Abstract
Background
Recently, the use of barbed pharyngoplasty (BP) has become widespread in snoring and obstructive sleep apnoea (OSA) palatal surgery, but there are no studies regarding the short- and long-term complications resulting from these different techniques. This systematic review aimed to report the complications and side effects of different BP techniques.
Methods
An electronic search was performed on PubMed/MEDLINE, Google Scholar, and Ovid databases. The PRISMA statement was followed. Databases were searched from inception through September 2, 2021.
Results
We included 14 prospective clinical studies consisting of 769 patients aged 23 to 81 years. The associated intra-operative complications of BP were as follows: partial thread extrusion (2.9%), self-limited bleeding (2.9%), broken needle (1.0%), and suture rupture (1.0%). Short-term complications were as follows: thread/knot extrusion (12.4%), dysphagia (5.6%), bleeding (1.5%), velopharyngeal insufficiency (1.5%), anterior pharyngoplasty dehiscence (1.2%), tonsillar haemorrhage (1.0%), excessive postnasal discharge (1.0%), barbed suture failure (0.5%), acute infection (0.2%), mucosal granulomas (0.2%), chipped tooth caused by mouth gag displacement (0.2%), and fibrous scar (0.2%). Long-term complications were as follows: foreign body sensation (7.8%), sticky mucus in throat (5.9%), dysphagia (3.6%), rhinolalia (3.1%), throat phlegm (1.1%), nose regurgitation (0.8%), dry throat (0.6%), and throat lump (0.3%).
Conclusion
BP is a safe technique free of significant side effects and major complications. However, in this review, patients undergoing BP were very heterogeneous in terms of characteristics of patients chosen and severity of diseases, surgical technique used (myoresective vs non-myoresective), time of follow-up, and mono level vs multilevel surgery. More studies on a larger scale with long-term follow-up are needed to confirm these promising results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnoea (OSA) is a complex disease characterized by the collapse at the upper airway (UA) during sleep. There may be several sites of obstruction such as the velopharynx, the lateral pharynx, and/or the tongue base. More often than not, the collapse is multilevel. The most common collapse site is the palate. For this reasons, over the years, the surgeons’ attention has turned to intrapharyngeal surgery, evolving from the older uvulopalatopharyngoplasty (UPPP) to the newer reconstructive palatal techniques [1]. To date, due to the high incidence of post-operative discomfort, complications, and lower long-term stability, older techniques have been abandoned in favour of new ones such as expansion pharyngoplasty, lateral pharyngoplasty, and modified barbed reposition pharyngoplasty (BRP) [2]. Barbed pharyngoplasty (BP) has recently become one of the most widely performed intra-pharyngeal surgical techniques in many countries [3]. Barbed sutures are special knot-free self-blocking threads characterized by directional projection called barbs. The use of barbed sutures has shown promising results in OSA patients and snorers with significant surgical success rate [3]. However, although these techniques have become quite widespread, to date, there are no studies about short- and long-term complications resulting from these different techniques. There is only a systematic review [1] on long-term complications after palatal surgery. But this study concerned different surgical techniques (newer and older) and only one BP, in particular BRP introduced by Vicini et al. [4]. Therefore, it would be useful to assess BP complications. This systematic review aimed to report complications and side effects of different BP techniques performed in many different countries.
Materials and methods
A systematic review was conducted on clinical studies on BP. The analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [5].
Data source and study searching
An electronic search was performed on PubMed/MEDLINE, Google Scholar, and Ovid databases. An example of a search strategy is the one used for PubMed/MEDLINE: “Barbed Suture” and “Complication”; “Barbed Suture” and “Post-operative”; “Barbed” and “Pharyngoplasty”; “Barbed” and “Palatoplasty”; “Barbed” and “Anterior Pharyngoplasty”; “Barbed” and “Lateral Pharyngoplasty”; “Barbed” and “Expansion Sphincter Pharyngoplasty”; “Barbed” and “Suspension Pharyngoplasty”; “Barbed” and “Reposition Pharyngoplasty”; “Barbed” and “Snore Surgery”; “Barbed” and “Roman Blinds Technique”; and “Barbed” and “Alianza Technique”. Searches were adjusted to fit the specific requirements for each database. A cross-reference search of the included studies was performed to minimize the risk of missing relevant data. The last search was run in June 2021.
Inclusion/exclusion criteria
The selection of studies was based on original articles that reported post-operative complications derived from the use of different types of BP. Exclusion criteria for the study were as follows: (1) studies not in English; (2) case reports, reviews, conference abstracts, letters, and paediatric studies; (3) studies with unclear and/or incomplete data; and (4) studies not reporting post-operative complication. No publication date restriction was imposed.
Data extraction and data analysis
All articles were initially screened by title and abstract. The full-text version of each publication was assessed and those whose content was judged not to be strictly related to the subject of this review were excluded. Data extraction of the studies included the population demographics and baseline characteristics, details on intervention and control conditions, study designs, and outcomes. A qualitative synthesis analysis was performed considering the selected studies regarding the complications resulting from different BP techniques.
Statistical analysis and summary of findings
It was impossible to perform the intended statistical analysis and summary of findings as described in our protocol due to heterogenic reporting style and lack of data in individual studies included in this review. Thus, the effect on individual outcomes and overall quality assessment were only narratively described. Available data in the retrospective studies were used. Authors of the included studies were not contacted for further information.
Results
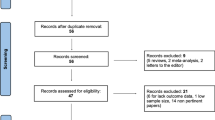
Search criteria returned 36 articles and 19 articles were removed as not relevant or duplicates. The remaining articles were screened and three more were excluded, resulting in 14 articles fulfilling criteria for inclusion in this review. A flow diagram is shown in Fig. 1 (PRISMA Flow Diagram) that depicts the selection process. All the original articles included were prospective clinical studies. The population in the included studies consisted of 769 patients aged 23 to 81 years. The baseline characteristics of these studies are showed in Table 1, and a further description of the studies conducted in the reports can be found in Table 2.
Intra-operative complication studies
Only two studies showed intra-operative complications regarding BRP. Montevecchi et al. [6] recorded in 103 patients the following complications: partial thread extrusion (3), intra-operative self-limited bleeding (3), broken needle (1), and intra-operative suture rupture (1). Pianta et al. [10] performed barbed expansion sphincter pharyngoplasty (BESP) on 17 patients, showing one case of chipped tooth caused by mouth gag displacement.
Short-term complication studies
In 2014, Salamanca et al. performed barbed anterior pharyngoplasty (BAP) on 24 subjects reporting post-operative pain as mild to moderate for the first 5–6 days and then slowly decreased. In many cases (19/24), a short segment of the extremity of the thread partially extruded, and the protruding piece of the suture was cut [7].
Elbassiouny et al. [8] introduced a modified barbed soft palatal posterior pillar webbing flap palatopharyngoplasty on 21 patients with severe OSA, recording some temporary complications (temporary velopharyngeal insufficiency and excessive postnasal discharge) which improved within 1 month after surgery. These investigators showed a significant reduction in pain severity after the first week (week 1, 7.1 ± 0.9; week 2, 1.4 ± 0.5).
In 2017, Mantovani et al. [9] performed the Alianza technique in 19 patients with mild to moderate OSA with concentric palatal collapse and recorded only a few minor complications, such as partial knot extrusions, mucosal granulomas, and anterior pharyngoplasty dehiscence. The Alianza technique was well tolerated in most patients (mean pain VAS scores on day 1, 6.0 ± 1.2; day 7, 2.4 ± 1.4).
Pianta et al. [10] performed a BESP showing 1 case of tonsillar haemorrhage, 1 case of acute post-operative infection, and 1 case of temporary episodic nasal liquid regurgitation, which regressed spontaneously after 2 weeks. No patient complained of post-operative pain.
Regarding the BRP complications described, these were foreign body sensation [4, 11], extrusion of short piece of suture [4, 6], transient dysphagia [6], post-operative bleeding [6], and post-operative pain after 1 week [4].
Barbieri et al. [12] conducted an observational retrospective study, and patients were divided into two groups: 22 patients underwent BRP and 20 barbed suspension pharyngoplasty (BSP). The medium length of hospital stay (range 1–4 days). Complications related to the surgical procedures encompassed one case of haemorrhage from tonsillar bed on 11th post-operative day managed by medical therapy, two cases of temporary velopharyngeal insufficiency, spontaneously solved before the discharge, and five cases of minimal partial thread extrusion (four among BRP group and one case among BSP one), that were treated by cutting the suture in the outpatient clinic.
Carrasco Llatas et al. [13] showed results after modified reposition pharyngoplasty (MRP) on 26 patients with mild to severe OSA with latero-lateral collapse. They reported post-tonsillectomy haemorrhaging in 2 patients (who required surgical review), nasopharyngeal insufficiency during the first week in two patients, and partial suture extrusion in thirteen of them.
Three studies explicitly reported no complications in a total of 92 patients [14]–[16].
Long-term complication studies
Two studies reported long-term post-operative complications. Pang et al. [1] recorded complications derived from 40 cases of BRP (mean 41.3 months of follow-up). Only seven patients had a bad feeling in the throat. These symptoms included foreign body sensation in one case, dry throat in two cases, and phlegm in four cases. Iannella et al. [17] evaluated subjective outcomes of BRP using a specific questionnaire named palate post-operative problem score (PPOPS), after an average time interval between surgery and the interview of 26 months (2–56 months). At the time of the PPOS interview the following data were recorded: mild to moderate dysphagia (9%), rhinolalia (8%), presented nose regurgitation (2%), foreign body sensation (20%), and sensation of sticky mucus in throat (15%). Painful sensation in the throat immediately after surgery was a very common problem but decreased over time and disappeared at the time of the PPOPS interview.
Discussion
Currently, there are no reviews in the literature about the short and long-term complications that occur after the different BP techniques. Most studies included in this review recorded intra-operative and short-term complications (13 studies, Table 1), while only two studies analysed long-term complications [1, 17].
From the 13 studies regarding short-term complications, it was found that thread/knot extrusion was the most frequent, followed by dysphagia, and both were found to be temporary. Indeed, even if partial knot extrusion can lead to stinging pain and foreign body sensation, it can be easily managed in the outpatient setting by removing the extrusion with forceps or cutting instruments, preferably at least 3 weeks after surgery in order to avoid impairing the scarring process. Other complications were post-operative bleeding and velopharyngeal insufficiency, tonsillar haemorrhage, and excessive postnasal discharge (1%). Barbed suture failure, acute post-operative infection, chipped tooth caused by mouth gag displacement, and fibrous scar occurred rarely. Also, mucosal granulomas occurred rarely and spontaneously improved after a few weeks of daily mouthwashes, and the anterior pharyngoplasty dehiscence spontaneously heals without any functional impairment within 3–4 weeks.
Another common complication is post-operative pain. Unfortunately, not all authors showed pain information, and many of them did not specify how many patients complained of it, so it was not possible to quantify this side effect. However, pain is typically present during the firsts post-operative days and tends to gradually disappear over 1 week [4, 8, 9]. Rinaldi et al. [20] observed that the post-operative pain was significantly less in the patients if low temperature plasma surgery was employed.
Concerning the longer-term complications after BRP [1, 17], patients infrequently experienced dry throat, throat lump, throat phlegm, mild and moderate dysphagia, rhinolalia, nose regurgitation, foreign body sensation, and a sensation of sticky mucus in the throat. The authors [17] considered rhinolalia and nasal regurgitation caused by velopharyngeal insufficiency as minor and occasional BRP-related complications.
For the management during the post-operative days, in the common clinical practice, it is recommended to give the same instructions for diet, activity, and pain relievers usually indicated after tonsillectomy. On average, post-operative pain lasts 2 or 3 days, and recovery is quick (within 1 week), but, if a tonsillectomy has been performed, patients should be strongly advised not be far from a medical facility at least for 2 weeks [18]. To manage the pain, it is advised to administer 1 g of paracetamol, 3 times a day for 5–7 days for analgesia and, if the pain is severe, in addition Ibuprofen. For the first 24 h after surgery, the patient should follow a liquid diet and then a soft diet for the next 2 weeks. Chlorhexidine mouthwashes after each meal are also recommended during the first post-operative week. After 2 weeks, the patient can come back to normal diet [19].
Several studies have shown that over the years, UPPP and other older palatal surgery techniques were associated with a high incidence of unfavourable post-operative complications and comorbidities such as dysphagia, rhinolalia, velopharyngeal insufficiency and nasopharyngeal regurgitation, phlegm in throat, and abnormal scarring with velopharyngeal stenosis. Throat discomfort and foreign body sensation may also occur due to fibrotic scar on the palatal edge caused by the tissue resection [17]. So, compared to the older techniques, these newer palatal surgery techniques (including BPs) based on reconstructive principles respecting the lateral pharyngeal walls and preserving some or part of the uvula are expected to have fewer long-term post-operative complications and comorbidities [17]. However, these new BP techniques differ mainly on the management of the palatopharyngeus muscle (PPM). The PPM is one of the crucial muscles involved in swallowing of food, opening the upper oesophageal sphincter. It is also known that the PPM assists in the phonation of high-pitched sounds and it is active in the production of oral and nasal speech sounds [21]. It is well known that cutting this muscle may expose the patient to an increased risk of late dysphagia especially in old age. In the era of the mini-invasive/conservative surgery, such muscle resection is questionable [22].
Dysphagia is often an underreported OSA problem, with an estimated prevalence range of 16 to 78%, as outlined in a recent systematic review. Even if the underlying pathophysiology of dysphagia in OSA has not yet been well understood, it has been hypothesized that low-frequency vibrations, intermittent hypoxia, frequent stretching, and inflammatory changes alter afferent mechanisms of the pharynx. These sensory alterations may lead to dysregulation of afferent inputs resulting in difficulty in swallow initiation. Together, these changes alter central respiratory-swallow integration [23]. For these reasons, sleep surgeons should determine if swallow dysfunction is present in the pre-operative assessment [24].
A crucial aspect that should be considered is that many of the post-operative complications after palatal surgery are related to the patient’s subjective perceptions. Therefore, to evaluate surgical outcome accurately, it is necessary to explore subjective perception, similar to Rashwan et al. [25] who designed a questionnaire, the palate post-operative problem score (PPOSS). This questionnaire investigates the patient’s perception and the most common problems arising after surgery in the short and long term.
Currently, there are no comparative studies on medium and long-term complications between the different BPs. Furthermore, no study has shown the superiority of one type of BP over other techniques in terms of results or complications. Given the extreme heterogeneity of the studies analysed, it is necessary to perform randomized controlled studies with larger samples aiming to define the best BP technique according to effectiveness, surgical success rate, patient adherence, and complications [3].
Conclusions
In conclusion, BP is a safe technique free of significant side effects and major complications. However, it is essential to specify that the studies included in this review were very heterogeneous in terms of characteristics of patients, disease severity, surgical technique used (myoresective vs non-myoresective), follow-up, and mono level vs multilevel surgery.
References
Pang KP et al (2020) Long-term complications of palate surgery: a multicenter study of 217 patients. Laryngoscope 130(9):2281–2284. https://doi.org/10.1002/LARY.28432
Martínez-Ruíz de Apodaca P, Carrasco-Llatas M, Matarredona-Quiles S, Valenzuela-Gras M, Dalmau-Galofre J (2021) Long-term stability of results following surgery for obstructive sleep apnea (OSA). Eur Arch Oto-Rhino-Laryngology. https://doi.org/10.1007/s00405-021-06781-x
Moffa A et al (2020) “Different barbed pharyngoplasty techniques for retropalatal collapse in obstructive sleep apnea patients: a systematic review,.” Sleep and Breathing 24(3):1115–1127. https://doi.org/10.1007/s11325-020-02088-z
Vicini C et al (2015) Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. ‘We are on the giant’s shoulders.’ Eur Arch Oto-Rhino-Laryngology 272(10):3065–3070. https://doi.org/10.1007/s00405-015-3628-3
A. Liberati et al., 2009 “The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration.,” BMJ, vol. 339, https://doi.org/10.1136/bmj.b2700.
Montevecchi F et al (2018) Prospective multicentre study on barbed reposition pharyngoplasty standing alone or as a part of multilevel surgery for sleep apnoea. Clin Otolaryngol 43(2):483–488. https://doi.org/10.1111/coa.13001
F. Salamanca et al., “Barbed anterior pharyngoplasty: an evolution of anterior palatoplasty.,” Acta Otorhinolaryngol. Ital., vol. 34, no. 6, pp. 434–438, 2014, [Online]. Available: http://www.ncbi.nlm.nih.gov/pubmed/25762837%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4346991.
Elbassiouny AMME (2016) Modified barbed soft palatal posterior pillar webbing flap palatopharyngoplasty. Sleep Breath 20(2):829–836. https://doi.org/10.1007/s11325-016-1335-y
Mantovani M, Carioli D, Torretta S, Rinaldi V, Ibba T, Pignataro L (2017) Barbed snore surgery for concentric collapse at the velum: the Alianza technique. J Cranio-Maxillofacial Surg 45(11):1794–1800. https://doi.org/10.1016/j.jcms.2017.08.007
Pianta L, Bertazzoni G, Morello R, Perotti P, Nicolai P (2018) Barbed expansion sphincter pharyngoplasty for the treatment of oropharyngeal collapse in obstructive sleep apnoea syndrome: a retrospective study on 17 patients. Clin Otolaryngol 43(2):696–700. https://doi.org/10.1111/coa.13008
Madkikar N, Pandey S, Ghaisas V (2019) Multi level single stage: barbed reposition pharyngoplasty and nasal surgery in treatment of OSA—our experience. Indian J Otolaryngol Head Neck Surg 71(3):309–314. https://doi.org/10.1007/s12070-019-01694-y
Barbieri M et al (2019) Barbed suspension pharyngoplasty for treatment of lateral pharyngeal wall and palatal collapse in patients affected by OSAHS. Eur Arch Oto-Rhino-Laryngology 276(6):1829–1835. https://doi.org/10.1007/s00405-019-05426-4
Carrasco Llatas M, Valenzuela Gras M, Martínez Ruiz de Apodaca P, DalmauGalofre J (2021) “Modified reposition pharyngoplasty for OSAS treatment: how we do it and our results,.” Acta Otorrinolaringol 72(3):152–157. https://doi.org/10.1016/j.otoeng.2020.02.015
Mantovani M, Rinaldi V, Torretta S, Carioli D, Salamanca F, Pignataro L (2016) Barbed Roman blinds technique for the treatment of obstructive sleep apnea: how we do it? Eur Arch Oto-Rhino-Laryngology 273(2):517–523. https://doi.org/10.1007/s00405-015-3726-2
Vicini C, Meccariello G, Cammaroto G, Rashwan M, Montevecchi F (2017) “La barbed reposition pharyngoplasty nella chirurgia multilivello robotica per il trattamento delle apnee ostruttive in sonno,.” Acta Otorhinolaryngol Ital 37(3):214–217. https://doi.org/10.14639/0392-100X-1203
Vicini C et al (2020) Effectiveness of barbed repositioning pharyngoplasty for the treatment of obstructive sleep apnea (OSA): a prospective randomized trial. Sleep Breath 24(2):687–694. https://doi.org/10.1007/s11325-019-01956-7
Iannella G et al (2020) “Long-term subjective outcomes of barbed reposition pharyngoplasty for obstructive sleep apnea syndrome treatment,.” Int. J. Environ. Res. Public Health 17(5):1542. https://doi.org/10.3390/IJERPH17051542
V. Rinaldi et al., “The efficacy of barbed sutures for anterior pharyngoplasty: technical aspects and preliminary results.,” J. Biol. Regul. Homeost. Agents, vol. 34, no. 5 Suppl. 3, pp. 123--126. Technology in Medicine, 2020, [Online]. Available: https://europepmc.org/article/med/33386042.
Dachuri S et al (2018) Barbed reposition pharyngoplasty in Indian population: a new palatal surgery for OSAS. Indian J Otolaryngol Head Neck Surg 71(2):249–253. https://doi.org/10.1007/S12070-018-1320-9
Rinaldi V et al (2019) “Postoperative pain and wound healing after coblation-assisted barbed anterior pharyngoplasty (CABAPh): an observational study.” Indian J Otolaryngol Head Neck Surg 71(Suppl 2):1157–1162. https://doi.org/10.1007/s12070-018-01577-8
Ezzat AM, El-Shenawy H (2015) Palatopharyngeus the missing palatal muscles: anatomical and physiological review. Ann Maxillofac Surg 5(2):226. https://doi.org/10.4103/2231-0746.175768
Casale M, Moffa A, Pignataro L, Rinaldi V (2021) Palatopharyngeus muscle in pharyngoplasty surgery for OSAS: cut or not to cut? Eur Arch Oto-Rhino-Laryngology 278(7):2657–2658. https://doi.org/10.1007/S00405-021-06761-1
Schar M et al (2018) “Pathophysiology of swallowing following oropharyngeal surgery for obstructive sleep apnea syndrome,.” Neurogastroenterol. Motil 30(5):e13277. https://doi.org/10.1111/nmo.13277
Bhutada AM, Broughton WA, Focht Garand KL (2020) “Obstructive sleep apnea syndrome (OSAS) and swallowing function-a systematic review,.” Sleep Breath 24(3):791–799. https://doi.org/10.1007/S11325-020-02037-W
Rashwan MS et al (2018) Let’s know from our patients: PPOPS score for palate surgery evaluation/a pilot study. Eur Arch Otorhinolaryngol 275(1):287–291. https://doi.org/10.1007/S00405-017-4795-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
No institutional review board approval was necessary because of the nature of this project.
Informed consent
This article does not contain any studies with human participants or live animal performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moffa, A., Giorgi, L., Cassano, M. et al. Complications and side effects after barbed pharyngoplasty: a systematic review. Sleep Breath 27, 31–38 (2023). https://doi.org/10.1007/s11325-022-02585-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02585-3