Abstract
Background
Hysteroscopy is an indispensable approach in gynecology. Miniaturization may reduce pain allowing office procedures without anesthesia.
Objectives
Our main objective is to determine if modifications in scope diameters have made office hysteroscopy less painful.
Search strategy
Studies were sought with key words “hysteroscopy” and “pain” from available online sources. Time frame was from 2000 onward. Thirty-three articles were retrieved for detailed analysis.
Selection criteria
Prospective randomized trials, studying pain as main outcome in office hysteroscopy expressed in means, confidence intervals and SD, comparing office mini-hysteroscopy to conventional hysteroscopy. Studies or arms within a study where conscientious sedation, anesthesia or non-steroidal drugs were used were excluded.
Data collection and analysis
We analyzed data from eight studies (seven RCT) comparing mini-hysteroscopy with conventional scopes, involving a total of twenty-three hundred and twenty-two participants, of which nineteen hundred and eighty-six completed the intervention.
Main results
A meta-analysis revealed a significant reduction pain score (MD: −3.64; 95 % CI −5.16 to −2.12; test for overall effect p < 0.00001) and available data support miniaturization decreases pain in outpatient hysteroscopy.
Conclusions
Pain in office hysteroscopy is lower with mini-hysteroscopes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hysteroscopy is a routine technique allowing direct visualization of unsuspected pathology: endometrial hyperplasia, cancer, and other conditions and is considered gold standard in uterine abnormal bleeding. It allows histological sampling cancer staging and foreign bodies can be retracted or inserted into cavity and tubes. Hysteroscopy is useful in infertile women.
Modern mini-hysteroscopes avoid cervical dilation, misoprostol facilitates operations [1, 2], either by vaginal or sublingual administration [3], and the vaginoscopic no-touch approach [4–8] improved tolerance as data in a 2010 systematic review by Cooper [8] demonstrate. Reduction in pain has led to performing examination and even operations without anesthesia [2, 9–11]. Ultrasonography and 3D sonohysterography are not as accurate in diagnosing intrauterine abnormalities [12], and hysteroscopy is generally needed to confirm diagnosis. It also plays an important role in fertility treatment workup [13]. Both rigid and flexible mini-hysteroscopes reduce pain and may be adequate for examination [14] but rigid scopes seem to have superior optical properties [15].
Distension media is important. Plain water can be harmful, glycine and sorbitol/mannitol are adequate for mono-polar electrosurgery, but can provoke fatal outcome. Gas embolization is common, even using normal saline as bipolar electrodes produce bubbles and can be life-threatening. Both CO2 and normal saline are adequate for diagnostic outpatient hysteroscopy [16] as Cooper’s 2010 systematic review on effect on pain concluded, but saline is more convenient if surgery is to be done [17].
Pain is responsible for vasovagal syndrome in 0.21–30 % and leads to halting of procedure. Various interventions [18, 19], medications [20, 21], para-cervical block cocktails, and conscious sedation have been suggested to control pain without convincing results [1, 22–26]. Cengiz [27] compared intrauterine lidocaine and paracervical block and concluded there was no significant difference, but lidocaine has a longer post-operative effect. Two recent systematic reviews in 2010, one by Cooper [24] and another by Ahmad [28] have, however, suggested a reduction of pain with local anesthetic, but “clinical significance of results is limited as the reduction in mean pain score is small” [28]. Success with outpatient technique without anesthesia is associated to very low cost of gynecological care and justifies its generalized use for some authors [5]. Pain perception may vary among population subgroups [29, 30].
A recent paper by Cicinelli [31] summarizes evidence gathered from various studies and sources.
Objectives
Our main objective is to determine if modifications in scope diameters has made office hysteroscopy less painful. While most studies agree that slender hysteroscopes reduce pain, one randomized controlled trial (RCT) from 2005 by Rullo [32] and one prospective cohort study by Torok in 2012 [33] failed to find statistical difference between scope diameters and pain scores. So the question remains: is reduction in hysteroscope diameter associated with lower pain perception?
Search strategy
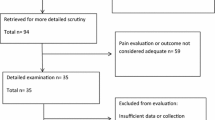
Studies were sought with key words “hysteroscopy” and “pain” from the following sources: Pubmed/Medline (465), Portal de Pesquisa da BVS (214), LILACS (13) CINHAL, Embase and Cochrane database (82) Cochrane systematic reviews (3) DARE systematic reviews (4) IBECS (3) Scielo (8) Global Health Library (GHL), (20) Western Pacific region Health Index (WPRIM) (12) Index Medicus for the Eastern Mediterranean Region (IMEMR) (8), and Index Medicus for South-East Asia Region (IMSEAR) (1) giving a total 834 hits. Time frame was from 2000 onward. After reading titles and eliminating duplicates, 94 abstracts were independently assessed by three authors (A.P., M. S. and C.P.) and of theses, 33 articles retrieved for detailed analysis.
Methods
Ethical and regulatory compliance: This study was conducted in compliance with the protocol, the Declaration of Helsinki, the Good Epidemiological Practice, and all applicable laws and regulations.
Seven papers (including eight studies) were selected from literature sources. Flow chart of selection is specified in Fig. 1.
Using standard meta-analysis software (RevMan 5.0),Footnote 1 we computed mean differences (MD) also known as Cohen’ d and 95 % confidence intervals (CI) for all studies. Because we expected considerable heterogeneity, we use a random-effects model taking into account both within and between-study variation to compute the overall effect estimate. However, we first tested the heterogeneity using the Q statistic and the I 2 statistic with values of 0.25, 0.50, and 0.75 indicating low, moderate, and high degrees of heterogeneity. Sensitivity analysis by excluding one study at each turn and pooling results from the remainder further confirms the robustness of our findings. To explore the heterogeneity across studies, we conducted subgroup meta-analyses (by assessing the difference between groups in trials with similar participant characteristics). Publication bias was assessed using funnel plot analysis. Visual inspection of a funnel plot can give an indication of publication bias; the studies can be expected to spread symmetrically about the pooled effect size when publication bias is absent.
Eligibility criteria
Seven RCT [1, 22, 32, 34–37] (giving a total of eight studies) comparing pain during mini-hysteroscopy versus conventional hysteroscopy, involving a total of twenty-three hundred and twenty-two patients were included and analyzed.
Other studies were rejected for the following reasons: De Iaco [38] was to our knowledge the first to publish data on pain and outpatient hysteroscopy, but his work was observational. For the same reason Siristatidis [9], Torok [33], and Cicinelli [30] were also excluded. Bettocchi’s studies had different objectives or were operative hysteroscopy as was De Placido’s paper [39], and authors judged they were not suitable for the purpose of this study.
Bias assessment
Our eight studies were assessed for bias using the Cochrane tool for bias assessment. Revision authors judged blinding of personnel in such studies was very unlikely to be effective as operators always knew which hysteroscope is being used. Randomization was judged low risk in seven series and unclear in one, and so was concealment. Blinding of outcome assessors was attained in three and unclear in five. All studies account for missing cases and selective reporting was unclear in one study. Authors believe studies are high quality, having an overall low risk of bias. (Fig. 2).
Results
In order to allow comparison of means and SD results, input was in reference to a 10 cm scale. Other results were converted as described: for Cicinelli’s 20 cm scale means variation has a \(Y = X/2\) relation with adopted scale. So accordingly \(E\left[ Y \right] = E\left[ Y \right]/2\) for means and \(V\left[ Y \right] = V\left[ X \right]/4\) for variance were taken as comparative values; Kassem reported in absolute numbers and revision authors converted rank classes 1–4 into categories and adapted results to a 0–10 scale, calculating means, variance, and SD for each category.
Giorda’s and Campo’s studies seem to have heterogeneity with all others; we doubled check our data extraction but found heterogeneity was high (I 2 = 99.6 %, p value <0.001). As a result, we conducted a subgroup meta-analysis (high and low effect studies) and the difference between subgroups effect sizes is significant (the correspondent confidence intervals have no overlapping). Meta-analysis of the eight studies showed a significant reduction in pain scores (MD: −3.64; 95 % CI −5.16 to −2.12; test for overall effect p < 0.00001). The implemented subgroup analysis dividing the studies according the effect size strength also showed, for both subgroups, a significant reduction in pain. Fig. 3.
For studies with high effect sizes, the meta-analysis presents MD: −11.26; 95 % CI −12.39 to −10.13 (test for overall effect p < 0.00001); for studies with low effect sizes the meta-analysis reveals MD: −1.15; 95 % CI −1.54 to −0.76 (test for overall effect p < 0.00001).
Results of sensitivity analysis excluding one by one each study in the analysis at a turn and pooling results from the remainder, further confirmed the robust findings of significant reduction in pain scores as shown in Table 1.
Furthermore, as was expected, Campo and Giorda studies show highest influence in the overall results. Inspection of the funnel plots (subgroup analysis) did not indicate possible publication bias as there seems to be a symmetrical distribution around the means (Fig. 4).
Discussion
Data from all studies suggest mini-hysteroscopy is less painful than conventional hysteroscopy in an office, anesthesia free setting. In the subgroup analysis results, although two studies seem outsiders in respect to others, they go in the same direction and favor reduction of pain with miniaturization. Furthermore, there seems to be no significant differences in quality of vision or diagnostic accuracy with reduction in hysteroscope diameter [1, 11, 22, 32, 34–37].
Not all mini-hysteroscopes used were the same size: 3 mm (Rullo), 3.3 mm (Angelis) and 3.5 mm (Pluchino, Campo, Cicinelli, Giorda and Kassem). Our forest plot does not seem to reflect a difference in pain with these small changes in diameter: the high effect size include two 3.5 mm series (Campo and Giorda), while both smaller diameter hysteroscopy studies (Rullos’ 3 mm and Angelis’ 3.3 mm) are in line with the other 3.5 mm studies which showed low effect size. We could be tempted to speculate that further reduction in scope diameters might lead to lower pain perception; however, our analysis suggests there may be a cut off around 3.5 mm, below which reduction of scope size might not further reduce pain. Additional studies comparing slender instruments may be warranted to answer this question.
Regarding the inconsistencies found we offer the following possible explanations: Giorda’s study was conducted exclusively on postmenopausal women, most likely giving rise to a selection bias; on the other hand in Campo’s series, the 5 mm scope arm had to be changed to the mini-hysteroscope in eighty-three cases to complete examination (34 %).
Main findings
Miniaturization of scopes shifts pain levels down, compared to traditional hysteroscopy, allowing accurate gynecological care in an office, anesthetic free environment.
Strengths and limitations
Results showed overall results are very consistent and there seems to be no doubt of a significant reduction of VAS using mini-hysteroscopy. Authors believe that evidence is convincing, accurate, reproducible, and can be extrapolated to general population. For details please refer to Table 2.
Interpretation (findings in light of other evidence)
Miniaturization reduces pain scores and has made hysteroscopy tolerable for most patients.
Conclusions
From the evidence gathered, we must conclude that mini-hysteroscopy is the most acceptable and suitable for office in outpatients. Traditional hysteroscopy (5 mm scopes) may not be the most adequate for this purpose.
Notes
Review manager (RevMan) [Computer Program]. Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration (2008).
References
De Angelis C, Santoro G, Re ME, Nofroni I et al (2003) Office hysteroscopy and compliance: mini-hysteroscopy versus traditional hysteroscopy in a randomized trial. Hum Reprod 18(11):2441–2445
Guida M et al (2006) Vaginoscopic versus traditional office hysteroscopy: a randomized controlled study. Hum Reprod 21(12):3253–3257
Tanha FD, Salimi S, Ghajarzadeh M (2013) Sublingual versus vaginal misoprostol for cervical ripening before hysteroscopy: a randomized clinical trial. Arch Gynecol Obstet 287(5):937–940
Sagiv R et al (2006) A new approach to office hysteroscopy compared with traditional hysteroscopy: a randomized controlled trial. Obstet Gynecol 108(2):387–392
Siristatidis C et al (2010) Office hysteroscopy: current trends and potential applications: a critical review. Arch Gynecol Obstet 282(4):383–388
Diniz DB et al (2010) Pain evaluation in office hysteroscopy: comparison of two techniques. Rev Bras Ginecol Obstet 32(1):26–32
Ekin MYL, Akgöl S (2009) Comparison of Vaginoscopic No Touch Method with The Traditional Method of Outpatient Hysteroscopy. Med J Bak›rköy 5(2):4
Cooper NA et al (2010) Vaginoscopic approach to outpatient hysteroscopy: a systematic review of the effect on pain. BJOG 117(5):532–539
Siristatidis C, Chrelias C (2011) Feasibility of office hysteroscopy through the “see and treat technique” in private practice: a prospective observational study. Arch Gynecol Obstet 283(4):819–823
Dealberti D et al (2013) New mini-resectoscope: analysis of preliminary quality results in outpatient hysteroscopic polypectomy. Arch Gynecol Obstet 288(2):349–353
Romani F et al (2013) The use of different size-hysteroscope in office hysteroscopy: our experience. Arch Gynecol Obstet 288(6):1355–1359
Lagana AS et al (2014) 3D sonohysterography vs hysteroscopy: a cross-sectional study for the evaluation of endouterine diseases. Arch Gynecol Obstet 290(6):1173–1178
Yang R et al (2014) The hysteroscopy and histological diagnosis and treatment value of chronic endometritis in recurrent implantation failure patients. Arch Gynecol Obstet 289(6):1363–1369
Baxter AJ, Beck B, Phillips K (2002) A randomized prospective trial of rigid and flexible hysteroscopy in an outpatient setting. Gynaecological Endoscopy 11(6):357–364
Unfried G et al (2001) Flexible versus rigid endoscopes for outpatient hysteroscopy: a prospective randomized clinical trial. Hum Reprod 16(1):168–171
Raimondo G et al (2010) A randomized controlled study comparing carbon dioxide versus normal saline as distention media in diagnostic office hysteroscopy: is the distension with carbon dioxide a problem? Fertil Steril 94(6): 2319–2322
Cooper NA et al (2011) A systematic review of the effect of the distension medium on pain during outpatient hysteroscopy. Fertil Steril 95(1):264–271
De Angelis C et al (2003) Suppression of pelvic pain during hysteroscopy with a transcutaneous electrical nerve stimulation device. Fertil Steril 79(6):1422–1427
Angioli R et al (2014) Use of music to reduce anxiety during office hysteroscopy: prospective randomized trial. J Minim Invasive Gynecol 21(3):454–459
Floris S et al (2007) Efficacy of intravenous tramadol treatment for reducing pain during office diagnostic hysteroscopy. Fertil Steril 87(1):147–151
Lin YH et al (2005) Use of sublingual buprenorphine for pain relief in office hysteroscopy. J Minim Invasive Gynecol 12(4):347–350
Campo R, Molinas CR, Rombauts L, Mestdagh G, Lauwers M, Braekmans P et al (2005) Prospective multicentre randomized controlled trial to evaluate factors influencing the success rate of office diagnostic hysteroscopy. Hum Reprod 20(1):258–263
Cooper NA et al (2011) Does cervical preparation before outpatient hysteroscopy reduce women’s pain experience? A systematic review. BJOG 118(11):1292–1301
Cooper NA, Khan KS, Clark TJ (2010) Local anaesthesia for pain control during outpatient hysteroscopy: systematic review and meta-analysis. BMJ 340:c1130
Kabli N, Tulandi T (2008) A randomized trial of outpatient hysteroscopy with and without intrauterine anesthesia. J Minim Invasive Gynecol 15(3):308–310
Soriano D et al (2000) Lidocaine spray and outpatient hysteroscopy: randomized placebo-controlled trial. Obstet Gynecol 96(5 Pt 1):661–664
Cengiz H et al (2014) Comparing the efficacy of intrauterine lidocaine and paracervical block in decreasing the pain associated with endometrial biopsy: a randomised trial. Arch Gynecol Obstet 289(3):609–614
Ahmad G et al (2010) Pain relief for outpatient hysteroscopy. Cochrane Database Syst Rev 10(11):CD007710
de Carvalho Schettini JA (2007) Pain evaluation in outpatients undergoing diagnostic anesthesia-free hysteroscopy in a teaching hospital: a cohort study. J Minim Invasive Gynecol 14(6):729–735
Cicinelli E et al (2007) Predictive factors for pain experienced at office fluid minihysteroscopy. J Minim Invasive Gynecol 14(4):485–488
Cicinelli E (2010) Hysteroscopy without anesthesia: review of recent literature. J Minim Invasive Gynecol 17(6):703–708
Rullo S, Sorrenti G, Marziali M, Ermini B, Sesti F, Piccione E et al (2005) Office hysteroscopy: comparison of 2.7- and 4-mm hysteroscopes for acceptability, feasibility and diagnostic accuracy. J Reprod Med 50(1):45–48
Torok P, Major T (2013) Evaluating the level of pain during office hysteroscopy according to menopausal status, parity, and size of instrument. Arch Gynecol Obstet 287(5):985–988
Pluchino N, Ninni F, Angioni S, Artini P, Araujo VG, Massimetti G et al (2010) Office vaginoscopic hysteroscopy in infertile women: effects of gynecologist experience, instrument size, and distention medium on patient discomfort. J Minim Invasive Gynecol 17(3):344–350
Cicinelli E et al (2003) Tolerability and cardiovascular complications of outpatient diagnostic minihysteroscopy compared with conventional hysteroscopy. J Am Assoc Gynecol Laparosc 10(3):399–402
Giorda G et al (2000) Feasibility and pain control in outpatient hysteroscopy in postmenopausal women: a randomized trial. Acta Obstet Gynecol Scand 79(7):593–597
Kassem A, El-Brombly W (2005) Outpatient minihysteroscopy and conventional hysteroscopy: a comparative study. Middle East Fertil Society J 10(3):231–237
De Iaco P et al (2000) Acceptability and pain of outpatient hysteroscopy. J Am Assoc Gynecol Laparosc 7(1):71–75
De Placido G et al (2007) Compliance and diagnostic efficacy of mini-hysteroscopy versus traditional hysteroscopy in infertility investigation. Eur J Obstet Gynecol Reprod Biol 135(1):83–87
Acknowledgments
Revision authors wish to thank Vera Afreixo for her expertise and advice on statistics.
Conflict of interest
The authors have no conflict of interest with any institution private or public.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Paulo, A.A.S., Solheiro, M.H.R. & Paulo, C.O.S. Is pain better tolerated with mini-hysteroscopy than with conventional device? A systematic review and meta-analysis. Arch Gynecol Obstet 292, 987–994 (2015). https://doi.org/10.1007/s00404-015-3731-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3731-0