Abstract
Background and Purpose
Stroke networks have been installed to increase access to advanced stroke specific treatments like mechanical thrombectomy (MT). This concept often requires patients to be transferred to a comprehensive stroke center (CSC) offering MT. Do patient referral, transportation, and logistic effort translate into clinical outcomes comparable to patients admitted primarily to the CSC?
Material and Methods
We categorized 112 patients with acute ischemic stroke in the anterior circulation, who received MT at our institution, into primary admissions (A) and referrals from either local (B) or regional (C) hospitals, assessed the clinical outcome, and tested the impact of distance and delay of transportation from the referring remote hospital.
Results
The median time from symptom onset to initial CT was similar in all groups (p = 0,939). Patients who were transferred to the CSC had significantly increasing median time between initial CT and MT (in minutes (interquartile range [IQR]); A: 83 [68–120]; B: 174 [159–208]; C: 220 [181–235]; p < 0.001) and median time between onset to MT (in minutes [IQR]; A: 178 [150–210]; B: 274 [238–349]; C: 293 [256–329]; p < 0.001).
After 90 days of MT there was no significant difference in clinical outcome (modified Rankin Scale ≤ 2) between primary admitted and referred patients (p = 0.502).
Conclusion
Clinical outcome in patients who received MT after transfer from either local or regional remote hospitals was not significantly worse than in patients primarily admitted to the CSC. In the event of an acute ischemic stroke patients living in urban or rural areas should, despite a possible delay, have access to MT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The implementation of stroke networks has been advocated to provide high-quality care in stroke medicine in urban as well as in rural areas [1]. As timely revascularization remains a critical component of acute ischemic stroke (AIS) therapy [2] mainstay of these networks is to increase and accelerate intravenous or intraarterial recanalization therapies. While intravenous thrombolysis (IVT) with recombinant tissue plasminogen activator (rtPA) is widely available in community or primary stroke center hospitals, it has a limited efficacy of only about 30 % in patients with large vessel occlusion (LVO) [3, 4].
Recently randomized, multicenter studies proved safety and efficacy of intraarterial treatment (mechanical thrombectomy, MT) in the setting of LVO [5–9]. Unfortunately, MT is frequently available at comprehensive stroke centers only. Thus eligible patients often require transferal to CSC for MT.
Delay in hospital-to-hospital transfer is a common reason for patients with AIS becoming ineligible for MT. The likelihood of receiving MT decreases rapidly by increasing transfer time [10]. Furthermore delays in hospital-to-hospital transfer reduce the probability of good outcomes among treated patients and recommendations to reduce transfer delays have been issued [11]. A previous study demonstrated that the use of a telemedicine stroke system for remote evaluation of the patient and of acute radiologic imaging studies (e.g., non-enhanced computed tomography (CT) of the brain) before transfer to a stroke center for further treatment was associated with favorable patient outcome [12, 13]. Stroke centers performing more than 50 endovascular interventions for acute stroke per year had significantly better patient outcome [12, 13].
Even within well-established stroke networks, it remains of interest if the efforts of secondary referral, transportation, and logistics translate into clinical outcomes comparable to patients admitted primarily. Here, we assessed the outcome of AIS patients who received MT at our institution and tested the impact of distance and delay of transportation from the referring remote hospital. We hypothesized that patients being transferred from remote either local or regional hospitals have a reduced probability of a good outcome in comparison to patients primarily admitted to the emergency service in-house.
Subjects and Methods
On the basis of a prospectively collected AIS patient cohort undergoing mechanical thrombectomy at our institution between 2006/2010 and 2012/2013 we categorized the following groups: patients who were primarily admitted to our institution (group A); and patients who were transferred from local (group B) or regional (group C) hospitals. Referring hospitals were very heterogeneous in terms of distance to the CSC, with the closest being only nine miles and the farthest being 87 miles away from the CSC. Since there is no international standardized definition of “local” and “regional” the distance of a marathon (42,195 kilometers or 26 miles and 385 yards) was chosen as a parameter to categorize hospitals according to their distance to our institution. Local, mostly urban hospitals were defined by a distance to the CSC of less than or equal to the distance of a marathon (group B). Regional, mostly rural hospitals were defined by a distance to the CSC of more than 42,195 km or 26 miles and 385 yards (group C). Distance was measured by the fastest route from the referring hospital to the CSC by car according to google.maps.
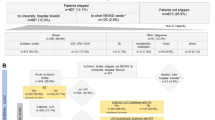
To maximize comparability between our groups we established the following inclusion and exclusion criteria. For this analysis we included only patients with anterior circulation ischemic stroke who had CT imaging before initiation of MT (n = 112). We excluded patients who received MR-imaging prior to MT because of the increased time needed for MR-imaging and the circumstance that these patients were exclusively primary admissions to the CSC. All elderly patients (age ≥ 80 years), who received MT at our institution, were primary admissions. To prevent the analysis from this possible bias, elderly patients were not eligible for this study. Patients with posterior circulation ischemic stroke, patients in whom initiation of therapy could not be accomplished within 8 h from symptom onset or unknown symptom onset (e.g., wake-up strokes) and those with clinical fluctuation of symptoms were excluded as well (Fig. 1).
Stroke Imaging, and Eligibility for Stroke Therapy
Patients with suspected acute ischemic stroke received a standardized stroke imaging protocol including a non-contrast enhanced CT of the brain and a CT angiography in the CSC or at the remote hospitals. If primarily admitted to the CSC, a CT perfusion was performed as well.
Patients were considered eligible for MT by the treating neurointerventionalist at the CSC if initiation of therapy could be accomplished within 8 h of onset, NIHSS score was ≥ 10 on evaluation at the primarily admitting hospital and initial CT of the head excluded hemorrhage or hypodensity more than one-third middle cerebral artery territory or ASPECTS < 6. Patients from referring hospitals were assessed for MT eligibility by same criteria via a telemedicine stroke system prior to a possible transport to the CSC. Mode of transportation (ambulance or helicopter) was chosen upon availability. Repeat brain imaging was performed before angiography to rule out a large infarct core or intracranial hemorrhage.
Use of mechanical and/or pharmacological treatments remained at the discretion of the treating stroke neurologist and neurointerventionalist. IVT eligibility and dosing was based on international standards. Almost exclusively stent retriever devices (e.g., Revive PV, Codman, Raynham, MA, USA; Solitaire Revascularization Device, Covidien, Dublin, Ireland) were used for MT.
Data Collection
Data collection included demographics (age and sex), previous medical history (hypertension, coronary artery disease, congestive heart failure, atrial fibrillation, diabetes mellitus, hypercholesterolemia, history of smoking, and previous stroke), symptom onset time, stroke severity (National Institutes of Health Stroke Scale (NIHSS)), initiation of CT, transportation mode, referring hospital location, start of angiography time, angiographic outcome as by thrombolysis in cerebral infarction score (TICI), and complications. Symptom onset time and patient history was documented according to admission papers at our institution or at the referring hospital. Time of CT and angiography were captured automatically by the CT-scanners and angiography system. Clinical outcome as by modified Rankin Scale (mRS) after 90 days was assessed by an independent stroke neurologist.
Statistical Analysis
We compared data between those patients who were primarily admitted to our institution (group A) versus those who were transferred from a local (group B) or regional (group C) hospital using Pearson χ2-Test and Fisher exact test for categorical variables and ANOVA and Student t Test for continuous variables when applicable. We also performed a univariate analysis to determine relevant continuous variables that could be considered independent predictors of good clinical outcome. Good clinical outcome was defined as mRS90 0–2. Variables with a P-value < 0.20 were entered into a multivariate logistic regression analysis. Odds ratios and 95 % confidence intervals were estimated for predictors of good clinical outcome. P < 0.05 was considered significant in the final model. All statistical analyses were performed using IBM SPSS Statistics 21.0.0.0 (Armonk, NY, USA).
The study was approved by the Institutional Review Board at our hospital.
Results
Between June 1, 2010 and December 31, 2013, 326 patients with AIS received MT at our institution. Two hundred fourteen (65.6 %) patients were excluded from this analysis because of aforementioned criteria (Fig. 1). One hundred twelve (34.4 %) patients were included in this analysis. Seventy-four patients were primarily admitted to the CSC and categorized into group A (22.7 %). Thirty-eight patients were transferred from over 6 local (group B: 20 (6.2 %)) and 11 regional (group C: 18 (5.5 %)) hospitals for intraarterial revascularization therapy.
The mean age of the included patients was 65 ± 13 years and median NIHSS score was 19 (interquartile range [IQR], 15–22). Patients in group A were older than patients from referring regional hospitals (age in years [standard deviation]: A: 67 [11], B: 64 [15], C: 57 [15]; p = 0.025; A vs. B, p = 0.423; A vs. C, p = 0.005; B vs. C, p = 0.172). With the exception of hypertension and coronary artery disease there was no significant difference between the patient groups in terms of sex and medical history including diabetes mellitus, atrial fibrillation, congestive heart failure, hypercholesterolemia, previous stroke, and history of smoking. Hypertension and coronary artery disease were more frequent in patients primarily admitted to the CSC compared to patients referred from regional hospitals (A vs. C: hypertension: p = 0.002; coronary artery disease: p = 0.019). With regards to history of hypercholesterolemia, congestive heart failure, and pre-ictus mRS there was a trend of a decreasing frequency with increasing distance to the CSC. Baseline characteristics of included patients are shown according to their primarily admitting hospital in Table 1.
IV rtPA was administered in 54 patients (73 %) in group A. Fifteen patients (75 %) in group B and 14 patients (77.8 %) in group C received IV rtPA before transfer in a “drip and ship” protocol (p = 0.912). The median distance between group B and group C was significantly different (p < 0.001). Mode of transportation was almost equally distributed between ambulance and helicopter (ambulance [%]; B: 9 [45 %]; C: 11 [61.1 %]; p = 0.080). There was no difference between both transportation modalities with regards to baseline characteristics, time between symptom onset and initial CT, time from initial CT to MT, time between symptom onset and MT and clinical outcome (data not shown). The majority of transferred patients received repeated brain imaging upon arrival at the CSC to confirm eligibility for MT (group B: 18 (90 %); group C: 15 (88.3 %)). We did not observe a case of intracranial hemorrhage or recanalization in referred patients prior to MT.
The median time from symptom onset to initial CT was similar in all groups (in minutes [IQR]; A: 82 [62–116]; B: 84 [61–111]; C: 77 [52–107]; p = 0.939). In comparison between patients who were transferred to the CSC and patients who were primarily admitted to the CSC median time between initial CT and MT was significantly increasing (in minutes [IQR]; A: 83 [68–120]; B: 174 [159–208]; C: 220 [181–235]; A vs. B and A vs. C: p < 0.001; B vs. C: p = 0.109) as well as the median time between onset to MT (in minutes [IQR]; A: 178 [150–210]; B: 274 [238–349]; C: 293 [256–329]; A vs. B and A vs. C: p < 0.001; B vs. C: p = 0.362). However, there was no significant difference between local and regional hospitals for these variables. Angiographic outcome after mechanical thrombectomy was comparable in all groups (TICI 2b/3: p = 0.407).
Routinely performed follow-up exams revealed no significant differences in infarct size (as per ASPECTS on a repeated non-contrast enhanced CT), NIHSS, and occurrence of symptomatic intracranial hemorrhage (sICH) 24 h after MT. Ninety days after the acute ischemic stroke there was no significant difference in clinical outcome between patients who were primarily admitted to the CSC and patients being transferred for MT from local or regional hospitals (mRS 0–2: A = 35.1 %, B = 40 %, C = 50 %; A vs. B: p = 0.794; A vs. C: p = 0.282; B vs. C: p = 0.745).
After a univariate analysis, a multivariate logistic regression model (Table 2) including TICI, diabetes mellitus, NIHSS score, age, prestroke mRS, previous stroke, atrial fibrillation and time to imaging, time to MT, and time between imaging and MT was performed. This analysis revealed TICI 2b/3 as positive and diabetes mellitus, NIHSS and age as negative predictive factors on good clinical outcome in this patient cohort.
Discussion
The efforts of transportation and logistics associated with a secondary referral of patients to undergo MT in a CSC are not negligible. Previous studies could not clarify whether these efforts provide referred patients with the same possibility for a good clinical outcome than primary admissions. We addressed this issue by analyzing patient outcome on the basis of a prospectively collected AIS patient cohort undergoing MT at our institution and determined the probability of a good clinical outcome depending on the primarily admitting hospital. Despite a significant increase in time between onset of symptoms and MT and time between CT imaging and MT, clinical outcome of transferred patients was not significantly worse than clinical outcome of patients primarily admitted to the CSC.
The concept of stroke networks requires patients, who are eligible for MT, to be transferred to a CSC offering this specific treatment. Similar to our findings, a previous study demonstrated that for transferred patients significantly more time passes between onset of symptoms and initiation of MT and between initial imaging and MT compared to patient primarily admitted to the CSC [11]. In our study, transferred patients received MT after 4.5–5 h after stroke onset, compared to 3 h in patients primarily admitted to the CSC. However, no significant difference in recanalization rates as well as NIHSS, ASPECTS, and the occurrence of symptomatic intracranial hemorrhage 24 h after MT was observed between the patient groups. Furthermore, good clinical outcome 90 days after MT was not statistically significant different in primary admissions and transferred patients. These findings stand in contrast to preceding studies in which a delay of MT was associated with significantly worse clinical outcome [11, 14].
The reasons for our findings are complex. IV rtPA as bridging for MT improves recanalization and clinical outcome [15, 16]. Our patient cohort demonstrates comparable IV rtPA administration rates of about 75–80 % within group A, B, and C. In this circumstance, it remains unclear if and to what extent an increased IV rtPA exposure time might have had an additional beneficial effect for transferred patients.
Our findings could be influenced by some sort of selection bias. Patient demographics and medical history are factors which influence recanalization rate, infarct size, and clinical outcome [17–21] and always need to be viewed cautiously. As referred patients tend to be younger and had a lower frequency of hypertension and coronary artery disease, the probability of good clinical outcome might have been altered within this study. Accordingly, the probability of good clinical outcome after MT might be lower in a subset of transferred patients with the similar age and comorbidities like patients primarily admitted to a CSC. The heterogeneity between the patients groups could be the consequence of patient selection. Referring hospitals were not obligated to consult with the CSC in every patient with ischemic stroke and might have contacted the CSC only in patients with favorable demographics and medical history during our study period between 2006/2010 and 2012/2013. However, following the publication of randomized stroke trials evaluating MT [5–9] we are likely to experience an increasing number of referred patients. To what extend these patients are going to have similar age and comorbidities as patients primarily admitted to the CSC needs to be evaluated separately.
The stability of ischemic core volume during the initial hours of acute ischemic stroke [22] could explain similar clinical outcome as well as similar infarction size after MT. A stable ischemic core volume implies a certain degree of additional time for patient transfer during the initial hours of stroke. Nevertheless, recanalization should be achieved as soon as possible and patients eligible for MT need to be transferred to a CSC for definite treatment without further delay.
Angiographic outcome after mechanical thrombectomy (TICI 2b/3) was the only positive predictor for good clinical outcome in our multivariate regression model. This underlines the importance of final recanalization status as the strongest predictor of clinical outcome [17]. Following the results of recently issued interventional stroke trials [5–9] mechanical thrombectomy is going to be increasingly applied and will become standard of care for patients with acute ischemic stroke. In this context, achieving a good final recanalization status will not only be crucial for treatment success, but also a marker for treatment quality.
Limitations
The relatively small cohort of the referred patients limits the value of our findings. Larger patient cohorts might delineate a stronger influence between transfer time and patient outcome after MT.
A potential bias might be given by the aforementioned circumstance that patients who received MRI imaging prior to MT were excluded from this analysis. Advance stroke imaging (e.g. Stroke-MRI) may cause a delay in initiation of MT, however, seems not to have a negativ impact on patient outcome [23]. Under this condition the results of our study might be transferrable for patients who received MRI imaging prior to MT.
Unfortunately, the positive aspects of this analysis must not be transferred to the subset of patients who did not meet the inclusion/exclusion criteria. Patients with posterior ischemic stroke, wake-up stroke, or clinical fluctuation of symptoms might not benefit from an integrated telemedicine stroke system within a high volume CSC because of different underlying pathophysiology and several, sometimes not yet detected variables influencing the outcome of these more complex patients. Because our data refers to patients who underwent MT, our findings could not be transferred to all patients who were admitted from remote hospitals and did not meet criteria for MT at the CSC.
Conclusion
Clinical outcomes of patients who received MT after transfer from local or regional hospitals were not significantly worse than clinical outcomes of patients primarily admitted to a comprehensive stroke center. Although a careful patient selection including patient demographics and medical history is needed, the data from this patient cohort suggest that final recanalization status is the strongest positive predictor of good clinical outcome and patients living in urban or rural areas should, despite a possible delay, have access to MT. However, larger patient cohorts are needed to examine the influence of time and patient characteristics on clinical outcome in detail for patients receiving MT after referral from a remote hospital.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Contributorship Statement
Guarantorship: Johannes Pfaff, Martin Bendszus, and Markus Möhlenbruch had access to all data, supervised data collection and analysis, writing and editing of this manuscript.
Contributorship: Mirko Pham, Christian Herweh, Marcel Wolf, Silvia Schönenberger, and Peter A. Ringleb contributed in data collection, as well as conduct and reporting of this study.
Abbreviations
- AIS:
-
Acute ischemic stroke
- CSC:
-
Comprehensive stroke center
- CT:
-
Computed tomography
- IVT:
-
Intravenous thrombolysis
- mRS:
-
Modified Rankin Scale
- MT:
-
Mechanical thrombectomy
- NIHSS:
-
National Institutes of Health Stroke Scale
- rtPA:
-
Recombinant tissue plasminogen activator
References
Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, Koroshetz W, Marler JR, Booss J, Zorowitz RD, Croft JB, Magnis E, Mulligan D, Jagoda A, O'Connor R, Cawley CM, Connors JJ, Rose-DeRenzy JA, Emr M, Warren M, Walker MD; Brain Attack Coalition. Recommendations for comprehensive stroke centers: a consensus statement from the brain attack coalition. Stroke. 2005;36(7):1597–616.
Saver JL. Time is brain—quantified. Stroke. 2006;37(1):263–6.
na. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581–7.
Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007;38(3):967–73.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM; EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-18.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD; ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-30.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW; MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.
Saver JL, Goyal M, Bonafe A, Diener H-C, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R; SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–95.
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López-Cancio E, Tomasello A, Castaño C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez-Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A; REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–306.
Prabhakaran S, Ward E, John S, Lopes DK, Chen M, Temes RE, Mohammad Y, Lee VH, Bleck TP. Transfer delay is a major factor limiting the use of intra-arterial treatment in acute ischemic stroke. Stroke. 2011;42(6):1626–30.
Sun CH, Nogueira RG, Glenn BA, Connelly K, Zimmermann S, Anda K, Camp D, Frankel MR, Belagaje SR, Anderson AM, Isakov AP, Gupta R. “Picture to puncture”: a novel time metric to enhance outcomes in patients transferred for endovascular reperfusion in acute ischemic stroke. Circulation. 2013;127(10):1139–48.
Pedragosa A, Alvarez-Sabín J, Rubiera M, Rodriguez-Luna D, Maisterra O, Molina C, Brugués J, Ribó M. Impact of telemedicine on acute management of stroke patients undergoing endovascular procedures. Cerebrovasc Dis. 2012;34(5–6):436–42.
Gupta R, Horev A, Nguyen T, Gandhi D, Wisco D, Glenn BA, Tayal AH, Ludwig B, Terry JB, Gershon RY, Jovin T, Clemmons PF, Frankel MR, Cronin CA, Anderson AM, Hussain MS, Sheth KN, Belagaje SR, Tian M, Nogueira RG. Higher volume endovascular stroke centers have faster times to treatment, higher reperfusion rates and higher rates of good clinical outcomes. J Neurointerv Surg. 2013;5(4):294–7.
Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009;73(13):1066–72.
Rubiera M, Ribo M, Pagola J, Coscojuela P, Rodriguez-Luna D, Maisterra O, Ibarra B, Piñeiro S, Meler P, Romero FJ, Alvarez-Sabin J, Molina CA. Bridging intravenous-intra-arterial rescue strategy increases recanalization and the likelihood of a good outcome in nonresponder intravenous tissue plasminogen activator-treated patients: a case-control study. Stroke. 2011;42(4):993–7.
Fjetland L, Kurz KD, Roy S, Kurz MW. Evaluation of the recombinant tissue plasminogen activator pretreatment in acute stroke patients with large vessel occlusions treated with the direct bridging approach. Is it worth the effort? Eur J Neurol. 2015;22(2):322–7.
Nogueira RG, Liebeskind DS, Sung G, Duckwiler G, Smith WS. Predictors of good clinical outcomes, mortality, and successful revascularization in patients with acute ischemic stroke undergoing thrombectomy: pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and multi MERCI trials. Stroke. 2009;40(12):3777–83.
Chandra RV, Leslie-Mazwi TM, Oh DC, Chaudhry ZA, Mehta BP, Rost NS, Rabinov JD, Hirsch JA, González RG, Schwamm LH, Yoo AJ. Elderly patients are at higher risk for poor outcomes after intra-arterial therapy. Stroke. 2012;43(9):2356–61.
Johnson JN, Haussen DC, Elhammady MS, Pao CL, Yavagal DR, Aziz-Sultan MA. Poor outcomes of elderly patients undergoing multimodality intra-arterial therapy for acute ischemic stroke. Clin Neurol Neurosurg. 2014;123:136–41.
Linfante I, Starosciak AK, Walker GR, Dabus G, Castonguay AC, Gupta R, Sun CJ, Martin C, Holloway WE, Mueller-Kronast N, English JD, Malisch TW, Marden FA, Bozorgchami H, Xavier A, Rai AT, Froehler MT, Badruddin A, Nguyen TN, Taqi MA, Abraham MG, Janardhan V, Shaltoni H, Novakovic R, Yoo AJ, Abou-Chebl A, Chen PR, Britz GW, Kaushal R, Nanda A, Issa MA, Nogueira RG, Zaidat OO. Predictors of poor outcome despite recanalization: a multiple regression analysis of the NASA registry. J Neurointerv Surg. 2015 Jan 6. [Epub ahead of print]
Tziomalos K, Spanou M, Bouziana SD, Papadopoulou M, Giampatzis V, Kostaki S, Dourliou V, Tsopozidi M, Savopoulos C, Hatzitolios AI. Type 2 diabetes is associated with a worse functional outcome of ischemic stroke. World J Diabetes. 2014;5(6):939–44.
Finitsis S, Kemmling A, Havemeister S, Thomalla G, Fiehler J, Brekenfeld C. Stability of ischemic core volume during the initial hours of acute large vessel ischemic stroke in a subgroup of mechanically revascularized patients. Neuroradiology. 2014;56(4):325–32.
Sheth KN, Terry JB, Nogueira RG, Horev A, Nguyen TN, Fong AK, Gandhi D, Prabhakaran S, Wisco D, Glenn BA, Tayal AH, Ludwig B, Hussain MS, Jovin TG, Clemmons PF, Cronin C, Liebeskind DS, Tian M, Gupta R. Advanced modality imaging evaluation in acute ischemic stroke may lead to delayed endovascular reperfusion therapy without improvement in clinical outcomes. J J Neurointerv Surg. 2013;5 Suppl 1:i62-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Pfaff, J., Pham, M., Herweh, C. et al. Clinical Outcome After Mechanical Thrombectomy in Non-elderly Patients with Acute Ischemic Stroke in the Anterior Circulation: Primary Admission Versus Patients Referred from Remote Hospitals. Clin Neuroradiol 27, 185–192 (2017). https://doi.org/10.1007/s00062-015-0463-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-015-0463-2