Abstract
Purpose
Anastomotic leakage (AL) after total mesorectal excision (TME) for rectal cancer is suspected to alter function. However, very few reports have been devoted to this problem. The aim of this study was to assess the influence of AL on function and quality of life (QoL) after laparoscopic TME for cancer.
Methods
A total of 170 patients who underwent laparoscopic TME and sphincter-saving surgery for mid and low rectal cancer were included (67 % after neoadjuvant chemoradiotherapy). Twenty-one patients with AL were assessed for function and QoL (Short Form 36 (SF-36), Fecal Incontinence Quality of Life (FIQL), CR-29, and Wexner’s score) at the most recent follow-up. These patients were matched to 42 patients without AL according to sex, body mass index, ypTNM, radiotherapy, and type of anastomosis.
Results
After a median follow-up of 30 months, AL significantly impaired physical activity (SF-36) (p = 0.004), self-respect (FIQL) (p = 0.029), wear pad’s score (Wexner’s score) (p = 0.043), and blood and mucus in stool score (CR-29) (p = 0.001). Overall Wexner’s score did not show any significant difference in the two groups, 8.9 in AL patients vs. 11.6 in patients without AL (p = 0.1).
Conclusion
AL significantly impairs both functional results and quality of life after laparoscopic sphincter-saving TME for rectal cancer. However, the observed difference was only limited, leading to similar outcomes on most of the tested scores. Patients with AL should be warned that if they initially experience severely impaired results, outcomes tend with time to become similar to those observed in noncomplicated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The recent advent of the intersphincteric resection technique [1], along with the reduction of the required distal resection margin [2], led to an increasing rate of sphincter-saving procedures for rectal cancer surgery [3]. As more and more patients are being proposed a restorative procedure, the risk of anastomosis-related complications occurrence is rising.
Anastomotic leakage (AL) remains the most feared complication following sphincter-saving surgery for rectal cancer. Its reported incidence varies widely from 3 to 27 % in the literature [4–7]. This variation is mainly due to differences in the definition of AL and whether it is defined on asymptomatic and/or symptomatic criteria including peri-anastomotic complications, i.e., rectovaginal fistula, or isolated pelvic abscess. AL has been shown to be associated with impaired short-term outcomes after surgery, as it leads to increased postoperative mortality and morbidity rates [8]. Furthermore, the occurrence of an AL after rectal cancer surgery might also impairs long-term outcomes as it might lead to an increased rate of permanent stoma [9, 10]. Finally, AL has been shown to jeopardize long-term oncologic outcomes as several studies provided evidence that AL was significantly associated with an increased local recurrence rate [11, 12].
However, long-term consequences of AL on functional results after sphincter-saving total mesorectal excision (TME) for rectal cancer have not been clearly assessed, as data regarding this specific situation are scarce and conflicting. Bittorf et al. [13] and Riss et al. [14] did not assess any functional impairment after AL, whereas Hallbook et al. [15], Nesbakken et al. [16], and, more recently, Ashburn et al. [17] highlighted a significant relationship between AL and poor functional outcomes.
The aim of this case-matched study was to assess the influence of AL on long-term functional results and quality of life after laparoscopic TME for cancer using standardized and validated scoring systems.
Patients and methods
Study population
All patients who underwent a laparoscopic TME for mid or low rectal adenocarcinoma with a curative intent from September 2004 to December 2010 were identified from our prospective single-center institutional review board-approved database [7] (anastomotic leakage group). To be included in the present study, patients had to fulfill the following criteria: (1) not to have a permanent or temporary stoma, (2) having a follow-up of 6 months or more from the intestinal continuity restoration, and (3) consent to participate and fill the questionnaires. From this latter population, all patients with postoperative AL were identified and constituted the “anastomotic leakage” group. These patients were manually matched in a 2:1 fashion to identical patients without AL after laparoscopic TME for mid or low rectal adenocarcinoma with a curative intent operated on over the same period, according to sex, body mass index (BMI), TNM on the final pathologic specimen, neoadjuvant treatment, and anastomosis type (“no anastomotic leakage” group).
Data collection included patient features (gender, age, BMI), preoperative treatment (neoadjuvant radiotherapy and chemotherapy), intraoperative features (type of anastomosis, intersphincter dissection, and conversion into laparotomy, defined as an unplanned abdominal incision longer than 5 cm), pathological features (tumor location and staging defined according to the TNM classification, circumferential resection margin (CRM), and distal resection margin (DRM)), postoperative outcomes (in-hospital and 30-day postoperative morbidity and mortality), and postoperative treatment (adjuvant chemotherapy).
Surgical procedure
Patients with a T3 and/or an N + tumor on ultrasound and/or magnetic resonance imaging (MRI) preoperative assessment received preoperative radiotherapy (50 Gy in 5 weeks) or chemoradiotherapy. Surgery was routinely performed 8 weeks later. The surgical procedure was performed using a straight laparoscopic approach, with 5-cm lower right quadrant incision, at the site of the temporary diverting stoma, for specimen extraction. The technique involved high ligation of the inferior mesenteric vessels and complete mobilization of the splenic flexure. Rectal dissection was carried on to the pelvic floor with TME and nerve preservation. Reconstruction was either a conventional, stapled, low colorectal anastomosis, or a hand-sewn coloanal anastomosis. In both cases, a side-to-end or an end-to-end anastomosis was fashioned, and a temporary diverting ileostomy was systematically constructed. A pelvic suction drain was always left in place behind the anastomosis. For very low rectal tumors (i.e., located less than 10 mm from proximal edge of the external anal sphincter), an intersphincteric resection (ISR) was performed with either partial or total resection of the internal anal sphincter, according to the level of anal division (i.e., at least 10 mm below the distal edge of the tumor). The diverting ileostomy was closed 6 to 8 weeks after primary surgery, if a systematic CT scan with contrast enema did not show any suspicion of anastomotic leakage.
Outcomes measures
AL was classified as symptomatic or asymptomatic. Symptomatic AL was defined by the presence of peritonitis, fever, or when gas, pus, or feces were discharged from the abdominal drain or from the vagina. All clinical suspicion of AL led to an early CT scan with contrast enema or an early reoperation. Asymptomatic AL was considered if an AL was assessed on the systematic CT scan with contrast enema performed before diverting stoma reversal, without any relevant clinical symptom. On CT scan, all anastomotic dehiscences with leakage into the perirectal cavity, leakages from the efferent limb of the colonic pouch, and isolated pelvic abscesses with no evidence of fistula were considered to be AL. Finally, AL management included conservative treatment with antibiotics, delayed stoma reversal, radiological or surgical drainage, and/or early reoperation, as previously detailed [10].
Functional outcome and quality of life assessment
Quality of life and functional outcomes were assessed using a questionnaire including the Short Form 36 (SF-36), Fecal Incontinence Quality of Life (FIQL), CR-29, and Wexner’s scores. It was submitted to patients by letter, phone, or during consultation at the time of last follow-up.
The SF-36 Health Survey is a validated survey of patient global quality of life [18]. The SF-36 consists of eight scaled scores, ranging from 0 (poorest quality of life) to 100 (best quality of life), including physical functioning (PF), role physical (RP), body pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH) scores. These scores are also grouped into two summary measures: the physical component summary (PCS) and the mental component summary (MCS). The FIQL score scale is a digestive disease-specific quality of life score, comprising 29 items in four scales: lifestyle, coping/behavior, depression/self-perception, and embarrassment [19]. Each item is scored from 1 to 4, with the poorest quality of life scored 1. The EORTC quality of life questionnaire is an integrated system for assessing the health-related quality of life of cancer patients [20]. The colorectal cancer module QLQ-CR-29 is meant to be used among a wide range of patients with colorectal cancer [20]. It includes 38 questions assessing functional scales (body image, anxiety, weight, sexual interest) and symptom scales (urinary frequency, blood/mucus in stool, stool frequency, urinary incontinence, dysuria, abdominal pain, buttock pain, bloating, dry mouth, hair loss, taste, flatulence, fecal incontinence, sore skin, embarrassment, stoma care problems, impotence, and dyspareunia). Finally, the Wexner Continence Grading Scale has become widely used for the assessment of severity of fecal incontinence that considers the frequency of incontinent episodes for solid and liquid stool and flatus, the number of pads required daily, and lifestyle alteration (no incontinence 0 points, severe incontinence 20 points) [21].
Statistical analysis
Quantitative data were reported as mean ± standard deviation and compared with the Mann-Whitney U test. Qualitative data were reported as number of patients (percentage of patients) and were compared with either the Pearson χ 2 test or the Fisher exact test, as appropriate. All tests were two-sided with a level of significance set at p < 0.05.
The overall population was split into two groups: good function and bad function. Bad function was defined as six or more daytime bowel movements and/or three or more nighttime bowel movements and/or Wexner’s score ≥12. Risk factors for bad function were analyzed in univariate and in multivariate analyses. The latter was performed according to a logistic regression model, including all variables with a p value of less than 0.2 in univariate analysis. The results of the multivariate analysis are presented as odds ratio [95 % confidence interval].
All analyses were performed using the Statistical Package for the Social Sciences (SPSS) for Mac OSX software (version 17.0, Chicago, IL, USA).
Results
Patient characteristics
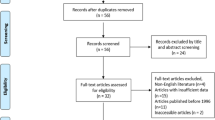
A total of 218 patients underwent a laparoscopic TME with a curative intent for rectal adenocarcinoma in our institution during the study period. Among them, 48 were excluded from the analysis because the surgical procedure performed was an abdominoperineal resection (n = 16) or because they presented a tumor of the upper rectum (n = 32). Therefore, 170 patients (100 males and 70 females) underwent a laparoscopic sphincter-saving TME for mid or low rectal adenocarcinoma with a curative intent during the study period. Fifty-two of the patients had AL complicated surgery (31 %), of whom 21 % had symptomatic AL (11/52) and 79 % asymptomatic AL (41/52). Management of AL included delayed intestinal continuity with (n = 17/52) or without (n = 11/52) antibiotic therapy, CT-guided drainage (n = 9/52), transanal drainage (n = 2), or reoperation (n = 13). At the end of follow-up, 7/52 patients were dead, 14/52 were still defunctionned, 3/52 had a follow-up <6 months from the intestinal conituity restoration, and 7/52 refused to participate. The remaining 21 patients constituted the anastomotic leakage group of the present study. These 21 patients were matched to 60 identical patients whithout AL. Among this latter population, the questionnaires were obtained for 42 patients, who constituted constituted the no anastomotic leakage group.
As detailled in Table 1, patients from both groups did not show any difference regarding gender, age, and BMI. Neoadjuvant radiotherapy, cancer stage, and postoperative chemotherapy did not show any difference between the two groups. Finally, the two groups did not statistically differ regarding tehnical feature of the anastomosis (intersphincteric dissection rate, hand-sewn anastomosis rate, end-to-end anastomosis rate, and level of anastomosis from the anal verge).
Median follow-up after restoration of bowel continuity was similar in the two groups: 30 months [6–70] in the anastomotic leakage group, as compared to 33 months [6–75] in the no anastomotic leakage group (p = 0.413).
Quality of life and functional outcomes
Bowel movement frequency and incontinence
As detailed in Table 2, at the most recent follow-up, frequency of bowel movements did not any show any difference between the two groups, either on daytime (p = 0.684) or nighttime (p = 0.965). Stool fragmentation and lack of ability to defer defection for 15 min were frequent but without any discrepancy, comparing patients with and without AL.
Use of pads was significantly more frequent in patients from the anastomotic leakage group, as compared to patients without anastomotic leakage (p = 0.043). However, overall Wexner’s score did not show any difference between the two groups (Table 3).
Quality of life
Regarding the SF-36 scores, as detailed in Fig. 1, the physical function subscale was significantly impaired in the anastomotic leakage group, as compared to patients without AL (p = 0.04). All other subscales did not show any difference comparing the two groups. Finally, neither the physical component summary nor the mental component summary showed any significant difference between the two groups (p = 0.605 and p = 0.386, respectively).
Figure 2 details the FIQL score for the two groups. Lifestyle, coping/behavior, depression/self-perception, and embarrassment scores were all decreased in the anastomotic leakage group as compared to the “no lifestyle, coping/behavior, depression/self-perception, and embarrassment anastomotic leakage” group although depression/self-perception was the only score to reach statistical difference (p = 0.029).
On the same way, the “blood and mucus in stool” score of the CR-29 was the only score to be significantly impaired in patients with anastomotic leakage (p = 0.001). All CR-29 scores in the two groups are detailed in Fig. 3.
Among the overall population, 33 patients were defined as having a bad function (six or more daytime bowel movements and/or three or more nighttime bowel movements and/or Wexner’s score of ≥12). In univariate analysis, intersphincteric resection and end-to-end anastomosis were significantly associated with bad function (p = 0.002 and p = 0.14, respectively) whereas anastomotic leakage was not associated with impaired function (p = 0.108). In multivariate analysis, intersphincteric resection was the only variable identified as an independent risk factor for bad function (p = 0.018, odds ratio 4.2 [1.3–14.0].
Discussion
This case-matched study aimed to assess the impact of the occurrence of an anastomotic leakage on quality of life and functional results after laparoscopic TME for rectal cancer. Including 21 patients with more than 6 months of follow-up and restored bowel continuity after TME complicated by an AL, matched to 42 patients without AL, we highlighted slightly impaired functional results and quality of life in patients with AL, although most of the studied scores did not show any difference comparing the two groups.
AL remains one the most feared complications after sphincter-saving rectal cancer surgery. Its occurrence has been clearly demonstrated to be associated with impaired short-term outcomes. In a population-based including 6,833 patients, Matthiessen et al. identified anastomotic leakage as an independent risk factor of postoperative mortality after anterior resection of the rectum [8]. AL can also be responsible for the necessity of reoperation that can lead to a risk of permanent stoma, as we previously suggested [10]. Furthermore, AL has been suggested to be associated with impaired oncologic outcomes. Indeed, a recent meta-analysis highlighted a significant relationship between the occurrence of a postoperative AL and the risk of local recurrence, leading to a higher risk of cancer-related mortality in AL patients [12]. For these reasons, we routinely performed a diverting ileostomy in all our sphincter-saving TME patients, as it has been demonstrated to lower the risk of symptomatic AL [4, 22].
Among the 170 patients who underwent a laparoscopic sphincter-saving TME for mid or low rectal adenocarcinoma with a curative intent during the study period, we reported here a 31 % rate of AL, which might be considered as high. However, several factors might explain this observation. Firstly, the included patients were exposed to a high risk of AL, as all only patients with tumors located to the mid or low rectum were included. This factor is now clearly demonstrated as an independent risk factor for AL [23]. Secondly, AL rate is largely dependent on its definition and its method of detection. In the present study, we considered an all-inclusive definition of AL, as both asymptomatic AL and isolated pelvic abscess were also considered. For asymptomatic AL diagnosis, a CT scan with contrast enema was systematically performed before planned intestinal continuity restoration. Our 24 % reported rate of symptomatic AL compares favorably to previous reports in a similar population [1, 24]. In our routine practice, we perform CT scan to detect asymptomatic leakage. Some authors have also reported AL detection using endoscopic procedures [25], which we do not perform routinely. However, to the best of our knowledge, no study to date compared the performance of CT scan and endoscopy for asymptomatic AL diagnosis.
Functional results of sphincter-saving TME are highly multifactorial and have been demonstrated to be correlated with age [26], neoadjuvant irradiation [27], and intersphincteric resection [28]. On the same way, reconstruction with a colonic J pouch was shown to be associated with a lower incidence of anastomotic leakage and better clinical bowel function when compared with straight end-to-end anastomosis [29]. In a more recent study, side-to-end colorectal anastomosis has been shown to be associated with similar surgical and functional results to colonic J pouch [30]. For this reason, we routinely perform a side-to-end anastomosis without J pouch, whenever it is technically possible, in all our TME patients. However, there is surprisingly a lack of data regarding the relationship between AL and functional outcomes after sphincter-saving TME in the literature. The hypothesis that AL might impair function and quality of life can however be proposed, as this relationship has been extensively studied after restorative proctocolectomy with ileal pouch-anal anastomosis [31].
To the best of our knowledge, only five studies assessed the impact of AL on function and quality of life after sphincter-saving TME for rectal cancer [13–17]. Results of these studies are conflicting as Bittorf et al. [13] and Riss et al. [14] did not assess any functional impairment after AL, whereas Hallbook et al. [15], Nesbakken et al. [16], and, more recently, Ashburn et al. [17] highlighted a significant relationship between AL and poor functional outcomes. Furthermore, these studies are impaired by their sample size or design. Indeed, only two were case-matched [15, 16] but those two studies included a very low number of patients: 38 patients [15] and 22 patients [16], respectively. The present study, including 63 patients, compares favorably to those previous reports. The three other studies were retrospective nonmatched study [13, 14, 17]. This nonmatched design can be regarded as a major risk of bias as it can lead to noncomparable groups regarding other risk factors of impaired function. In the present study, patients with and without leakage were matched on major risk factors for bad function and quality of life after sphincter-saving TME (gender, BMI, TNM on the final pathologic specimen, neoadjuvant treatment, and anastomosis type). Furthermore, the two groups did not show any significant difference regarding patients or technical characteristics that might affect the functional prognosis, leading to the constitution of two comparable groups regarding the risk of impaired functional outcomes, besides the AL. However, albeit not significant, there was a difference in the present study regarding the rate of patients having undergone neoadjuvant radiotherapy: 81 % in the AL group versus 62 % in the no AL group. This difference might be regarded as a potential negative selection bias, as neoadjuvant treatment has been shown to alter function [32].
In the present study, all patients who still have a stoma after anastomotic leakage were excluded, as functional results of those patients were not assessable. Among the 45 patients with leakage still alive, 14 still have a stoma: 3 have ileostomy (because of persistent septic complications) and 11 have colostomy (4 for local recurrence and 7 for functional or septic problems). The majority of these patients will probably keep a permanent stoma, leading to an 8 % rate of permanent stoma among the 170 patients who underwent a laparoscopic sphincter-saving TME. Furthermore, it is not clear if patients with permanent stoma have poorer quality of life measures as compared to nonstoma patients: a recent review did not allow firm conclusions as to the question of whether the quality of life after rectal resection for cancer is superior with or without permanent colostomy [33].
In the present study, both functional outcomes and quality of life showed a significant impairment after AL, as compared to patients without AL. But, interestingly, the difference was not as marked as we initially expected. Several reasons might explain this. First, both functional outcomes and quality of life were performed at the end of follow-up, more than 30 months after the intestinal continuity restoration following laparoscopic TME. This important follow-up might not allow the detection of an initial impairment of AL on function, which may improve with time. The results of the study from Ashburn et al. support this hypothesis as the authors reported a more significant impact of AL on functional outcomes at 1 year after surgery than at 3 years postoperatively [17]. This improvement of function with time is of primary importance for patients who experienced an AL after TME.
Second, this lack of important difference between function of patients with and without AL might highlight a crucial point of AL healing physiopathology. Several studies have proposed the negative effect of pelvic sepsis as a cause of fibrosis contributing to poor anorectal function, as a result of reduced neorectal compliance and capacity [17, 21, 34]. However, the results of the present study might not support this theory, as we did not observe any difference regarding number of bowel movements and stool fragmentation between the two groups. One possible explanation of the function impairment of AL might be an excessive inflammation, probably related to a pelvic chronic sinus. This inflammation might be responsible for excessive inflammatory secretion resulting in more frequent neorectal spillage. The increased rate of patients requiring pads observed in the present study supports this hypothesis and could lead to the slight decreased quality of life assessed here.
In conclusion, AL significantly impairs both functional results and quality of life after laparoscopic sphincter-saving TME for rectal cancer. However, the observed difference was only limited, leading to similar outcomes on most of the tested scores. Patients with AL should be warned that if they initially experience severely impaired results, outcomes tend with time to become similar to those observed in noncomplicated patients.
References
Rullier E, Laurent C, Bretagnol F, Rullier A, Vendrely V, Zerbib F (2005) Sphincter-saving resection for all rectal carcinomas: The end of the 2-cm distal rule. Ann Surg 241:465–469
Bokey EL, Ojerskog B, Chapuis PH, Dent OF, Newland RC, Sinclair G (1999) Local recurrence after curative excision of the rectum for cancer without adjuvant therapy: Role of total anatomical dissection. Br J Surg 86:1164–1170
Martin ST, Heneghan HM, Winter DC (2012) Systematic review of outcomes after intersphincteric resection for low rectal cancer. Br J Surg 99:603–612
Matthiessen P, Hallbook O, Rutegard J, Simert G, Sjodahl R (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: A randomized multicenter trial. Ann Surg 246:207–214
Yeh CY, Changchien CR, Wang JY, Chen JS, Chen HH, Chiang JM et al (2005) Pelvic drainage and other risk factors for leakage after elective anterior resection in rectal cancer patients: A prospective study of 978 patients. Ann Surg 241:9–13
Peeters KC, Tollenaar RA, Marijnen CA, Klein Kranenbarg E, Steup WH, Wiggers T et al (2005) Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg 92:211–216
Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K (2005) Postoperative mortality and morbidity in french patients undergoing colorectal surgery: Results of a prospective multicenter study. Arch Surg 140:278–284
Matthiessen P, Hallbook O, Rutegard J, Sjodahl R (2006) Population-based study of risk factors for postoperative death after anterior resection of the rectum. Br J Surg 93:498–503
den Dulk M, Smit M, Peeters KC, Kranenbarg EM, Rutten HJ, Wiggers T et al (2007) A multivariate analysis of limiting factors for stoma reversal in patients with rectal cancer entered into the total mesorectal excision (TME) trial: A retrospective study. Lancet Oncol 8:297–303
Maggiori L, Bretagnol F, Lefevre JH, Ferron M, Vicaut E, Panis Y (2011) Conservative management is associated with a decreased risk of definitive stoma after anastomotic leakage complicating sphincter-saving resection for rectal cancer. Colorectal Dis 13:632–637
Bell SW, Walker KG, Rickard MJ, Sinclair G, Dent OF, Chapuis PH et al (2003) Anastomotic leakage after curative anterior resection results in a higher prevalence of local recurrence. Br J Surg 90:1261–1266
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: Systematic review and meta-analysis. Ann Surg 253:890–899
Bittorf B, Stadelmaier U, Merkel S, Hohenberger W, Matzel KE (2003) Does anastomotic leakage affect functional outcome after rectal resection for cancer? Langenbecks Arch Surg 387:406–410
Riss S, Stremitzer S, Riss K, Mittlbock M, Bergmann M, Stift A (2011) Pelvic organ function and quality of life after anastomotic leakage following rectal cancer surgery. Wien Klin Wochenschr 123:53–57
Hallbook O, Sjodahl R (1996) Anastomotic leakage and functional outcome after anterior resection of the rectum. Br J Surg 83:60–62
Nesbakken A, Nygaard K, Lunde OC (2001) Outcome and late functional results after anastomotic leakage following mesorectal excision for rectal cancer. Br J Surg 88:400–404
Ashburn JH, Stocchi L, Kiran RP, Dietz DW, Remzi FH (2013) Consequences of anastomotic leak after restorative proctectomy for cancer: Effect on long-term function and quality of life. Dis Colon Rectum 56:275–280
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG et al (2000) Fecal incontinence quality of life scale: Quality of life instrument for patients with fecal incontinence. Dis Colon Rectum 43:9–16, discussion -7
Whistance RN, Conroy T, Chie W, Costantini A, Sezer O, Koller M et al (2009) Clinical and psychometric validation of the EORTC QLQ-CR29 questionnaire module to assess health-related quality of life in patients with colorectal cancer. Eur J Cancer 45:3017–3026
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I. (2010) Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev: CD006878.
Matthiessen P, Hallbook O, Andersson M, Rutegard J, Sjodahl R (2004) Risk factors for anastomotic leakage after anterior resection of the rectum. Colorectal Dis 6:462–469
Motson RW, Khan JS, Arulampalam TH, Austin RC, Lacey N, Sizer B (2011) Laparoscopic total mesorectal excision following long course chemoradiotherapy for locally advanced rectal cancer. Surg Endosc 25:1753–1760
Hirst N, Tiernan J, Millner P, Jayne D. (2013) Systematic review of methods to predict and detect anastomotic leakage in colorectal surgery. Colorectal Dis.
Graf W, Ekstrom K, Glimelius B, Pahlman L (1996) A pilot study of factors influencing bowel function after colorectal anastomosis. Dis Colon Rectum 39:744–749
Parc Y, Zutshi M, Zalinski S, Ruppert R, Furst A, Fazio VW (2009) Preoperative radiotherapy is associated with worse functional results after coloanal anastomosis for rectal cancer. Dis Colon Rectum 52:2004–2014
Lewis WG, Holdsworth PJ, Stephenson BM, Finan PJ, Johnston D (1992) Role of the rectum in the physiological and clinical results of coloanal and colorectal anastomosis after anterior resection for rectal carcinoma. Br J Surg 79:1082–1086
Hallbook O, Pahlman L, Krog M, Wexner SD, Sjodahl R (1996) Randomized comparison of straight and colonic J pouch anastomosis after low anterior resection. Ann Surg 224:58–65
Machado M, Nygren J, Goldman S, Ljungqvist O (2003) Similar outcome after colonic pouch and side-to-end anastomosis in low anterior resection for rectal cancer: A prospective randomized trial. Ann Surg 238:214–220
Fazio VW, Kiran RP, Remzi FH, Coffey JC, Heneghan HM, Kirat HT et al (2013) Ileal pouch anal anastomosis: Analysis of outcome and quality of life in 3707 patients. Ann Surg 257:679–685
Bregendahl S, Emmertsen KJ, Lous J, Laurberg S (2013) Bowel dysfunction after low anterior resection with and without neoadjuvant therapy for rectal cancer: A population-based cross-sectional study. Colorectal Dis 15:1130–1139
Pachler J, Wille-Jorgensen P (2012) Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev 12, CD004323
Carmona JA, Ortiz H, Perez-Cabanas I (1991) Alterations in anorectal function after anterior resection for cancer of the rectum. Int J Colorectal Dis 6:108–110
Author information
Authors and Affiliations
Corresponding author
Additional information
What does this paper had contributed to the literature?
This case-matched study highlighted a slight effect of anastomotic leakage on functional results and quality of life after laparoscopic sphincter-saving total mesorectal excision for rectal cancer.
Rights and permissions
About this article
Cite this article
Mongin, C., Maggiori, L., Agostini, J. et al. Does anastomotic leakage impair functional results and quality of life after laparoscopic sphincter-saving total mesorectal excision for rectal cancer? A case-matched study. Int J Colorectal Dis 29, 459–467 (2014). https://doi.org/10.1007/s00384-014-1833-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-1833-y