Abstract
Purpose
Radial magnetic resonance imaging (MRI) is the most accurate diagnostic tool in assessing cam-type femoroacetabular impingement. Plain radiographs, however, are useful for the initial diagnosis in the daily practice and there is still debate regarding the optimal lateral view. The purpose of this study was to investigate the reliability of detecting cam deformities using the frog-leg view or the 45° Dunn view by comparison with radial MRI.
Material
66 consecutive hips with plain radiographs (36 with AP and frog-leg views, 30 with AP and 45° Dunn views) and radial MRI were assessed. Alpha angle measurements were obtained both for radiographs and for radial MRI reformats by two investigators. Statistics included frequency analysis, bivariate linear correlation analyses, and cross-table analyses testing the sensitivity and specificity of the radiographic projections for detecting an alpha angle larger than 55°.
Results
The intra-class correlation revealed excellent agreement between the two raters [ICC = 0.959, CI (0.943; 0.972)]. 50% (33/66) had the maximum alpha angle in the superior–anterior aspect of the femoral head–neck junction. Cam deformity was found in 40/66 cases (61%) in radial MRI. Pearson correlation demonstrated that the 45° Dunn view was most accurate for the superior–anterior aspect (0.730, p < 0.05). The frog-leg view was best suited for the anterior aspect (0.703, p < 0.05). The sensitivity for detecting cam deformities in the 45° Dunn view was 84 vs 62% in the frog-leg view.
Conclusion
The frog-leg lateral radiograph does not provide reliable measurements of the alpha angle. This study highlights the importance of the 45° Dunn view for early detection of femoroacetabular cam-type impingement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) is postulated to be a major risk factor for early osteoarthritis of the hip [1,2,3]. Cam-type FAI is characterized by an aspherical cartilage bearing area at the femoral head–neck junction, which is the result of a relative prominence of the head or a decreased femoral head offset. The abutment of the head–neck junction against the acetabulum will lead to labral tears and cartilage damage [1,2,3,4,5,6,, 4, 5]. Therefore, the early diagnosis is important to plan the surgical correction of the head deformity prior the onset of significant osteoarthritis [6]. The most accurate diagnostic imaging to examine the full circumference of the femoral head–neck junction and thus not to miss any subtle deformity is magnetic resonance imaging (MRI) with radial slices [7,8,9]. In this technique, the slices are positioned in a clockwise way around the axis of the femoral neck. As a quantitative measure of the sphericity of the femoral head, the alpha angle is a reliable indicator of cam-type FAI and may also be used for assessing operative correction [10]. However, this complex diagnostic technique is restricted to specialist radiologists and surgeons in the field of hip joint MRI. In terms of first-line diagnostics of cam-type FAI, plain radiographs are essential as representing a widely available and less costly diagnostic tool. Several lateral view radiographs including the cross-table view, frog-leg lateral view, 90° Dunn view, and 45° Dunn view for assessing FAI have been described with varying results [11,12,13,14,15,16]
Clohisy et al. [11] concluded that the frog-leg lateral view is a good predictor of femoral head–neck offset in patients with FAI. Another study [16], however, has demonstrated that it is not a reliable method for measuring the alpha angle. Recent studies suggest that the 45° Dunn view is superior to other lateral radiographic projections in the detection of cam-type FAI [13, 15, 17, 18]. In clinical routine, however, a two-view radiographic series including an anteroposterior (AP) pelvis view and a frog-leg view is widely used in the initial evaluation of the painful hip and there is still debate on the optimal lateral view to screen for cam deformities. Thus, the purpose of this study was to evaluate the accuracy of the frog-leg view in identifying cam deformities by comparison with radial MRI. We hypothesized that the frog-leg view is not as sensitive as the 45° Dunn view and that radiographic assessment alone would not detect all cam lesions.
Materials and methods
We reviewed a prospectively collected MRI database of a consecutive series of patients who had obtained three-dimensional (3D) MRI between January 2010 and December 2011 for diagnostic evaluation of a painful hip. The inclusion criteria were met if both radial MRI and radiographs in two planes including either 45° Dunn or frog-leg views were available, and MRI and radiographs had been obtained within 3 months. Cases with slipped capital femoral epiphysis, Legg–Calve–Perthes disease, or prior femoral neck fracture were excluded. The study design was approved by the local institutional review board.
A total of 66 hips in 60 patients (30 female and 30 male) with a mean age of 41 years (17–69) were identified. 36 hips had been assessed with AP pelvis and frog-leg views and 30 hips with AP pelvis and 45° Dunn views. All cases were investigated at the orthopaedic and radiology departments of a single institution.
Imaging protocols
All plain radiographs were taken by radiology technologists using standardized techniques with a tube-to-film distance of approximately 100 cm. For the AP views, all projections were obtained in a supine position with the legs in 15° internal rotation and the crosshairs of the beam centred midway between the symphysis pubis and the field included both iliac crests. The frog-leg lateral view was taken with the patient supine on the radiographic table and the ipsilateral knee was flexed, so that the foot contacted the contralateral knee. The thigh was abducted and externally rotated while ensuring that the plane of the pelvis was parallel to the plane of the table. The projection was directed anterior to posterior and centred on the femoral head. The 45° Dunn view was obtained with the patient supine and the symptomatic hip flexed at 45° and abducted 20° in neutral rotation [19].
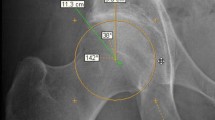
MRI images were obtained with a 3 Tesla system (Achieva, Philips Medical System, Hamburg, Germany) using a flexible eight channel surface coil. The imaging protocol included an isotropic 3D dual flip angle T1 sequence with a 160 mm field-of-view (FOV) and 192 pixels base resolution resulting in a voxel size of 0.83 mm × 0.83 mm × 0.83 mm. Repetition times (TR) were between 10 and 18 ms, echo times (TE) ranged from 3 to 7 ms, the flip angles (FA) were 25°/28°, and an acceleration factor of 2 was used resulting in a time of acquisition of 10 min. Consequently, this 3D data set was used to reconstruct radial reformats rotating around the femoral head–neck axis in 30° intervals on a Picture Archiving and Communications System (PACS) using OsiriX® (Version 4.1.2—32-Bit,© Antoine Rosset, 2003–2013) (Fig. 1).
Alpha angle measurement
All angle measurements were carried out using a custom software programmed on a Java™ platform. To establish reliability, measurements were made by two observers (CH and MT) in a blinded manner. The alpha angle was measured according to the method described by Nötzli et al. and an angle greater than 55° on the image was considered indicative of cam deformity [10]. The centre of the femoral head was determined using a circular template interpolated from three reference points on the femoral head: the first point was at the level of lateral edge of the sourcil, the second point at the level of the medial border of the sourcil, and the third point at the inferior-medial femoral head. The axis of the femoral neck was defined by the centre of the femoral head and the mid-point of the narrowest part of the femoral neck. The alpha angle was then defined as the angle between the femoral neck axis and the line from the circle centre to the point, where the anterolateral prominence was seen at the head–neck junction outside the best-fit circle and extended in a convex shape to the base of the neck (Fig. 2). The alpha angle measured on the plain radiographs was compared with that calculated using the 3D reconstructed MRI. In MRI, the alpha angles were measured using the reconstructed radial slices of the MRI in seven cuts (anterior, anterior–superior, superior–anterior, superior, superior–posterior, posterior–superior, and posterior) around the femoral head–neck junction [10]. In each plane, a best-fit circle was drawn based on three points on the bony outline of the femoral head. Two points were chosen at the edge of the acetabulum and a third point at the medial edge of the sourcil; in the coronal plane, the lateral and medial edge of the sourcil, and a third point at the offset on the opposite side were chosen. The femoral neck axis and alpha angle were assessed using the same technique, as described above (Fig. 3).
Statistical analyses
An intra-class correlations coefficient (ICC) was calculated to test for agreement between the two observers. Consequently, the mean of these readings was used for statistical analysis. As a baseline measure, frequency analysis of the maximum alpha angle location and descriptive analysis of mean alpha angle size were carried out. A two-sided t test was performed to test for differences between the two patient subgroups (frog-leg/45° Dunn view). To test for the correlation of different MRI measures with the two different radiograph techniques, Pearson correlation coefficients were calculated. The alpha level for all tests was set at p = 0.05.
Using the maximum alpha angles assessed in radial MRI as state variable, cross-table analyses were carried out to test for the sensitivity and specificity for the detection of alpha angles larger than 55° of both radiographs and of radiographs augmented with oblique axial MRI, as seen in the anterior radial reconstruction.
All statistical analyses were performed by an investigator (VS) using the Statistical Package for the Social Sciences, Version 20.0 (SPSS, Chicago, IL, USA).
Results
The ICC of the alpha angle measurements revealed excellent agreement between the two observers [ICC = 0.959, CI (0.943; 0.972)].
Radial MRI demonstrated that the maximum alpha angle was located in the superior–anterior region in 50% of the cases. Cam deformity (alpha angle > 55°) was found in 40/66 of the cases (60.6%). Maximum alpha angles ranged from 36.6° to 94.9° (Table 1). The age, the sex, the maximum alpha angle as well as the location of the deformity assessed in radial MRI did not differ significantly between the patient subgroups (p > 0.05).
Cam deformity in radiographs was found in 31.8% (21/66) of the AP views and in 48.5% (32/66) of the lateral views (frog-leg/45° Dunn view). In the frog-leg view subgroup 61.9% (13/21) and in the 45° Dunn view subgroup, 84.2% (16/19) of the MRI detected cam lesions could be detected, respectively. When all radiographic views were utilized, 77.5% of the cam deformities (31/40) were identified. The range of the alpha angles was 36.7°–90.5° in the AP view, 31.5°–89.6° in the frog-leg view, and 39.9°–81.9° in the 45° Dunn view.
Bivariate correlation analysis of the alpha angles obtained moderate-to-high correlation scores for both radiographic views with the radial MRI (Table 2); the highest correlation was found between the 45° Dunn view and the superior–anterior MRI radial alpha angle. In the frog-leg view group, the highest correlation coefficient was found with the anterior MRI alpha angle. Overall, the correlation for the 45° Dunn view group was stronger than for the frog-leg view group; however, this was not significant.
The sensitivity of the frog-leg view for an alpha angle > 55° in radial MRI was 61.9% (13/21). 38.1% (8/21) were falsely negative (alpha angle smaller than 55° in the frog-leg view but larger than 55° in radial MRI), and 13.3% (2/15) were falsely positive. For the 45° Dunn view, the sensitivity for detection of a cam lesion was 84.2% (16/19). The specificity was 90.9% (10/11), 15.8% (3/19) were falsely negative, and 9.1% (1/11) falsely positive (Table 3). The ratio of right-positive cases was significantly higher in the 45° Dunn view than in the frog-leg view (p < 0.05, Chi-Square test).
Discussion
An accurate radiological evaluation is critical for diagnosis and surgical-decision making in cam-type FAI. Yet, the most sensitive diagnostic tool is MRI including radial oblique reformats, representing the current gold standard in the assessment of cam deformities as well as labral and chondral lesions [8, 13]. While investigators agree that the deformity of the femoral head–neck junction most commonly occurs at the superior–anterior quadrant, it remains unclear if those abnormalities can be accurately characterized in standardized plain radiographs [10, 12, 13, 15, 18, 20]. In our study, we evaluated the effectiveness of two plain lateral radiographic views (frog-leg and 45° Dunn view) in identifying cam-type FAI by comparison with radial MRI. We have found that frog-leg lateral radiographs are inferior compared to 45° Dunn views in characterizing head–neck abnormalities and that radial MRI still remains necessary as gold standard in terms of operative planning and follow-up. In concordance with the results recently reported by Saito et al. [15], our study underlines the importance of the 45° Dunn view to improve first-line diagnostics and establish a screening method for cam deformities.
Our data must be viewed with limitations. First, although orthopedic radiology technicians performed the radiographs, variations in patient positioning were possible and could have affected the uniformity of the radiographs. This variability is minimized with the standardized technique performed at a single institution. Second, due to the retrospective design, no subjects having both lateral views were analyzed and the study lacks a control group of subjects without hip pain, causing a potential bias. The matching of the two groups was based on the radiographic baseline data. Third, despite standardized technique to reconstruct radial MRI slices, there could be limited accuracy in determining the exact location on the femoral head–neck junction.
We used the alpha angle described by Nötzli et al. [10] for the characterization of an aspheric head because of its high reliability and considered an angle of 55° as a threshold between normal and abnormal offset. More recently, a value of > 50.5° was used for diagnosing cam FAI; however, it is still controversial what alpha angle values definitely represent an abnormal femoral head–neck junction [17, 21, 22].
In the current study population, the inter-observer reliability was excellent for all views, again underlining the reproducibility of this radiographic parameter. We found that 40 of 66 cases had cam deformity in radial MRI and the maximum extent was found in the superior–anterior position in half of the cases. Overall, radiographs were less sensitive than radial MRI for the detection of cam deformity (77.5% sensitivity).
Separate evaluation of the frog-leg and 45° Dunn view showed that only 61.9% were detected with frog-leg views, whereas the 45° Dunn view provided good sensitivity (84.2%). Correlation analyses demonstrated that the frog-leg view apparently has good agreement with the alpha angles in the anterior radial reconstruction; in contrast, the 45° Dunn view measurements predominantly agreed with the superior–anterior aspect of the femoral head–neck junction. These findings are similar compared to those recently reported in the literature [13, 14, 15, 17]. Some previous studies, however, have not demonstrated a strong correlation between the frog-leg view and locations on the femoral head–neck junction [11, 16].
Clohisy et al. [11] compared three radiological modalities (AP, cross-table lateral, and frog-leg view) and concluded that the frog-leg view was the best predictor of femoral head–neck offset in patients with FAI. Konan et al. [16] questioned the validity of the frog-leg lateral radiograph in evaluating FAI. These authors have only seen poor correlation of alpha angles on frog-leg lateral radiographs to measurements on three-dimensional imaging. However, in our study, there was a strong correlation between the frog-leg view and the anterior position. These findings are consistent with the study previously reported by Nepple et al. [14]. At least, these data emphasize that the frog-leg view can be clinically useful in identifying malformations, especially on the anterior head–neck junction. Furthermore, the ‘hip vacuum sign’, which was described recently, can be found only on frog-leg lateral views as a direct hint for mechanical relevant impingement deformities [23]. Therefore, the frog-leg view may also play an important role in first-line diagnostics of cam-type FAI.
Based on the current series and on reports in the literature, the majority of cases can be expected to have the maximum cam deformity in the superior–anterior aspect of the femoral head [8, 12, 13, 20, 24]. As the 45° Dunn view most strongly correlates with this location, it may be best suited for the detection of cam deformities. In fact, the 45° Dunn view showed high sensitivity (84.2%) as well as specificity (90.9%) in our series and as expected strongly correlated with the superior–anterior radial oblique image, the most common location of deformity in this cohort. Surprisingly, the correlation with the anterior–superior location was not as strong as previously reported in the literature [13, 14, 15]. In 10.6% of the current population, however, maximal deformity was present at the superior or anterior neck.
Several previous studies showed that the cross-table lateral radiograph does not appear to provide high sensitivity or additional information [11, 13, 14, 17]. We have also found that the frog-leg lateral radiograph is more consistently reliable than the cross-table lateral radiograph in clinical use. This may be contributed to the facts that the positioning for this view is easier and the radiation exposure is lower compared to the cross-table lateral view. Additional shielding of the gonads is also not applicable when performing cross-table radiographs. The frog-leg view, however, has the disadvantage of an overlap of the greater trochanter with the head–neck junction and alpha angle measurements, therefore, can be difficult.
Beaule et al. [25] initially suggested CT of the hip for the assessment of FAI, and later, Nepple et al. [14] used it as their 3D imaging standard. With regard to radiation exposure [26] and additional visualization of the structural anatomy, we find that MRI with radial oblique reformats is preferable to 3D CT. Nepple et al. [14] also reported, that for diagnostic and treatment purposes, a three-view radiographic hip series (AP, 45° Dunn, and frog-leg view) accurately identifies femoral head–neck junction malformations without the need of additional three-dimensional imaging/CT. In our study, radiographic assessment alone did only detect 77.5% of all cam deformities, and therefore, we find that MRI remains indispensable for an accurate characterization of the femoral head–neck junction, especially with respect to operative treatment [27].
Conclusion
The frog-leg view is the less sensitive plain lateral radiograph compared to the 45° Dunn view in detecting cam-type FAI. The frog-leg and AP pelvis view best characterize the anterior and superior aspect of the femoral head–neck junction, respectively. The 45° Dunn view particularly aims at the superior–anterior position, where maximum cam deformity is found in the majority of cases. Therefore, the 45° Dunn view may be the optimal lateral view in the radiographic evaluation of the young adult hip to screen for cam deformities.
References
Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 417:112–120
Ganz R, Leunig M, Leunig-Ganz K, Harris WH (2008) The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 466:264–272
Tanzer M, Noiseux N (2004) Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res 429:170–177
Beck M, Kalhor M, Leunig M, Ganz R (2005) Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Jt Surg Br 87:1012–1018
Siebenrock KA, Wahab KHA, Werlen S, Kalhor M, Leunig M, Ganz R (2004) Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res 418:54–60
Spencer S, Millis MB, Kim Y-J (2006) Early results of treatment of hip impingement syndrome in slipped capital femoral epiphysis and pistol grip deformity of the femoral head–neck junction using the surgical dislocation technique. J Pediatr Orthop 26:281–285
Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R (2004) Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res 418:74–80
Pfirrmann CWA, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J (2006) Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology 240:778–785
Klenke FM, Hoffmann DB, Cross BJ, Siebenrock KA (2015) Validation of a standardized mapping system of the hip joint for radial MRA sequencing. Skelet Radiol 44:339–343
Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J (2002) The contour of the femoral head–neck junction as a predictor for the risk of anterior impingement. J Bone Jt Surg Br 84:556–560
Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL (2007) The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res 462:115–121
Dudda M, Albers C, Mamisch TC, Werlen S, Beck M (2009) Do normal radiographs exclude asphericity of the femoral head–neck junction? Clin Orthop Relat Res 467:651–659
Domayer SE, Ziebarth K, Chan J, Bixby S, Mamisch TC, Kim YJ (2011) Femoroacetabular cam-type impingement: diagnostic sensitivity and specificity of radiographic views compared to radial MRI. Eur J Radiol 80:805–810
Nepple JJ, Martel JM, Kim Y-J, Zaltz I, Clohisy JC, ANCHOR Study Group (2012) Do plain radiographs correlate with CT for imaging of cam-type femoroacetabular impingement? Clin Orthop Relat Res 470:3313–3320
Saito M, Tsukada S, Yoshida K, Okada Y, Tasaki A (2017) Correlation of alpha angle between various radiographic projections and radial magnetic resonance imaging for cam deformity in femoral head–neck junction. Knee Surg Sports Traumatol Arthrosc 25(1):77–83
Konan S, Rayan F, Haddad FS (2010) Is the frog lateral plain radiograph a reliable predictor of the alpha angle in femoroacetabular impingement? J Bone Jt Surg Br 92:47–50
Barton C, Salineros MJ, Rakhra KS, Beaulé PE (2011) Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res 469:464–469
Meyer DC, Beck M, Ellis T, Ganz R, Leunig M (2006) Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res 445:181–185
Dunn DM (1952) Anteversion of the neck of the femur; a method of measurement. J Bone Jt Surg Br 34-B:181–186
Rakhra KS, Sheikh AM, Allen D, Beaulé PE (2009) Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res 467:660–665
Beaulé PE, Le Duff MJ, Zaragoza E (2007) Quality of life following femoral head–neck osteochondroplasty for femoroacetabular impingement. J Bone Jt Surg Am 89:773–779
Tannast M, Siebenrock KA, Anderson SE (2007) Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol 188:1540–1552
Schroeder JH, Marschalek N, Hufeland M, Perka C (2016) The “Hip Vacuum Sign”—a new radiographic phenomenon in femoro-acetabular impingement. J Hip Preserv Surg 3:346–351
Ito K, Minka MA, Leunig M, Werlen S, Ganz R (2001) Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head–neck offset. J Bone Jt Surg Br 83:171–176
Beaulé PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ (2005) Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res 23:1286–1292
Berrington de González A, Darby S (2004) Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 363:345–351
Radetzki F, Saul B, Hagel A, Mendel T, Döring T, Delank KS, Wohlrab D, Stoevesandt D (2015) Three-dimensional virtual simulation and evaluation of the femoroacetabular impingement based on “black bone” MRA. Arch Orthop Trauma Surg 135:667–671
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No funding was received.
Rights and permissions
About this article
Cite this article
Hipfl, C., Titz, M., Chiari, C. et al. Detecting cam-type deformities on plain radiographs: what is the optimal lateral view?. Arch Orthop Trauma Surg 137, 1699–1705 (2017). https://doi.org/10.1007/s00402-017-2793-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2793-9