Abstract
Background
Recent attention has been focused on the relationship between carcinoembryonic antigen (CEA) and pathological complete response (pCR), without consensus regarding its predictive value. This study aims to examine the association between CEA and pCR.
Methods
We conducted a retrospective review of a prospectively maintained database of all patients who underwent primary rectal cancer resection after neo-adjuvant chemoradiotherapy (nCRT). Patients were divided into two groups, pCR or no-pCR, based on final pathology. CEA levels were measured at the initial visit with the surgeon/oncologist and post-completion of nCRT.
Results
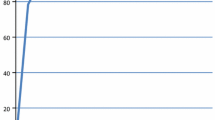
One hundred and forty-one patients underwent primary rectal cancer resections after nCRT. Nineteen patients (13.5 %) achieved pCR, while 122 (86.5 %) had no-pCR. Pre-nCRT CEA levels were not significantly different between groups (2.75 vs 4.5 μg/L, p = 0.65). However, post-nCRT CEA levels were significantly lower in patients with pCR (1.7 vs 2.4 μg/L, p < 0.01). On multivariate logistic regression analyses, low post-nCRT CEA level was an independent predictor of pCR (OR 1.74, CI 1.06, 3.81) and normalization of CEA from an initially elevated level was a highly significant predictor of pCR (OR 64.8, CI 2.53, 18,371).
Conclusion
Low post-nCRT CEA is an independent predictor of pCR, and normalization of CEA post-nCRT is a strong predictor of pCR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant chemoradiation therapy (nCRT) followed by total mesorectal excision (TME) is the current standard of care for locally advanced rectal cancer.1 Neoadjuvant CRT has been shown to decrease rates of local recurrence and is associated with increased incidence of tumor regression and sphincter preservation with negative surgical margins.2 , 3 Following nCRT, between 10 and 30 % of patients will have a pathologic complete response (pCR) with no viable tumor cells remaining in the operative specimen.4 Pathologic complete response is associated not only with decreased rates of local recurrence but also with improved overall as well as disease-free survival.5 – 9
The ability to determine which patients are more likely to achieve pCR following nCRT would be beneficial to guide individualized treatment strategies for this select group of patients, potentially avoiding unnecessary surgery and associated complications. Several studies investigating factors predictive of pCR have been undertaken. However, to date, a definitive set of such predictors remains elusive. Table 1 lists positive and negative predictors of pCR in the current literature.
Several authors have investigated the relationship between carcinoembryonic antigen (CEA) and pCR. Low levels of CEA prior to initiation of nCRT have been associated with pCR.4 , 10 – 13 Two studies described cutoff levels of CEA, post-nCRT and prior to surgery, that have been associated with pCR. These levels were <2.61 and <5 ng/mL, respectively.14 , 15 Conversely, Restivo et al.11 found that a higher CEA level prior to nCRT, more specifically a CEA >5 ng/dL, was associated with incomplete tumor response. The aforementioned studies selected these cutoff levels either by utilizing their laboratory’s upper limit of normal CEA or by constructing receiver operating characteristic (ROC) curves.
The primary aim of this study was to examine the relationship between CEA and pCR in our patient population, more specifically, to determine the predictive potential of normal CEA levels before and after nCRT.
Methods
After institutional review board approval, we conducted a retrospective chart review of a prospectively maintained database of all patients who underwent resection of primary rectal carcinoma after having completed nCRT between January 2007 and November 2013. Demographic variables and clinical and tumor characteristics were collected.
All operations were performed by six colorectal surgeons at our institution. Preoperative diagnosis of rectal adenocarcinoma was confirmed pathologically, by one of four pathologists, via biopsy specimens from colonoscopy. Patients were excluded from the study if they had recurrent disease, had familial colon cancer syndromes, or had undergone previous transanal resections or if information regarding pretreatment or post-treatment tumor staging was missing from their medical file.
Prior to initiation of nCRT, all patients underwent similar diagnostic evaluation in order to determine clinical stage. Thorough physical examination including digital rectal examination (DRE), flexible or rigid sigmoidoscopy, and complete colonoscopy were performed. Endorectal ultrasound and/or pelvic MRI was used to assess tumor stage and nodal status. The presence of distant metastatic disease was assessed with computed tomography scans of the abdomen and chest. Pretreatment CEA level was defined as the level measured at the initial visit with the surgeon or oncologist, prior to initiating nCRT. Post-treatment CEA was defined as the level obtained just prior to surgery. Normalization of CEA was defined as a normal post-treatment CEA level after an initial abnormally elevated pretreatment CEA level. Seventy-nine (56 %) patients had a post-treatment CEA level available. In our laboratory, a normal CEA level ranges from 0 to 3.0 μg/L.
A single radiation oncologist supervised all radiotherapy, which was delivered by one of two methods. Patients received either external beam radiation therapy (EBRT) via a three-field technique, delivering a total radiation dose of between 25 and 60 Gy, or brachytherapy. Brachytherapy for rectal carcinoma involves the introduction of an endorectal applicator consisting of eight catheters surrounding an inflatable tube which, when inflated, serves to immobilize the applicator in the desired location within the rectum. A radiation dose of 26 Gy, given in four fractions, is then administered.20 All patients then underwent TME, consisting of either low anterior resection or abdominoperineal resection, at a median of 8 weeks [IQR 6.5, 11] post-completion of nCRT.
The primary outcome measure of this study was pathologic complete response, defined as absence of viable tumor cells in the operative specimen, including the surrounding lymph nodes (T0N0). Partial response was defined as pathologic tumor downstaging without complete response, while no response was defined as either an absence of tumor downstaging or progression of disease.
Statistical analyses
Categorical variables were reported as percentages, while continuous variables were reported as means (SD). Chi-square, Student’s t, and Wilcoxon rank-sum tests were used for univariate analyses for categorical, normally distributed continuous, and non-normally distributed continuous variables, respectively. All variables with a p value <0.15 on univariate analysis were included in a multivariate logistic regression model. For all analyses, a p value <0.05 was considered to be significant.
Results
One hundred forty-one patients who underwent nCRT prior to primary resection of rectal cancer were identified and included in the study. Of the 141 patients, 85 (60 %) were males and the mean age was 63 (43–87 years). The median pretreatment CEA level was 4.2 μg/L [IQR 2.1–8], and median post-treatment CEA level was 2.4 μg/L [IQR 1.3–4.1]. The majority of patients had a pretreatment clinical stage II (30.5 %) or III (44.6 %) carcinoma. Seventy-four (52.5 %) patients had external beam radiation therapy, while the remainder received brachytherapy. The median interval between completion of nCRT and surgery was 8 weeks [IQR 6.5, 11]. Nineteen patients (13.5 %) achieved pCR, 53 patients (37.6 %) had a partial response, and 69 patients (48.9 %) had either no tumor downstaging or progression of disease. For the purpose of this study, partial responders and non-responders were grouped together as a no-pCR group of 122 patients (86.5 %).
Demographic, tumor, and treatment characteristics are shown in Table 2. Patients who achieved pCR were of similar age, gender, and smoking status when compared to those without pCR. We observed more cases of pCR in diabetic patients whose disease was treated with metformin (26.3 vs 10.7 %, p = 0.07) and in those on statin therapy for dyslipidemia (42.1 vs 25.4 %, p = 0.17); however, these observations did not achieve statistical significance.
Preoperative tumor stage was similar between groups, with the majority of patients from both groups having T3 disease. However, on preoperative clinical staging, we observed fewer involved lymph nodes in patients who achieved pCR compared to those without pCR; however, this difference was not statistically significant (Table 2). We found no other differences in tumor characteristics or treatment characteristics between the two groups.
Pre-nCRT CEA values were available for 136 patients, post-nCRT CEA values were available for 79 patients, and both pre-nCRT and post-nCRT values were available in 79 patients, respectively. On univariate analysis, comparison of CEA levels as a continuous variable between patients who achieved pCR and those who did not demonstrated a strong association between low post-treatment CEA and pCR (Table 3). Furthermore, we found that patients who achieved pCR had normal pretreatment CEA levels 55.6 % (n = 10) compared to 35.6 % (n = 42) of those with no pCR (p = 0.11); however, this observation did not reach statistical significance. Similarly, 90.0 % (n = 9) of patients with pCR had normal CEA post-nCRT, prior to surgery, compared to only 59.4 % (n = 41) of those with no pCR (p = 0.08). When patients with a normal pretreatment CEA (n = 19) were excluded, we found that normalization of CEA was more likely in the pCR group compared to the no-pCR group (83.3 vs 50.9 %, p = 0.11); however, this finding did not reach statistical significance (Table 3).
On multivariate logistic regression for pCR, accounting for age, diabetic patients treated with metformin, pretreatment nodal status, and post-treatment CEA levels, post-treatment CEA levels were a significant independent predictor of PCR with an odds ratio of 1.74 (95 % CI 1.06–3.81) (Table 4). Similarly, when patients with normal pretreatment CEA values were excluded, we observed that normalization of CEA post-nCRT was a strong predictor of pCR with an odds ratio of 64.8 (95 % CI 2.53–18,371) (Table 5).
Discussion
Carcinoembryonic antigen level is a commonly used, inexpensive, and easily measured tumor marker in the diagnostic work-up and surveillance of colorectal cancer.14 The prognostic value of this marker has been widely investigated; however, limited data exists regarding its value in predicting pCR.
In our study, 13.5 % of patients who underwent primary resection for rectal cancer post-nCRT achieved pCR, which correlates well with the 10–30 % pCR rate reported in the literature.4 Contrary to prior studies, we did not find that patients achieving pCR had a significantly lower pre-nCRT CEA level compared to the no-pCR group.4 , 10 – 13 However, we did observe that the pCR group had a significantly lower CEA level post-nCRT, compared to the no-pCR group. On multivariate logistic regression for pCR, taking into account age, diabetic patients treated with metformin, pre-nCRT nodal status, and post-nCRT CEA levels, post-nCRT CEA levels were a significant independent predictor of PCR with an odds ratio of 1.74 (95 % CI 1.06, 3.81). To our knowledge, only two previous studies have demonstrated that low post-nCRT CEA levels are predictive of pCR.14 , 15 Yang et al. found lower post-nCRT CEA levels to be predictive of pCR. More specifically, using ROC curves, they determined that 2.61 ng/mL was the optimal cutoff level for CEA with a sensitivity and specificity of 76 and 58.4 %, respectively. This calculated cutoff value falls within their institution’s laboratory normal range of 0–6 ng/mL. Furthermore, patients whose post-nCRT CEA levels fell below this value had significantly improved 5-year survival compared to those who fell above it (89.3 vs 67.9 % 5-year overall survival).14 Similarly, Perez et al. found that post-nCRT CEA levels of <5 ng/dL were predictive of both pCR as well as 5-year overall survival. These authors also found that low pre-nCRT CEA levels were associated with complete clinical response but not with pCR or improved overall survival. The cutoff of 5 ng/dL was selected since it represents the cutoff of normal CEA at the authors’ institution.15 These findings suggest that a low post-nCRT CEA level is not only predictive of pCR but of overall survival and may be a more useful prognostic tool than pre-nCRT CEA levels.
Furthermore, it is intuitive that a normal post-nCRT CEA value in a patient with a previously elevated value may be of significant prognostic value. Yang et al. demonstrated that normalization of CEA levels post-nCRT predicts tumor regression.14 In our study, when patients with a normal pre-nCRT CEA level were excluded, we found that normalization of CEA post-nCRT, from an initially elevated CEA level, was a significant predictor of pCR resulting in a near 65-fold increased likelihood of achieving pCR. To our knowledge, this is the first study to report that normalization of CEA levels post-nCRT is a strong predictor of pCR. Clinically, this finding is quite interesting as a prognostic factor and can be used as an adjunct in the assessment of complete clinical response.
CEA is widely accepted as an important measure in surveillance following colorectal cancer resection, where post-resection normalization of CEA is expected and is used to monitor for recurrence. It follows that measurement of CEA during and following neoadjuvant treatment may also be used to monitor for disease regression and possible pCR. Our findings that low post-nCRT CEA levels as well as normalization of CEA post-nCRT are strong predictors of pCR in patients with rectal carcinoma reinforce, as well as add, relevant findings to the current literature.
Much of the current research has focused on identifying certain patient, tumor, and treatment characteristics that predict complete regression of the tumor following nCRT, as the achievement of such regression is associated with excellent oncological outcomes.7 At the present time, the gold standard method of assessment of pCR in rectal carcinoma is full pathological examination of the resected specimen following TME. Ideally, a certain subset of patients with tumors more likely to undergo complete regression post-nCRT could be identified, perhaps obviating the need for invasive surgical resection and the associated morbidity and mortality with excellent oncologic outcomes.6 , 21 – 23 For these reasons, the ability to identify certain patient, tumor, or treatment characteristics that may predict pCR is of great importance. Carcinoembryonic antigen is a simple tool that, when used in conjunction with other predictors of pCR, may be beneficial to guide individualized treatment strategies that may potentially allow patients to avoid unnecessary surgery and associated complications.
The major limitation of our study was that it was a single-institution retrospective study with inherent information bias and missing data. Only 42 % (N = 59) of patients had both pre- and post-treatment CEA values, while 136 patients had pretreatment CEA values and 79 had post-treatment CEA values. Due to this missing data, we appropriately reported the available sample size with each reported proportion. Despite these limitations, the strongly significant findings in this study enhance the current understanding of the role of CEA in the assessment of complete pathologic response.
Another limitation of our study that deserves mention is the fact that a large proportion of patients (45.7 %) received neoadjuvant radiation in the form of brachytherapy. While we recognize that brachytherapy for locally advanced rectal cancer is not the standard of care at most institutions, it is being pioneered in our institution with excellent results that have proven to be at least equivalent to external beam radiation.24 Our results are consistent with this finding, as we did not find any statistically significant differences in the rates of pCR in patients receiving brachytherapy compared to conventional EBRT. While radiation modality may differ from other institutions, we believe that normalization of CEA post-nCRT, as demonstrated in our study, remains a strong predictor of pCR.
Conclusion
We demonstrated a significant association between low post-nCRT CEA levels and pCR. Furthermore, we have shown that normalization of CEA post-nCRT from an initially elevated value is a strong predictor of pCR. The ability to predict which patients are likely to achieve pCR, coupled with vigorous surveillance in this subset of patients, may decrease the need for radical surgery and associated morbidity and mortality. In the future, normalization of CEA may be used in conjunction with other validated clinical examination and diagnostic tests to robustly predict pCR.
References
Monson JRT, Weiser MR, Buie WD, Chang GJ, Rafferty JF, Buie WD, Rafferty J; Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of rectal cancer (revised). Dis. Colon Rectum 2013;56:535-550.
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, Karstens JH, Liersch T, Schmidberger H,Raab R; German Rectal Cancer Study Group.Preoperative versus postoperative chemoradiotherapy for rectal cancer. N. Engl. J. Med. 2004;351:1731-1740.
Crane CH, Skibber JM, Feig BW, Vauthey JN, Thames HD, Curley SA, Rodriguez-Bigas MA, Wolff RA, Ellis LM, Delclos ME, Lin EH, Janjan NA.. Response to preoperative chemoradiation increases the use of sphincter-preserving surgery in patients with locally advanced low rectal carcinoma. Cancer 2003;97:517-524.
Wallin U, Rothenberger D, Lowry A, Luepker R, Mellgren A. CEA—a predictor for pathologic complete response after neoadjuvant therapy for rectal cancer. Dis. Colon Rectum 2013;56:859-68.
García-Aguilar J, Hernandez de Anda E, Sirivongs P, Lee SH, Madoff RD, Rothenberger DA. A pathologic complete response to preoperative chemoradiation is associated with lower local recurrence and improved survival in rectal cancer patients treated by mesorectal excision. Dis. Colon Rectum 2003;46:298-304.
Maas M, Nelemans PJ, Valentini V, Das P, Rödel C, Kuo LJ, Calvo FA, García-Aguilar J, Glynne-Jones R, Haustermans K, Mohiuddin M, Pucciarelli S, Small W Jr, Suárez J, Theodoropoulos G, Biondo S, Beets-Tan RG, Beets GL. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol. 2010;11:835-844.
Yeo S-G, Kim DY, Kim TH, Chang HJ, Oh JH, Park W, Choi DH, Nam H, Kim JS, Cho MJ, Kim JH, Park JH, Kang MK, Koom WS, Kim JS, Nam TK, Chie EK, Kim JS, Lee KJ..Pathologic complete response of primary tumor following preoperative chemoradiotherapy for locally advanced rectal cancer: long-term outcomes and prognostic significance of pathologic nodal status. Ann. Surg. 2010;252:998-1004.
Capirci C, Valentini V, Cionini L,De Paoli A, Rodel C, Glynne-Jones R, Coco C, Romano M, Mantello G, Palazzi S, Mattia FO, Friso ML, Genovesi D, Vidali C,Gambacorta MA, Buffoli A, Lupattelli M, Favretto MS, La Torre G.. Prognostic value of pathologic complete response after neoadjuvant therapy in locally advanced rectal cancer: long-term analysis of 566 ypCR patients. Int J Radiat Oncol Biol Phys 2008;72:99-107.
Park Y-A, Sohn S-K, Seong J, Baik SH, Lee KY, Kim NK, Cho CW.Serum CEA as a predictor for the response to preoperative chemoradiation in rectal cancer. J. Surg. Oncol. 2006;93:145-150.
Huh JW, Kim HR, Kim YJ. Clinical prediction of pathological complete response after preoperative chemoradiotherapy for rectal cancer. Dis. Colon Rectum 2013;56:698-703.
Restivo A, Zorcolo L, Cocco IM, Manunza R, Margiani C, Marongiu L, Casula G.. Elevated cea levels and low distance of the tumor from the anal verge are predictors of incomplete response to chemoradiation in patients with rectal cancer. Ann. Surg. Oncol. 2013;20:864-871.
Lin JZ, Pan ZZ, Zeng ZF, Ding PR, Wan D. Multivariate analysis of clinicopathologic factors correlated with pathological complete response following preoperative radiotherapy in rectal adenocarcinoma. Chin. J. Cancer 2009;28:1-5.
Skinner HD, Crane CH, Garrett CR, Eng C, Chang GJ, Skibber JM, Rodriguez-Bigas MA, Kelly P, Sandulache VC, Delclos ME, Krishnan S, Das P. Metformin use and improved response to therapy in rectal cancer. Cancer Med. 2013;2(1):99-107.
Yang KL, Yang SH, Liang WY, Kuo YJ, Lin JK, Lin TC, Chen WS, Jiang JK, Wang HS, Chang SC, Chu LS, Wang LW. Carcinoembryonic antigen (CEA) level, CEA ratio, and treatment outcome of rectal cancer patients receiving pre-operative chemoradiation and surgery. Radiat. Oncol. 2013;8:43-51.
Perez RO, São Julião GP, Habr-Gama A, Kiss D, Proscurshim I, Campos FG, Gama-Rodrigues JJ, Cecconello I. The role of carcinoembriogenic antigen in predicting response and survival to neoadjuvant chemoradiotherapy for distal rectal cancer. Dis. Colon Rectum 2009;52:1137-1143.
Das P, Skibber JM, Rodrigues-Bigas MA, Feig BW, Chang GJ, Wolff RA, Eng C, Krishnan S, Janjan NA, Crane CH.Predictors of tumor response and downstaging in patients who receive preoperative chemoradiation for rectal cancer. Cancer 2007;109:1750-1755.
Kalady MF, de Campos-Lobato LF, Stocchi L, Geisler DP, Dietz D, Lavery IC, Fazio VW.Predictive factors of pathologic complete response after neoadjuvant chemoradiation for rectal cancer. Ann Surg 2009;250:582-589.
Steinhagen E, Shia J, Riedel E, Nash GM, Weiser MR, Temple LK, Paty PB, Guillem JG. Response to neoadjuvant therapy in patients with early age-of-onset rectal cancer. Dis. Colon Rectum 2013;56:58-63.
Jayanand SB, Seshadri RA, Tapkire R. Signet ring cell histology and non-circumferential tumors predict pathological complete response following neoadjuvant chemoradiation in rectal cancers. Int. J. Colorectal Dis. 2011;26:23-27.
Vuong T, Devic S, Moftah B, Evans M, Podgorsak EB. High-dose-rate endorectal brachytherapy in the treatment of locally advanced rectal carcinoma: technical aspects. Brachytherapy 2005;4:230-235.
Habr-Gama A, Perez RO, Wynn G, Marks J, Kessler H, Gama-Rodrigues J. Complete clinical response after neoadjuvant chemoradiation therapy for distal rectal cancer: characterization of clinical and endoscopic findings for standardization. Dis. Colon Rectum 2010;53:1692-1698.
Habr-Gama A, Sabbaga J, Gama-Rodrigues J, São Julião GP, Proscurshim I, Bailão Aguilar P, Nadalin W, Perez RO. Watch and wait approach following extended neoadjuvant chemoradiation for distal rectal cancer: are we getting closer to anal cancer management? Dis. Colon Rectum 2013;56(10):1109-1117.
Habr-Gama A, Perez R, Proscurshim I, Gama-Rodrigues J. Complete clinical response after neoadjuvant chemoradiation for distal rectal cancer. Surg. Oncol. Clin. N. Am. 2010;19:829-845.
Vuong T, Belliveau PJ, Michel RP, Moftah BA, Parent J, Trudel JL, Reinhold C, Souhami L. Conformal preoperative endorectal brachytherapy treatment for locally advanced rectal cancer—early results of a phase i/ii study. Dis. Colon Rectum 2002;45(11):1486 - 1495.
Acknowledgments
We thank Ms. Marie Demian, MSc, for her editorial services.
Author information
Authors and Affiliations
Corresponding author
Additional information
The data in this paper was presented at a Society for Surgery of the Alimentary Tract Quick Shot Presentation at Digestive Disease Week (May 2014, Chicago, IL).
Rights and permissions
About this article
Cite this article
Kleiman, A., Al-Khamis, A., Farsi, A. et al. Normalization of CEA Levels Post-Neoadjuvant Therapy is a Strong Predictor of Pathologic Complete Response in Rectal Cancer. J Gastrointest Surg 19, 1106–1112 (2015). https://doi.org/10.1007/s11605-015-2814-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2814-3