Abstract
Purpose
To evaluate the efficacy of two routes of misoprostol (sublingual and vaginal) for cervical ripening before hysteroscopy.
Methods
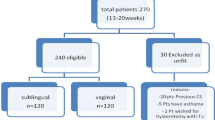
One hundred and ten perimenopausal women who were referred to a tertiary hospital for surgical hysteroscopy enrolled in this double-blind randomized clinical trial. They were divided into two groups to receive 400 mg misoprostol either sublingually or vaginally 6 h before hysteroscopy. The duration of dilatation, Hegar number inserted into the cervix without resistance, and hysteroscopic and drug complications were recorded for all cases.
Results
Forty-nine women in sublingual and 51 in vaginal group participated in the study. Dilatation time was significantly lower in sublingual group (P < 0.001). Median Hegar number passed into the cervix without resistance was 5 in sublingual versus 4 in vaginal group (P = 0.002). Cramp followed by vomiting and diarrhea were the most common side effects of misoprostol in the sublingual group, while cramp followed by vomiting was the most frequent side effect in the vaginal group. Diarrhea was not reported in the vaginal group (P = 0.008).
Conclusion
Sublingual route of misoprostol could be considered as an effective medication before surgical hysteroscopy in perimenopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hysteroscopy is the main diagnostic and therapeutic procedure applied for patients with infertility, suspected intra-uterine pathologies and abnormal bleeding [1, 2]. It is also a therapeutic method for several uterine pathologies all over the world. Its low cost and quick and simple procedure have made it widely popular.
Although hysteroscopy has been considered as a safe and less invasive procedure, some complications such as cervical tear, bleeding, uterine perforation, pain and discomfort may occur during the process [3, 4]. Many women need dilatation prior to hysteroscopy to make the procedure simpler.
Misoprostol (prostaglandin E1 analog) is a drug of choice for cervical ripening, labor induction, post-partum hemorrhage and pregnancy termination [5]. Cervical ripening before hysteroscopy with misoprostol could make passage of hysteroscope easier with fewer complications [6] (Fig. 1).
Sublingual and vaginal routes are common routes of misoprostol applied for cervical ripening before hysteroscopy. Rapid absorption leading to reach peak concentration and higher bioavailability are advantages of sublingual route administration, while vaginal route administration leads to longer sustained and regular uterine contractions [7, 8]. The objective of this study was to compare the effectiveness of sublingual versus vaginal misoprostol used to facilitate cervical dilatation before surgical hysteroscopy.
Materials and methods
One hundred and ten perimenopausal women, admitted in tertiary hospital of women’s health (affiliated hospital of Tehran University of Medical Sciences) for surgical hysteroscopy between June 2011 to January 2012, enrolled in this randomized double-blind clinical trial. Exclusion criteria were: glaucoma, hypertension, allergic reaction to misoprostol, asthma, renal failure, vaginal prolapse and previous cervical surgery.
They were randomly allocated to either to the sublingual group or the vaginal group by computer-generated random sequences and a blinded technician. All patients filled informed consent forms for being involved in the study, although the study had been approved by Ethics committee of Tehran University of Medical Sciences (ID number: IRCT201012272576N3). Six cases from sublingual and four from vaginal group withdrew before the study commenced. Both the investigator and the patients were blinded to the treatment assignment.
Women in sublingual group took a 400 μg misoprostol tablet under the tongue 6 h before hysteroscopy, and a vit-B6 tablet was administered into their posterior fornix by investigator. While in the other group, a 400 μg misoprostol was administered into the posterior fornix by investigator and the patient took a vit-B6 tablet.
Hysteroscopy was done under general anesthesia by a simple expert surgeon. A rigid hysteroscope with an outer sheath of 9-mm in diameter and a 30° fore-oblique lens was used (Karl Storz, Tuttlingen, Germany). The uterine cavity was distended with normal saline; 25–30 mL of normal saline was injected for 1 min with an average flow and at a pressure of 100−150 mm Hg. Duration of dilatation, Hegar number inserted into the cervix without resistance, and hysteroscopic and drug complications were recorded for all cases.
Statistical analyses were performed with SPSS software version 18.0 (Statistical Product and Service Solutions, SSPS Inc., Chicago). Results are presented as mean ± SDs, median and frequencies. The Student’s t test was used for continuous variables, and the Pearson χ 2 test with Fisher’s exact test was applied for categorical variables. P value <0.05 was considered statistically significant.
Results
Forty-nine women in sublingual and 51 in vaginal group were evaluated.
There was no difference in women’s age, gravidity, number of previous cesarean sections, and reason for hysteroscopy (Table 1).
Dilatation time was significantly lower in sublingual group. Median Hegar number passed into cervix without resistance was 5 in sublingual versus 4 in vaginal group (Table 2).
Cramp followed by vomiting and diarrhea were the most common side effects of misoprostol in sublingual group, while cramp followed by vomiting was the most frequent side effects in vaginal group. Diarrhea was not reported in vaginal group (Table 3).
We observed no complication of hysteroscopy in either group.
Discussion
Our study was the first study evaluating effectiveness of vaginal versus sublingual misoprostol for cervical ripening in Iranian women. We found that dilatation time was significantly lower in sublingual group, and the most frequent Hegar number applied into the cervix without resistance for dilation was 5 in sublingual group and 4 in vaginal group, indicating more effectiveness of sublingual route for ripening in comparison with vaginal group. In a study by Mulayim et al., two groups of women who received sublingual misoprostol or placebo before hysteroscopy were compared with each other. Dilatation time was higher in placebo group. Furthermore, cervical tearing had occurred more often in placebo group than in misoprostol group [9]. In another study, Bisharah et al. evaluated 40 women who were randomly assigned to treatment with 100 mg sublingual misoprostol or placebo before hysteroscopy. They observed no difference in degree of cervical dilatation between the two groups [10]. One of the prominent strengths of our study was evaluation of two different routes of misoprostol in one study. Most previous studies evaluated only one route of misoprostol. For instance, Preutthipan and Herabutya [11] recognized that vaginal misoprostol could reduce time of dilation to Hegar number 9 in premenopausal nulliparous women. On the other hand, Fernandez et al. [12] found that vaginal misoprostol applied 4 h before hysteroscopy in premenopausal women was not effective for cervical dilatation.
The other form of misoprostol, oral route, had also been previously investigated for cervical ripening. Sordia-Hernandez et al. [13] applied oral and vaginal forms before hysteroscopy in 75 infertile patients. They reported that surgical time was significantly lower in vaginal group in comparison with oral and placebo groups. On the other hand, Choksuchat et al. [14] suggested that 400 μg oral misoprostol is as effective as 200 μg vaginal route for cervical ripening before hysteroscopy.
In our study, cramp and vomiting were the most frequent side effects of misoprostol in both groups, although diarrhea and vomiting were higher in sublingual group. Previous studies indicate that chills, fever, diarrhea and vomiting had higher rates in cases who underwent sublingual route of misoprostol for treatment [15, 16]. In a study by Sordia-Hernandez et al. [13] nausea and abdominal pain were reported as side effects more frequently occurred in vaginal group than in oral customers.
Conclusion
Sublingual route of misoprostol could be considered as an effective medication before surgical hysteroscopy in perimenopausal women.
References
Munro MG, Jensen J, Purdon TF (1994) Narrow caliber office hysteroscope. J Am Assoc Laparosc 1:S24
Campo R, Van Belle Y, Rombatus L, Brosens I, Gordts S (1999) Office mini-hysteroscopy. Hum Reprod Update 5:73–81
Jansen FW, Vredevoogd CB, van Ulzen K, Hermans J, Trimbos JB, Trimbos-Kemper TC (2000) Complications of hysteroscopy: a prospective, multicenter study. Obstet Gynecol 96:266–270
Loffer FD (1989) Hysteroscopy with selective endometrial sampling compared with D&C for abnormal uterine bleeding: the value of a negative hysteroscopic view. Obstet Gynecol 73:16–20
Goldberg AB, Greenberg MB, Darney PD (2001) Misoprostol and pregnancy. N Engl J Med 344:38–47
Ngai SW, Chan YM, Liu KL, Ho PC (1997) Oral misoprostol for cervical priming in non-pregnant women. Hum Reprod 12:2373–2375
Khan RU, El-Refaey H, Sharma S, Sooranna D, Stafford M (2004) Oral, rectal and vaginal pharmacokinetics of misoprotol. Obstet Gynecol 103:866–870
Tang OS, Schweer H, Seyberth HW, Lee SW, Ho PC (2002) Pharmacokinetics of different routes of administration misprostol. Hum Reprod 17:332–336
Mulayim B, Celik NY, Celik G, Bagis T, Zeyneloglu HB (2010) Sublingual misoprostol for cervical ripening before diagnostic hysteroscopy in premenopausal women: a randomized, double blind, placebo-controlled trial. Fertil Steril 93:2400–2404
Bisharah M, Al-Fozan H, Tulandi T (2003) A randomized trial of sublingual misoprostol for cervical priming before hysteroscopy. J Am Assoc Gynecol Laparosc 10:390–391
Preutthipan S, Herabutya Y (2006) A randomized comparison of vaginal misoprostol and dinoprostone for cervical priming in nulliparous women before operative hysteroscopy. Fertil Steril 86:990–994
Fernandez H, Alby JD, Tournoux C, Chauveaud-Lambling A, DeTayrac R, Frydman R et al (2004) Vaginal misoprostol for cervical ripening before operative hysteroscopy in pre-menopausal women: a doubleblind, placebo-controlled trial with three dose regimens. Hum Reprod 19:1618–1621
Sordia-Hernandez LH, Rosales-Tristan E, Vazquez-Mendez J, Merino M, Iglesias JL, Garza-Leal JG, Morales A (2011) Effectiveness of misoprostol for office hysteroscopy without anesthesia in infertile patients. Obstet Gynecol 95:759–761
Choksuchat C, Cheewadhanaraks S, Getpook C, Wootipoom V, Dhanavoravibul K (2006) Misoprostol for cervical ripening in non-pregnant women: a randomized double-blind controlled trial of oral versus vaginal regimens. Hum Reprod 21:2167–2170
Saxena P, Salhan S, Sarda N (2004) Comparison between the sublingual and oral route of misoprostol for pre-abortion cervical priming in first trimester abortions. Hum Reprod 19:1–4
Tang OS, Gemzell-Danielsson K, Ho PC (2007) Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynaecol Obstet 99(Suppl 2):S160–S167
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanha, F.D., Salimi, S. & Ghajarzadeh, M. Sublingual versus vaginal misoprostol for cervical ripening before hysteroscopy: a randomized clinical trial. Arch Gynecol Obstet 287, 937–940 (2013). https://doi.org/10.1007/s00404-012-2652-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2652-4