Abstract
Background and purpose
Randomized controlled trials have demonstrated that mechanical thrombectomy (MT) could provide more benefit than standard medical care for acute ischemic stroke (AIS) patients due to emergent large vessel occlusion. However, most primary stroke centers (PSCs) are unable to perform MT, and MT can only be performed in comprehensive stroke centers (CSCs) with on-site interventional neuroradiologic services. Therefore, there is an ongoing debate regarding whether patients with suspected AIS should be directly admitted to CSCs or secondarily transferred to CSCs from PSCs. This meta-analysis was aimed to investigate the two transportation paradigms of direct admission and secondary transfer, which one could provide more benefit for AIS patients treated with MT.
Methods
We conducted a systematic review and meta-analysis through searching PubMed, Embase and the Cochrane Library database up to March 2020. Primary outcomes are as follows: symptomatic intracerebral hemorrhage (sICH) within 7 days; favorable functional outcome at 3 months; mortality in hospital; mortality at 3 months; and successful recanalization rate.
Results
Our pooled results showed that patients directly admitted to CSCs had higher chances of achieving a favorable functional outcome at 3 months than those secondarily transferred to CSCs (OR = 1.26; 95% CI, 1.12–1.42; P < 0.001). In addition, no significant difference was found between the two transportation paradigms in the rate of sICH (OR = 0.86; 95% CI, 0.62–1.18; P = 0.35), mortality in hospital (OR = 0.84; 95% CI, 0.51–1.39; P = 0.51), mortality at 3 months (OR = 1.01; 95% CI, 0.85–1.21; P = 0.91), and successful recanalization (OR = 1.03; 95% CI, 0.88–1.20; P = 0.74). However, in the 100% bridging thrombolysis usage rate subgroup, our subgroup analysis indicated that no difference was found in any outcome between the two transportation paradigms.
Conclusion
Patients with AIS directly admitted to CSCs for MT may be a feasible transportation paradigm for AIS patients. However, more large-scale randomized prospective trials are required to further investigate this issue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2015, five randomized controlled trials demonstrated that patients with acute ischemic stroke (AIS) treated by mechanical thrombectomy (MT) had higher chances of achieving a favorable functional outcome at 3 months than those treated by standard medical care with recombinant tissue plasminogen activator (tPA) [1,2,3,4,5]. A subsequent meta-analysis conducted by HERMES (Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials) collaboration, which pooled individual data for 1287 patients of the above five trials, further confirmed that, in comparison to the standard medical care, MT could significantly reduce the disability rate of AIS patients caused by proximal large vessel occlusion, irrespective of patients demographics or geographical positions [6]. However, it should be noted that most primary stroke centers (PSCs) are unable to perform MT, and MT is usually performed only in comprehensive stroke centers (CSCs) which could provide on-site interventional neuroradiologic services. Currently, there are two main transportation paradigms for patients with a suspected stroke. One is that patients are directly admitted to the nearest PSCs and secondarily transferred to CSCs for MT. Another is that patients are directly admitted to CSCs with on-site thrombectomy capacity, and bypassing the nearest PSCs. However, there is an ongoing debate about which transportation paradigm could provide more benefit for AIS patients. In recent years, some retrospective studies have been performed to investigate this issue. However, results from them are not consistent. Therefore, we conducted this systematic review and meta-analysis of published studies to investigate which transportation paradigm could provide more benefit for AIS patients treated with MT.
Methods
This meta-analysis was conducted according to the recommendations of the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [7].
Literature search
Two reviewers (Weisong Zhao and Pengju Ma) independently searched the PubMed, Embase and Cochrane Library databases up to March 2020, using the following broad search terms: stroke, direct, admission, secondary, transfer, mothership, drip and ship, and thrombectomy. The detailed search terms in PubMed can be found in the supplemental file. In addition, the references of all studies included in this meta-analysis were manually searched to identify other potentially eligible studies. Any disagreement during the literature search process was addressed through a full discussion with a third reviewer (Xuejing Yue).
Outcomes and study selection
Primary outcomes of this meta-analysis include symptomatic intracerebral hemorrhage (sICH) within 7 days; favorable functional outcome at 3 months (defined as a modified Rankin scale (mRS) score of 0–2); mortality in hospital; mortality at 3 months; and successful recanalization (defined as modified Thrombolysis in Cerebral Infarction (mTICI) ≥ 2b). Two reviewers (Weisong Zhao and Jinbao Chen) independently screened all titles/abstracts first, and then read the full text for possible eligibility. Any disagreement during the study selection process was resolved through a full discussion with a third reviewer (Xuejing Yue). Studies were included in our meta-analysis if they met the following criteria: (a) retrospective or prospective studies; (b) AIS patients are divided into two groups, one group is that patients are directly admitted to the nearest PSCs and secondarily transferred to CSCs for performing MT, another group is that patients are directly admitted to CSCs for performing MT; (c) at least one pre-established outcome was reported. Studies were excluded if they met the following criteria: (a) non-English language; (b) reviews, conference abstracts, unrelated studies, and case reports; (c) different studies using the same database; (d) AIS patients received thrombolytic therapy only.
Data extraction and quality assessment
For each study, two reviewers (Weisong Zhao and Jinbao Chen) independently extracted the following baseline characteristics: first author, published year, age, admission National Institutes of Health Stroke Scale (NIHSS) score, study design, devices used for MT, time of symptoms onset to thrombolysis (OTT), time of symptoms onset to groin puncture (OTP), time of symptoms onset to successful reperfusion (OTR), patients recruitment period, vascular occlusion sites. In addition, the rate of intravenous thrombolysis (IVT) prior to performing MT (bridging thrombolysis) was also extracted. Two reviewers (Weisong Zhao and Pengju Ma) independently used the Newcastle–Ottawa Scale (NOS) to evaluate the quality of each study, with a NOS score ≥ 7 points, suggesting high quality. If there was any discrepancy during the above processes, a consensus was reached through consulting a third reviewer (Xuejing Yue).
Statistical analysis
The statistical software “Review Manager 5.3” was used to perform all statistical analyses. The odds ratios (ORs) and corresponding 95% confidence intervals (CIs) of each outcome were calculated. The heterogeneity across all studies was assessed by I2 statistics. I2 > 50% suggested the existence of significant heterogeneity, and a random-effects model was subsequently used to pool the estimates of each comparison. A fixed-effects model was used when I2 < 50%. Publication bias was evaluated using visual funnel plots. Furthermore, subgroup analysis was conducted according to the bridging thrombolysis usage rate in each study (100% VS. non-100%).
Results
Study selection and study characteristics
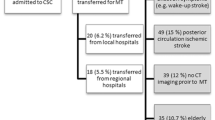
A total of 624 potentially eligible studies for this meta-analysis were initially identified through searching electronic databases, among them 76 were excluded because they were duplicates. After screening the titles/abstracts of the remaining 548 studies, 522 were further excluded because they were reviews, letters, conference abstracts, case reports, and unrelated studies. And then, 26 studies were eligible for full-text review, of which 19 studies contained available data and were finally included in our meta-analysis [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. A flow chart demonstrating the study selection process was shown in supplemental Fig. 1. Among the 19 studies, 13 studies reported the devices used for MT [9,10,11,12,13,14, 17, 18, 20, 23,24,25,26], mainly the new-generation devices such as “stent retriever” and “a direct aspiration first pass technique” (ADAPT). 17 studies reported the sites of the vascular occlusion [8,9,10,11,12,13,14,15,16,17,18,19,20, 22,23,24,25], of which 9 studies included a small portion of AIS patients due to the posterior circulation artery occlusion [8, 9, 12, 15, 18, 19, 22,23,24]. The baseline characteristics and outcomes of each study were shown in Table 1, supplemental Table 1 and supplemental Table 2. The visual funnel plots suggested that no significant publication bias was found across the 19 studies (Supplemental Figs 2, 3, 4, 5 and 6). In addition, the NOS scores indicated a moderate and high quality of most included studies, with a NOS score ranged from 6 to 8 (Supplemental Table 2).
Symptomatic intracerebral hemorrhage (sICH)
Thirteen studies involving 3857 patients provided information about sICH within 7 days. A fixed-effects model was used to pool the results because no significant heterogeneity was found across the thirteen studies. The pooled results indicated that there was no significant difference in the rate of sICH between the direct admission group and the secondary transfer group (OR = 0.86; 95% CI, 0.62–1.18; P = 0.35) (Fig. 1).
Favorable functional outcome at 3 months (mRS ≤ 2)
Sixteen studies involving 5258 patients reported the information about favorable functional outcome at 3 months. No significant heterogeneity was detected across the sixteen studies, and we used a fixed-effects model to pool the results. The pooled results showed that directly admitted patients had higher chances of achieving a favorable functional outcome at 3 months compared with those secondarily transferred to CSCs (OR = 1.26; 95% CI, 1.12–1.42; P < 0.001) (Fig. 2).
Mortality in hospital and at 3 months
Fourteen studies reported the information on mortality, among them, four studies reported mortality in hospital, eight studies reported mortality at 3 months, and two studies reported the mortality both in hospital and at 3 months. For the outcome of mortality in hospital, the pooled results of six studies indicated that there was no significant difference between the direct admission group and the secondary transfer group (OR = 0.84; 95% CI, 0.51–1.39; P = 0.51) (Fig. 3). A random-effects model was used to pool the results since substantial heterogeneity was detected across the six studies. In addition, similar results were also found in mortality at 3 months (OR = 1.01; 95% CI, 0.85–1.21; P = 0.91) (Fig. 4), with no substantial heterogeneity was detected across the ten studies.
Successful recanalization rate
Fifteen studies reported information about the successful recanalization rate. A fixed-effects model was used to pool the results because none significant heterogeneity was detected across the fifteen studies. Our pooled results indicated that there was no significant difference in the rate of successful recanalization between the direct admission group and the secondary transfer group (OR = 1.03; 95% CI, 0.88–1.20; P = 0.74) (Fig. 5).
Subgroup analysis according to the rate of IVT prior to performing MT
Among the nineteen studies included in this meta-analysis, a total of five studies reported 100% bridging thrombolysis usage rate. In the non-100% bridging thrombolysis usage rate subgroup, the pooled results of subgroup analysis were consistent with previous analyses in the rate of sICH, mortality at 3 months, and successful recanalization between the direct admission group and the secondary transfer group (Supplemental Figs. 7, 8, 9). Meanwhile, in the non-100% bridging thrombolysis usage rate subgroup, patients had higher chances of achieving a favorable functional outcome at 3 months in direct admission group than that in secondary transfer group, which was also consistent with previous analysis (OR = 1.27; 95% CI, 1.10–1.46; P = 0.001) (Supplemental Fig. 10). However, this difference was not statistically significant in the 100% bridging thrombolysis usage rate subgroup, either using a fixed-effects model or a random-effects model (OR = 1.24; 95% CI, 0.99–1.57; P = 0.06) and (OR = 1.18; 95% CI, 0.84–1.67; P = 0.34) (Supplemental Figs. 10, 11).
Discussion
Previously, before the advent of MT, several studies have reported that AIS patients directly admitted to the nearest PSCs to receive IVT with tPA and secondarily transferred to CSCs for postoperative care is a safe paradigm [27,28,29,30]. However, for those patients who meet MT criteria, the secondary transfer will delay the time of performing MT, thus prolonging the reperfusion time, which is a crucial predictor for patients achieving a favorable functional outcome at 3 months.
In the HERMES meta-analysis, the authors found that patients receiving MT and medical therapy within the first 7.3 h after symptoms onset had lower degrees of disability at 3 months compared to those receiving medical therapy alone [31]. However, this benefit became nonsignificant when patients were treated with MT more than 7.3 h after symptoms onset [31]. Similarly, in another study which pooled data from the SWIFT PRIME (Solitaire FR With the Intention for Thrombectomy as Primary Endovascular Treatment for Acute Ischemic Stroke) trial, the authors found that patients receiving MT within the first 2.5 h after symptoms onset had higher chances of achieving a favorable functional outcome at 3 months, but this rate decreased by 10% over the next hour and by 20% with every subsequent hour of delay [32].
This meta-analysis was aimed to evaluate which transportation paradigm could provide more benefit for AIS patients treated with MT. Our pooled results are based on 19 studies totally enrolling 4205 patients directly admitted to CSCs and 4546 patients secondarily transferred to CSCs. According to the primary analysis, the pooled results indicated that the rate of sICH, mortality in hospital, mortality at 3 months, and successful recanalization were not significantly different between the direct admission group and the secondary transfer group. However, partial heterogeneity was detected across some studies, which reduced the accuracy of these results. Difference in the use of devices for MT, inclusion and exclusion criteria of patients in each study, and medical level across hospitals may be the possible resources of this heterogeneity. In addition, our pooled results indicated that patients directly admitted to CSCs had higher chances of achieving a favorable functional outcome at 3 months than those secondarily transferred to CSCs, which could be explained by the difference in the time of OTP and OTR between the two groups. Previously, Froehler et al. reported that AIS patients directly admitted to CSCs had higher chances of achieving a functional independence at 3 months than those patients secondarily transferred to CSCs [13]. However, there was no difference in any outcome between the two groups after adjusting the time from symptoms onset to treatment, suggesting that the difference in the rate of achieving a favorable functional outcome between the two groups was mainly attributable to the time delay of performing MT [13]. According to the baseline characteristics of each study included in this meta-analysis (Table 1), we found that the time of OTP and OTR was significantly shorter in the direct admission group than that in the secondary transfer group. The mean difference in the time of OTP and OTR between the two groups were 92.89 min and 82.38 min, respectively.
Several recent studies have reported that patients receiving bridging thrombolysis before performing MT had lower morality rate and higher chances of achieving a favorable functional outcome at 3 months than those patients treated with MT alone [33,34,35]. It is possible that the difference in the rate of bridging thrombolysis usage in each study could affect the outcomes of AIS patients after performing MT. Therefore, we conducted a subgroup analysis according to the utilization rate of the bridging thrombolysis in each study (100% VS. non-100%). Interestingly, in the 100% bridging thrombolysis usage rate subgroup, the pooled results showed that there was no difference between the two transportation paradigms in sICH, favorable functional outcome at 3 months, mortality at 3 months, and successful recanalization. We think that implementing intravenous thrombolysis before performing MT could partially compensate for the negative effects caused by the delayed reperfusion time. However, in fact, according to the baseline characteristics of each study included in this meta-analysis, we found that the utilization rate of bridging thrombolysis in most studies are less than 60%. The primary reason is that, in the clinical reality, some AIS patients are not eligible for IVT due to they have a history of intracranial hemorrhage, receive surgical operation recently, use novel oral anticoagulants (NOACs), or have contraindications to tPA [36,37,38]. For those patients with suspected AIS but not eligible for IVT, going directly to the nearest CSCs to perform MT seems to be the best choice.
Although our pooled results indicated that direct admission for AIS patients seems to be superior to secondary transfer, however, this doesn’t mean that all patients with suspected AIS should be directly admitted to CSCs. On the one hand, at present, there is a lack of an accurate and widely used prehospital clinical scale that can screen eligible AIS patients for MT, therefore, too many patients with suspected AIS directly admitted to CSCs may beyond the capacity of CSCs and strain the medical resources [39]. On the other hand, the distribution of CSCs in rural areas are much less than that of urban areas, therefore, the transportation time for patients living in rural areas is longer than those living in urban areas, which may lead some patients beyond the optimal treatment window of IVT, and thus they would inevitably be treated by MT [5, 13]. At present, there is an ongoing randomized controlled trial, RACECAT (Direct Transfer to an Endovascular Center Compared to Transfer to the Closest Stroke Center in Acute Stroke Patients with Suspected Large Vessel Occlusion) (NCT02795962), aiming to investigate which transportation paradigm is more beneficial for patients with suspected large vessel occlusion. We hope the results of RACECAT could provide more information regarding this topic. However, we also think that more large-scale studies are required to further investigate this topic, in particular, focusing on how to manage patients from rural areas and urban areas separately. As we know, different areas have different medical systems, therefore; for patients from different regions, different transportation paradigms may be required. In addition, it is also urgent to develop some accurate prehospital clinical scales that can screen eligible patients for MT, thus helping clinicians to make the best prehospital triage decision for patients with suspected AIS and helping to use the limited medical resources rationally [40, 41].
The following limitations regarding this meta-analysis have to be considered. First, most studies included in this meta-analysis are retrospective design. Second, many baseline characteristics are missing, which might introduce information bias. Third, different regions such as metropolitan areas and rural areas have different medical level, especially in PSCs, which could also affect the pooled results. Fourth, the results from subgroup analysis may be not accurate since only 5 studies with small samples were included in the 100% bridging therapy usage rate subgroup. Further studies should be conducted to investigate the difference between the two transportation paradigms in patients eligible for IVT and not eligible for IVT, respectively.
Conclusions
Our primary pooled results indicated that patients with suspected AIS directly admitted to CSCs had a better outcome than those secondarily transferred to CSCs from PSCs. However, subgroup analysis indicated that there was no difference in any outcome between the two transportation paradigms in the 100% bridging thrombolysis usage rate subgroup. Due to several limitations of this meta-analysis, more large-scale randomized prospective trials are required to further investigate this topic.
References
Berkhemer OA et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. New England J Med 372:11–20. https://doi.org/10.1056/NEJMoa1411587
Campbell BCV et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. New England J Med 372:1009–1018. https://doi.org/10.1056/NEJMoa1414792
Goyal M et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. New England J Med 372:1019–1030. https://doi.org/10.1056/NEJMoa1414905
Saver JL et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. New England J Med 372:2285–2295. https://doi.org/10.1056/NEJMoa1415061
Jovin TG et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. New England J Med 372:2296–2306. https://doi.org/10.1056/NEJMoa1503780
Goyal M et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet (London, England) 387:1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Adams KM et al (2019) Outcomes after Thrombectomy in Belfast: Mothership and Drip-and-Ship in the Real World. Cerebrovasc Dis 47:231–237. https://doi.org/10.1159/000500849
Asaithambi G et al (2018) Real-world treatment of large vessel occlusions: combined outcomes of directly presenting and transferred-in patients to a stroke center. Neurol Res 40:637–643. https://doi.org/10.1080/01616412.2018.1460700
Barlinn J et al (2017) Acute endovascular treatment delivery to ischemic stroke patients transferred within a telestroke network: a retrospective observational study. Int J Stroke 12:502–509. https://doi.org/10.1177/1747493016681018
Bücke P et al (2018) Endovascular Thrombectomy in Acute Ischemic Stroke: Outcome in Referred Versus Directly Admitted Patients. Clin Neuroradiol 28:235–244. https://doi.org/10.1007/s00062-017-0558-z
Feil K et al (2020) Drip and ship for mechanical thrombectomy within the Neurovascular Network of Southwest Bavaria. Neurology 94:e453–e463. https://doi.org/10.1212/WNL.0000000000008753
Froehler MT et al (2017) Interhospital Transfer Before Thrombectomy Is Associated With Delayed Treatment and Worse Outcome in the STRATIS Registry (Systematic Evaluation of Patients Treated With Neurothrombectomy Devices for Acute Ischemic Stroke). Circulation 136:2311–2321. https://doi.org/10.1161/circulationaha.117.028920
Gerschenfeld G et al (2017) Two Paradigms for Endovascular Thrombectomy After Intravenous Thrombolysis for Acute Ischemic Stroke. JAMA Neurol 74:549–556. https://doi.org/10.1001/jamaneurol.2016.5823
Hiyama N et al (2016) Safety and effectiveness of drip, ship, and retrieve paradigm for acute ischemic stroke: A single center experience. Neurol Med Chir 56:731–736. https://doi.org/10.2176/nmc.oa.2016-0102
Jayaraman MV et al (2020) Field triage for endovascular stroke therapy: a population-based comparison. J Neurointervent Surg 12:233–239. https://doi.org/10.1136/neurintsurg-2019-015033
Drip PMS et al (2016) ship, and on-demand endovascular therapy for acute ischemic stroke. PLoS ONE. https://doi.org/10.1371/journal.pone.0150668
Prothmann S et al (2017) Acute Recanalization of Thrombo-Embolic Ischemic Stroke with pREset (ARTESp): the impact of occlusion time on clinical outcome of directly admitted and transferred patients. J Neurointervent Surg 9:817–822. https://doi.org/10.1136/neurintsurg-2016-012556
Rinaldo L et al (2017) Hospital transfer associated with increased mortality after endovascular revascularization for acute ischemic stroke. J Neurointervent Surg 9:1166–1172. https://doi.org/10.1136/neurintsurg-2016-012824
Sarraj A et al (2019) Outcomes of thrombectomy in transferred patients with ischemic stroke in the late window: A subanalysis from the defuse 3 trial. JAMA Neurol 76:682–689. https://doi.org/10.1001/jamaneurol.2019.0118
Seker F et al (2019) Direct Admission vs. Secondary Transfer to a Comprehensive Stroke Center for Thrombectomy: Retrospective Analysis of a Regional Stroke Registry with 2797 Patients. Clin Neuroradiol. https://doi.org/10.1007/s00062-019-00842-9
Shigeta K et al (2019) Widening time disparities between two paradigms: tama-registry of acute endovascular thrombectomy. J Stroke Cerebrovascular Dis 28:1267–1273. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.01.021
Van Veenendaal P et al (2018) Endovascular clot retrieval by hub-and-spoke service delivery is feasible compared with direct-to-mothership. Cerebrovasc Dis 46:170–175. https://doi.org/10.1159/000490421
Weber R et al (2016) Outcome and periprocedural time management in referred versus directly admitted stroke patients treated with thrombectomy. Therapeut Adv Neurol Dis 9:79–84. https://doi.org/10.1177/1756285615617081
Weisenburger-Lile D et al (2019) Direct admission versus secondary transfer for acute stroke patients treated with intravenous thrombolysis and thrombectomy: Insights from the endovascular treatment in ischemic stroke registry. Cerebrovasc Dis 47:112–120. https://doi.org/10.1159/000499112
Saver JL et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs t-PA alone in stroke. New England J Med 372:2285–2295. https://doi.org/10.1056/NEJMoa1415061
Mansoor S, Zand R, Al-Wafai A, Wahba MN, Giraldo EA (2013) Safety of a "drip and ship" intravenous thrombolysis protocol for patients with acute ischemic stroke. J Stroke Cerebrovasc Dis 22:969–971. https://doi.org/10.1016/j.jstrokecerebrovasdis.2011.12.010
Qureshi AI et al (2012) Outcome of the 'Drip-and-Ship' Paradigm among Patients with Acute Ischemic Stroke: Results of a Statewide Study. Cerebrovasc Diseases Extra 2:1–8
Silverman IE, Beland DK, Chhabra J, McCullough LD (2005) The, "drip-and-ship" approach: starting IV t-PA for acute ischemic stroke at outside hospitals prior to transfer to a regional stroke center. Conn Med 69:613–620
Tekle WG et al (2012) Drip-and-ship thrombolytic treatment paradigm among acute ischemic stroke patients in the United States. Stroke 43:1971–1974. https://doi.org/10.1161/STROKEAHA.112.657817
Saver JL et al (2016) Time to Treatment With Endovascular Thrombectomy and Outcomes From Ischemic Stroke: A Meta-analysis. JAMA 316:1279–1288. https://doi.org/10.1001/jama.2016.13647
Goyal M et al (2016) Analysis of Workflow and Time to Treatment and the Effects on Outcome in Endovascular Treatment of Acute Ischemic Stroke: Results from the SWIFT PRIME Randomized Controlled Trial. Radiology 279:888–897. https://doi.org/10.1148/radiol.2016160204
Fan L et al (2020) Outcomes of mechanical thrombectomy with pre-intravenous thrombolysis: a systematic review and meta-analysis. J Neurol. https://doi.org/10.1007/s00415-020-09778-4
Mistry EA et al (2017) Mechanical Thrombectomy Outcomes With and Without Intravenous Thrombolysis in Stroke Patients: A Meta-Analysis. Stroke 48:2450–2456. https://doi.org/10.1161/STROKEAHA.117.017320
Broeg-Morvay A et al (2016) Direct Mechanical Intervention Versus Combined Intravenous and Mechanical Intervention in Large Artery Anterior Circulation Stroke: A Matched-Pairs Analysis. Stroke 47:1037–1044. https://doi.org/10.1161/STROKEAHA.115.011134
Whiteley WN et al (2016) Risk of intracerebral haemorrhage with alteplase after acute ischaemic stroke: a secondary analysis of an individual patient data meta-analysis. Lancet Neurol 15:925–933. https://doi.org/10.1016/s1474-4422(16)30076-x
Lees KR et al (2010) Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 375:1695–1703. https://doi.org/10.1016/s0140-6736(10)60491-6
Jansen IGH, Mulder M, Goldhoorn RB (2018) Endovascular treatment for acute ischaemic stroke in routine clinical practice: prospective, observational cohort study (MR CLEAN Registry). BMJ Clin Res. https://doi.org/10.1136/bmj.k949
van Meenen LCC et al (2020) Interhospital transfer vs direct presentation of patients with a large vessel occlusion not eligible for IV thrombolysis. J Neurol. https://doi.org/10.1007/s00415-020-09812-5
Rodríguez-Pardo J et al (2020) Prehospital selection of thrombectomy candidates beyond large vessel occlusion: M-DIRECT scale. Neurology. https://doi.org/10.1212/WNL.0000000000008998
Turc G (2017) Mothership or drip-and-ship in the era of thrombectomy: can we use prehospital clinical scales as a compass? Eur J Neurol 24:543–544. https://doi.org/10.1111/ene.13261
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Weisong Zhao and Pengju Ma: literature search, data analysis, interpretation of the data, drafting and revision of the manuscript. Jinbao Chen: data analysis, interpretation of the data. Xuejing Yue: interpretation of the data, and critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None declared.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhao, W., Ma, P., Chen, J. et al. Direct admission versus secondary transfer for acute ischemic stroke patients treated with thrombectomy: a systematic review and meta-analysis. J Neurol 268, 3601–3609 (2021). https://doi.org/10.1007/s00415-020-09877-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09877-2