Abstract
Purpose
This systematic review aims to compare the efficacy and safety of multilevel and single level surgery, including barbed pharyngoplasties, in the treatment of obstructive sleep apnea (OSA).
Methods
The study followed PRISMA guidelines and searched PubMed/MEDLINE, Google Scholar, and Ovid databases for studies evaluating the effect of barbed pharyngoplasties on adults with OSA. Prospective and retrospective cohort studies were included with pre- and post-treatment comparisons of sleep tests and self-reported clinical outcomes. Exclusion criteria were non-English studies, case reports, reviews, conference abstracts, letters, and pediatric studies. Successful surgery was classified using Sher’s criteria.
Results
The study selected a total of 1014 patients from 26 studies, 24 of which were longitudinal studies with 10 retrospective trials and 14 prospective studies. The average age of the patients was 46.9 years, with an average Body Mass Index (BMI) of 25.6 kg/m2. Most of the patients were male (84.6%). The study included only palatal surgical techniques with barbed sutures, and patients who underwent cardio-respiratory monitoring and Drug Induced Sleep Endoscopy (DISE) before surgery. Mean Apnea Hypopnea Index (AHI) preoperative was 32.9/h, AHI postoperative was 11.9/h, and mean reduction of AHI was 62.3%. The most commonly adopted palatoplasty was Barbed Repositioning Pharyngoplasty (BRP) in 16 out of 26 studies, followed by its subsequent modifications in 3 studies.
Conclusions
Barbed pharyngoplasties appear to be effective both on objective measurement and subjective scores. DISE represents a fundamental tool to assess uni-level or multilevel obstruction. When retro-palatal collapse is present, barbed pharyngoplasty appears to be effective. Barbed pharyngoplasties maintain their good results both in single level or multilevel surgery. Randomized clinical controlled trials with multi-center cooperation and long-term study are necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a prevalent sleep disorder that affects a significant portion of the population and is characterized by repetitive episodes of partial or complete collapse of the upper airway during sleep [1]. This leads to reduced oxygenation, fragmented sleep and excessive daytime sleepiness, among other symptoms. While continuous positive airway pressure (CPAP) therapy is the most common treatment for OSA, many patients find it intolerable or ineffective, leading to a search for alternative treatments [2].
Surgical intervention for OSA has gained increased attention in recent years, and multilevel and single level surgical procedures, including barbed pharyngoplasties, have emerged as promising treatment options [3]. A systematic review of the literature is crucial to evaluate the available evidence on the efficacy and safety of these surgical approaches in treating OSA and to provide guidance for clinical decision making.
The purpose of this systematic review is to compare the outcomes of multilevel and single level surgery, including barbed pharyngoplasties, in the treatment of OSA. The review will critically assess the current evidence on the efficacy of these surgical approaches in terms of improving OSA-related symptoms, such as excessive daytime sleepiness and quality of life, as well as the safety of these procedures.
This systematic review will follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and will be conducted using a comprehensive search strategy, including electronic databases and manual searches of the relevant literature. The inclusion criteria will be established a priori, and the quality of the eligible studies will be assessed using validated tools.
In conclusion, this systematic review will provide a comprehensive evaluation of the available evidence on the efficacy and safety of multilevel and single level surgery, including barbed pharyngoplasties, in the treatment of OSA. The results of this review will be of significant value to healthcare professionals and patients considering surgical intervention for OSA.
Materials and methods
The study was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [4]. The study was developed by The Sleep Surgery (SS) Study Group of Young Otolaryngologists of the Italian Society of Otolaryngology (GOS-SIO).
Data source and study searching
An electronic search was performed on PubMed/MEDLINE, Google Scholar, and Ovid databases. An example of a search strategy is the one used for PubMed/MEDLINE: “Barbed” and “Mono-level surgery”; “Multilevel surgery”; “Pharyngoplasty”; “Palatoplasty”; “Anterior Pharyngoplasty”; “Lateral Pharyngoplasty”; “Expansion Sphincter Pharyngoplasty”; “Suspension Pharyngoplasty”; “Reposition Pharyngoplasty”; “Snore Surgery”; “Roman Blinds Technique”; “Alianza Technique”.
The other searches were adjusted to fit the specific requirements for each database. Then, a cross-reference search of the included studies was performed to minimize the risk of missing relevant data. The last search was run on August 2022.
Inclusion/exclusion criteria
Only studies regarding the effect of different types of barbed pharyngoplasty (BP) to treat snorers and obstructive sleep apnea (OSA) patients with one or multiple collapse performed as a single procedure and/or as a part of multilevel surgery were included according to the PICOS acronym: patients (P), adults with from OSA; Intervention (I), barbed pharyngoplasty; Comparison (C), pre- and post-treatment; Outcome (O), preoperatively and postoperatively polysomnographic (PSG) result, such as apnea–hypopnea index (AHI), Oxygen desaturation index (ODI), minimum of oxygen desaturation (LOS) and self-reported (e.g., Epworth Sleepiness Scale, ESS) clinical outcomes; and Study design (S), both prospective and retrospective cohort studies.
The PICO process is a mnemonic used in evidence-based medicine to frame and answer a clinical or health care-related question.
Exclusion criteria for the study were as follows: (1) not English studies; (2) case reports, reviews, conference abstracts, letters, and pediatric studies; (3) studies with unclear and/or incomplete data; and (4) studies regarding the comparison between barbed and non-BP techniques. No publication date restriction was imposed.
Papers were selected based on their appropriateness, that is, publication in peer-reviewed journals.
If present, Sher’s criteria [5] was reported to classify a surgery as successful (reduction of AHI by 50% from the baseline and postoperative AHI less than 20/h).
For each study we also calculated the mean relative reduction as previous described by De Apodaca P.M. (AHI pre–AHI post/AHI pre × 100) [6].
Results
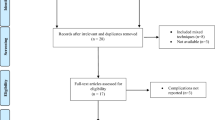
The flow diagram shown in Fig. 1 (PRISMA flow diagram) depicts the selection process that includes a total of 1014 patients. The baseline characteristics are reported in Table 1.
In particular, 24 out of 26 were longitudinal studies, 10 of these were retrospective trials(507 patients included), 14 were prospective studies (390 patients included). Only 2 were randomized clinical trial (117 patients included). Studies less than 10 patients were excluded (see inclusion criteria). Studies were mainly single patient series, just one multicenter study was included. The mean age was 46.9 years (range 37.5–64 years). Most of the studies selected excluded obese patients with BMI higher than 32. Average BMI of selected patients was 25.6 kg/m2. Subject included in the studies were mainly male (84.6%, 577/682), with a minority of female (15.4%, 106/682). This data is missing in 32.7% (332/1014), because not fully expressed in text or tables.
The different types of BP techniques are reported in Table 2.
All patients were screened with cardio-respiratory monitoring (level III polysomnography). Most studies included OSAS patients, with mild to severe disease. 3 studies included also patients suffering of simple snoring, with AHI lower than 5/h.
Mean AHI preoperative (weighted on the number of subjects included) was 32.9/h (ranged from 22 to 46.3/h, median AHI was 32.6/h), AHI postoperative was 11.9/h (ranged from 5 to 21.6/h, median AHI was 12.9/h). Mean relative reduction of AHI (AHI pre–AHI post/AHI pre × 100) was 62.3%. When not expressed, we calculated this data. Its value was 63.2%.
Information about ODI preoperative and postoperative was available in 19/26 studies (73%, 642/1014 patients).
Mean ODI preoperative was 30.1/h (range 17–44.7/h, median 29/h), mean ODI postoperative was 13/h (range 2–25.8/h, median ODI 12/h). Mean reduction of ODI (ODI pre–ODI post /ODI pre × 100) was 60.3% (range 9.4–90.9/h).
Mean preoperative ESS, available in 21 studies (80.7%), was 10.5 (range 6–15.3, median 10.2). Mean postoperative ESS was 4.6 (range 0–11, median 4.4).
All patients (100%) underwent also, before surgery, a drug induced sleep endoscopy (DISE) to assess the site or sites of collapse during a pharmacologically induced sleep [7].
Different protocols, settings and drugs for patient’s sedation were utilized (DEXA, Propofol, Midazolam or both of them). Indications to palatal barbed surgery were quite homogeneous: palatal or oropharyngeal collapse in DISE was required. Patients treated with multilevel surgery could have also retroglossal (hypopharyngeal or at the level of tongue base) or epiglottic collapse.
Retro-palatal collapse could be transversal, antero-posterior or circular pattern. According to the surgical palatal technique adopted, patients included should have antero-posterior palatal collapse (3 studies), circular complete palatal collapse (3 studies) or lateral/oropharyngeal (4 studies).
If tongue base or epiglottic collapse was present, multilevel surgery was mostly associated.
All patients enrolled to surgery refused ventilatory therapy or showed low adherence to CPAP.
The study included only palatal surgical techniques with barbed sutures. We divided the selected studies into two groups:
-
Single palatal surgery: palatal barbed surgery was performed as single surgical procedure. These patients could have done only a synchronous or previous nasal surgery (septoplasty of turbinoplasty).
-
Multilevel surgery: palatal barbed surgery was done as a part of as multilevel surgery the multiple procedures undergone on the airway. In this group we allocated patients that underwent nasal and hypopharyngeal or tongue base reduction or epiglottoplasty or hyoid suspension were performed at the same time or in multi-step surgeries.
In 17/26 studies barbed surgery was performed as a single surgery; usually (8 studies) patients underwent nasal surgery (septoplasty or turbinoplasty or both) during or before surgical palatal procedure.
In other 9 studies, barbed surgery was part of a multilevel surgery, in a single simultaneous step or multiple step (previous or further) surgery.
In 6 out of 9 multilevel surgery, palatal surgery was associated to trans oral robotic surgery (TORS) or hyoid suspension. The most adopted palatal surgical technique was BRP (16/26 studies, 718 subjects) with its subsequent modifications (3 studies, 85 patients): 70.8% and 8.4%, respectively (See Table 2). 3 studies included barbed sutures for ESP in 79 patients.
Two studies included patients treated with barbed anterior pharyngoplasty described by Salamanca in 2014 (42 subjects). One study included the Modified barbed soft palatal posterior pillar webbing flap palatopharyngoplasty.
Mean time of follow up (with post-operative cardiorespiratory monitoring and AHI value) varied from 4 to 12 months. These data were not available in three studies.
All analyzed studies reported satisfactory outcomes. According to Sher’s criteria [5], mean surgical success rate was 77.6% (range 54.4–95%). In five studies (19%) these data were not available. The cure rate (reduction of AHI of 50% from baseline and AHI postoperative less than 5/h) was 22.6% (data was available in 31.8%).
Main relative reduction of AHI was similar in patients who underwent uni-level or multilevel surgery (62.4 vs 64.1% respectively), but surgical success according to Sher’s criteria was slightly higher in single palatal surgery 68.7 vs 57.3%. No differences were present in preoperative AHI between single palatal/multilevel group (31.1 vs 34.7/h), with lower post-operative AHI in multilevel group 5.3 vs 11.2/h, as seen in Fig. 2.
The differences between two groups are shown in Table 1 (single palatal vs multilevel surgery).
Discussion
In the last decades, sleep surgery has moved from phase 1 and 2 Stanford algorithm by Riley and Powell to a more individualized approach [8]. The original phase 1 and phase 2 Stanford Protocol was created in order to target the multilevel obstruction typical of patients with severe OSAS. Phase 1 involved multi-level surgery including tonsillectomy and uvulo-palatal flap or/with genioglossus advancement (GA), according to the site of obstruction (oropharynx/soft palate, or hypopharynx/base of tongue or both). Inadequate responders to phase 1, after having repeated polysomnography, were recommended to undergo phase 2 surgery which consisted of maxillomandibular advancement (MMA). Non-surgical alternatives to phase 1 and phase 2 were CPAP and oral appliances.
Two important concepts from these papers were [9]: (a) the anatomic basis should be the true prognosis factor for OSA surgery, not only the severity of the disease, and (b) if you add the additional tongue base surgery to the UPPP, the surgical success rate will increase [10]. Nevertheless the collapsible tract of the upper airway starts from the retro-palatal level, also nasal reconstruction is performed during phase 1 surgery if patients present with obstructive nasal deformities. Nasal surgery was initially not considered strictly part of the multilevel surgery, but an update to the Stanford algorithm by Riley and Powell developed by Liu SY in 2020 [11] included nasal surgery in phase 1 surgery.
Nasal airway patency and the minimization of mouth breathing is fundamental in OSAS patients, because mouth opening during sleep results in posterior displacement of the tongue into the hypopharyngeal airway causing a secondary obstruction.
Nowadays, drug induced sleep endoscopy (DISE) represents a possible and useful pre-surgical evaluation to assess or confirm the site or sites of collapses in the airway in OSAS patients. DISE permits potentially to phenotype patients during a pharmacologically induced sleep, assessing which kind of surgery fits better with anatomical patient’s features [12]. This approach permitted to avoid unnecessary surgical intervention and a to make more tailored surgery: one surgery does not fits all patients.
DISE permits also to assess that, usually, multilevel obstruction is presents. Several studies showed a prevalence of multilevel obstruction: 93.3% [13], 87% [14], 68.2% [15].
Different multiple palatal techniques have been described in the last decade, trying to overcome not satisfying long-term outcomes or side the effects (first of all the velar insufficiency) [16] of the previous most utilized uvulo-palato-pharyngoplasty (UPPP) [17].
Moreover, independently from the surgical technique, barbed sutures have represented a ground-breaking development in term of effectiveness, handling, sparring time and preservation of anatomical structure [18].
Barbed sutures allowed the transition from resective palatal procedures (UPPP [17], Laser assisted uvulo-pharyngoplasty LAUP [19], trans-palatal pharyngoplasty TPA [20], expansion pharyngoplasty by Pang [21, 22], functional expansion pharyngoplasty FEP by Sorrenti [23]) to no-cutting remodeling intra-pharyngeal [24] and muscle sparring procedures.
In well-selected patients by DISE, barbed palatal surgeries showed optimal outcomes, according to Sher’s criteria.
Aim of this paper is to review the efficacy of palatal surgery with barbed sutures. Previous studies have already shown the efficacy and safety of palate techniques performed with non-barbed threads[25]. Surgical complications (bleeding, exposure or extrusion of barbed suture, post-operative symptoms complained by patients) weren’t taken into account in this study, because were previously described in a more specific reviews [26,27,28,29].
This paper compared the effectiveness of barbed palatal surgery in OSAS patients in a single level surgery and multilevel surgery (nasal surgery, tongue base reduction) in a single-step or multi-step approach. After a revision of the current literature, we selected 26 studies that focused of barbed sutures in OSA patients, including 1014 patients. Figure 3 shows the increasing interest in literature in the last 4 years.
The most utilized technique in the selected studies was BRP in 70.8% (718/1014) described by Vicini [25] or its modifications (8.4%, 85/1014), followed by Alianza technique, described by Mantovani [30]. Other barbed techniques are listed in Table 1.
In 65.4% (17/26 studies) barbed palatal surgery was performed as a single level surgery; if necessary, usually (30.8% of cases) patients underwent also nasal surgery (septoplasty or turbinoplasty or both) during or before surgical palatal procedure. Nevertheless, also in the same study, this data could not be uniform or not totally available.
In the remaining nine studies, barbed surgery was part of a multilevel surgery, in a single simultaneous step or multiple step (previous or further) surgery. In 6 out of 9 multilevel surgery, palatal surgery was associated to trans oral robotic surgery (TORS) or hyoid suspension. In these cases, retroglossal collapse in DISE was the main finding.
Trans-oral robotic surgery (TORS) consists of reduction of hypertrophic lymphatic tongue base, eventually associate to epiglottoplasty, if DISE assessed primary or secondary epiglottic collapse [31].
According to Sher’s criteria, mean surgical success rate in barbed pharyngeal surgery was 77.6% (range 54.4–95%), while in 19% this data was missing. The cure rate, defined as the reduction of AHI of 50% from baseline and AHI postoperative less than 5/h was lower, 22.6%.
These results are better than UPPP, showed in a review by Lin HC [9], where the success rate, according to Sher’s criteria, was 40.7% in uni-level surgery and 61.6% in multilevel surgery.
Thaler [32] showed a surgical success rate in multilevel surgery with not barbed and different palatal technique (UPPP + TORS) of 56%, lower (30%) in patients with previous surgery (multi-step surgery).
Main relative reduction of AHI in our study was similar in patients who underwent pharyngeal surgery in uni-level or multilevel setting: 62.4 vs 64.1% respectively. Nevertheless, the surgical success (pondered) according to Sher’s criteria was slightly higher in uni-level surgery (78.1%, CI 54.4–95%) than in multilevel setting (74.7%, CI 60–94.1%).
The minimal decrease of surgical success in multilevel setting compared to uni-level setting could be explained not by the lower effectiveness of non-palatal surgical techniques, but by the higher severity of AHI [33]. In this study, DISE could have helped to optimize results, with the identification of the correct sites of collapse.
Saenwandee [34] in a recent meta-analysis of barbed pharyngoplasty described higher results according to Sher’s criteria, with success rate of 85.2% (CI 77.6–92.7%), whereas in single-level surgery the success rate was 74.63% (CI 69.92–79.33%) in multilevel surgery. Not all these patients were previously studied with DISE, and they didn’t report the pattern and sites of airway collapse.
Barbed palatal surgery appears to be effective also on OSA symptoms such as daytime sleepiness. According to Epworth’s sleepiness Scale (ESS), ESS average reduced from 10.6 to 4.6 in single-level pharyngeal surgery and from 9.7 to 4.4 in multilevel pharyngeal surgery. It’s important to note that, nevertheless the improving in sleepiness, patients selected to surgery weren’t not sleepy (ESS: 10.6, lower than 12, pathologic sleepiness).
Most of studies included with pharyngeal surgery (50%) included exclusive retro-palatal collapse in DISE, but the pattern of collapse was not specified: anteroposterior, lateral, or circular. Barbed palatal surgery isolated seem to be more effective on circular collapse as seen in Table 3, with lower effect on anteroposterior collapse. Nevertheless, these data referred to different surgical techniques (anterior pharyngoplasty vs lateral/BRP pharyngoplasty), and this small difference could be most related to the surgical procedure rather than to the selection inclusion criteria.
Limitations of the current literature
Most of the study included are longitudinal (92.3%, 24/26), 38.5%% (10) of these were retrospective trials (507 patients included), 53.8% (14) prospective studies (390 patients included). Only two were randomized trial (117 patients included).
The majority of the patients included, 84.6% were non-obese men, average BMI of 25.6 kg/m2. This data could not be representative of the sex prevalence of OSA (men: women, 2:1). This bias could be explained by the tendency by men to surgical intervention in OSA, being more socially accepted.
Most of studies evaluated preoperative and postoperative BMI and they did not show any difference. On the contrary, most of the studies did not take into account supine AHI and the comparison of supine sleeping time between PSG before and after surgery. If difference was present, global AHI could be consequently altered by lateral position instead of supine position (if patients were positional OSA), rather than by efficacy of surgical procedure on AHI.
High heterogeneity was seen upon tonsillar grade or tonsillar management. Mantovani [35] underwent tonsillectomy to all patients several months before the palatal surgery to avoid bias on surgical success. Vicini 2019 [36] and Iannella 2021 [37], with the same purpose, excluded to palatal surgery patterns with previous tonsillectomy. In this case, previous tonsillectomy could have altered muscular and mucosal tissues. On the other hand, many surgical palatal technique require tonsillectomy during surgery, and tonsillar volume could be a bias in surgical result.
Information about tonsillar grade, according to Friedman [38] score was not available in all studies (9/26). Vicini 2019 [36] excluded high tonsillar grade (3–4), Tsou [39] excluded low tonsillar grade (grade 1). When data were fully described, 48% of patients have tonsillar grade 1–2, 36.2% tonsillar grade 3, 11.2% grade 4.
These missing information could impact surgical success: Matarredona-Quiles [40] showed a positive association between not only tonsillar grade, but tonsillar volume and the success of pharyngeal surgery during OSA treatment.
Tonsillar volume (evaluated with Archimedes’ method or calculating Ellipsoid formula measuring longitudinal, transverse an anteroposterior diameter) was not available in included studies.
Conclusions
Barbed pharyngoplasties, if patients are correctly selected before surgery, are effective both on objective measurement (AHI and ODI) and subjective score (ESS).
DISE represents a fundamental tool to assess uni-level or multilevel obstruction. When retro-palatal collapse is present, barbed pharyngoplasty are effective in OSA surgical treatment.
Barbed pharyngoplasties maintain their good results both in single level or multilevel surgery.
Randomized clinical controlled trials with multi-center cooperation and long-term study are necessary.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
Change history
24 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00405-023-08145-z
References
American Academy of Sleep Medicine (2017) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien
Vitiello MV, Boehlecke B (2015) Barriers to continuous positive airway pressure use in adults with obstructive sleep apnea. Sleep Med Clin 10(3):259–268
Chan A, Remmers JE (2019) Surgical management of obstructive sleep apnea. Chest 156(4):826–836
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. https://doi.org/10.1371/journal.pmed.1000097
Sher AE (2002) Upper airway surgery for obstructive sleep apnea. Sleep Med Rev 6:195–212
De Apodaca PM, Llatas MC, Gras MV, Galofre JD (2020) Improving surgical results in velopharyngeal surgery: our experience in the last decade. Acta Otorrinolaringol (English Edition) 71(4):197–203
De Vito A, Carrasco Llatas M, Ravesloot MJ, Kotecha B, De Vries N, Hamans E, Maurer J, Bosi M, Blumen M, Heiser C, Herzog M, Montevecchi F, Corso RM, Braghiroli A, Gobbi R, Vroegop A, Vonk PE, Hohenhorst W, Piccin O, Sorrenti G, Vanderveken OM, Vicini C (2018) European position paper on drug-induced sleep endoscopy: 2017 Update. Clin Otolaryngol 43(6):1541–1552. https://doi.org/10.1111/coa.13213. (Epub 2018 Sep 30 PMID: 30133943)
Riley RW, Powell NB, Guilleminault C (1993) Obstructive sleep apnea syndrome: a surgical protocol for dynamic upper airway reconstruction. J Oral Maxillofac Surg 51(7):742–747. https://doi.org/10.1016/s0278-2391(10)80412-4. (Discussion 748-9 PMID: 8509912)
Lin HC, Weaver EM, Lin HS, Friedman M (2017) Multilevel obstructive sleep apnea surgery. Adv Otorhinolaryngol 80:109–115. https://doi.org/10.1159/000470879. (Epub 2017 Jul 17. PMID: 28738374)
Friedman M, Ibrahim H, Lee G, Joseph NJ (2003) Combined uvulopalatopharyngoplasty and radiofrequency tongue base reduction for treatment of obstructive sleep apnea/hypopnea syndrome. Oto- laryngol Head Neck Surg 129:611–621
Liu SY, Riley RW, Yu MS (2020) Surgical algorithm for obstructive sleep apnea: an update. Clin Exp Otorhinolaryngol 13(3):215–224. https://doi.org/10.21053/ceo.2020.01053. (Epub 2020 Jul 1. PMID: 32631040; PMCID: PMC7435437)
Vanderveken OM (2018) Drug-induced sleep endoscopy (DISE) as a guide towards upper airway behaviour and treatment outcome: the quest for a vigorous standardization of DISE. Sleep Breath 22(4):897–899. https://doi.org/10.1007/s11325-018-1743-2. (Epub 2018 Oct 18 PMID: 30338440)
Riley RW, Powell NB, Guilleminault C (1993) Obstructive sleep apnea syndrome: a review of 306 consecutively treated sur- gical patients. Otolaryngol Head Neck Surg 108:117–125
Abdullah VJ, van Hasselt CA (2005) Video sleep nasendoscopy. In: Terris DJ, Goode RL (eds) Surgical management of sleep apnea and snoring. Taylor and Francis, Boca Raton, pp 143–154
Vroegop AV, Vanderveken OM, Boudewyns AN et al (2014) Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1249 cases. Laryn- goscope 124:797–802
Tang JA, Salapatas AM, Bonzelaar LB, Friedman M (2017) Long-term incidence of velopharyngeal insufficiency and other sequelae following uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 156(4):606–610. https://doi.org/10.1177/0194599816688646. (Epub 2017 Jan 24 PMID: 28116979)
Friberg D, Sundman J, Browaldh N (2019) Long-term evaluation of satisfaction and side effects after modified uvulopalatopharyngoplasty. Laryngoscope 2019:12
Pinto V, Piccin O (2018) Making pharyngoplasty simple and safe: when plastic surgery meets sleep surgery. Plast Reconstr Surg 142(6):987e–988e. https://doi.org/10.1097/PRS.0000000000005036
Kamami YV (1994) Outpatient treatment of sleep apnea syndrome with CO 2 laser, LAUP: laser-assisted UPPP results on 46 patients. J Clin Laser Med Surg 12(4):215–219. https://doi.org/10.1089/clm.1994.12.215. (PMID: 10172096)
Volner K, Dunn B, Chang ET, Song SA, Liu SY, Brietzke SE, O’Connor P, Camacho M (2017) Transpalatal advancement pharyngoplasty for obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 274(3):1197–1203. https://doi.org/10.1007/s00405-016-4121-3. (Epub 2016 Jun 11 PMID: 27289234)
Pang KP, Woodson BT (2007) Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg 137(1):110–114. https://doi.org/10.1016/j.otohns.2007.03.014
Pang KP, Pang EB, Win MT, Pang KA, Woodson BT (2016) Expansion sphincter pharyngoplasty for the treatment of OSA: a systemic review and meta-analysis. Eur Arch Otorhinolaryngol 273(9):2329–2333. https://doi.org/10.1007/s00405-015-3831-2
Sorrenti G, Piccin O (2013) Functional expansion pharyngoplasty in the treatment of obstructive sleep apnea. Laryngoscope 123(11):2905–2908. https://doi.org/10.1002/lary.23911
Casale M, Moffa A, Giorgi L et al (2022) No-cutting remodelling intra-pharyngeal surgery can avoid CPAP in selected OSA patients: myth or reality? Eur Arch Otorhinolaryngol 279(10):5039–5045. https://doi.org/10.1007/s00405-022-07261-6
Vicini C, Hendawy E, Campanini A et al (2015) Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. “We are on the giant’s shoulders.” Eur Arch Otorhinolaryngol 272(10):3065–3070. https://doi.org/10.1007/s00405-015-3628-3
Gulotta G, Iannella G, Meccariello G, Cammaroto G, Visconti IC, de Vincentiis M, Greco A, Pelucchi S, Magliulo G, Ruoppolo G, Maniaci A, Cocuzza S, La Mantia I, De Vito A, Abita P, Vicini C (2021) Barbed suture extrusion and exposure in palatoplasty for OSA: what does it mean? Am J Otolaryngol 42(4):102994. https://doi.org/10.1016/j.amjoto.2021.102994. (Epub 2021 Feb 20. PMID: 33639448)
Moffa A, Giorgi L, Cassano M, Lugo R, Baptista P, Casale M (2022) Complications and side effects after barbed pharyngoplasty: a systematic review. Sleep Breath. https://doi.org/10.1007/s11325-022-02585-3. (Epub ahead of print. PMID: 35217931)
Pang KP, Vicini C, Montevecchi F et al (2020) Long-term complications of palate surgery: a multicenter study of 217 patients. Laryngoscope 130(9):2281–2284. https://doi.org/10.1002/lary.28432
Iannella G, Vallicelli B, Magliulo G et al (2020) Long-term subjective outcomes of barbed reposition pharyngoplasty for obstructive sleep apnea syndrome treatment. Int J Environ Res Public Health 17(5):1542. https://doi.org/10.3390/ijerph17051542. (Published 2020 Feb 27)
Mantovani M, Carioli D, Torretta S, Rinaldi V, Ibba T, Pignataro L (2017) Barbed snore surgery for concentric collapse at the velum: the Alianza technique. J Craniomaxillofac Surg 45(11):1794–1800. https://doi.org/10.1016/j.jcms.2017.08.007
Baptista PM, Diaz Zufiaurre N, Garaycochea O et al (2022) TORS as part of multilevel surgery in OSA: the importance of careful patient selection and outcomes. J Clin Med 11(4):990. https://doi.org/10.3390/jcm11040990. (Published 2022 Feb 14)
Thaler ER, Rassekh CH, Lee JM, Weinstein GS, O’Malley BW Jr (2016) Outcomes for multilevel surgery for sleep apnea: obstructive sleep apnea, transoral robotic surgery, and uvulopalatopharyngoplasty. Laryngoscope 126(1):266–269. https://doi.org/10.1002/lary.25353. (Epub 2015 Jul 7 PMID: 26153069)
Ravesloot MJ, de Vries N (2011) One hundred consecutive patients undergoing drug- induced sleep endoscopy: results and evaluation. Laryngoscope 121:2710–2716
Saenwandee P, Neruntarat C, Saengthong P et al (2022) Barbed pharyngoplasty for obstructive sleep apnea: a meta-analysis. Am J Otolaryngol 43(2):103306–103307. https://doi.org/10.1016/j.amjoto.2021.103306
Mantovani M, Rinaldi V, Torretta S, Carioli D, Salamanca F, Pignataro L (2016) Barbed Roman blinds technique for the treatment of obstructive sleep apnea: how we do it? Eur Arch Otorhinolaryngol 273(2):517–523. https://doi.org/10.1007/s00405-015-3726-2. (Epub 2015 Jul 21 PMID: 26194006)
Vicini C, Meccariello G, Montevecchi F et al (2020) Effectiveness of barbed repositioning pharyngoplasty for the treatment of obstructive sleep apnea (OSA): a prospective randomized trial. Sleep Breath 24(2):687–694. https://doi.org/10.1007/s11325-019-01956-7
Iannella G, Magliulo G, Cammaroto G et al (2022) Effectiveness of drug-induced sleep endoscopy in improving outcomes of barbed pharyngoplasty for obstructive sleep apnea surgery: a prospective randomized trial. Sleep Breath 26(4):1621–1632. https://doi.org/10.1007/s11325-021-02528-4
Friedman M, Ibrahim H, Bass L (2002) Clinical staging for sleep-disordered breathing. Otolaryngol Head Neck Surg 127(1):13–21. https://doi.org/10.1067/mhn.2002.126477
Tsou YA, Hsu CC, Shih LC, Lin TC, Chiu CJ, Tien VH, Tsai MH, Chang WD (2021) Combined transoral robotic tongue base surgery and palate surgery in obstructive sleep apnea syndrome: modified uvulopalatopharyngoplasty versus barbed reposition pharyngoplasty. J Clin Med 10(14):3169. https://doi.org/10.3390/jcm10143169.PMID:34300335;PMCID:PMC8306291
Matarredona-Quiles S, Carrasco-Llatas M, Apodaca PM, Ortega-Beltrá N, Dalmau-Galofre J (2022) Is there a relationship between tonsil volume and the success of pharyngeal surgery among adult patients with obstructive sleep apnea? Braz J Otorhinolaryngol. https://doi.org/10.1016/j.bjorl.2021.12.002
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luca, C., Pasquale, C., Caterina, T. et al. Barbed palatal surgery: single stage or multilevel setting—a systematic review by the Young Otolaryngologists of the Italian Society of Otolaryngology. Eur Arch Otorhinolaryngol 280, 3905–3913 (2023). https://doi.org/10.1007/s00405-023-08018-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08018-5