Abstract
To investigate the frequency, details, and consequences of falls in patients with autosomal dominant spinocerebellar ataxias (SCAs) and to derive specific disease-related risk factors that are associated with an increased fall frequency. Two hundred twenty-eight patients with SCA1, SCA2, SCA3, or SCA6, recruited from the EuroSCA natural history study, completed a fall questionnaire that assessed the frequency, consequences, and several details of falls in the previous 12 months. Relevant disease characteristics were retrieved from the EuroSCA registry. The database of the natural history study provided the ataxia severity scores as well as the number and nature of non-ataxia symptoms. Patients (73.6%) reported at least one fall in the preceding 12 months. There was a high rate of fall-related injuries (74%). Factors that were associated with a higher fall frequency included: disease duration, severity of ataxia, the presence of pyramidal symptoms, the total number of non-ataxia symptoms, and the genotype SCA3. Factors associated with a lower fall frequency were: the presence of extrapyramidal symptoms (more specifically dystonia of the lower limbs) and the genotype SCA2. The total number of non-ataxia symptoms and longer disease duration were independently associated with a higher fall frequency in a logistic regression analysis, while the presence of extrapyramidal symptoms was independently associated with a lower fall frequency. Our findings indicate that, in addition to more obvious factors that are associated with frequent falls, such as disease duration and ataxia severity, non-ataxia manifestations in SCA play a major role in the fall etiology of these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autosomal dominant spinocerebellar ataxias (SCAs) are a group of heredodegenerative disorders that mainly affect the cerebellum. These usually adult-onset ataxias share features of slowly progressive gait and limb ataxia, dysarthria, and abnormal oculomotor control. At present, 27 genetic loci are known to be involved in SCAs and 20 of the corresponding genes have been cloned [1]. The exact pathophysiological mechanisms are yet unresolved and there is still no curative treatment.
At present, we can only provide supportive care, which aims to prevent the functional consequences and complications of the disease. One of these major consequences is falling, of which the devastating physical and emotional corollaries have been reviewed extensively [2–4]. In a recent pilot study, we showed that 93% of patients with degenerative cerebellar ataxias reported one or more falls in the preceding 12 months and many suffered injuries due to these falls [5]. Because of the relatively small number of patients in that preliminary study, specific clinical or genetic characteristics that would allow fall prediction could not be extracted.
The ongoing natural history study of SCA patients as embedded in the EuroSCA collaborative project provided us with a unique opportunity to study falls in a large cohort of fully characterized SCA patients. We sought to investigate the frequency, details, and consequences of falls in SCA patients and specifically aimed to explore patient and disease characteristics that are associated with a high fall frequency. Such data allow us to understand the fall etiology in SCA and are also relevant for future interventional efforts and perhaps more tailored prevention.
Subjects and Methods
Subjects
Patients were recruited from the EuroSCA natural history study, which is a European, clinically based, 3-year follow-up study in 526 patients with SCA1, SCA2, SCA3, or SCA6. At the baseline visit, the ataxia disease stage was assessed, while the following scales were applied: the Scale for the Assessment and Rating of Ataxia (SARA), the inventory of non-ataxia symptoms (INAS), and the Functional Composite score [6–8].
Ten of the seventeen EuroSCA centers participated in this fall study, which would result in a maximum sample size of 383 patients. Exclusion criteria included: complete loss of ambulation or permanent use of wheelchair, severe visual impairment, cognitive disturbances (judged to interfere with obtaining informed consent or with recalling previous fall incidents), and orthopedic disorders that affect balance. Relevant disease characteristics per patient were retrieved from the EuroSCA registry and included age, gender, age at onset, SCA type, and length of expanded CAG repeat. The database of the natural history study provided the baseline SARA score and INAS count.
Patients that participated in the EuroSCA natural history study, but not in this fall study, will be referred to as “non-participants.”
Questionnaire
At the baseline visit of the EuroSCA natural history study, participants were asked to complete a modified version of a standard fall questionnaire, which we had used in our pilot study and which was previously used in studies on falls in Parkinson’s disease and progressive supranuclear palsy [5, 9, 10]. The questionnaire was available in Dutch and English and was translated into German and French by local investigators. The questionnaire had to be self-completed, but if necessary, patients were assisted by the local research physician.
A fall was defined as “every event that results in you ending up on the floor (or any other lower surface) unintentionally” [10]. The questionnaire specifically addressed the first fall after disease onset, the frequency of falls within the last 12 months, fear of falling, restrictions in daily activities due to the falls, measures undertaken to prevent falling, and an estimation of the self-perceived confidence in one’s own balance (0: no confidence, 100: full confidence) [11]. Participants were also asked about fall-related injuries, fall circumstances, and directions of falls, but only if they had indicated to have suffered a fall within the last month, in order to minimize possible recall bias. Finally, the questionnaire also contained questions concerning living circumstances, relevant past medical history, the use of walking aids, and the use of medication. Regarding the latter, only drugs considered to be psychotropic were documented; these mainly included anticholinergics, dopaminergic drugs, benzodiazepines, antidepressants, antiepileptic drugs, and antipsychotics.
Data Analysis and Statistics
Patients were classified as “fallers” if they reported one or more falls in the preceding 12 months covered by the questionnaire. In order to derive factors that are associated with a higher fall frequency, the study group was divided into “non-frequent fallers” and “frequent fallers” prior to data analysis. Those who reported to fall never to just once a year were classified as non-frequent fallers, those who fell at least once a month were classified as frequent fallers. The reason that both the non-fallers and the participants with one fall were put into the group of “non-frequent fallers” is that one fall in the past 12 months might be a chance occasion. For example, in previous studies, 24% of healthy controls also suffered one fall in a 12-month period [10, 11]. We therefore found those who reported to fall at least once a month to represent a group with clinically relevant and likely disease-related falls. To assess ataxia severity, we only used the SARA total score and the scores of the gait and stance items (SARA1 and SARA2, respectively). To study the influence of non-ataxia symptoms, the INAS items were grouped into categories that reflect the various extracerebellar systems, e.g., neuropathy or pyramidal tract pathology.
To study potential selection bias, differences between participants and non-participants were tested for significance using unpaired t tests for age, age at onset disease, disease duration, and SARA and INAS total scores. To examine possible correlations between the INAS scores and SARA total score, as well as other variables, we used bivariate correlations with Spearman’s rho. Chi-square and Fisher exact tests were used for variables expressed as proportions.
To test the significance of differences between the frequent and non-frequent fallers, non-parametric testing was used, including the Mann–Whitney and Kruskal–Wallis tests for numeric data and bivariate correlations with Spearman’s rho for proportions. Multiple comparisons between the four different genotypes, including age, disease duration, age at onset, and SARA and INAS scores, were made using a one-way ANOVA test. To evaluate whether any variable or a combination of variables influenced the frequency of falls, logistic regression analysis with Bonferroni correction was carried out on those variables that significantly differed between the frequent and non-frequent fallers. Odds ratios and 95% confidence intervals were calculated.
Results
From the source population of 383 patients, 234 patients agreed to participate which corresponds to 61.6%. Of these 234 patients, four were excluded because they were found to be asymptomatic. The questionnaire of two further patients was incomplete. Thus, we were able to fully analyze the data from 228 patients, except for the analysis between the different genotypes for which we had to exclude two patients as their genotype could not be confirmed.
The EuroSCA registry contained some missing items and we only analyzed items of which the data were available for more than half (i.e., 115) of the participants, unless specifically stated otherwise.
Study Group and Baseline Characteristics
Participants and non-participants were comparable with respect to gender, disease duration, ataxia severity (SARA), and total number of non-ataxia symptoms (INAS; Table 1). Participating patients were slightly older than non-participants and had a slightly higher age at the onset of disease. Also, the relative frequencies of the different genotypes in the study group did not match those in the group non-participating patients. The proportion of patients with SCA6 was significantly higher in the participant group compared to the non-participant group (Table 1).
Compared to the non-participating patients, the participants with SCA1 had a smaller mean length of the expanded CAG repeat (45.4 ± 5.7 vs. 47.8 ± 5.4, p = 0.031) and the participants with SCA3 had larger mean CAG repeat expansions (70.6 ± 4.6 vs. 67.9 ± 3.8, p < 0.001). There were no such differences for SCA2 and SCA6.
In the group of participants, ataxia severity as expressed by SARA correlated with disease duration (r = 0.525, p = 0.001) and the number of non-ataxia symptoms correlated with ataxia severity (r = 0.292, p < 0.001).
Fall Questionnaire
The mean age at onset of the disease was 41.9 ± 12.8 years and ranged from 7 to 77 years (Table 1). The majority of the patients lived independently (82.6%). With regard to potential contributors to falls, 35.0% of all patients reported to use psychotropic medication. A small proportion of the study group had impaired vision (6.2%) and 14.3% had SCA-unrelated musculoskeletal pathology. Less than half of the patients were able to walk without support or walking aid (49.3%).
At least one fall in the preceding 12 months was reported by 73.6% of the patients (Table 2). The majority of the patients fell once a year to once a month (57.7%), 12.3% indicated to fall once a week and 3.5% experienced a fall every day.
The mean estimated interval between disease onset and the first fall was 4.6 ± 4.8 years, but ranged from 0 to 25 years, implying that a fall had been the presenting feature in some patients (Table 2). More than one third of the patients, who had fallen within the last month, fell forward, backward, or sideways equally frequent (37.4%), while 47.1% mostly fell in the anterior–posterior direction and 15.5% mostly fell sideways.
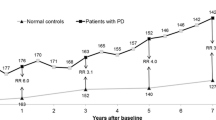
Of the patients who reported one or more falls in the past month, 73.6% had suffered an injury due to a fall and 22.5% had suffered a fracture. A fear of falling occurred in 60.3% of the patients and a similar proportion avoided activities because of this fear. The mean estimation of the self-perceived confidence in one’s own balance was 45.8 (for comparison, in a previous study of 82 healthy controls with a mean age of 59.4 ± 14.2 years, this was 95.4 ± 9.7) [5]. The majority of patients reported to have taken measures to prevent falling, such as using a walking aid or avoiding activities (Table 2).
Differences between Frequent and Non-frequent Fallers
The mean disease duration of frequent fallers was longer (Table 3). The group of frequent fallers contained relatively more SCA3 patients and less SCA2 patients (Table 3). The severity of ataxia, including ataxia of gait (SARA1) and stance (SARA2), was significantly greater in the group of frequent fallers. The total number of non-ataxia symptoms (INAS count) was higher in the group of frequent fallers and the proportion of patients with pyramidal symptoms was larger. Contrarily, the percentage of patients with extrapyramidal symptoms was smaller (Table 3). Upon further study, it became apparent that leg dystonia was particularly more common in SCA3 patients who were classified as non-frequent fallers (data not shown).
Frequent fallers reported more injurious falls and less balance confidence. They also used a walking aid or walking support more often than non-frequent fallers, and frequent fallers were less often able to go outdoors alone. Physiotherapy was given to 29.8% of the non-frequent fallers, compared to 18.8% of the frequent fallers (p = 0.186).
Differences between Genotypes
Relatively more SCA3 patients, followed by SCA1, were classified as frequent fallers. Yet, the different SCA types were comparable with respect to disease duration, SARA1, SARA2, and SARA total scores, as well as to the INAS items “impaired vibration sense,” “impaired visual acuity,” and “extrapyramidal symptoms” (Table 4). However, in SCA1 and SCA3, pyramidal features were much more frequent than in SCA2 and SCA6. SCA3 patients also had the highest frequency of neuropathy and ophthalmoparesis. The SCA6 patients were older, had a later age at onset, and had the lowest INAS count.
Logistic Regression
The variables disease duration, genotype, SARA1, SARA2, SARA total score, INAS count, INAS “pyramidal symptoms,” and INAS “extrapyramidal symptoms” were entered into a logistic regression model. Stepwise forward logistic regression analysis showed that disease duration and the number of non-ataxia symptoms were significantly associated with a higher fall frequency. For disease duration (per year): odds ratio 1.07, confidence interval 1.01–1.13, p = 0.029; for the number of non-ataxia symptoms (per INAS count): odds ratio 1.35, confidence interval 1.12–1.63, p = 0.002. The presence of extrapyramidal symptoms was significantly associated with a lower fall frequency (odds ratio 0.07, confidence interval 0.01–0.76, p = 0.028).
Discussion
Falls have been studied extensively in patients with neurological diseases, such as Parkinson’s disease, progressive supranuclear palsy, and neuromuscular diseases [2–4, 9–13]. Little is known about falls in patients with hereditary cerebellar ataxias. In 2005, a pilot study was conducted in 42 patients with late-onset degenerative cerebellar ataxias, and the results indicated that falls are frequent and often injurious in these patients [5]. However, this study group was too small to derive specific factors that are associated with a higher fall frequency. Such data are relevant, not only for obvious clinical purposes, but also to gain more insight into the causes of falling in these patients.
In this fall study, as part of the ongoing EuroSCA natural history study, 74% of the patients reported at least one fall in the past 12 months. In most patients, falls occurred in an early disease stage (often within the first 2 years of disease) and were even the presenting feature in 10%. The majority of the patients fell in the anterior–posterior direction, which corresponds to a previous study that examined trunk sway in SCA patients that demonstrated more anterior–posterior than lateral postural instability during everyday stance and walking tasks [14].
Our study showed that falls often have major consequences for SCA patients, including (severe) injuries and avoidance of activities due to a fear of future falls. Factors that predicted a higher frequency of falls in the whole study group were disease duration, severity of ataxia, the INAS count (i.e., number of non-ataxia symptoms), the presence of pyramidal features, and the genotype SCA3. Contrary to other fall studies, psychotropic medication did not influence the frequency of falls [12, 13, 15]. We were not able to study the potential influence of spasmolytic drugs as the number of patients on these agents was too low. The genotype SCA2 and the presence of extrapyramidal symptoms were associated with a lower fall frequency.
The genotype SCA3 was identified to be one of the factors associated with a higher fall frequency. Indeed, frequent fallers were more common amongst SCA3 patients, while the four different genotypes were comparable with respect to disease duration and severity of ataxia. Interestingly, the total number of non-ataxia symptoms was highest in the SCA3 and SCA1 groups and pyramidal features in particular were much more frequent in these subtypes. The relevance of pyramidal features is also evident from the fact that within the SCA6 group, frequent fallers were observed to have more pyramidal tract involvement (data not shown).
In a logistic regression analysis, the disease duration and the number of non-ataxia symptoms were independently associated with a higher fall frequency. The number of non-ataxia symptoms, ataxia severity, and disease duration were all interrelated, and the number of non-ataxia symptoms was also significantly different for the various genotypes. This might in part explain why INAS count and disease duration were identified by logistic regression analysis as a contributing factor, and ataxia severity was not. Given the clinical heterogeneity of the SCAs, in particular SCA3, it was not unexpected that the logistic regression analysis did not point to a certain genotype as predictive but rather to associated disease features.
The presence of extrapyramidal features was correlated with a lower fall frequency in the logistic regression analysis. Considering these extrapyramidal symptoms, of which the overall prevalence was low, particularly dystonia of the lower limbs was responsible for the significant difference between frequent and non-frequent fallers. Leg dystonia was mostly observed in SCA3 patients within the group of non-frequent fallers, and neither present in SCA1 patients, SCA6 patients, nor in the total group of frequent fallers (data not shown). Upon further analysis of the data, however, it was apparent that pyramidal features were less prevalent in those with dystonia (20%) than in those without dystonia (46.1%). So although extrapyramidal features came out as a separate factor in the logistic regression analysis, this might largely be explained by the absence of pyramidal features. The presence or absence of dystonia was not related to disease duration or age at onset.
We are not aware of any fall study in patients with primary or secondary dystonia, but it would be interesting to see whether falls are indeed less common in this movement disorder compared with other neurological diseases.
The results of our study should be interpreted in the context of several limitations. The first is the retrospective nature of this questionnaire study. This might have introduced a recall bias, with an underreporting or overestimation of falls. Still, the basic results of this study are to a large extent biologically plausible. Second, the questionnaire was not available in all languages and the local investigators had to translate the questions for the patients in some centers. That might have led to a slightly different interpretation of the various questions. Third, there was no full match between the participating and non-participating SCA patients, as there were some differences in age, age at onset, relative SCA frequencies, and CAG repeat expansion in SCA1 and SCA3. It is however difficult to speculate how these differences might have influenced our results, as sufficient matching was obtained for disease duration, ataxia severity, and total INAS count. Finally, the current EuroSCA natural history study does not include detailed neuropsychological evaluations and the potential influence of cognitive dysfunction might hence have remained unrecognized.
We conclude that falls are very common in SCA patients and that falls have major consequences for these patients. For SCA patients in general, disease duration, the severity of ataxia, the total number of non-ataxia symptoms, and the presence of pyramidal symptoms seem to predict a higher fall frequency. Patients with extensive extracerebellar pathology and more specifically, frequent pyramidal tract involvement (such as in SCA3 and SCA1) are more prone to fall. It is yet unclear how to translate these findings to the clinical practice, i.e., to the individual SCA patient. However, in the design of fall intervention trials in SCAs, which are currently initiated, these contributory factors should be taken into account.
References
Bloem BR, Boers I, Cramer M, Westendorp RG, Gerschlager W (2001) Falls in the elderly. I. Identification of risk factors. Wien Klin Wochenschr 113:352–362
Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ (1997) Fear of falling and restriction of mobility in elderly fallers. Age Ageing 26:189–193
Zijlstra GA, van Haastregt JC, van Eijk JT, van Rossum E, Stalenhoef PA, Kempen GI (2007) Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of activity in the general population of community-living older people. Age Ageing 36:304–309
Van de Warrenburg BPC, Steijns JA, Munneke M, Kremer HP, Bloem BR (2005) Falls in degenerative cerebellar ataxias. Mov Disord 20:497–508
Schmitz-Hübsch T, du Montcel ST, Baliko L et al (2006) Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66:1717–1720
Klockgether T, Lüdtke R, Kramer B et al (1998) The natural history of degenerative ataxia: a retrospective study in 466 patients. Brain 121:589–600
Lynch DR, Farmer JM, Tsou AJ et al (2006) Measuring Friedreich ataxia: complementary features of examination and performance measures. Neurology 66:1711–1716
Bloem BR, Munneke M, Mazibrada G et al (2004) The nature of falling in progressive supranuclear palsy. Mov Disord 19:359–360
Bloem BR, Grimbergen YAM, Cramer M, Willemsen M, Zwinderman AH (2001) Prospective assessment of falls in Parkinson’s disease. J Neurol 248:950–958
Bloem BR, Mazibrada G, Schrag A et al (2002) Falls and injuries in progressive supranuclear palsy (PSP). Mov Disord 17(Suppl):252
Pieterse AJ, Luttikhold TB, De Laat B, Bloem BR, Van Engelen BG, Munneke M (2006) Falls in patients with neuromuscular disorders. J Neurol 251:87–90
Stolze H, Klebe S, Zechlin C, Baecker C, Friege L, Deuschl G (2004) Falls in frequent neurological diseases. J Neurol 251:79–84
Van de Warrenburg BPC, Bakker M, Kremer HP, Bloem BR, Allum JHJ (2005) Trunk sway in patients with spinocerebellar ataxia. Mov Disord 20:1006–1013
Stolze H, Friedrich HJ, Steinauer K, Vieregge P (2000) Stride parameters in healthy young and old women -measurement variability on a simple walkway. Exp Aging Res 26:159–168
Acknowledgment
This study was supported by the European Committee (6th Framework Program, EuroSCA, LSHM-CT-2004-503304) and GeneMove/01 GM 0503 from the German Ministery of Education and Research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding organizations
This study was supported by the European Committee (6th Framework Program, EuroSCA, LSHM-CT-2004-503304) and GeneMove/01 GM 0503 from the German Ministery of Education and Research.
Financial disclosure
The authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Fonteyn, E.M.R., Schmitz-Hübsch, T., Verstappen, C.C. et al. Falls in Spinocerebellar Ataxias: Results of the EuroSCA Fall Study. Cerebellum 9, 232–239 (2010). https://doi.org/10.1007/s12311-010-0155-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-010-0155-z