the operation range (Fig. 1).
A total of 5.3 % (n = 30) of the patients operated with Onstep had complaints from the ring in the Polysoft® mesh. These patients were generally slim with a median BMI of 23.1 kg/m2 (range 19.3–29.4). For the majority (87 %), the surgeon could palpate the ring through the skin. Of the 30 patients, 10 could feel the ring through the skin without any pain. Thirteen patients had complaints, especially from the lateral part of the mesh (just medial to anterior superior iliac spine); either they could feel a lump, had pain, or the skin was sore when wearing trousers. Until now, 15 patients have had the ring removed by an incision near the lateral part of the mesh and there after extraction of the ring, leaving the mesh in place. For three of the patients, it was necessary also to remove the most lateral part of the mesh. Six patients had a follow-up visit a couple of months postoperatively, and the results have been satisfying with less or no complaints, and no recurrence of the hernia.
Discussion
In our study, 4.6 % of the patients with a primary Onstep operation developed a recurrence. The type of primary hernia that recurred was mostly medial. Available details from operations for a recurrence revealed that three possible mechanisms could explain the reason for recurrence: (1) displacement of the mesh cranially or caudally in the opening in the transversalis fascia, (2) break of the sutures in the mesh with the subsequent lateral or medial displacement of the mesh, and (3) break of the sutures without the displacement of the mesh, but recurrence through the slit in the mesh laterally. The majority of the patients with a recurrence had their primary operation in the first part of the operation range. Apart from these results, a number of patients had complaints from the stiff ring in the mesh at its lateral position. Some of these had the ring surgically removed with subsequent symptom relief.
Three factors help keep the mesh in place; the ring in the mesh, the opening in fascia transversalis medially, and the sutures in the mesh around the spermatic cord laterally. Explanations to the mechanism of a recurrence could be found in the last two factors. The mesh is placed through the opening in fascia transversalis, which allows the medial part to be placed preperitoneally and the lateral part of the mesh to be placed in the inguinal canal between the fascias of the internal and external oblique [2]. Since the mesh is not fixated with sutures to the surrounding tissue, the opening in the fascia transversalis is thought to be important in securing the mesh in the caudal–cranial direction and an opening too big will allow the mesh to displace. The opening could also have been too narrow, leading to a folded mesh, which in turn may have led to a suboptimal placement of the mesh preperitoneally. The mesh should lay flat in the preperitoneal area medially, allowing the surrounding tissue to adhere to the mesh over time. If that is not the case, it could result in a displaced mesh because of poor tissue ingrowth in the mesh.
Another possible explanation to a displaced mesh could be that the sutures around the spermatic cord had either been absorbed too early (if using absorbable sutures) or broken, which also was described specifically for two patients. Apart from this, the mesh was displaced laterally to the hernia for three patients, and for two patients, the mesh was displaced cranially/medially and caudally/laterally. This must be the result of broken sutures in the mesh, since it otherwise cannot slide laterally/medially. If this happens, the mesh covers the hernia orifice insufficiently laterally, and medially it can slide in all directions. Of the 15 recurrences where the placement of the mesh in relation to the hernia was described, at least 6 recurrences must be a result of broken or absorbed sutures in the mesh. The type of suture used in the mesh was only described/registered for one patient, so it is unknown if the sutures were absorbed too early or broke postoperatively. When securing the mesh around the spermatic cord, permanent sutures would give greater strength [5], and the knotting technique could be optimized using square knots (instead of sliding knots) [6, 7].
Our results pointed at a learning effect with more recurrences occurring in the first half of the operations than in the second half. Some of the earliest recurrences could be due to technical failure. Onstep is still a quite new operation, and the same tendency has been seen in the previous studies with TAPP, where a decreasing recurrence rate was demonstrated for pioneers for the first 200 patients [8]. When they compared the results with young doctors 11 years later, they could not find a learning curve, but by this time, the technique had been standardized. However, our results do not allow for a firm conclusion towards a minimum number of repairs for surgeons to be proficient in the Onstep technique.
The primary hernia size was described for 23 of the recurrent hernias and 10 were either described as large or was classified to be size 3 according to the EHS classification [4]. A meta-analysis has shown that the hernia size does not seem to influence the risk of developing a recurrence [9]. Nevertheless, this might not be true for the Onstep technique, since the mesh is not secured to the surrounding tissue. Regarding the hernia type, two recurrent hernias were of another type than the primary (which were medial and lateral), and were presumably overseen hernias at the primary operation. Our finding is not a specific limitation for Onstep, since surgeons always should look for both medial and lateral hernias at every hernia operation. One study has shown that the odds ratio to find the same type of hernia both at primary and re-operation was 7.1 for medial hernias and 3.0 for lateral hernias [10].
Our recurrence rate of 4.6 % can be compared with other studies. A study based on the Danish Hernia Database found a re-operation rate of about 3.5 % for Lichtenstein and 6 % for laparoscopic repairs after 96 months follow-up [11]. However, since many patients will not seek a surgeon with their recurrence, the true recurrence rate is higher. A Swedish study showed that re-operations for a recurrence only included 72 % of the total recurrences [12]. Thus, our finding of 4–5 % recurrence rate is not alarming, and with the learning curve effect, it should be possible to minimize the recurrence rate even further if proper training is secured [13]. The pioneers of the Onstep technique reported a recurrence rate of 0.6 % [2], which is far lower than the result in this study. This may be explained by a learning curve effect, since the two surgeons that performed the 693 Onstep operations were very experienced before they started the Onstep technique, and then practiced the technique for 693 cases, which is far more than the individual surgeons performed in this study.
The TIPP (transinguinal preperitoneal) technique is another open procedure using the Polysoft mesh for a preperitoneal repair. In the TIPP repair, the entire mesh is placed preperitoneally, either through the internal orifice for lateral hernias or through a medial hernia defect, and it might be necessary to secure the mesh with one suture to the surrounding tissue [14, 15]. A case series on the TIPP procedure showed a recurrence rate of 0.2 %, but a rate of moderate/severe chronic pain of 15 % [14]. Like the pioneers of Onstep, two senior surgeons performed several hundred TIPP procedures, which may explain the low recurrence rate. However, even though the rate of chronic pain was much lower in the Onstep study (<1 %) [2], it is difficult to compare the results, since the authors have used different evaluation tools [2, 14]. A randomized trial compared TIPP with Lichtenstein and found no difference in the recurrence rate, but a significantly lower rate of chronic pain for the TIPP procedure [16]. For Onstep, there are two ongoing randomized trials [17, 18] that compare Lichtenstein with Onstep and laparoscopy (TAPP) with Onstep, regarding chronic pain, sexual dysfunction, and recurrence rates.
Thirty patients in our study had postoperative complaints from the ring in the mesh. They could feel the ring through the skin, and for 20 patients, the skin was irritated/painful superficial to the mesh, or specifically in the lateral part. The lateral part of the ring is only covered by skin, subcutaneous fat, and the fascia of the external oblique. Most of these patients were slender, and they were, therefore, at risk of having a prominent ring, which may result in sore skin (especially when wearing trousers). Until now, 15 patients have had the ring removed. For those patients who have had a follow-up, the complaints have disappeared or been reduced, without a recurrence of the hernia. Pioneers of the Onstep operation have shown similar results, where three patients with post-operative pain had their ring removed, resulting in the disappearance of the pain [2]. Surgeons should ensure that the lateral margins of the mesh do not lie on top of each other, and the mesh should lay as flat as possible in its lateral part.
The strengths with our study were that the operations were described the same day, and we can expect little if any recall bias. Limitations were that the re-operation records did not describe the mesh location for all patients and the follow-up time was varying. For patients operated in the second half of the period, there may not have been enough time to detect a recurrence in all patients. Even so, there was enough time to find a recurrence for the majority of the patients, since median time from primary Onstep operation until the diagnosis of a recurrence was only 2.2 months (range 0–17.1).
Surgeons should carefully make sure that the mesh lies flat and covers the hernia sufficiently, the opening in fascia transversalis should neither be too small nor be too large, and when closing the mesh around the spermatic cord, only permanent sutures should be used with a meticulous knotting technique. For specific recommendations, see Table 1. When examining recurrence rate for a new operation, the technique need to have time to become optimized/standardized—which has been done for both Lichtenstein and laparoscopy—before the true recurrence rate can be found. Thus, with the Lichtenstein technique, it became evident that the medial mesh overlap should be sufficient [19, 20], and in laparoscopic repair mesh sizes increased over time, where the mesh has to be at least 10 × 15 cm to minimize recurrences [21–25]. These findings were not available at the initial introduction of the techniques but became evident after some time. With the Onstep technique, we expect a similar pattern that the surgical technique can be optimized after an implementation period with the subsequent lowering of recurrence rates.
In conclusion, we have identified several likely reasons for recurrence. They were mainly broken sutures in the mesh and suboptimal size of the opening in fascia transversalis. The results also indicated a learning curve.
References
Kingsnorth A (2004) Treating inguinal hernias. BMJ 328:59–60
Lourenco A, da Costa RS (2013) The ONSTEP inguinal hernia repair technique: initial clinical experience of 693 patients, in two institutions. Hernia 17:357–364. doi:10.1007/s10029-013-1057-z
Andresen K, Burcharth J, Rosenberg J (2015) The initial experience of introducing the Onstep technique for inguinal hernia repair in a general surgical department. Scand J Surg 104:61–65. doi:10.1177/1457496914529930
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH et al (2007) The European Hernia Society groin hernia classification: simple and easy to remember. Hernia 11:113–116
Brown RP (1992) Knotting technique and suture materials. Br J Surg 79:399–400
Brouwers JE, Oosting H, de Haas D, Klopper PJ (1991) Dynamic loading of surgical knots. Surg Gynecol Obstet 173:443–448
van Rijssel EJ, Trimbos JB, Booster MH (1990) Mechanical performance of square knots and sliding knots in surgery: comparative study. Am J Obstet Gynecol 162:93–97
Bokeler U, Schwarz J, Bittner R, Zacheja S, Smaxwil C (2013) Teaching and training in laparoscopic inguinal hernia repair (TAPP): impact of the learning curve on patient outcome. Surg Endosc 27:2886–2893. doi:10.1007/s00464-013-2849-z
Burcharth J, Pommergaard HC, Bisgaard T, Rosenberg J (2015) Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov 22:303–317. doi:10.1177/1553350614552731
Burcharth J, Andresen K, Pommergaard HC, Bisgaard T, Rosenberg J (2014) Recurrence patterns of direct and indirect inguinal hernias in a nationwide population in Denmark. Surgery 155:173–177. doi:10.1016/j.surg.2013.06.006
Kehlet H, Bay-Nielsen M (2008) Nationwide quality improvement of groin hernia repair from the Danish Hernia Database of 87,840 patients from 1998 to 2005. Hernia 12:1–7
Kald A, Nilsson E, Anderberg B, Bragmark M, Engstrom P, Gunnarsson U et al (1998) Reoperation as surrogate endpoint in hernia surgery: a three year follow-up of 1565 herniorrhaphies. Eur J Surg 164:45–50
Rosenberg J, Andresen K, Laursen J (2014) Team training (training at own facility) versus individual surgeon’s training (training at trainer’s facility) when implementing a new surgical technique: example from the Onstep inguinal hernia repair. Surg Res Pract 2014:762761. doi:10.1155/2014/762761
Gillion JF, Chollet JM (2013) Chronic pain and quality of life (QoL) after transinguinal preperitoneal (TIPP) inguinal hernia repair using a totally extraperitoneal, parietalized, polysoft memory ring patch: a series of 622 hernia repairs in 525 patients. Hernia 17:683–692. doi:10.1007/s10029-013-1121-8
Berrevoet F, Sommeling C, De Gendt S, Breusegem C, de Hemptinne B (2009) The preperitoneal memory-ring patch for inguinal hernia: a prospective multicentric feasibility study. Hernia 13:243–249. doi:10.1007/s10029-009-0475-4
Koning GG, Keus F, Koeslag L, Cheung CL, Avçi M, van Laarhoven CJ, Vriens PW (2012) Randomized clinical trial of chronic pain after the transinguinal preperitoneal technique compared with Lichtenstein’s method for inguinal hernia repair. Br J Surg 99:1365–1373. doi:10.1002/bjs.8862
Andresen K, Burcharth J, Fonnes S, Hupfeld L, Rothman JP, Deigaard S, Winther D, Errebo MB, Therkildsen R, Hauge D, Sørensen FS, Bjerg J, Rosenberg J (2015) Short-term outcome after Onstep versus Lichtenstein technique for inguinal hernia repair: results from a randomized clinical trial. Hernia 19:871–877. doi:10.1007/s10029-015-1428-8
Andresen K, Burcharth J, Rosenberg J (2015) ONSTEP versus laparoscopy for inguinal hernia repair: protocol for a randomised clinical trial. Dan Med J 62:A5169
Amid PK, Shulman AG, Lichtenstein IL (1993) Critical scrutiny of the open “tensionfree” hernioplasty. Am J Surg 165:369–371
Bay-Nielsen M, Nordin P, Nilsson E, Kehlet H (2001) Operative findings in recurrent hernia after a Lichtenstein procedure. Am J Surg 182:134–136
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Kumar S (2004) Open mesh versus laparoscopic mesh hernia repair. N Engl J Med 351:1463–1465 (author reply-5)
Phillips EH, Rosenthal R, Fallas M, Carroll B, Arregui M, Corbitt J et al (1995) Reasons for early recurrence following laparoscopic hernioplasty. Surg Endosc 9:140–144 (discussion 144–145)
Heikkinen T, Bringman S, Ohtonen P, Kunelius P, Haukipuro K, Hulkko A (2004) Five-year outcome of laparoscopic and Lichtenstein hernioplasties. Surg Endosc 18:518–522
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403. doi:10.1007/s10029-009-0529-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SÖ reports no potential conflicts of interest, KA reports personal fees from Bard outside the submitted work, DH reports no potential conflicts of interest, JR reports grants from Johnson & Johnson, grants and personal fees from Bard, personal fees from Merck, outside the submitted work.
Ethical approval
The study was approved by the Danish Data Protection 76 Agency (Journal number 03142, ID: HEH-2014-084). The 77 study did not need ethical approval according to the Danish 78 law.
Financial support
This study received no financial support from extramural sources.
Rights and permissions
About this article
Cite this article
Öberg, S., Andresen, K., Hauge, D. et al. Recurrence mechanisms after inguinal hernia repair by the Onstep technique: a case series. Hernia 20, 681–685 (2016). https://doi.org/10.1007/s10029-016-1496-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1496-4