Abstract
Purpose
The concentration of plasma high glucose (HGu) in diabetes mellitus (DM) induces the retinal pigment epithelial cell (ARPE19) death via the increase of inflammation, cytosolic (cytROS), and mitochondrial (mitROS) free oxygen radical generations. Transient potential melastatin 2 (TRPM2) cation channel is stimulated by cytROS and mitROS. Hence, the cytROS and mitROS-mediated excessive Ca2+ influxes via the stimulation of TRPM2 channel cause to the induction of DM-mediated retina oxidative cytotoxicity. Because of the antioxidant role of carvacrol (CRV), it may modulate oxidative cytotoxicity via the attenuation of TRPM2 in the ARPE19. We aimed to investigate the modulator action of CRV treatment on the HGu-mediated TRPM2 stimulation, oxidative stress, and apoptosis in the ARPE19 cell model.
Material and methods
The ARPE19 cells were divided into four groups as normal glucose (NGu), NGu + Carv, HGu, and HGu + CRV.
Results
The levels of cell death (propidium iodide/Hoechst rate) and apoptosis markers (caspases 3, 8, and 9), cytokine generations (IL-1β and TNF-α), ROS productions (cytROS, mitROS, and lipid peroxidation), TRPM2 currents, and intracellular free Ca2+ (Fluo/3) were increased in the HGu group after the stimulations of hydrogen peroxide and ADP-ribose, although their levels were diminished via upregulation of glutathione and glutathione peroxidase by the treatments of CRV and TRPM2 blockers.
Conclusion
Current results confirmed that the HGu-induced overload Ca2+ influx and oxidative retinal toxicity in the ARPE19 cells were induced by the stimulation of TRPM2, although they were modulated via the inhibition of TRPM2 by CRV. CRV may be noted as a potential therapeutic antioxidant to the TRPM2 activation-mediated retinal oxidative injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Diabetes mellitus (DM) is induced by the increase of fasting blood glucose levels. The induction of DM causes several adverse actions in the body cells, including the retina cells. In turn, it causes loss of vision and blindness via the induction of diabetic retinopathy. Hence, diabetic retinopathy is a main cause of blindness in the aged population in developed countries [1, 2]. Around 400 million patients have type 2 DM, and over 45% of them have diabetic retinopathy worldwide. The incidence rises to 50% at 10 years after the onset of DM and arises to 90% at 25 years [3].
Prolonged hyperglycemia-mediated retinopathy is a leading etiological cause of retinal apoptosis and inflammation in patients with DM. The cellular effects of hyperglycemia are not accurately known. A possible mechanism is excessive generation of cytosolic (cytROS) and mitochondrial (mitROS) free oxygen radical (ROS) [4,5,6]. Chronic hyperglycemia causes excessive generations of cytROS and mitROS in the retinal cells and leads to the release of apoptotic and inflammatory factors [4,5,6]. Fructose, the end product of the polyol pathway, contributes to the production of advanced glycosylation products in several cells, including the retina [7, 8]. As a result of this, the excessive generations of cytROS and mitROS cannot be overcome, and the retinal cells are injured by the excessive cytosolic Ca2+ (cytCa2+)-mediated the increase of mitochondrial membrane potential (mitMP) [9]. The activations of polyol pathways also cause diabetic apoptosis in retina cells, including the human retinal pigment epithelial (ARPE19) cells [10]. It was reported that the inhibition of polyol pathway via the treatments of antioxidants, sarco(endo)plasmic reticulum Ca2+-ATPase (SERCA) pump stimulator, and transient receptor potential (TRP) melastatin 2 (TRPM2) blocker induces protective action against the adverse actions of diabetes such as inflammation, apoptosis, and oxidative injury in several cells, except retina [9, 11,12,13]. The involvement of TRPM2 was reported on the DM-mediated overload cytCa2+ influx and mitROS generation in the neuronal cells [14]. However, its involvement in the retina cells has not been evaluated yet.
TRP superfamily contains 28 members such as TRPM2 and TRPM7 in the mammalian cell membranes [15]. TRPM2 channel is a Ca2+ permeable channel, and its main activators are ADP-ribose (ADPR), NAD+, and hydrogen peroxide (H2O2) [16, 17]. The influx of Ca2+ acts modulator action on the modulation of the insulin secretion in the glucose metabolism [18, 19]. However, the high plasma glucose concentration-induced excessive Ca2+ accumulation into mitochondria induced adverse actions such as excessive mitROS generation and apoptosis via the activation of TRPM2 in the hippocampus and dorsal root ganglions (DRGs) of rodents [9, 14, 20]. It has been shown that the incubation of retinal cells with high glucose concentrations causes an increase via the overload Ca2+ influx in pro-inflammatory cytokines such as IL-β and TNF-α [21]. The modulator role of antioxidants such as selenium, melatonin, and N-acetylcysteine via the inhibition of TRPM2 channel on the adverse actions and pro-inflammatory cytokine generations was recently reported in the hippocampus and DRGs of rats [9, 14, 20]. However, the modulator role of carvacrol (CRV) on the adverse action and TRPM2 inhibition in the ARPE19 cells has not been clarified yet.
CRV (2-methyl-5-isopropylphenol) is a monoterpenic phenol and major component of essential oils produced by various plants and spices [22]. The results of recent studies have shown that the treatment of CRV diminished inflammatory cytokine, mitMP, and mitROS generations via the inhibition of Ca2+ influx and TRPM7 in some cells such as rat liver and mice skin [23, 24]. It has been shown experimentally that CRV reverses the oxidative stress and inflammatory cytokine generation symptoms in the DM. The treatment of CRV induces anti-hyperglycemic and antioxidant actions, and reduces DM-related testis oxidative toxicity, cognitive disorders, and apoptosis [25, 26]. The cerebral ischemia-induced oxidative stress was decreased via the inhibition of TRPM7 in rat brain by the treatment of antioxidant CRV [27]. The antioxidant property of CRV may modulate the high glucose (HGu)-induced adverse actions such as mitROS, cytROS, apoptosis, and inflammatory cytokine generations via the modulation of TRPM2 in the ARPE19 cells.
In this study, we investigated the involvement of TRPM2 on the HGu-induced apoptotic, inflammatory, and oxidative adverse actions in the ARPE19 cells. CRV may induce a role in restoring the adverse actions via the inhibition of TRPM2 in the cells.
Material and methods
Cell culture and study groups
The ARPE-19 cells are considered an accepted model for studying retinal pigment epithelial cell metabolism despite the fact that they lack some of characteristics of physiologic RPE. The ARPE19 cells were experimentally used as a model of human retinal pigment epithelium in the high glucose studies [28, 29]. The natural presence of TRPM2 in the ARPE19 cells was also recently reported [30,31,32]. Based on these reasons, we preferred the cells in the current study, and they were a gift from Dr. Xinhua Shu (Glasgow, UK). The cells were incubated at a concentration of 1×106 cells/flask in a T25 flask with filter cap (n = 6) and incubated with a medium mixture (DMEM-LPX/HAM-12-A) supplemented with FBS (10%) and antibiotics (penicillin/streptomycin) (1%) combination at 37 °C in a cell culture incubator. After the incubation of cells for 24 h with the normal (5 mM) concentration of D-glucose (NGu), the medium in the T25 flasks was taken, and the cells were exposed to either NGu (5 mM) or HGu (33 mM) concentrations of D-glucose for another 48 h [28, 29]. In the NGu + CRV and HGu + CRV groups, the cells were further incubated with 200 μM CRV (Sigma Chemical Co., MO, USA) for 24 h [33]. In addition to the T25 flasks, the cells (1×104/ml) were incubated with MatTek 35-mm dishes with bottom glasses (Istanbul, Turkey) in the incubator (NB-203QS) for the analyses of laser confocal microscope (CLSM-800, Carl-Zeiss Foundation, Oberkochen, Germany) and patch-clamp electrophysiology. The analyses were performed in the attached cells. Before treatment induction and analysis, they were kept in the cell culture condition for 24 h. The cells in the 25 T flasks were used for the analyses of antioxidant (spectrophotometer), cytokine, and automatic plate reader (Infinite 200 PRO, Tecan Life Sci., Austria GmbH, Groedig, Austria).
The measurement of cytosolic free Ca2+ (ctyCa.2+) concentration
We assayed HGu incubation-mediated changes on the cytCa2+ concentration in the captured images of ARPE19, which were stained with Fluo 3/AM (1 μM at dark for 60 min) (Thermo Fisher Sci. GmbH, Dreieich, Germany) [31, 32]. For the stimulation of the Fluo 3/AM in the stained cells, argon laser at 488 nm in the CLSM-800 setup attached with Axio Observer 7 inverted microscope with × 20 objective (Carl-Zeiss) was used. Before addition of the TRPM2 stimulator (1 mM and H2O2) to the glass bottom dishes, the dye of Fluo 3/AM from the cells was washed by the extracellular solution. In the CLSM-800 experiments of Fluo 3/AM, 100 μM 2-aminoethoxydiphenyl borate (2APB) was used for antagonizing the TRPM2. The changes of fluorescence intensity in the captured images in ARPE19 were measured in a computer with high resolution by using a specific ZEN program (version ZEN 3.2 blue edition, Carl-Zeiss, Oberkochen, Germany). The unit of arbitrary (a.u.) was used for expressing the fluorescence intensity result.
Patch-clamp electrophysiology analyses
The current records of whole cell configuration were taken in the ARPE19 cells by using the HEKA USB 10 amplifier and Patch-master software (Lamprecht, Germany). The patch pipettes with 1–5 μm tips were fabricated in a PC-10 puller (Narishige Group, Tokyo, Japan) from borosilicate capillary tubes. The ADPR (1 mM) in the cytosolic solution (via path pipette) was administrated into the cells, although the 25 μM TRPM2 antagonist N-(p-amylcinnamoyl)anthranilic acid (ACA) in the heat-controlled chamber was extracellularly administrated to the cells [9, 31, 32]. After obtaining the Giga-Ohm seal in a holding potential (-60 mV), the whole cell records were taken. High ctyCa2+ concentration (886 nM) instead of normal ctyCa2+ concentration (100 nM) in the records was used, because TRPM2 is activated in the presence of high ctyCa2+ concentration [34]. The content details of standard intracellular and extracellular solutions were described in previous studies [9, 31, 35]. The obtained current density data were indicated as pA/pF.
The assays of cell viability and apoptosis
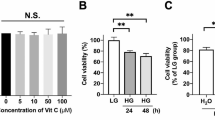
The viability of ARPE19 cells was assayed by using a colorimetric MTT assay as described previously [9, 31, 35]. The absorbance change in the 96-well black plates was determined at 570 nm in the plate reader (Infinite PRO 200).
The HGu-caused apoptosis level in the cells was analyzed at 550 nm in a spectrophotometer (UV-1800, Shimadzu Corporation, Kyoto, Japan) by using an APOPercentage stain (Biocolor Ltd. Northern Ireland). After calculating the rate of optic density/mg protein, the levels of MTT and apoptosis were presented as % of control.
The assays of caspase-3 (CASP/3), caspase-8 (CASP/8), caspase-9 (CASP/9), cytROS, and mitMP
The Ac-DEVD-AMC (for CASP/3), Ac-IETD-AFC (for CASP/8), and Ac-LEHD-AFC (for CASP/9) (Bachem AG., Bubendorf, Switzerland) are three main fluorogenic substrates of passive caspases. When they were incubated with apoptotic cell lysates, AMC and AFCs can be specifically cleaved by the active CASP/3, CASP/8, and CASP/9. The free AMC and AFCs were analyzed in the Infinite 200 PRO at excitation wavelengths of 360–400 nm and emission wavelengths of 460–505 nm [36]. After normalization of the values as optic density/total protein concentration, the fluorescence levels of free AFC and AMCs were indicated as percentage changes of control.
The non-fluorescent version of cytROS is 2′,7′-dichlorofluorescein diacetate (DCFH-DA) (Abcam, Istanbul, Turkey), and it is converted to fluorescent form (DCF) in the cytosol of live cells by oxidants [37]. After incubating the cells with 1 μM DCFH-DA for 35–40 min, its fluorescent form (DCF) was detected in the black plates in the Infinite 200 PRO by using the excitation (at 485 nm)/emission (at 535 nm) rate. The data of DCF were presented as % of control.
JC1 (Abcam) is a fluorescent dye of mitMP (ΔΨm), and it accumulates into mitochondria forming fluorescent aggregates at high ΔΨm [38]. ARPE19 cells in the black plates were incubated with 3 μM JC1 dye at dark for 30–40 min. After washing the dye, they were analyzed in the plate reader (Infinite 200 PRO). After exciting (488 nm) the cells, the fluorescence intensity of JC1 aggregates was detected at 590 nm, although JC1 monomers were assayed at 525 nm in the cells. The obtained data of JC1 dye from the emission ratios (590/525) were presented as % of control.
The analyses of cytROS, mitROS, and mitMP in the confocal laser scanning microscope (CLSM-800)
Mitochondria of live cells are stained by MitoTracker Red CM-H2XRos (Thermo Fisher Sci., Waltham, MA, USA). The accumulation of MitoTracker Red into the live cells is dependent upon membrane potential. The non-fluorescent stain, MitoTracker Red CM-H2XRos, is converted to fluorescent form (MitoTracker Red) in the mitochondria of live cells by the oxidant radicals. We repeated DCFH-DA and JC1 analyses in the ARPE19 by using the CLSM-800. The ARPE19 cells were incubated in the medium of dishes with MitoTracker Red CM-H2XRos (1 μM), DCFH-DA (1 μM), and JC1 (3 μM) for 35–40 min. After removing the dye, the images of mitROS, cytROS, and JC1 in the mitochondria and cytosol were captured in the CLSM-800 [31, 32]. The fluorescence intensity changes of MitoTracker Red, DCF, and JC1 were detected in the area (15 mm2) of each cell for the calibration of intensity, and their changes were calculated in the ZEN program. The data of MitoTracker Red, DCF, and JC1 were shown as a.u.
Cell death rate (PI/Hoechst) analyses
The dye of Hoechst (33342) represents blue color under laser stimulation (at 405 nm), because it can easily pass into the live cell nucleus. The dye of propidium iodide (PI) stains cells with red color under laser stimulation (at 561 nm), because it can accumulate in the injured nucleus. The cells in the medium of dishes were incubated with the mixture of PI (2 μg/ml) and Hoechst 33342 (5 μM) (Cell Signaling Technology, Ankara, Turkey) for 35–40 min before the CLSM-800 analyses [31]. After removing the dyes by washing, the images of red/blue (PI/Hoechst) were recorded in the computer of CLSM-800 (objective: × 20). The fluorescence intensity ratio of PI/Hoechst was determined in the recorded images by using the ZEN, and then the result was shown as percentage changes.
The assay of cytosolic free Zn2+ (cytZn.2+) concentration
FluoZin3 is an active form of RhodZin3/AM fluorescent dye, and it has a high affinity in the labile Zn2+ pool for binding cytZn2+. After the supplementation of 1 μM RhodZin3/AM (Thermo Fisher Sci.) to the medium of ARPE19 cells in the dishes, the cells were kept for 35–40 min [31]. After removing the dye by using the extracellular solution, the images of cells were recorded in the CLSM after the laser excitation (488 nm) (objective: × 20). The laser wavelengths of fluorescence were 493 nm (excitation) and 513 nm (emission) in the cells, respectively. After the detection of fluorescence intensity by using the ZEN program, the mean data were presented a.u.
The analysis of glutathione, glutathione peroxidase (GPx), and lipid peroxidation (LPO)
The concentrations of glutathione as reduced glutathione and the activity GPx in the ARPE19 cells were determined at 412 nm by using the spectrophotometer (UV-1800), whereas the concentration of LPO was measured at 532 nm. The details of glutathione, GPx, and LPO analyses are shown in the previous studies [9, 39].
The analysis of cytokines
The analyses of IL- β and TNF-α were performed in the ELISA (Infinite 200 PRO) by using the R&D System commercial kits (Minneapolis, MN, USA). In the analyses, the company’s instruction was used [35]. Total protein levels in the cells were analyzed by using Biuret’s solution. After the calculation of IL-β and TNF-α levels for the standard curves, the results were expressed as % of control (NGu).
Statistical analysis
The analyses of statistics were performed in the SPSS program. The data were presented as means ± standard deviation (SD) according to the one-way ANOVA test and Student t-test. The mean ± standard deviation (SD) was used for the expression of the current data. A p value of < 0.05 was accepted to be of statistical significance and indicated by using the asterisks (*, x,, Δ).
Results
The treatment of CRV diminished HGu-mediated increase of cytCa.2+ concentration via the attenuation of TRPM2 in the ARPE19 cells
The HGu-induced oxidative stress may activate the TRPM2, and its activation may be modulated by the treatment of CRV. Therefore, we investigated the protective role of antioxidant CRV on the upregulation of HGu-induced TRPM2 stimulation and cytCa2+ concentration in the cells.
The images of cytCa2+ in four groups (NGu, NGu + CRV, HGu + CRV, and HGu + CRV) are shown in the Fig. 1a. The concentration of cytCa2+ was significantly (p ≤ 0.05) upregulated in the four groups after the stimulation of H2O2 (1 mM) (Fig. 1b); its concentration was markedly (p ≤ 0.05) downregulated in the H2O2 + 2APB groups by the treatment of 2APB (Fig. 1c). The images of cytCa2+ from the groups of HGu and HGu + CRV were continually recorded for 201 s, and their concentrations were shown in Fig. 1d and g. The concentration of cytCa2+ was higher in the HGu group (Fig. 1e and f) as compared to the HGu + CRV group (Fig. 1h and i). However, the concentration of cytCa2+ was decreased in the HGu + CRV (Fig. 1e) by the CRV treatment (p ≤ 0.05). In addition, the concentration of cytCa2+ was further decreased in the groups of HGu + CRV + 2APB by the CRV + 2APB treatment (p ≤ 0.05). Hence, we observed the modulator role of CRV on the HGu-induced TRPM2 activation in the cells.
The TRPM2 stimulation-induced upregulation of cytCa2+ was downregulated in the ARPE19 by the CRV treatment. (n = 25–30). After staining the ARPE19 cells with the cytCa2+ indicator dye (1 μM Fluo 3/AM for 90 min), the TRPM2 stimulators (H2O2 and 1 mM) and blockers (2APB and 100 μM) were applied to the cells in four groups (NGu, NGu + CRV, HGu, and HGu + CRV). The fluorescence intensity of Fluo 3/AM in the captured ARPE19 images was analyzed at 515 nm in the CLSM-800 attached with Axio Observer 7 microscope and objective (× 20). The changes of fluorescence intensity were shown by the unit of arbitrary (a.u.). (a) The images of the Fluo 3/AM in the four groups. (b) and (c) The representation of mean fluorescence intensities in the four groups with/without H2O2 and 2APB were shown by columns. (d) The images of HGu. (e) and (f) The mean fluorescence intensity changes of cytCa2+ in the HGu group for 201 s. (g) The images of HGu + CRV. (h) and (i) The mean fluorescence intensity of cytCa2+ in the group of HGu + CRV (*p ≤ 0.05 vs. (-H2O2) group. p ≤ 0.05 vs. NGu and NGu + CRV. Δp ≤ 0.05 vs. H2O2 group. ap ≤ 0.05 vs. HGu. bp ≤ 0.05 vs. HGu + H2O2)
The ADPR-induced TRPM2 current density in the ARPE19 was increased by the treatment of HGu: Protective role of CRV
The patch-clamp technique is a valuable method for checking the activation of cation channels, including the TRPM2. In addition to the Fluo 3/AM analyses, we further tested HGu-mediated stimulation of TRPM2 in the cells by using cytosolic (in patch pipette) TRPM2 stimulator (ADPR and 1 mM). In the patch-clamp analyses, we induced whole cell configuration in the cells (Fig. 2a and b). There was limited current (0.05nA) in the cells of HGu group without stimulation (Fig. 2c). In the NGu groups, the TRPM2 was activated up to 0.4nA (Fig. 2d) by the ADPR, although it was gated up to 0.9nA in the HGu group (Fig. 2e). Hence, the current density was higher in the HGu than in the NGu (p ≤ 0.05) (Fig. 2i). The ADPR-mediated current records in the NGu and HGu groups were downregulated to control levels by the treatments of NMDG+ and ACA (Fig. 2d and e). The treatment of HGu accelerated TRPM2 activation in the ARPE19, and the activation time as minute was longer in the NGu group (1.41 min) than in the HGu group (0.89 min) (p ≤ 0.05) (Fig. 2h). In the HGu (0.06nA) (Fig. 2f) and NGu (0.04nA) (Fig. 2g) groups, there were limited (as control) currents after the ADPR stimulation. The TRPM2 currents were lower in the NGu + ADPR + CRV and HGu + ADPR + CRV than in the groups of NGu + ADPR and HGu + ADPR (p ≤ 0.05) (Fig. 2i). These data obviously evidenced the involvement of HGu on TRPM2 stimulation in the ARPE19 cells. By the patch-clamp record results, the modulator role of CRV on the HGu-induced TRPM2 stimulation in the ARPE19 was further confirmed.
The ADPR-induced stimulation of TRPM2 was increased in the ARPE19 by the treatment of HGu (33 mM for 48 h), although TRPM2 activity was diminished by the treatment of CRV (200 μM for 24 h). (Mean ± SD and n = 3–6). The patch-clamp records were taken as whole cell (W.C.) configuration after inducing the voltage-clamp (at − 60 mV). (a) The image of W.C. configuration in the cells of patch-chamber. (b) The image of W.C. configuration between cell and patch pipette. (c) The current records of HGu without cytosolic ADPR (1 mM) stimulation. (d) The TRPM2 current and current (I)/voltage (V) rate changes in the NGu + ADPR group. The ADPR (1 mM) stimulation-induced TRPM2 currents were inhibited by the administration of ACA (25 μM) and NMDG+. (e) The TRPM2 current and I/V changes in the HGu + ADPR group. (f) The currents of the HGu + ADPR + CRV group after ADPR stimulation. (g) The TRPM2 currents from the NGu + ADPR + CRV group after ADPR stimulation. (h) The TRPM2 activation times in the NGu and HGu after ADPR stimulation were indicated by columns. (i) The mean current density changes in the four groups (NGu, NGu + CRV, HGu + CRV, and HGu + CRV) with/without ADPR and ACA treatments (ap ≤ 0.05 vs. NGu. bp ≤ 0.05 vs. NGu + ADPR. cp ≤ 0.05 vs. HGu + ADPR)
The HGu-induced increase of mitROS, mitMP, and cytROS concentrations was downregulated via the inhibition of TRPM2 by the treatment of CRV
To our knowledge, there is no report on the HGu-induced mitROS, mitMP, and cytROS changes via the activation of TRPM2 activation in the ARPE19 cells. After observing the increase of TRPM2 stimulation in the ARPE19, we suspected whether mitROS, mitMP, and cytROS upregulated via the increase of TRPM2.
The normal (Fig. 3a) and 2.5D (Fig. 3b) images of the mitROS, JC1, and cytROS were recorded in the confocal microscope (CLSM-800). The JC1 (Fig. 3f) and DCF (Fig. 3g) analyses were also repeated in the microplate reader. The mean fluorescence intensities of mitROS (Fig. 3c), mitMP (Fig. 3d and f), and cytROS (Fig. 3e and g) were markedly upregulated in the HGu group as compared to the NGu and NGu + CRV (p ≤ 0.05). However, the treatments of CRV and 2APB diminished the action of HGu via the decrease of mitROS, mitMP, and cytROS in the cells (p ≤ 0.05). The upregulation of TRPM2 stimulation following HGu corresponded with upregulated mitROS, mitMP, and cytROS, although their increases were downregulated in the HGu + CRV and HGu + 2APB by the treatments of CRV and 2APB. Hence, the data of mitROS, mitMP, and cytROS further supported the activation of TRPM2 on mitochondrial oxidative stress generation in the cells.
The HGu-induced increases of mitROS (MitoTracker), mitMP (JC1), and cytROS (DCF) concentrations were downregulated in the ARPE19 by the treatments of CRV and TRPM2 antagonist (2APB). (Mean ± SD). After staining the cells with MitoTracker Red CM-H2ros (1 μM), JC1 (3 μM), and DCFH-DA (1 μM) dyes, the normal (a) and 2.5D (b) images of MitoTracker Red, JC1, and DCF were captured in the CLSM-800 with the × 20 objective. The mean fluorescence intensities of MitoTracker (c), JC1 (d), and DCF (e) were measured in the images by using the ZEN program. Arbitrary unit: a.u. The JC1 (f) and DCF (g) analyses were also repeated in the microplate reader (*p ≤ 0.05 vs NGu and NGu + CRV groups. × p ≤ 0.05 vs HGu group)
The results of LPO, glutathione, and GPx in the ARPE19
The presence of a direct relationship between glutathione and TRPM2 activation in the neurons was reported [31]. However, the relationship has not been clarified in the ARPE19 yet. Hence, we analyzed LPO level (Fig. 4a), glutathione concentration (Fig. 4b), and GPx activity (Fig. 4c) in the ARPE19. The glutathione concentration and LPO activity were diminished in the ARPE19 by the HGu exposure, although the LPO level was increased in the cells by the exposure (p ≤ 0.05). However, the glutathione concentration and GPx activity were upregulated in the ARPE19 by the treatments of 2APB and CRV, whereas the LPO level was decreased in the HGu + CRV and HGu + 2APB groups by the treatments (p ≤ 0.05). The present results indicate that the HGu-induced decrease of the antioxidants (glutathione and GPx) was upregulated via the inhibition of LPO in the cells by the CRV treatment and TRPM2 inhibition.
The HGu-induced increases of lipid peroxidation (LPO), glutathione, and glutathione peroxidase (GPx) were diminished via the TRPM2 inhibition (ACA) in the ARPE19 cells by the treatment of CRV. (N = 7 and mean ± SD). The concentrations of LPO (a), glutathione (b), and GPx (c) were manually determined in the spectrophotometer (UV-1800) (*p ≤ 0.05 vs NGu and NGu + CRV groups. × p ≤ 0.05 vs HGu group)
The treatments of CRV and TRPM2 antagonists attenuated the markers of apoptosis and ARPE19 death
The inactive caspases such as CASP/3, CASP/8, and CASP/9 are activated by the increase of mitMP [40, 41]. The TRPM2-mediated overload Ca2+ influx induces the increase of mitMP in the ARPE19 [31, 32, 35]. After finding the increase of TRPM2-mediated cytCa2+ and mitMP in the ARPE19, we predicted the increase of apoptotic and ARPE19 death markers in the cells.
The activities of CASP/3 (Fig. 5a), CASP/8 (Fig. 5b), and CASP/9 (Fig. 5c) and the percentage of apoptosis (Fig. 5d) were increased in the HGu compared with the NGu and NGu + CRV, whereas cell viability level was diminished in the cells by the HGu treatment (p ≤ 0.05) (Fig. 5e). However, the treatments of CRV and ACA decreased the levels of CASP/3, CASP/8, and CASP/9, and apoptosis in the ARPE19. The ARPE19 viability level was increased in the HGu + CRV and HGu + ACA group by the CRV and ACA treatments (p ≤ 0.05). The cell death was observed in the images of bright field (BF) (Fig. 6a), PI, Hoechst, merge (Fig. 6b), and 2.5D (Fig. 6c) after the HGu incubation. The percentage changes of PI/Hoechst rate were increased in the HGu group compared with the NGu and NGu + CRV groups, although the ARPE19 death rate was diminished in the HGu + CRV and HGu + ACA by the CRV and ACA treatments (p ≤ 0.05) (Fig. 6d).
The HGu (33 mM for 48 h)-induced increases of CASP/3, CASP/8, CASP/9, and apoptosis were diminished in the ARPE19 cells by the treatments of CRV (200 μM for 24 h) and TRPM2 antagonist (ACA). (N = 6 and mean ± SD). The activities of CASP/3 (a), CASP/8 (b), and CASP/9 (c) were assayed in the plate reader (Infinite PRO 200) by using the caspase substrates, although apoptosis (d) and cell viability (e) level were manually determined in the plate reader in the spectrophotometer (UV-1800) by using the commercial dye (APOPercentage) and MTT, respectively (*p ≤ 0.05 vs NGu and NGu + CRV groups. × p ≤ 0.05 vs HGu group)
The HGu (33 mM for 48 h)-induced ARPE19 cell death was downregulated by the treatments of CRV (200 μM for 24 h) and TRPM2 antagonist (2APB). (N = 20–30 and mean ± SD). The bright field (BF) (a), red PI, blue Hoechst, and merge (b) images were recorded in the CLSM-800 setup attached with Axio Observer 7 inverted microscope with 20 × objective. (c) The percentage changes of PI/Hoechst rate (*p ≤ 0.05 vs NGu and NGu + CRV groups. × p ≤ 0.05 vs HGu group)
The HGu (33 mM for 48 h)-induced increase of cytZn.2+ was modulated in the ARPE19 by the treatments of CRV and 2APB
The excessive influx of cytZn2+ into mitochondria upregulates mitMP and mitROS via the decrease of glutathione and GPx in the ARPE19 [31, 42]. We aimed to clarify the HGu-induced increase of cytZn2+ concentration in the ARPE19 treated with CRV and 2APB. The fluorescence intensity changes of cytZn2+ were measured in the captured cells by using the ZEN program (Fig. 7a). The concentration of cytZn2+ was increased in the cells as a result of HGu treatment (p ≤ 0.05). However, the treatments of CRV and 2APB diminished the action of HGu via the inhibition of cytZn2+ accumulation in the cells (p ≤ 0.05) (Fig. 7b).
The HGu (33 mM for 48 h)-induced cytZn.2+ increase was downregulated via the TRPM2 inhibition (2APB) by the treatment of CRV (200 μM for 24 h). (N = 20–30 and mean ± SD). The RhodZn3 green and 2.5D images (a) were recorded in the CLSM-800 setup attached with Axio Observer 7 inverted microscope with 20 × objective. (b) The percentage changes of RhodZn3 (*p ≤ 0.05 vs NGu and NGu + CRV groups. × p ≤ 0.05 vs HGu group)
The HGu (33 mM for 48 h)-induced cytokine (IL-1β and TNF-α) production increase was modulated in the ARPE19 by the treatments of CRV and 2APB
The HGu-mediated increase of mitMP and mitROS stimulates the generations of cytokines such as IL-1β and TNF-α in the ARPE19 [6, 29], although the involvements of TRPM2 and CRV have not been clarified yet. We analyzed generations of IL-1β and TNF-α in the ARPE19 after the treatments of HGu, CRV, and 2APB. The generation of IL-1β (Fig. 8a) and TNF-α (Fig. 8b) was increased in the cells as a result of HGu treatment (p ≤ 0.05). However, the treatments of CRV and 2APB decreased the action of HGu via the inhibition of IL-1β and TNF-α productions in the cells (p ≤ 0.05).
The HGu (33 mM for 48 h)-induced cytokine (IL-1β and TNF-α) production increase was downregulated via the TRPM2 inhibition (2APB) by the treatment of CRV (200 μM for 24 h). (N = 9 and mean ± SD). The activities of IL-1β (a) and TNF-α (b) were assayed in the ELISA (Infinite PRO 200) by using the commercial kit (R&D Systems) (*p ≤ 0.05 vs NGu and NGu + CRV groups. × p ≤ 0.05 vs HGu group)
Discussion
We aimed to investigate the modulator action of CRV treatment via the block of TRPM2 on the HGu-induced oxidative stress and apoptosis in the ARPE19. The levels of apoptosis (CASP/3, CASP/8, and CASP/9), cell death (PI/Hoechst) rate, cytokine generations (IL-1β and TNF-α), ROS generations (cytROS, mitROS, and LPO), TRPM2 currents, and cytCa2+ concentration were upregulated in the HGu group by the stimulations of TRPM2 (ADPR and H2O2), although their levels were diminished via the upregulation of glutathione and GPx by the treatments of TRPM2 antagonists (ACA and 2APB) and CRV. In summary, the current data obviously demonstrate that the HGu as a model of DM induces ARPE19 cell death and oxidative toxicity via the stimulation of TRPM2, although the treatment of CRV via the modulation of TRPM2 induces the cell death and toxicity.
C-terminal NUDT9H domain of TRPM2 contains ADPR hydrolase enzyme, and the enzyme is essential for the activation of TRPM2 [43, 44]. Hence, ADPR involves in the TRPM2 channel regulation in several cells, including ARPE19 [9, 31, 32]. In accordance with the reports, the present electrophysiology results indicate that TRPM2 is activated in the NGu group by the cytosolic ADPR stimulation. ADPR is produced in the nucleus of cells by mitochondria oxidative stress and DNA repair mechanisms (via PARP1 activity) [16, 17, 45]. DM is characterized HGu-induced increase of mitochondria oxidative stress and DNA damage [3,4,5]. In the experiments of patch-clamp and Fura 3/AM, the TRPM2 is further gated in the HGu group as compared to the NGu group after the stimulations of H2O2 and ADPR. The antioxidant and TRPM7 blocker properties of CRV were reported in several cells, except ARPE19 [23, 24]. It has been reported that CRV reverses the oxidative stress symptoms in the DM, and it reduces DM-related testis oxidative toxicity, cognitive disorders, and apoptosis via its anti-hyperglycemic and antioxidant properties [25, 26]. In the current study, we observed similar cation channel modulator action of CRV in the ARPE19 cells, and the HGu-induced TRPM2 activation was fully inhibited in the HGu + CRV group by the treatment of CRV.
The essential actors in the extrinsic and intrinsic pathways of apoptosis are CASP/3, CASP/8, and CASP/9 in several cells, including the ARPE19 [45]. The increase of cytCa2+ via the activation of TRPM2 stimulates the release of CASP/3, CASP/8, and CASP/9 in the ARPE19 [31, 32], although the increases of caspases were downregulated in neuronal cell lines by treatment of CRV treatment [46]. We observed that HGu treatment at 33 mM for 48 h greatly decreased ARPE19 viability. However, pretreatment with CRV significantly modulated this reduction in the ARPE19 viability. There are evidences showing that the HGu-induced retina oxidative injury and neurotoxicity occur in the ARPE19 and SH-SY5Y cells by the activation of apoptotic pathways [3, 6, 7, 9, 47]. It was suggested that the increases in mitROS and cytROS formations that are induced by HGu-induced excessive Ca2+ influx via the TRPM2 activation lead to ARPE19 cell apoptosis via the accumulations of CASP/3, CASP/8, and CASP/9 [31, 32]. In turn, the induction of apoptosis causes ARPE19 cell death via the additional activation of TRPM2 [35]. Therefore, the inhibition of CASP/3, CASP/8, and CASP/9 activities via the inhibition of TRPM2 may be associated with retina protective actions against HGu. Consistent with these results, in the current study, the treatment of HGu caused an increase in the cell death (PI/Hoechst) ratio and elevations in CASP/3, CASP/8, and CASP/9 activities in ARPE19 cells. This effect, however, was markedly modulated by the treatments of CRV and TRPM2 antagonists (ACA and 2APB), suggesting that CRV effectively protects ARPE19 cells against HGu-induced retina toxicity and apoptosis by inhibiting the TRPM2 channel activity signaling pathways.
It has been suggested that HGu-mediated inflammation is involved in the ARPE19 death and that a wide range of inflammatory factors such as TNF-α and IL-1β causes oxidative toxicity to the ARPE19 [29]. The excessive generation of mitROS and cytROS may also initiate inflammatory responses via the activation of calcium signaling pathways [45, 46]. The activation of TRPM2 has been implicated as an important pathway in the inflammatory cytokine responses such as TNF-α and IL-1β, exerting direct ARPE19 oxidative cytotoxic effects [35]. In the current study, we observed that exposing ARPE19 cells to HGu resulted in increased cytokine (TNF-α and IL-1β) levels and that treatment with CRV modulated the HGu-mediated increase in IL-1β and TNF-α activity in ARPE19.
The retina is an essential target of cytROS and mitROS because of the high oxygen consumption rate [3, 8]. The excessive Ca2+ influx via the activation of TRPM2 increases the generation of cytROS and mitROS by the opening mitochondrial permeability transition pore and injuring mitMP [43]. The inhibition of TRPM2 via the antioxidant treatments such as glutathione and N-acetyl cysteine regulates mitochondrial permeability transition pore via the regulation of Ca2+ influx by decreasing the cytROS and mitROS in several cells [9, 48, 49]. The production of ADPR is induced in the nucleus of ARPE19 by the activity of PARP1 enzyme, and its production activates TRPM2 in several cells, including the ARPE19 [43]. The anti-hyperglycemic and antioxidant actions of CRV were reported in neurons and testis [25, 26, 50], and its treatment upregulated the antioxidant levels such as glutathione and GPx in the testis of diabetic animals [22, 26]. In the arsenite-stressed canine retinal pigment epithelium cells, the modulator role of CRV on the stress proteins was recently reported [51]. The diabetes-induced adverse actions were attenuated in the liver of the mice with streptozotocin-induced diabetes and oxygen-induced retinopathy rat model [52, 53]. In accordance with the cytROS, mitROS, glutathione, and GPx reports, we observed that the modulation of TRPM2 downregulated the generations of cytROS, mitROS, and LPO via the upregulation of glutathione and GPx in the ARPE19 cells (Fig. 9). Moreover, the upregulation of mitROS was downregulated when the cells were treated with the treatments of TRPM2 antagonists (ACA and 2APB). Hence, the inhibitions of cytROS and mitROS via the CRV treatment are possibly inhibitor signals, which TRPM2 modulates mitMP. Similarly, the HGu-induced increase of mitROS and the decrease of the glutathione and GPx were modulated in the ARPE19 cell by the inhibition of TRPM2 [35].
The proposed protective pathways of carvacrol against high glucose (HGu)-induced TRPM2 activation, apoptosis, oxidative stress, and cytokine generation in the ARPE19 cells. The C domain of TRPM2 in NUDT9 is activated by PARP1 activation-induced ADP-ribose (ADPR) and oxidative stress, although TRPM2 is blocked in the ARPE19 cells by glutathione (GSH), ACA, and 2APB. The HGu stimulates mitochondrial membrane potential (mitMP), which may promote TRPM2-mediated Ca2+ influx. The increased TRPM2-mediated Ca.2+ influx induces the increased activity of oxidative stress (cytosolic and mitochondrial ROS productions), inflammatory (IL-1β and TNF-α), and apoptotic factors (caspase-3, caspase-8, and caspase-9), which stimulate apoptotic signaling pathways, ultimately resulting in cell death. Carvacrol reduces HGu-induced ARPE19 apoptosis, inflammatory cytokine generation, cytosolic ROS, and mitochondrial ROS productions via downregulation of TRPM2 activity, but upregulation of GSH and glutathione peroxidase (GPx). Arrow pointing upward (↑), increase. Arrow pointing downward (↓), decrease
In summary, present data indicate that the exposure to HGu upregulates TRPM2 activity in the ARPE19 cells. This suggests that it may contribute to the initiation and propagation of apoptosis, inflammation, and mitochondrial oxidative stress. We demonstrated that the treatment of CRV inhibits the HGu-induced retina oxidative cytotoxicity by downregulating apoptotic signaling pathway that involves TRPM2 signaling and by reducing cytCa2+ increase-mediated inflammatory factors in the ARPE19 cells. Hence, inhibiting the TRPM2 via the CRV treatment may defend the ARPE19 against diabetes mellitus-mediated mitochondrial oxidative injury and cellular death. Therefore, the treatment of CRV may be considered a beneficial strategy against TRPM2 activation-induced ARPE19 cell death.
Data availability
The data analyses in the current study were performed in the BSN Health, Analyses, Innov., Consul., Org., Agricul. and Industry Ltd (Isparta, Turkey) https://www.bsnsaglik.com.tr/. The details of current analyses are available from Prof. Dr. M. Nazıroğlu on reasonable request.
Abbreviations
- 2APB:
-
2-Aminoethoxydiphenyl borate
- ACA:
-
N-(p-amylcinnamoyl)anthranilic acid
- ADPR:
-
ADP-ribose
- ARPE19:
-
Adult retinal pigment epithelial 19
- BF:
-
Bright field
- Ca2+ :
-
Calcium ion
- CASP/3:
-
Caspase 3
- CASP/8:
-
Caspase 8
- CASP/9:
-
Caspase 9
- CLSM:
-
Confocal laser scanning microscope
- CRV:
-
Carvacrol
- cytCa2+ :
-
Cytosolic free calcium ion
- cytROS:
-
Cytosolic free reactive oxygen radicals
- cytZn2+ :
-
Cytosolic free Zn2+
- DM:
-
Diabetes mellitus
- DRG:
-
Dorsal root ganglion
- ROS:
-
Free reactive oxygen radicals
- GPx:
-
Glutathione peroxidase
- HGu:
-
High glucose
- LPO:
-
Lipid peroxidation
- mitROS:
-
Mitochondrial free reactive oxygen radicals
- mitMP:
-
Mitochondrial membrane potential
- NGu:
-
Normal glucose
- PARP1:
-
Poly [ADP-ribose] polymerase 1
- SERCA:
-
Sarco(endo)plasmic reticulum Ca2+-ATPase
- TRP:
-
Transient receptor potential
- TRPM2 :
-
Transient receptor potential melastatin 2
References
Buch H, Vinding T, La Cour M, Appleyard M, Jensen GB, Nielsen NV (2004) Prevalence 9 and causes of visual impairment and blindness among 9980 Scandinavian adults: The 10 copenhagen city eye study. Ophthalmology 111:53–61
Quartilho A, Simkiss P, Zekite A, Xing W, Wormald R, Bunce C (2016) Leading causes of certifiable visual loss in England and Wales during the year ending 31 March. Eye (Lond) 30(4):602–607. https://doi.org/10.1038/eye.2015.288
Calderon GD, Juarez OH, Hernandez GE, Punzo M, De la Cruz ZD (2017) Oxidative stress and diabetic retinopathy: development and treatment. Eye (Lond) 31(8):1122–1130. https://doi.org/10.1038/eye.2017.64
Tsai FJ, Li TM, Ko CH et al (2017) Effects of Chinese herbal medicines on the occurrence of diabetic retinopathy in type 2 diabetes patients and protection of ARPE-19 retina cells by inhibiting oxidative stress. Oncotarget. 8(38): 63528–63550. https://doi.org/10.18632/oncotarget.18846
van der Schaft N, Schoufour JD, Nano J et al (2019) Dietary antioxidant capacity and risk of type 2 diabetes mellitus, prediabetes and insulin resistance: The rotterdam study. Eur J Epidemiol 34:853–861. https://doi.org/10.1007/s10654-019-00548-9
Sun H, Zhao H, Yan Z, Liu X, Yin P, Zhang J (2021) Protective role and molecular mechanism of action of Nesfatin-1 against high glucose-induced inflammation, oxidative stress and apoptosis in retinal epithelial cells. Exp Ther Med 22(2):833. https://doi.org/10.3892/etm.2021.10265
Madsen-Bouterse SA, Kowluru RA (2008) Oxidative stress and diabetic retinopathy: pathophysiological mechanisms and treatment perspectives. Rev Endocr Metab Disord 9(4):315–327. https://doi.org/10.1007/s11154-008-9090-4
Eshaq RS, Wright WS, Harris NR (2014) Oxygen delivery, consumption, and conversion to reactive oxygen species in experimental models of diabetic retinopathy. Redox Biol 2:661–666. https://doi.org/10.1016/j.redox.2014.04.006
Kahya MC, Nazıroğlu M, Övey İS (2017) Modulation of diabetes-induced oxidative stress, apoptosis, and Ca2+ entry through TRPM2 and TRPV1 channels in dorsal root Ganglion and hippocampus of diabetic rats by melatonin and selenium. Mol Neurobiol 54(3):2345–2360. https://doi.org/10.1007/s12035-016-9727-3
Park J, Kim H, Park SY et al (2014) Tonicity-responsive enhancer binding protein regulates the expression of aldose reductase and protein kinase C δ in a mouse model of diabetic retinopathy. Exp Eye Res 122:13–19. https://doi.org/10.1016/j.exer.2014.03.001
Tang WH, Cheng WT, Kravtsov GM et al (2010) Cardiac contractile dysfunction during acute hyperglycemia due to impairment of SERCA by polyol pathway-mediated oxidative stress. Am J Physiol Cell Physiol 299(3):C643–C653. https://doi.org/10.1152/ajpcell.00137.2010
Mahmoud AM, Abd El-Twab SM, Abdel-Reheim ES (2017) Consumption of polyphenol-rich Morus alba leaves extract attenuates early diabetic retinopathy: the underlying mechanism. Eur J Nutr 56(4):1671–1684. https://doi.org/10.1007/s00394-016-1214-0
Al-Kharashi AS (2018) Role of oxidative stress, inflammation, hypoxia and angiogenesis in the development of diabetic retinopathy. Saudi J Ophthalmol 32(4):318–323. https://doi.org/10.1016/j.sjopt.2018.05.002
Nazıroğlu M, Dikici DM, Dursun S (2012) Role of oxidative stress and Ca2+ signaling on molecular pathways of neuropathic pain in diabetes: focus on TRP channels. Neurochem Res 37(10):2065–2075. https://doi.org/10.1007/s11064-012-0850-x
Koivisto AP, Belvisi MG, Gaudet R, Szallasi A. (2021) Advances in TRP channel drug discovery: from target validation to clinical studies. Nat Rev Drug Discov 2021 15:1–19. Epub ahead of print. https://doi.org/10.1038/s41573-021-00268-4
Hara Y, Wakamori M, Ishii M et al (2002) LTRPC2 Ca2+-permeable channel activated by changes in redox status confers susceptibility to cell death. Mol Cell 9(1):163–173. https://doi.org/10.1016/s1097-2765(01)00438-5
Nazıroğlu M, Lückhoff A (2008) A calcium influx pathway regulated separately by oxidative stress and ADP-Ribose in TRPM2 channels: single channel events. Neurochem Res 33(7):1256–1262. https://doi.org/10.1007/s11064-007-9577-5
Uchida K, Tominaga M (2014) The role of TRPM2 in pancreatic β-cells and the development of diabetes. Cell Calcium 56(5):332–339. https://doi.org/10.1016/j.ceca.2014.07.001
Yosida M, Dezaki K, Uchida K et al (2014) Involvement of cAMP/EPAC/TRPM2 activation in glucose- and incretin-induced insulin secretion. Diabetes 63(10):3394–3403. https://doi.org/10.2337/db13-1868
Sözbir E, Nazıroğlu M (2016) Diabetes enhances oxidative stress-induced TRPM2 channel activity and its control by N-acetylcysteine in rat dorsal root ganglion and brain. Metab Brain Dis 31(2):385–393. https://doi.org/10.1007/s11011-015-9769-7
Saadane A, Du Y, Thoreson WB et al (2021) Photoreceptor cell calcium dysregulation and calpain activation promote pathogenic photoreceptor oxidative stress and inflammation in prodromal diabetic retinopathy. Am J Pathol 191(10):1805–1821. https://doi.org/10.1016/j.ajpath.2021.06.006
Shoorei H, Khaki A, Khaki AA, Hemmati AA, Moghimian M, Shokoohi M (2019) The ameliorative effect of carvacrol on oxidative stress and germ cell apoptosis in testicular tissue of adult diabetic rats. Biomed Pharmacother 111:568–578. https://doi.org/10.1016/j.biopha.2018.12.054
Custódio JB, Ribeiro MV, Silva FS, Machado M, Sousa MC (2011) The essential oils component p-cymene induces proton leak through Fo-ATP synthase and uncoupling of mitochondrial respiration. J Exp Pharmacol 3:69–76. https://doi.org/10.2147/JEP.S16387
Gatica S, Eltit F, Santibanez JF, Varela D, Cabello-Verrugio C, Simon F (2019) (2019) Expression suppression and activity inhibition of TRPM7 regulate cytokine production and multiple organ dysfunction syndrome during endotoxemia: a new target for sepsis. Curr Mol Med 19(8):547–559. https://doi.org/10.2174/1566524019666190709181726
Deng W, Lu H, Teng J (2013) Carvacrol attenuates diabetes-associated cognitive deficits in rats. J Mol Neurosci 51(3):813–819. https://doi.org/10.1007/s12031-013-0069-6
Arkali G, Aksakal M, Kaya ŞÖ (2021) Protective effects of carvacrol against diabetes-induced reproductive damage in male rats: modulation of Nrf2/HO-1 signalling pathway and inhibition of Nf-kB-mediated testicular apoptosis and inflammation. Andrologia 53(2):e13899. https://doi.org/10.1111/and.13899
Hong DK, Choi BY, Kho AR et al (2018) Carvacrol attenuates hippocampal neuronal death after global cerebral ischemia via inhibition of transient receptor potential melastatin 7. Cells 7(12):231. https://doi.org/10.3390/cells7120231
Xie P, Fujii I, Zhao J, Shinohara M, Matsukura M (2012) A novel polysaccharide compound derived from algae extracts protects retinal pigment epithelial cells from high glucose-induced oxidative damage in vitro. Biol Pharm Bull 35(9):1447–1453. https://doi.org/10.1248/bpb.b110706
Li H, Li R, Wang L, Liao D, Zhang W, Wang J (2021) Proanthocyanidins attenuate the high glucose-induced damage of retinal pigment epithelial cells by attenuating oxidative stress and inhibiting activation of the NLRP3 inflammasome. J Biochem Mol Toxicol 35(9):e22845. https://doi.org/10.1002/jbt.22845
Meléndez García R, Arredondo Zamarripa D, Arnold E et al (2016) Prolactin protects retinal pigment epithelium by inhibiting sirtuin 2-dependent cell death. EBioMedicine 7:35–49. https://doi.org/10.1016/j.ebiom.2016.03.048
Özkaya D, Nazıroğlu M (2021) Bevacizumab induces oxidative cytotoxicity and apoptosis via TRPM2 channel activation in retinal pigment epithelial cells: Protective role of glutathione. Graefes Arch Clin Exp Ophthalmol 259(6):1539–1554. https://doi.org/10.1007/s00417-021-05074-7
Özkaya D, Shu X, Nazıroğlu M (2021) Deletion of mitochondrial translocator protein (TSPO) gene decreases oxidative retinal pigment epithelial cell death via modulation of TRPM2 channel. Biology (Basel) 10(5):382. https://doi.org/10.3390/biology10050382
Chenet AL, Duarte AR, de Almeida FJS, Andrade CMB, de Oliveira MR (2019) Carvacrol depends on heme oxygenase-1 (HO-1) to exert antioxidant, anti-inflammatory, and mitochondria-related protection in the human neuroblastoma SH-SY5Y cells line exposed to hydrogen peroxide. Neurochem Res. 44(4):884–896. https://doi.org/10.1007/s11064-019-02724-5
McHugh D, Flemming R, Xu SZ, Perraud AL, Beech DJ (2003) Critical intracellular Ca2+ dependence of transient receptor potential melastatin 2 (TRPM2) cation channel activation. J Biol Chem 278(13):11002–11006. https://doi.org/10.1074/jbc.M210810200
Özkaya D, Nazıroğlu M, Vanyorek L, Muhamad S (2021) Involvement of TRPM2 channel on hypoxia-induced oxidative injury, inflammation, and cell death in retinal pigment epithelial cells: modulator action of selenium nanoparticles. Biol Trace Elem Res 199(4):1356–1369. https://doi.org/10.1007/s12011-020-02556-3
Bejarano I, Espino J, Marchena AM et al (2011) Melatonin enhances hydrogen peroxide-induced apoptosis in human promyelocytic leukaemia HL-60 cells. Mol Cell Biochem 353(1–2):167–176. https://doi.org/10.1007/s11010-011-0783-8
Kalyanaraman B, Darley-Usmar V, Davies KJ et al (2012) Measuring reactive oxygen and nitrogen species with fluorescent probes: challenges and limitations. Free Radic Biol Med 52(1):1–6. https://doi.org/10.1016/j.freeradbiomed.2011.09.030
Sivandzade F, Bhalerao A, Cucullo L. (2019) Analysis of the mitochondrial membrane potential using the cationic JC-1 dye as a sensitive fluorescent probe. Bio Protoc. 9(1): e3128. https://doi.org/10.21769/BioProtoc
Özkaya D, Nazıroğlu M, Armağan A et al (2011) Dietary vitamin C and E modulates oxidative stress induced-kidney and lens injury in diabetic aged male rats through modulating glucose homeostasis and antioxidant systems. Cell Biochem Funct 29(4):287–293
Chang YS, Lin CF, Wu CL et al (2011) Mechanisms underlying benzyl alcohol cytotoxicity (triamcinolone acetonide preservative) in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 52(7):4214–4222. https://doi.org/10.1167/iovs.10-6058
Lin YC, Shen ZR, Song XH, Liu X, Yao K (2018) Comparative transcriptomic analysis reveals adriamycin-induced apoptosis via p53 signaling pathway in retinal pigment epithelial cells. J Zhejiang Univ Sci B 19(12):895–909. https://doi.org/10.1631/jzus.B1800408
Song J, Lee SC, Kim SS et al (2004) Zn2+-induced cell death is mediated by the induction of intracellular ROS in ARPE-19 cells. Curr Eye Res 28(3):195–201. https://doi.org/10.1076/ceyr.28.3.195.26251
Nazıroğlu M (2007) New molecular mechanisms on the activation of TRPM2 channels by oxidative stress and ADP-ribose. Neurochem Res 32(11):1990–2001
Perraud AL, Fleig A, Dunn CA et al (2001) ADP-ribose gating of the calcium-permeable LTRPC2 channel revealed by Nudix motif homology. Nature 411(6837):595–599. https://doi.org/10.1038/35079100
Han D, Wu X, Liu L, Shu W, Huang Z (2018) Sodium tanshinone IIA sulfonate protects ARPE-19 cells against oxidative stress by inhibiting autophagy and apoptosis. Sci Rep 8(1):15137. https://doi.org/10.1038/s41598-018-33552-2
Nazıroğlu M. (2021) A novel antagonist of TRPM2 and TRPV4 channels: carvacrol. Metab Brain Dis. https://doi.org/10.1007/s11011-021-00887-1
Cui ZW, Xie ZX, Wang BF et al (2015) Carvacrol protects neuroblastoma SH-SY5Y cells against Fe(2+)-induced apoptosis by suppressing activation of MAPK/JNK-NF-κB signaling pathway. Acta Pharmacol Sin 36(12):1426–1436. https://doi.org/10.1038/aps.2015.90
Armağan HH, Nazıroğlu M (2021) Glutathione depletion induces oxidative injury and apoptosis via TRPM2 channel activation in renal collecting duct cells. Chem Biol Interact 334:109306. https://doi.org/10.1016/j.cbi.2020.109306
Belrose JC, Xie YF, Gierszewski LJ, MacDonald JF, Jackson MF (2012) Loss of glutathione homeostasis associated with neuronal senescence facilitates TRPM2 channel activation in cultured hippocampal pyramidal neurons. Mol Brain 5:11. https://doi.org/10.1186/1756-6606-5-11
Baser KHC (2008) Biological and pharmacological activities of carvacrol and carvacrol bearing essential oils. Curr Pharm Des 14:3106–3120
Lyu Q, Ludwig IS, Kooten PJS, Sijts AJAM, Rutten VPMG, van Eden W, Broere F (2020) Leucinostatin acts as a co-inducer for heat shock protein 70 in cultured canine retinal pigment epithelial cells. Cell Stress Chaperones 25(2):235–243. https://doi.org/10.1007/s12192-019-01066-z
Li Y, Mai Y, Qiu X et al (2020) Effect of long-term treatment of Carvacrol on glucose metabolism in Streptozotocin-induced diabetic mice. BMC Complement Med Ther 20(1):142. https://doi.org/10.1186/s12906-020-02937-0
Kaymaz A, Ulaş F, Çetinkaya A, Erimşah S (2021) Investigating the effects of carvacrol in rats using oxygen-induced retinopathy model. Indian J Ophthalmol 69(5):1219–1223. https://doi.org/10.4103/ijo.IJO_1935_20
Acknowledgements
The authors would like to thank Dr. Xinhua Shu for his valuable contributions to preparation of ARPE19 cells.
Funding
The study was performed with a financial support of the company (BSN Health) (Project No: 2021–03. Project owner: Dr. Hatice Daldal).
Author information
Authors and Affiliations
Contributions
H Daldal: The design, data analyses, manuscript preparation, conception, and critical revision of present study. M. Nazıroğlu: The analyses and preparation of figures in the manuscript. The manuscript submission was approved by both authors.
Corresponding author
Ethics declarations
Ethical approval
Samples from human participants and experimental animals were not used in the present study by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Daldal, H., Nazıroğlu, M. Carvacrol protects the ARPE19 retinal pigment epithelial cells against high glucose-induced oxidative stress, apoptosis, and inflammation by suppressing the TRPM2 channel signaling pathways. Graefes Arch Clin Exp Ophthalmol 260, 2567–2583 (2022). https://doi.org/10.1007/s00417-022-05731-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05731-5