Abstract
Introduced in the late 90s, the active middle ear implant Vibrant Soundbridge (VSB) is nowadays used for hearing rehabilitation in patients with mild to severe sensorineural hearing loss (SNHL) unable to tolerate conventional hearing aids. In experienced hands, the surgical implantation is fast done, safe and highly standardized. Here, we present a systematic review, after more than 15 years of application, to determine the efficacy/effectiveness and cost-effectiveness, as well as patient satisfaction with the VSB active middle ear implant in the treatment of mild to severe SNHL. A systematic search of electronic databases, investigating the safety and effectiveness of the VSB in SNHL plus medical condition resulted in a total of 1640 papers. After removing duplicates, unrelated articles, screening against inclusion criteria and after in-depth screening, the number decreased to 37 articles. 13 articles were further excluded due to insufficient outcome data. 24 studies remained to be systematically reviewed. Data was searched on safety, efficacy and economical outcomes with the VSB. Safety-oriented outcomes included complication/adverse event rates, damage to the middle/inner ear, revision surgery/explant rate/device failure and mortality. Efficacy outcomes were divided into audiological outcomes, including hearing thresholds, functional gain, speech perception in quiet and noise, speech recognition thresholds, real ear insertion gain and subjective outcomes determined by questionnaires and patient-oriented scales. Data related to quality of life (QALY, ICER) were considered under economical outcomes. The VSB turns out to be a highly reliable and a safe device which significantly improves perception of speech in noisy situations with a high sound quality. In addition, the subjective benefit of the VSB was found to be mostly significant in all studies. Finally, implantation with the VSB proved to be a cost-effective and justified health care intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Introduced in the late 90s, the active middle ear implant Vibrant Soundbridge (VSB) is used for hearing rehabilitation in patients with mild to severe sensorineural hearing loss (SNHL) unable to tolerate conventional hearing aids (HAs). VBS can be also used in the treatment of conducting or mixed hearing loss with a suitable vibratory structure to benefit from amplification, as for reconstruction of the hearing after cholesteatoma or ear surgery with good benefit.
SNHL originates from a deterioration of the inner ear function and can be acquired or congenital. Acquired SNHL is the most common reason of hearing loss, affecting 20–30% of the population, mainly the elderly due to age related deterioration of the sensory function, but also younger people due to noise exposure or ototoxic events [1, 2].
In cases with mild to severe SNHL, HAs are commonly fitted matching the residual hearing. HAs may provide adequate amplification for many patients, however, there are limitations ranging from acoustic feedback, gain limitations, sound and voice distortion, frequent servicing and maintenance of their devices or discontinued use, due to discomfort. Moreover, conventional HAs generally occlude the ear canal, which may exacerbate conditions such as otitis externa and media. It is estimated that only one fifth of the individuals, who would benefit from an acoustic hearing device, actually own a HA. In addition, 12% who own a HA never use it [3]. Of those, who regularly wear a HAs, only 58% are fully satisfied with their HA [4].
For candidates that cannot benefit from conventional external amplification for medical reasons, such as external otitis, external ear aplasia, external ear skin irritations or not enough amplification with conventional HAs, implantable middle ear prostheses, such as the VSB have been used since 1996. The principle of this middle ear implant is based on the direct drive of the ossicular chain using mechanical vibrations, relayed via an implanted transducer. Implantation involves a surgical procedure under general anesthesia. The vibrating ossicular prostheses (VORP) is implanted subcutaneously and the floating mass transducer (FMT) is crimped to the long process of the incus, the stapes footplate or suprastructure, or is coupled to the round window via surgery known as Vibroplasty. The audioprocessor, worn externally and hold in place by a magnet, receives the audio signals by a microphone system and sends them to the VORP which converts it into mechanical vibrations carried out by the FMT. The transducer vibrates the ossicular chain and delivers frequency information up to 8 kHz.
In experienced hands the implantation is fast done, safe and highly standardized. Like in all operations of the middle ear, complications may occur compromising chorda tympani or facial nerve damaging or inner ear deterioration.
After more than 15 years of application, a systematic review of evidence from existing research on the safety, efficacy/effectiveness, patient satisfaction and economical outcomes of the VSB for the treatment of mild to severe SNHL plus medical condition, which does not allow treatment with HAs, was performed following the Cochrane Collaboration Guidelines and the PRISMA statement [5].
The main question to be addressed was whether the VSB is the most appropriate treatment for the above mentioned population.
Materials and methods
Methods of the inclusion criteria, procedures and analysis were determined following the guidelines of the Cochrane Collaboration Handbook.
Study eligibility criteria
Electronic databases were searched to identify systematic reviews, meta-analysis and clinical trials published as of December 2012. All papers were assessed against the set “PICOS” below.
Participants
Subjects of any age, gender or ethnicity with mild to severe SNHL of any etiology in one or both ear(s) who failed all other conservative medical, surgical, pharmaceutical treatment and could not benefit from conventional HAs were included. Subjects with mixed or conductive hearing loss or profound unilateral hearing loss were excluded.
Intervention
The intervention included was unilateral implantation with the VSB middle ear implant by means of incus vibroplasty. Any surgical approach was considered.
Comparators
Unilateral VSB implantation was compared to receiving no surgical intervention and to the Esteem and Carina fully implantable hearing devices.
Outcomes
Data was searched on safety, efficacy and economical outcomes with the VSB. Safety-oriented outcomes included complication/adverse event rates, damage to the middle ear/inner ear revision surgery/explant rate/device failure and mortality. Efficacy outcomes were divided into audiological outcomes (hearing thresholds, functional gain, speech perception in quiet and noise, speech recognition thresholds, real ear insertion gain) and subjective outcomes (questionnaires and scales). Data related to quality of life (QALY, ICER) were considered under economical outcomes.
Study design
Systematic reviews, meta-analysis, clinical studies, including randomized or non-randomized comparative studies, case series, case–control studies, controlled/uncontrolled before-and-after studies and interrupted time series (ITS) analysis were included. Non-systematic reviews, case reports, letters, editorials, animal, in vitro/laboratory studies and clinical studies n < 5 were excluded.
Study identification and search strategy
The electronic databases search included the Cochrane Consumers and Communication Review Group Specialised Register, PubMed (MEDLINE), OVIDSP (EMBASE), NHSEED (CRD) and the Turning Research into practice database (TRIP). Relevant papers, authors and citied references were cross-checked using PUBMED and Journal/Author Name Estimator (JANE).
Study selection
Following the deletion of duplicates, all articles found to be not related to the middle ear implants were removed from the review. The titles and abstracts of the remaining articles were screened against the “PICOS” described above. The full texts of articles matching the inclusion criteria were obtained for further evaluation. Studies were excluded, if they still did not fulfill the eligibility criteria or if the study was of low quality. All articles selected were screened again for qualitative data synthesis by two independent authors with discrepancies resolved by discussion or consulting a third reviewer. Inter-rater reliability was calculated using Cohen’s kappa statistic [6] which revealed good to strong agreement between the authors at the two levels of full text selection (r = 0.74 and r = 0.95, respectively).
Data extraction
A data extraction sheet was developed according to the Cochrane Consumers and Communication Review Group [7], piloting the template on three randomly selected included articles and subsequently refining it. Data were extracted, if reported in the text or tables or if it could be accurately calculated from graphs, figures or raw data sets. Information was extracted from each article on (1) sample characteristics (age, gender, etiology, diagnosis, treatment received/receiving), (2) type of intervention (use of HAs, surgical approach, audio processor type) and (3) type of outcome measures (testing intervals, surgical complications, pure tone thresholds, sound field thresholds, functional gain, hearing preservation, speech perception/recognition, APHAB, GBI). The evidence level presented in the selected studies was assessed and classified according to the Oxford Centre for Evidence-based Medicine (2011).
Assessment of study quality
The quality of each study was assessed using a checklist available from the Evidence Analysis Library, Academy of Nutrition and Diabetics [8], making it possible to identify bias in prospective designs. The quality or validity of the studies was determined by the number of items ticked.
Data synthesis
The effect of treatment was primarily measured by the mean change in pure tone averages, speech perception and subjective ratings after receiving the VSB, as well as by determining the occurrence of adverse events postoperatively on all primary outcomes along with tabulated study characteristics.
Results
Search results
The systematic search of electronic databases for studies investigating the safety and effectiveness of the VSB in SNHL plus medical condition resulted in a total of 1640 papers. The number decreased to 209 after removing duplicates and unrelated articles. These results were screened against inclusion criteria, resulting in 86 being kept for in-depth screening. 49 articles were excluded due to irrelevant study design, only mixed HL, no or incorrect description of outcomes, no original data being reported or insufficient reporting of statistical tests. Of the remaining 37 articles, 13 were excluded due to insufficient outcome data or inability to extract tabulated data. 24 studies remained to be systematically reviewed (Diagram A, Supplemental Digital Content 1).
Study characteristics and quality
Included in the 24 studies were 22 original articles, one conference proceeding [9] and one FDA Report on the Esteem implant [10]. 23 studies were conducted in Europe, one in the US [11]. The articles covered a total of 679 participants with a sample size from n = 5–125. Moreover, Labassi and Beliaeff [9] reviewed a total of 1100 cases on the safety of the VSB. All participants were 18–86 years and diagnosed with pure SNHL in 16 studies and SNHL plus medical condition in six studies. Follow-up time in most studies ranged from 2 to 24 months, with long-term results reported up to 11 years postoperatively. According to the Oxford levels of evidence, 14 studies had level 4 and nine studies level 3 evidence.
Of the 22 original articles, 12 pro-and ten retrospective studies have been identified. Patients served as their own control. Postoperative performance with the VSB was compared to unaided or preoperative HA performance. Sample characteristics and inclusion/exclusion criteria were sufficiently described in 17 papers, including an adequate follow-up method and period in 14 papers. In five studies withdrawals or patients lost of follow-up (<20%) were reported. The intervention was sufficiently described in all studies with extra/unplanned treatments in 13 papers. Statistical analysis of outcome data was performed correctly in 17 studies. One study used an inappropriate parametric test, their significance values were not considered within this review [12]. Negative findings, bias and study limitations were reported in seven studies. A conflict of interest was indicated in three prospective studies [13–15].
Results of individual studies
Safety
The safety of the VSB was assessed by either calculating the amount of hearing preservation or the occurrence of adverse events. Ten studies investigated hearing preservation of 375 patients and seven studies investigated adverse events of 1398 patients.
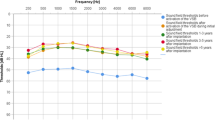
Hearing preservation was reported as the shift in unaided pure tone averages (PTA) with a different range of frequencies from 0.5 to 6 kHz (Fig. 1). Most studies reported a clinically non-significant shift of 1–3 dB [16]. Schmutziger et al. [17] reported a significant shift of 8 dB after surgery. This could be related to the timing of hearing threshold measurement, as they tested patients 2 years after implantation, whereas others reported PTA shifts of 2.75 dB at 12 months [18] or 1 dB at 18 months [19]. Moreover, Schmutziger et al. [17] described several surgery related complications and side effects, while Todt et al. [19] reported no surgical complications.
Adverse events occurring with VSB implantation were in general low, presenting mainly aural fullness (27%) or taste disturbances (9%) (Table 1). Implant failures from a batch of first generation VSBs, explanted due to a conductor lead breakage, were reported with 14% [9]. The number of implant failures improved with the next generation device and the implant was exposed to higher quality assessment. The most common reasons for revision surgery were implant failure (36.8%), problems with FMT fixation during surgery or dislocation postoperative due to MRI or fibrous tissue (18.4%). Pooling the numbers of implant failures across the studies, the rate of 2.6% was much lower compared to the failure rate of first generation implants.
Audiological outcomes: functional gain
15 studies reported on sound field audiometry to calculate the functional gain obtained with the VSB. Two publications measured pure tone averages over different frequency ranges from 1 to 6 kHz in 38 patients at activation [20] and from 1 to 3 kHz in seven patients [21]. 13 publications reported the results as PTA4 measured over 0.5–4 kHz in a total of 370 patients (Fig. 2a). On average, the functional gain with the VSB ranged from 12.5 to 33 dB HL, with a higher range of 25–33 dB HL in studies n > 30 [11, 15, 22, 23]. In three publications [11, 14, 19], results with the analog (A) and digital audio processor (D) were displayed (Fig. 2a). In three cases [15, 18, 22], the audio processor type was not specified.
A comparison of the hearing benefit with the VSB and HAs within the frequency range of 0.5–4 kHz was performed by seven independent studies (Fig. 2b). In six studies of 108 patients, the functional gain was significantly better with the VSB plus digital audio processor, with a gain from 12.9 to 33.4 dB HL for the VSB and 7.5–27 dB HL for HAs. Only Saliba et al. [18], reported a worse FGVSB than for HAs (FGVSB = 18 dB HL vs FGHA = 27 dB HL).
Audiological outcomes: speech perception in quiet and noise
Speech tests were conducted by several studies; however, there was large variety in the type of tests, including differences in settings/conditions and in the amount of data reported.
Considering speech in quiet, various approaches were taken. Snik et al. [24], assessed phoneme recognition, while the majority assessed speech perception at a word level using lists of monosyllables (Hungarian monosyllables [21], NU-6 word lists [11], Freiburger monosyllables [12, 19, 23, 25–28] or disyllabic words [French Fournier’s word lists: 15, 18, 22, 29–31]. Böheim et al. [26] also used a plurisyllabic Freiburger number test in combination with monosyllabic word lists.
Figure 3 displays studies with the Freiburger monosyllable word lists in quiet at 65 dB SPL. Boeheim et al. [26], Pok et al. [23] and Todt et al. [19] provided a comparison of VSB and HAs, thereby Pok and Todt significantly favored the VSB. Comparing unaided and aided conditions with the VSB, speech perception improved from ~30 to ~60% with VSB. Even when the speech perception in the unaided situation was as good as 56%, an improvement of ~30% in the aided condition could be reported [19].
French disyllabic test in quiet was used in several publications, using different methods [15, 18, 22, 31]. Even more heterogeneity in the methods was reported on speech perception in noise by ten studies, presenting eight different speeches in noise tests of 177 patients (Table, Supplemental Digital Content 2). In both settings, the test scores improved with the VSB.
Subjective outcomes
Ten studies investigated the subjective outcomes of the VSB of 373 patients. Seven different self-assessment scales were used with the most frequent ones being the APHAB and the Glasgow Benefit Inventory (GBI). Five studies implemented the APHAB, drew comparisons between the VSB and preoperatively worn HAs (Fig. 4a). Patients seem to have most difficulty in listening in background noise and least difficulty in communicating. A comparison of the mean response profile of the VSB with HAs revealed that patients present less difficulty on all subscales with the VSB (Fig. 4b). In all studies comparing VSB and HA benefit, differences between the subscales were mostly found significant.
VSB users’ performance on GBI is provided in Fig. 4c. A similar amount of benefit was reported by three studies, except one [32]. Snik et al. [32] evaluated patients with chronic otitis externa and SNHL who received a VSB or an Otologics middle ear transducer (MET). The results on the GBI were not reported separately for the implants which might be a reason for the different outcome.
Cost utility
Information on the economic impact of the middle ear implants (MEI) in general is limited. Only five studies or systematic reviews dealing with economic analysis could be identified. The quality of the evaluation was low. One study comprised a systematic review of studies [33], describing the effect of MEIs on quality of life, the results of which were used to infer cost-effectiveness. In general, costs captured were limited to those related to the procedure/implantation of the device.
Primary studies on cost-effectiveness
Snik et al. [32] investigated the cost-effectiveness of MEI in patients with chronic otitis externa. In the context of the Dutch health care system, the cost per QALY of MEI implantation was calculated to be € 18,655. The authors conclude that “middle-ear implantation proved to be a cost-effective and justified health care intervention for the treatment of hearing impaired patients with severe external otitis”. In Scandinavia, Edfeldt et al. [34] conducted a cost-utility study of VSB implantation, presenting a cost per QALY of € 7259 for SNHL, compared to € 12,502 for conductive and mixed HL.
Comparison to WTP data
Each health system defines a willingness to pay (WTP) threshold. Shiroiwa et al. [35] investigated the WTP in Japan, South Korea, Taiwan, UK, Australia and US. Figure 5 shows the data of Shiroiwa et al., (converted into Euro) in comparison to the reported costs by Snik et al. [32] and Edfeldt et al. [34]. The graph shows that actual costs per QALY lie below the defined WTP threshold in all countries, which indicates that middle ear implantation with the VSB is cost-effective.
Discussion
During the past decade, the application of the active middle ear implant VSB in cases of SNHL has been topic of many publications. To achieve a statistical relevant conclusive result in an adequate amount of cases, this systemic review has been undertaken to examine the safety, effectiveness and patient satisfaction with VSB in the treatment of mild to severe SNHL.
The study selection followed the standardized procedure for systematic reviews, based on the Cochrane guidelines. A template was used to extract the data with assessment of the evidence presented in the selected studies using the levels of evidence defined by the Oxford Centre for Evidence-based Medicine (2011). 24 publications of initially 1640 identified, could be systematically reviewed for safety, efficacy and economical outcomes with the VSB.
The safety of the VSB was assessed by either calculating the amount of hearing preservation or the occurrence of adverse events. Discussing the safety data of the VSB to other active middle ear implants, it is relevant to identify products that cover the same indication. The most suitable comparison is the active middle ear implant Esteem [10], which also is implanted by an antrotomy, posterior tympanotomy approach to the long process of the incus.
The literature review revealed data of 3562 VSB cases (Table 1) compared to 56 Esteem cases (Table, Supplemental Digital Content 3). The rate of surgery related complications implanting the device is ranging from 2 to 9% in the VSB patients (Table 1), compared to 5–44% in the Esteem patients. The leading symptoms of the in general low adverse events of the VSB were associated with complications occurring during routine middle ear surgery, taste disturbances, middle ear effusion, aural fullness, predominantly resolving over time. The surgical steps of VSB implantation did not relevantly change the measured pure tone audiometric results, little shifts of 1–3 dB could also be directly attributed to surgical remnants, like scare formation in the middle ear. In comparison to the complications arising from classical middle ear surgery, especially using the posterior tympanotomy approach, the surgical complication rate during implantation of the VSB was not increased.
Revision surgery was needed in cases of implant failure or dislocation after application of the magnetic field of the MRT. Implant failures rates massively decreased with the second generation of VSB development to currently 2.6% of all devices, which is almost half compared to the Esteem data.
The audiological outcome in terms of functional gain is hard to describe in a standardized way, since not all authors mentioned which audio processor they used. According to the date of publication, the predominant numbers of patients might have been supplied with the newer digital processor AP404 released in 2000, compared to earlier analog versions which clearly leads to improved hearing outcome (Fig. 2). Although the numbers are small to be comparable in the overall calculation, the VSB provided a functional gain from 25 to 33 HL in sound field audiometry and pure tone averages over different frequency ranges [11, 15, 22, 23]. In addition, the functional gain showed a markedly better outcome for the VSB plus digital audio processor to conventional behind the ear HAs (Fig. 2b).
The speech perception in quiet and noise is a major tool to evaluate the functionality and dynamic range of a HA. The more publications referred to the topic, the more apparent became the variety of testing tools. The most compact group that could be discussed, applied the Freiburger Sprachtest at 65 dB (Fig. 3). In this setting, the VSB leaded to an improvement of speech understanding of ~30% from unaided to aided conditions with the VSB and showed a significant better speech understanding compared to conventional HAs [19, 23].
Discussing the subjective evaluation of the VSB implantation, the number of available testing tools again outweighs the results. Only five eligible studies drew comparisons between the VSB and preoperatively worn HAs, revealing patients having much less difficulty on all subscales with the VSB (Fig. 4). In all comparative studies, patients benefit from a VSB or HA. However, the VSB is described as much more comfortable, clearer in sound perception and with less events of unease.
Considering the economical benefit of the VSB implantation, there is little information on the economic impact of the MEIs available (Fig. 5) and the overall quality of the evaluations based on published guidelines for economic evaluations in health care is low. In general, costs captured were limited to those related to the procedure. In comparison to WTP threshold data, an implantation with the VSB is cost-effective (Fig. 5).
In conclusion, the VSB turns out to be a highly reliable device which significantly improves perception of speech in noisy situations with a high sound quality and can be a safe tool in surgically experienced hands. Nonetheless, more standard operating procedures to compare functional outcomes or measure subjective qualities of VSB device performance are necessary to increase the validity of measured data.
References
Lin HW, Bhattacharyya N (2011) Otologic diagnoses in the elderly: current utilization and predicted workload increase. Laryngoscope 121:1504–1507
Wilson DH, Walsh PG, Sanchez L, Davis AC, Taylor AW, Tucker G, Meagher I (1999) The epidemiology of hearing impairment in an Australian adult population. Int J Epidemiol 28:247–252
Kochin S (1992) MarkeTrak III identifies key factors in determining consumer satisfaction. Hear J 458:39–44
Kochin S (1992) MarkeTrak III identifies key factors in determining consumer satisfaction. Hear J 458:47–54
Moher D, Liberati A, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. PLoS Med 6(7):e1000100. doi:10.1371/journal.pmed.1000100
Cohen JA (1960) A coefficient of agreement for nominal scales. Educ Psychol Measur 20:37–46. doi:10.1177/001316446002000104
Cochrane Consumers and Communication Review Group (2015) http://www.latrobe.edu.au/chcp/cochrane/resources.html. Accessed Aug 2015
Evidence Analysis Library, Academy of Nutrition and Diabetics (2015) http://andevidencelibrary.com/topic.cfm?cat=1317&auth=1. Accessed Aug 2015
Labassi S, Beliaeff M (2005) Retrospective of 1000 patients implanted with a Vibrant Soundbridge middle-ear implant. Cochlear Implants Int 6(Suppl 1):74–77. doi:10.1002/cii.294
FDA (2010) Esteem safety and effectiveness. Multicenter study. Prospective single arm trial
Luetje CM, Brackman D, Balkany TJ, Maw J, Baker RS, Kelsall D, Backous D, Miyamoto R, Parisier S, Arts A (2002) Phase III clinical trial results with the Vibrant Soundbridge implantable middle ear hearing device: a prospective controlled multicenter study. Otolaryngol Head Neck Surg 126(2):97–107
Todt I, Seidl RO, Ernst A (2005) Hearing benefit of patients after Vibrant Soundbridge implantation. ORL J Otorhinolaryngol Relat Spec 67(4):203–206
Fisch U, Cremers CW, Lenarz T, Weber B, Babighian G, Uziel AS, Proops DW, O’Connor AF, Charachon R, Helms J, Fraysse B (2001) Clinical experience with the Vibrant Soundbridge implant device. Otol Neurotol 22(6):962–972
Fraysse B, Lavieille JP, Schmerber S, Enée V, Truy E, Vincent C, Vaneecloo FM, Sterkers O (2001) A multicenter study of the Vibrant Soundbridge middle ear implant: early clinical results and experience. Otol Neurotol 22(6):952–961
Mosnier I, Sterkers O, Bouccara D, Labassi S, Bebear JP, Bordure P, Dubreuil C, Dumon T, Frachet B, Fraysse B, Lavieille JP, Magnan J, Martin C, Meyer B, Mondain M, Portmann D, Robier A, Schmerber S, Thomassin JM, Truy E, Uziel A, Vanecloo FM, Vincent C, Ferrary E (2008) Benefit of the Vibrant Soundbridge device in patients implanted for 5 to 8 years. Ear Hear 29(2):281–284
Vincent C, Fraysse B, Lavieille JP, Truy E, Sterkers O, Vaneecloo FM (2004) A longitudinal study on postoperative hearing thresholds with the Vibrant Soundbridge device. Eur Arch Otorhinolaryngol 261(9):493–496
Schmuziger N, Schimmann F, àWengen D, Patscheke J, Probst R (2006) Long-term assessment after implantation of the Vibrant Soundbridge device. Otol Neurotol 27(2):183–188
Saliba I, Calmels MN, Wanna G, Iversenc G, James C, Deguine O, Fraysse B (2005) Binaurality in middle ear implant recipients using contralateral digital hearing AIDS. Otol Neurotol 26(4):680–685
Todt I, Seidl RO, Gross M, Ernst A (2002) Comparison of different Vibrant Soundbridge audioprocessors with conventional hearing AIDS. Otol Neurotol 23(5):669–673
Luetje CM, Brown SA, Cullen RD (2010) Vibrant Soundbridge implantable hearing device: critical review and single-surgeon short- and long-term results. Ear Nose Throat J 89(9):E9–E14
Sziklai I, Szilvássy J (2011) Functional gain and speech understanding obtained by Vibrant Soundbridge or by open-fit hearing aid. Acta Otolaryngol 131(4):428–433. doi:10.3109/00016489.2011.557394
Sterkers O, Boucarra D, Labassi S, Bebear JP, Dubreuil C, Frachet B, Fraysse B, Lavieille JP, Magnan J, Martin C, Truy E, Uziel A, Vaneecloo FM (2003) A middle ear implant, the Symphonix Vibrant Soundbridge: retrospective study of the first 125 patients implanted in France. Otol Neurotol 24(3):427–436
Pok SM, Schlögel M, Böheim K (2010) Clinical experience with the active middle ear implant Vibrant Soundbridge in sensorineural hearing loss. Adv Otorhinolaryngol 69:51–58. doi:10.1159/000318522
Snik AF, Cremers CW (2001) Vibrant semi-implantable hearing device with digital sound processing: effective gain and speech perception. Arch Otolaryngol Head Neck Surg 127(12):1433–1437
Böheim K, Nahler A, Schlögel M (2007) Rehabilitation of high frequency hearing loss: use of an active middle ear implant. HNO 55(9):690–695
Boeheim K, Pok SM, Schloegel M, Filzmoser P (2010) Active middle ear implant compared with open-fit hearing aid in sloping high-frequency sensorineural hearing loss. Otol Neurotol 31(3):424–429. doi:10.1097/MAO.0b013e3181cabd42
Lenarz T, Weber BP, Issing PR, Gnadeberg D, Ambjørnsen K, Mack KF, Winter M (2001) Vibrant Sound Bridge System. A new kind hearing prosthesis for patients with sensorineural hearing loss. 2. Audiological results. Laryngorhinootologie 80(7):370–380
Wiedmann J (2010) Die Rehabilitation der Schallempfindungsschwerhörigkeit mittels teilimplantierbarem Vibrant Soundbridge System. Dissertation, University of Ulm
Garin P, Thill MP, Gerard JM (2002) Speech discrimination in background noise with the Vibrant® Soundbridge™ middle ear implant. Otorhinolaryngol Nova 12:119–123
Garin P, Debaty M, Galle C (2005) Hearing in noise with the vibrant Soundbridge middle-ear implant. Cochlear Implants Int 6(Suppl 1):72–74. doi:10.1002/cii.293
Uziel A, Mondain M, Hagen P, Dejean F, Doucet G (2003) Rehabilitation for high-frequency sensorineural hearing impairment in adults with the Symphonix Vibrant Soundbridge: a comparative study. Otol Neurotol 24(5):775–783
Snik AF, van Duijnhoven NT, Mylanus EA, Cremers CW (2006) Estimated cost-effectiveness of active middle-ear implantation in hearing-impaired patients with severe external otitis. Arch Otolaryngol Head Neck Surg 132(11):1210–1215
Snik A, Verhaegen V, Mulder J, Cremers CW (2010) Cost-effectiveness of implantable middle ear hearing devices. Adv Otorhinolaryngol 69:14–19. doi:10.1159/000318517
Edfeldt L, Strömbäck K, Grendin J, Bunne M, Harder H, Peebo M, Eeg-Olofsson M, Petersson CM, Konradsson K (2014) Evaluation of cost-utility in middle ear implantation in the ‘Nordic School’: a multicenter study in Sweden and Norway. Acta Otolaryngol 134(1):19–25. doi:10.3109/00016489.2013.834459
Shiroiwa T, Sung YK, Fukuda T, Lang HC, Bae SC, Tsutani K (2010) International survey on willingness-to-pay (WTP) for one additional QALY gained: what is the threshold of cost effectiveness? Health Econ 19(4):422–437. doi:10.1002/hec.1481
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have read and approved the manuscript and have no conflict of interest related to this paper.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bruchhage, KL., Leichtle, A., Schönweiler, R. et al. Systematic review to evaluate the safety, efficacy and economical outcomes of the Vibrant Soundbridge for the treatment of sensorineural hearing loss. Eur Arch Otorhinolaryngol 274, 1797–1806 (2017). https://doi.org/10.1007/s00405-016-4361-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4361-2