Abstract
Introduction
The aim of the study was to evaluate the factors that may affect experienced pain during office hysteroscopy performed without anesthesia in an outpatient setting.
Materials and methods
We enrolled the patients into six groups, differentiated by parity, menopausal status and type of the sheath that was used for the examination. During office hysteroscopy the pain score was recorded using a visual analog scale.
Conclusion
Statistical analysis of the results revealed no evidence that parity, menopausal status, or the thickness of the instrument influence the level of experienced pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hysteroscopy is widely accepted as the gold standard for investigation of intrauterine pathologies [1]. Traditionally, hysteroscopy is performed as an inpatient procedure. Anesthesia is required for this method due to the pain caused by grasping and dilatation of the cervix. Blind mechanical dilatation of the cervix increases the risk of uterine perforation. An operating room, with its increased running costs, is also necessary.
Technological improvements resulted in reduced instrument diameters for office hysteroscopes [2]. Dilatation of the cervix can be avoided, so the procedure can be performed in an outpatient setting, without anesthesia. With no risk of anesthetic complications, decreased costs, and shorter hospitalization and recovery times, benefits are evident. Office hysteroscopy allows diagnostic and operative interventions as well [3], and patients tend to respond with increased acceptance and compliance.
On the other hand, fear of pain can be a deterrent factor for patients. The aim of the study was to evaluate the level of pain during office hysteroscopy, depending on parity, menopausal status, and type of procedure.
Materials and methods
The prospective study was conducted at the University of Debrecen Medical and Health Science Center, Department of Obstetrics and Gynecology, between 01.01.2010 and 01.01.2011. Office hysteroscopy was performed for the well-known indications such as abnormal uterine bleeding, infertility, recurrent miscarriage, and lost intrauterine device (IUD).
Contraindications were pelvic inflammatory disease (PID), pregnancy, cervical malignancy, and profuse bleeding. These factors were ascertained via routine gynecological examination.
All examinations were performed between the 5th and the 10th cycle days by the same physician. Written informed consent was obtained from each patient. The modified, “no touch” technique was applied, using a speculum but no tenaculum [4]. The speculum was acceptable for patients as a part of a general gynecological examination, and provided an opportunity for thorough disinfection. The duration of the procedures ranged from 1 to 8 min (diagnostic 1–5 min, operative 2–8 min). No complications were reported during the study. A vasovagal side effect [5] occurred in one case causing nausea, but no vomiting.
A rigid 30°, 2.7 mm optic (EMD Hungary) was used, with a 3.7-mm outer diameter diagnostic and a 5.5-mm outer diameter operative sheath. For the distension, normal saline was used [6] at a controlled pressure of 80–100 mmHg. Diagnostic or operative procedures were used as required. Operative procedures included perturbation, polypectomy, biopsy, and removal of IUD.
Our aim was to evaluate the factors that can influence the experience of pain during diagnostic and operative interventions.
In fact, patients were selected in six main groups: nulliparous premenopausal (nulliparous) diagnostic and operative, non-nulliparous premenopausal (non-nulliparous) diagnostic and operative, and non-nulliparous postmenopausal diagnostic and operative. Non-nulliparous patients had at least one delivery in the anamnesis, in reproductive age. Postmenopausal patients were at least 1 year beyond their last menstruation. Pain scoring by the patient on a visual analog scale (VAS) was recorded [7]. The VAS was a 10-cm printed horizontal line with major and minor tick marks at each cm and mm, respectively, representing a linear continuum from no pain at all (left end, numeric value 0) to maximum pain (right end, numeric value 10); patients were asked after the procedure to place a mark across an unmarked VAS using a pen, at the point they felt most consistent with their experienced pain level. Descriptive statistics of group-specific pain scores including means, standard deviations, standard errors and 95 % confidence intervals of means, and extreme values were calculated. Results were compared statistically across all groups using one-way analysis of variance (ANOVA) with the null hypothesis of expected group means being equal. Post hoc pairwise comparisons were made using student’s two-sample t tests with Bonferroni correction to control overall type I error. The SPSS software package version 18 was used for analysis. P values <0.05 were considered to indicate significance unless the Bonferroni correction was involved.
Results
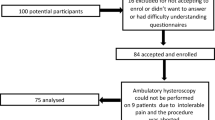
Hysteroscopic examinations on an outpatient basis were performed in 70 cases. Ten cases were included in each but the nulliparous-diagnostic group where we had 20 patients, because most of the procedures were performed upon the indication of infertility. The patients’ mean age was 41.1 years. The mean (SD) pain scores in the groups were: nulliparous-diagnostic, 3.4 (1.27); nulliparous-operative, 3.5 (0.85); non-nulliparous-diagnostic, 3.27 (0.65); non-nulliparous-operative, 3.4 (1.07); postmenopausal-diagnostic, 3.4 (0.84); and postmenopausal-operative, 4.2 (0.92). The overall mean (SD) pain score of the 70 patients was 3.51 (1.01) (Table 1).
One-way ANOVA produced no evidence of a significant overall pain score difference between the groups (p = 0.366) (Table 2). The mean pain score in postmenopausal patients with an operative procedure was higher, but no pairwise difference formed with any of the remaining groups was significant. The severity of experienced pain was not proven to be affected by menopausal status, parity, or type of procedure.
Discussion
For the assessment of the uterine cavity, hysteroscopy is accepted as the gold-standard procedure. Using this endoscopic method, uterine pathology can be diagnosed and treated at the same session. Recent technological developments have led to a decrease in instrument diameter, making it possible for the procedure to be performed in an office setting [8]. Grasping and dilating of the cervix are no longer involved, which precludes the necessity of anesthesia. The indications and contraindications are the same as those for traditional hysteroscopy. Requiring no anesthesia, operating theatre and requisite staff, the office procedure is much more cost-effective. Due to faster recovery and thus less time away from work, cost savings also manifest at the community health care/insurance system level [9].
The aim of the study was to evaluate factors that may influence the experience of pain during hysteroscopy. Pain scores obtained using a VAS were analyzed statistically [10]. Six groups were differentiated according to parity, menopausal status, and diameter of the instrument (diagnostic, 3.7 mm outer sheath diameter; and operative, 5.5 mm outer sheath diameter).
Evaluating data in the literature, we can state, that pain scores during hysteroscopy comparable to scores registered by other authors using the same size instrument [11]. These values satisfy the criteria of mild pain category. In light of the results we can say that the evaluated factors (menopausal status, parity, diameter of the instrument) have not been proven to affect the level of experienced pain. Interpreting these findings, we can propose that the pain levels observed may have been influenced by individual differences of pain tolerance only.
A potential limitation of the study is its sample size. However, working with a scenario based on our group sizes, assuming observed overall sample pain score SD in each group, and all group means but one being expected to be equal, the study was sufficiently (80 %) powered for the detection of a 1.3-point difference on the pain score scale used if the deviating group was a 10-subject group, or for the detection of a 1-point difference if it was the 20-subject group (based on empirical type II error rates from 3,000 simulated ANOVA runs). We believe that these detection thresholds are acceptably close to where between-group differences begin to be clinically meaningful.
Office hysteroscopy is known to be a viable and appropriate method in the diagnosis and treatment of the uterine cavity. Thanks to improved parameters of the instrument and the new procedural technique, both diagnostic and operative hysteroscopy can be carried out without anesthesia, as an outpatient care procedure [12]. By diagnosing and operating deformities hysteroscopically in an office setting, considerable costs, strain, and time can be saved, to benefit both the patient and the physician. In experienced hand the associated discomfort is tolerable [13], and our explorative findings are consistent with the hypothesis that it is uniform in intensity across levels of parity, menopausal status, and instrument diameter, although proof thereof will be the matter of a subsequent equivalence study [14]. Future directions of related research include the evaluation of further stratification factors for heterogeneity in experienced pain intensity (comorbidities, concomitant medication used, etc.), with the potential of identifying patient subgroups where special pain management considerations may be warranted due to elevated levels of discomfort sensitivity.
References
Bettocchi S, Nappi L, Ceci O, Selvaggi L (2004) Office hysteroscopy. Obstet Gynecol Clin North Am 31:641–654
Nagele F, O’Connor H, Davies A, Badawy A, Mohamed H, Magos A (1996) 2,500 Outpatient diagnostic hysteroscopies. Obstet Gynecol 88:87–92
Bettocchi S, Ceci O, Nappi L et al (2004) Operative office hysteroscopy without anesthesia: analysis of 4,863 cases performed with mechanical instruments. J Am Assoc Gynecol Laparosc 11:59–61
Bettocchi S, Selvaggi L (1997) A vaginoscopic approach to reduce the pain of office hysteroscopy. J Am Assoc Gynecol Laparosc 4:255–258
Agostini A, Bretelle F, Ronda I, Roger V, Cravello L, Blanc (2004) Risk of vasovagal syndrome during outpatient hysteroscopy. J Am Assoc Gynecol Laparosc 11:245–247
Cooper NA, Smith P, Khan KS, Clark TJ (2011) A systematic review of the effect of the distension medium on pain during outpatient hysteroscopy. Fertil Steril 95(1):264–271 (Epub 2010 Jun 23)
de Carvalho Schettini JA, Ramos de Amorim MM, Ribeiro Costa AA, Albuquerque Neto LC (2007) Pain evaluation in outpatients undergoing diagnostic anesthesia-free hysteroscopy in a teaching hospital: a cohort study. J Minim Invasive Gynecol 14(6):729–735
Siristatidis C, Chrelias C, Salamalekis G, Kassanos D (2010) Office hyster-oscopy: current trends and potential applications: a critical review. Arch Gynecol Obstet 282(4):383–388
Marsh F, Kremer C, Duffy S (2004) Delivering an effective outpatient service in gynaecology. A randomised controlled trial analysing the cost of outpatient versus daycase hysteroscopy. BJOG 111(3):243–248
Huskisson EC (1974) Measurement of pain. Lancet 2:1127–1131
Cicinelli E (2010) Hysteroscopy without anesthesia: review of Recent Literature. J Minim Invasive Gynecol 17(6):703–708
Isaacson K (2002) Office hysteroscopy: a valuable but under-utilized technique. Curr Opin Obstet Gynecol 14:381–385
Leone FPG, Carsana L, Lanzani C, Vago G, Ferrazzi E (2007) Sonohysterographic endometrial sampling and hysteroscopic endometrial biopsy: a comperative study. Ultrasound Obstet Gynecol 29:443–448
Cooper NA, Smith P, Khan KS, Clark TJ (2011) Does cervical preparation before outpatient hysteroscopy reduce women’s pain experience?A systematic review. BJOG 118(11):1292–1301
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Török, P., Major, T. Evaluating the level of pain during office hysteroscopy according to menopausal status, parity, and size of instrument. Arch Gynecol Obstet 287, 985–988 (2013). https://doi.org/10.1007/s00404-012-2667-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2667-x