Abstract
During human locomotion, vestibular feedback control is fundamental for maintaining dynamic stability and adapting the gait pattern to external circumstances. Within the supraspinal locomotor network, the cerebellum represents the key site for the integration of vestibular feedback information. The cerebellum is further important for the fine-tuning and coordination of limb movements during walking. The aim of this review article is to highlight the shared structural and functional sensorimotor principles in vestibular and cerebellar locomotion control. Vestibular feedback for the maintenance of dynamic stability is integrated into the locomotor pattern via midline, caudal cerebellar structures (vermis, flocculonodular lobe). Hemispheric regions of the cerebellum facilitate feed-forward control of multi-joint coordination and higher locomotor functions. Characteristic features of the gait disorder in patients with vestibular deficits or cerebellar ataxia are increased levels of spatiotemporal gait variability in the fore-aft and the medio-lateral gait dimension. In the fore-aft dimension, pathologic increases of gait fluctuations critically depend on the locomotion speed and predominantly manifest during slow walking velocities. This feature is associated with an increased risk of falls in both patients with vestibular hypofunction as well as patients with cerebellar ataxia. Pharmacological approaches for the treatment of vestibular or cerebellar gait ataxia are currently not available. However, new promising options are currently tested in randomized, controlled trials (fampridine/FACEG; acetyl-dl-leucine/ALCAT).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maintaining dynamic balance during locomotion, i.e., the ability to return to the default movement pattern after small perturbations, relies on a complex interaction between spinal and supraspinal locomotor networks and sensory feedback cues from the vestibular, visual, and proprioceptive systems. Vestibular feedback is required to adjust the intended movement pattern to internal and external disturbances. Integration of vestibular information into the locomotion pattern takes place via a modulation of vestibulospinal reflexes but also at the supraspinal level, in particular within the cerebellum. Vestibular projections that originate from the vestibular nuclei reach several midline and caudal cerebellar structures, i.e., the nodulus, vermis, flocculus, and paraflocculus. These regions are commonly summarized as the “vestibulocerebellum”. Projections from the vestibulocerebellum go back to the vestibular nuclei, but also reach spinal locomotor centers (via the nuclei ruber, reticularis, and inferior olivary), the basal ganglia and frontal loops as well as oculomotor centers in the brainstem (for overview [25]). The functional significance of the vestibulocerebellum for the control of static postural functions such as head and trunk tilt [4] as well as the regulation of eye movements [11] is well established. The role of the vestibulocerebellum in dynamic postural contexts is less understood. Besides the integration of vestibular information, structures in the hemispheric cerebellum play a major role for the fine-tuning and coordination of motor commands. These coordinative motor functions essentially contribute to the stability during the execution of repetitive locomotion movement patterns.
The aim of this review article is to provide a topodiagnostic overview on the different pathomechanisms underlying the emergence of gait ataxia in patients with vestibular or cerebellar dysfunctions. Special emphasis will be placed on the control of dynamic stability and the risk of falls in these patients.
Features of the ataxic gait disorders in patients with cerebellar ataxia and bilateral vestibular failure
The gait pattern of patients with severe bilateral vestibulopathy (BVP) is characterized by an increased trunk sway, reduced step length, broadened base of support, prolonged double support phases, and increased spatiotemporal gait variability [1, 16]. Similar to this pattern, patients with cerebellar ataxia (CA) typically walk with a reduced step length, broadened base of support, and a high spatiotemporal variability of movements (for overview [10]). Whereas some changes of both gait patterns (e.g., base of support, stride length) most likely reflect unspecific, compensatory strategies for balance restabilization, high spatiotemporal gait variability is considered to be an essential pathologic feature of ataxic gait [10]. Typically, gait variability levels are higher in cerebellar ataxia compared to vestibular gait ataxia. Increased stride-to-stride fluctuations during walking indicate the occurrence of instabilities during the execution of repetitive locomotor commands. Two distinct factors mainly drive a more variable timing and spatial irregularity of the foot placement during walking: (1) a dyscoordination in multi-joint limb movements and (2) a disturbed regulation of a stable upright position during walking that is linked to irregular movement trajectories in recordings of different body segments and of the center of mass.
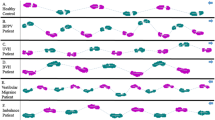
Disturbances of sensory feedback control during walking (regardless of the sensory modality) are tightly linked to increased spatiotemporal gait variability. Thus, several studies found increased stride-to-stride fluctuations to be a typical feature of the walking pattern in patients with either impaired visual feedback, proprioceptive deficits due to sensory neuropathy or in BVP [21, 27, 28]. Earlier studies suggested that the impact of sensory feedback on locomotion control depends on the actual gait velocity and decreases with increasing locomotion speeds [3]. In line with this, it was found that the increase of gait variability in patients with visual, proprioceptive, and vestibular deficits is generally strongest during slow walking modes and gait fluctuations normalize during fast walking (Fig. 1).
Scheme of the speed-dependent impairment of dynamic walking stability: The pattern of sensory ataxia shows increased variability predominantly during slow walking and a tendency to decrease to near-to-normal values at self-selected and fast walking modes. In contrast, the pattern in cerebellar ataxia is characterized by increased gait variability during both slow and fast walking modes. The pattern in patients with predominant vestibulocerebellar disorders (downbeat nystagmus syndrome) or patients with severe proprioceptive disorders (Friedreich’s ataxia) resembles the pattern of sensory ataxia with normal gait fluctuations at fast walking
In patients with CA, both a disturbed integration of sensory feedback cues as well as a dyscoordination of limb movements account for the occurrence of increased gait variability levels. This twofold pathomechanism manifests in a highly irregular gait pattern during both slow and fast walking speeds. On the one hand, increased spatiotemporal gait variability in patients with CA during slow walking most likely reflects an impaired cerebellar integration of sensory feedback cues [21, 26]. On the other hand, cerebellar pacemaker function and feed-forward coordination of multi-joint movements become most prominent during fast walking modes. A dysfunction within these domains presumably accounts for the high spatiotemporal gait variability in patients with CA at fast walking [21]. This idea is further supported by the finding that in patients with CA high limb ataxia scores in the Scale for the Assessment and Rating of Ataxia (SARA) are particularly correlated with increased levels of gait variability during fast walking conditions [16]. In contrast, cerebellar patients with a predominant dysfunction within the vestibulocerebellum, i.e., downbeat nystagmus syndrome (DBN) [19] as well as cerebellar patients with severe proprioceptive impairments, i.e., Friedreich ataxia (unpublished data), have near-to-normal gait fluctuations at fast walking modes.
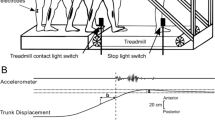
Topodiagnostic aspects in cerebellar gait ataxia
The above discussed twofold impact of cerebellar dysfunction on locomotion control is reflected in the functional structure of cerebellar locomotor centers. Ilg et al. have established the concept of three different functional zones: (I) the midline structures with the vermis and the flocculonodular lobes; (II) the intermediate zones; and (III) the lateral zones of the cerebellar hemispheres. Animal and human lesion studies provide evidence that the structures within the vermis are significantly involved in dynamic balance regulation. Dysfunctions within this region are associated with a disturbance of the gain or duration of long latency reflexes, disturbed rhythmic flexor/extensor muscle activity, and impaired sensorimotor processing that results in maladaptive postural adjustments (for overview [10]). The flocculonodular lobe integrates vestibular afferent information required for motion detection and graviceptive feedback. Several studies have investigated floccular function within the context of oculomotor control. However, its involvement in locomotor control has yet to be determined. A recent study in patients with hypofunction of the flocculus (DBN) provides first evidence that the flocculus essentially mediates vestibular control of dynamic stability during walking [19]. Accordingly, patients with pure floccular hypofunction exhibit a walking pattern comparable to that of patients with BVP with increased walking irregularities predominantly during slow locomotion. A further increase of gait fluctuations during fast walking—as typical in patients with CA—was only observed in a small subgroup of patients with DBN with an additional dysfunction of cerebellar hemispheric regions (Fig. 2).
Topodiagnostic scheme for the different locomotor control functions within the cerebellum. Midline structures (vermis, nodulus, and flocculus) are important for the regulation of upright position during walking. The flocculus appears to be also important site for the integration of vestibular information into the locomotor network. Intermediate zones of the cerebellar hemispheres mediate the feed-forward control of multi-joint movements and are important for intra- and inter-limb coordination during walking. Higher locomotor functions, such as target-guided locomotion and visual-controlled stepping, appear to be particularly controlled by the lateral zones of the cerebellar hemispheres
The intermediate zones of the cerebellar hemispheres are directly involved in the adjustment of intra- and inter-limb coordination patterns required for a stable locomotion execution. Ilg et al. demonstrated that subscores of the clinical ataxia scale which reflect deficits in the control of limb dynamics and the intra-limb coordination for goal-directed movements are highly correlated with the variability of stepping in patients with CA [9]. In a similar study, clinical rating scores of limb ataxia were most strongly associated with increased gait variability during fast walking [15]. Finally, the lateral parts of the cerebellar hemispheres are thought to be important for the regulation of complex walking tasks such as walking with target-guided stepping or visually guided locomotion [10].
Clinical aspects of falls risk estimation in patients with cerebellar ataxia and vestibular disorders
Patients with peripheral vestibular disorders are at a moderate risk of falls (OR: 5.7 compared to healthy subjects). One-third of patients with BVP experience frequent falls with more than two falls within the preceding 12 months. The risk of fall-related injuries is not increased in patients with peripheral vestibular dysfunction [14]. The presence of increased gait fluctuations during slow walking indicates a particular risk of falling in patients with BVP [16]. Moreover, the presence of a concomitant peripheral neuropathy further critically impairs postural stability in these patients (OR: 3.6).
The fall risk of patients with CA is markedly increased and commonly higher compared to patients with sensory deficits [14]. In a cross-sectional study of patients with balance disorders, patients with CA had the highest rates of fall events (OR: 15.7 for frequent falls compared to healthy subjects). More than 30% of falls in patients with CA result in injuries that require medical attention [14]. Valid predictive markers to identify patients with CA at a particular risk of falling as well as effective fall prevention procedures for these patients are, therefore, highly desirable to improve their quality of life. Within recent years, several studies attempted to identify fall-risk-related factors in patients with CA with in part contradictory results. Accordingly, within the framework of the EUROSCA project, a large retrospective analysis of patients with spinocerebellar ataxias revealed a significant association between the SARA score and the risk of falling of these patients [6]. In contrast, a subsequent prospective study of the same cohort of patients found non-ataxic symptoms to be most associated with the fall status of these patients [7]. This finding promotes the necessity of examining non-ataxia features in patients with ataxia to improve fall-risk estimation. Neither the total SARA score, nor its subscores for gait and posture showed any significant correlation with the fall frequency of patients in this study. This indicates that the SARA rating inadequately represents dynamic balance capacities of patients, since the gait assessment within this rating is focused on the patient’s gait performance during preferred walking speeds—a condition that has been shown to be least affected by cerebellar ataxia [21]. This weakness might contribute to the discrepant outcomes of the EuroSCA studies.
Another study investigating the relationship between quantitative gait parameters and the fall risk in patients with CA found that high levels of gait variability, particularly during slow walking, are significantly correlated with an increased risk of falling [22]. Furthermore, the SARA score was found to highly correlate to increased gait fluctuations at fast walking modes [15]. These findings were manifest in both sporadic and hereditary forms of ataxia.
In summary, these findings stress the importance for a clinical assessment of concomitant (sensory) dysfunctions in patients with BVP and CA to improve fall-risk estimation. Moreover, the evaluation of gait variability during slow and fast walking might further improve the quality of the estimation. Therefore, instructions to walk detectably slower than self-selected speed (<0.6 m/s) without interuptions and to walk as fast as possibly, without allowing the transition to running (>1.5 m/s), could be recommended.
Pharmacotherapy of cerebellar ataxia: new developments
So far, there is no effective pharmacotherapeutic approach for the treatment of cerebellar gait ataxia. Exceptions to this statement are specific treatment options in a few recessive ataxia forms, such as Ataxia with vitamin E deficiency (with α-tocopherol), Cerebrotendinous Xanthomatosis (with HMG-CoA reductase inhibitor), Niemann- Pick type C (with Miglustat), Abetalipoproteinaemia (with α-tocopherol), Refsum disease (lifelong dietary restriction of phytanic acid combined with a high-calorie diet), and ataxia with coenzyme Q deficiency (ADCK3/SCAR9) (with CoQ10). Moreover, there is some evidence for Varenicline in patients with spinocerebellar ataxia (SCA) and Amantadine in degenerative forms of ataxia (for overview [24]). Further studies found a positive effect of Riluzole in hereditary and sporadic forms of ataxia. A recent randomized, placebo-controlled study in patients with spinocerebellar ataxia and Friedreich ataxia showed that Riluzole (50 mg orally, twice daily) increased the rate of patients with improved SARA score from 11 to 50% compared to placebo in an intention-to-treat analysis [13].
4-Aminopyrdine (4-AP), a voltage-gated potassium channel blocker, was recently tested in cerebellar gait ataxia with first promising results. Accordingly, 4-AP improved the precision of stepping (temporal gait variability) in two case series of patients with different entities of CA, in particular during fast walking modes. The beneficial effect of 4-AP on gait performance in patients was independent of their severity of ataxia (assessed by the SARA rating), but associated with a high magnitude of temporal gait variability prior to treatment [18, 20]. The putative mode of action of 4-AP is considered to be an improvement in the precision of the intrinsic pacemaker function of Purkinje cells [2], which might lead to the more regular timing of the walking pattern in patients. A case series of 16 patients with hereditary and sporadic forms of ataxia did not show significant changes of the SARA score, but found a moderate improvement in walking speed and speech under treatment with 2 × 10 mg of the sustained release form of 4-AP (fampridine) for 2 weeks [8]. Two randomized, controlled trials with fampridine are currently ongoing (FACEG in patients with different forms of ataxia, NCT01811706 in patients with SCA 1, 2, 3, 6) (Table 1).
Another recent case series in patients with different forms of CA found that the modified amino acid acetyl-dl-leucine significantly improved ataxic symptoms, such as improvements in subscores for gait, speech, finger chase, nose–finger test, rapid-alternating movements, and heel-to-shin of the SARA [23]. However, a consecutive fall series on patients with sporadic forms of ataxia and spinocerebellar ataxias was not able to confirm these positive effects [12]. Acetyl-dl-leucine has been shown to facilitate central sensory compensation in brainstem vestibular centers, thalami, basal ganglia, and insular regions (for overview [5]). In the context of cerebellar gait ataxia, acetyl-dl-leucine treatment in patients with CA led to a decrease of temporal gait variability, in particular during slow walking [17]. A multi-center, multinational placebo-controlled trial on the effect of acetyl-dl-leucine on different ataxia symptoms (including gait ataxia) is currently ongoing (ALCAT, recruitment finished).
In summary, Riluzole appears to be a treatment option for patients with spinocerebellar ataxia and Friedreich ataxia. Both response rate and clinical improvement were low to moderate. For patients with a fast deterioration of ataxia, Riluzole could be recommended to decrease the disease progression.
Alternative symptomatic treatment options such as 4-AP and acetyl-dl-leucine might offer new and promising approaches to improve dynamic instability in patients with cerebellar gait ataxia, although the literature shows conflicting results. Both drugs are currently evaluated in randomized controlled trials. The putative modes of action differ between these two drugs: 4-Aminopyrdine primarily acts via an increase of Purkinje cell pacemaker precision and particularly improves the rhythmicity of stepping during fast walking. In contrast, acetyl-dl-leucine presumably improves vestibulocerebellar functions and thereby improves dynamic stability control during slow walking. This indicates the possibility for a complementary treatment approach to improve both aspects of cerebellar gait ataxia.
References
Allum JH, Adkin AL (2003) Improvements in trunk sway observed for stance and gait tasks during recovery from an acute unilateral peripheral vestibular deficit. Audiol Neurootol 8:286–302
Alvina K, Khodakhah K (2010) The therapeutic mode of action of 4-aminopyridine in cerebellar ataxia. J Neurosci 30:7258–7268
Brandt T, Strupp M, Benson J (1999) You are better off running than walking with acute vestibulopathy. Lancet 354:746
Dieterich M, Brandt T (1993) Ocular torsion and tilt of subjective visual vertical are sensitive brainstem signs. Ann Neurol 33:292–299
Feil K, Bremova T, Muth C, Schniepp R, Teufel J, Strupp M (2016) Update on the pharmacotherapy of cerebellar ataxia and nystagmus. Cerebellum 15:38–42
Fonteyn EM, Schmitz-Hubsch T, Verstappen CC, Baliko L, Bloem BR, Boesch S, Bunn L, Charles P, Durr A, Filla A, Giunti P, Globas C, Klockgether T, Melegh B, Pandolfo M, De Rosa A, Schols L, Timmann D, Munneke M, Kremer BP, van de Warrenburg BP (2010) Falls in spinocerebellar ataxias: results of the EuroSCA Fall Study. Cerebellum 9:232–239
Fonteyn EM, Schmitz-Hubsch T, Verstappen CC, Baliko L, Bloem BR, Boesch S, Bunn L, Giunti P, Globas C, Klockgether T, Melegh B, Pandolfo M, Schols L, Timmann D, van de Warrenburg BP (2013) Prospective analysis of falls in dominant ataxias. Eur Neurol 69:53–57
Giordano I, Bogdanow M, Jacobi H, Jahn K, Minnerop M, Schoels L, Synofzik M, Teufel J, Klockgether T (2013) Experience in a short-term trial with 4-aminopyridine in cerebellar ataxia. J Neurol 260:2175–2176
Ilg W, Golla H, Thier P, Giese MA (2007) Specific influences of cerebellar dysfunctions on gait. Brain 130:786–798
Ilg W, Timmann D (2013) Gait ataxia–specific cerebellar influences and their rehabilitation. Mov Disord 28:1566–1575
Marti S, Palla A, Straumann D (2002) Gravity dependence of ocular drift in patients with cerebellar downbeat nystagmus. Ann Neurol 52:712–721
Pelz JO, Fricke C, Saur D, Classen J (2015) Failure to confirm benefit of acetyl-dl-leucine in degenerative cerebellar ataxia: a case series. J Neurol 262:1373–1375
Romano S, Coarelli G, Marcotulli C, Leonardi L, Piccolo F, Spadaro M, Frontali M, Ferraldeschi M, Vulpiani MC, Ponzelli F, Salvetti M, Orzi F, Petrucci A, Vanacore N, Casali C, Ristori G (2015) Riluzole in patients with hereditary cerebellar ataxia: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 14:985–991
Schlick C, Schniepp R, Loidl V, Wuehr M, Hesselbarth K, Jahn K (2016) Falls and fear of falling in vertigo and balance disorders: a controlled cross-sectional study. J Vestib Res 25:241–251
Schniepp R, Schlick C, Pradhan C, Dieterich M, Brandt T, Jahn K, Wuehr M (2016) The interrelationship between disease severity, dynamic stability, and falls in cerebellar ataxia. J Neurol 263:1409–1417
Schniepp R, Schlick C, Schenkel F, Pradhan C, Jahn K, Brandt T, Wuehr M (2017) Clinical and neurophysiological risk factors for falls in patients with bilateral vestibulopathy. J Neurol 264(2):277–283
Schniepp R, Strupp M, Wuehr M, Jahn K, Dieterich M, Brandt T, Feil K (2016) Acetyl-dl-leucine improves gait variability in patients with cerebellar ataxia—a case series. Cerebellum & Ataxias 3:1
Schniepp R, Wuehr M, Ackl N, Danek A, Brandt T, Strupp M, Jahn K (2011) 4-Aminopyridine improves gait variability in cerebellar ataxia due to CACNA 1A mutation. J Neurol 258:1708–1711
Schniepp R, Wuehr M, Huth S, Pradhan C, Schlick C, Brandt T, Jahn K (2014) The gait disorder in downbeat nystagmus syndrome. PLoS One 9:e105463
Schniepp R, Wuehr M, Neuhaeusser M, Benecke AK, Adrion C, Brandt T, Strupp M, Jahn K (2012) 4-aminopyridine and cerebellar gait: a retrospective case series. J Neurol 259:2491–2493
Schniepp R, Wuehr M, Neuhaeusser M, Kamenova M, Dimitriadis K, Klopstock T, Strupp M, Brandt T, Jahn K (2012) Locomotion speed determines gait variability in cerebellar ataxia and vestibular failure. Mov Disord 27:125–131
Schniepp R, Wuehr M, Schlick C, Huth S, Pradhan C, Dieterich M, Brandt T, Jahn K (2014) Increased gait variability is associated with the history of falls in patients with cerebellar ataxia. J Neurol 261:213–223
Strupp M, Teufel J, Habs M, Feuerecker R, Muth C, van de Warrenburg BP, Klopstock T, Feil K (2013) Effects of acetyl-dl-leucine in patients with cerebellar ataxia: a case series. J Neurol 260:2556–2561
van de Warrenburg BP, van Gaalen J, Boesch S, Burgunder JM, Durr A, Giunti P, Klockgether T, Mariotti C, Pandolfo M, Riess O (2014) EFNS/ENS Consensus on the diagnosis and management of chronic ataxias in adulthood. Eur J Neurol 21:552–562
Voogd J, Glickstein M (1998) The anatomy of the cerebellum. Trends Cognitive Sci 2:307–313
Wuehr M, Schniepp R, Ilmberger J, Brandt T, Jahn K (2013) Speed-dependent temporospatial gait variability and long-range correlations in cerebellar ataxia. Gait Posture 37:214–218
Wuehr M, Schniepp R, Pradhan C, Ilmberger J, Strupp M, Brandt T, Jahn K (2013) Differential effects of absent visual feedback control on gait variability during different locomotion speeds. Exp Brain Res 224:287–294
Wuehr M, Schniepp R, Schlick C, Huth S, Pradhan C, Dieterich M, Brandt T, Jahn K (2014) Sensory loss and walking speed related factors for gait alterations in patients with peripheral neuropathy. Gait Posture 39:852–858
Acknowledgements
The work was supported by Federal Ministry for Education and Science (BMBF, IFB 01EO1401) of Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Roman Schniepp declares that there are no financial disclosures or conflicts of interest. Ken Möhwald declares that there are no financial disclosures or conflicts of interest. Max Wuehr declares that there are no financial disclosures or conflicts of interest.
Funding sources for the study
The work was supported by the Federal Ministry for Education and Science (BMBF, Nr. 80121000-49) of Germany.
Additional information
This manuscript is part of a supplement sponsored by the German Federal Ministry of Education and Research within the funding initiative for integrated research and treatment centers.
Rights and permissions
About this article
Cite this article
Schniepp, R., Möhwald, K. & Wuehr, M. Gait ataxia in humans: vestibular and cerebellar control of dynamic stability. J Neurol 264 (Suppl 1), 87–92 (2017). https://doi.org/10.1007/s00415-017-8482-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8482-3